Abstract
We retrospectively evaluated demographic and biochemical parameters associated with depression and health-related quality of life (HRQOL) in maintenance peritoneal dialysis (PD) patients. This study included 105 patients maintaining PD at Seoul National University Hospital. Data were collected from electronic medical record. Korean Beck's Depression Inventory and Korean version of Kidney Disease Quality of Life short form, version 1.3 were used to evaluate depression and HRQOL, respectively. Moderate to severe depression was found in 24.8% of patients. Patients with lower normalized protein equivalent of nitrogen appearance (nPNA) (< 1.2 g/kg/day), lower weekly renal Kt/Vurea (< 0.2), and lower serum albumin level (≤ 4.0 g/dL) were associated with depression (P < 0.05). Among them, lower weekly renal Kt/Vurea was the only independent risk factor associated with depression (OR = 3.1, P = 0.007). Depressed patients showed significantly lower scores in every dimension of HRQOL (P < 0.001). Lower weekly renal Kt/Vurea (β = 0.24, P = 0.005) and lower nPNA (β = 0.15, P = 0.03) were the independent risk factors associated with lower kidney dialysis component summary, whereas lower plasma hemoglobin level was the consistent risk factor for lower physical component summary (β = 0.22, P = 0.03) and mental component summary (β = 0.22, P = 0.01). Depression is a prevalent psychological problem in PD population. Residual renal function is the most important factor associated with depression and impaired HRQOL in PD patients.
Keywords: Peritoneal Dialysis, Depression, Health-Related Quality of Life, Residual Renal Function, Beck's Depression Inventory, KDQOL-SF
INTRODUCTION
Depression is the most widely acknowledged psychological problem among end-stage renal disease (ESRD) patients (1, 2). About 28% of chronic kidney disease patients facing impending dialysis have major depression, and even larger proportions of dialysis patients suffer from depression (3). According to the previous studies, several modifiable risk factors such as anemia, poor nutritional status, and high peritonitis rates were reported to be associated with depression (4).
Depression is a serious problem in ESRD patients not only because it is prevalent but also because it is associated with decreased health-related quality of life (HRQOL). Since both patient's survival rate and technical survival rate have been improved over decades, quality of remaining life in peritoneal dialysis (PD) patients became an important issue more than ever. In addition, decreased HRQOL per se is related to higher mortality and hospitalization rate (5). Therefore, defining contributing factors to depression and HRQOL is crucial to properly manage them to improve dialysis outcomes in PD patients.
In Korea, PD population has been steadily increased for several years. According to the nation-wide ESRD Registry data from Korean Society of Nephrology, approximately 20% of dialysis population maintains PD, and about 1,000-2,000 patients start PD every year (6). One of the important factor influencing chronic kidney disease patients to favor PD on hemodialysis (HD) is that it is known to be better for preserving residual renal function (RRF) (7, 8). However, the effect of RRF and depression or HRQOL has not been elucidated well in previous studies. This is a single-center, cross-sectional study designed to evaluate depression and HRQOL among maintenance PD patients and to define contributing factors including RRF.
MATERIALS AND METHODS
Subjects
Total of one hundred and nine maintenance PD patients aged over 18 yr from Seoul National University Hospital were screened. Four patients refused to enroll, and total of 105 patients were enrolled in the study from October 2008 until December 2008. They were diagnosed with ESRD and had been on PD for more than 6 months. The trained clinical research coordinator (CRC) read and filled out the questionnaires for the patients with reading and writing difficulties.
Data collection
Demographic and laboratory data were obtained from medical records. Age, gender, marital status, causes of ESRD, duration of dialysis, education level, and religious status were reviewed in all patients. The information on job status - employed or unemployed- was also collected. The causes of ESRD were categorized into diabetes mellitus, glomerulonephritis, hypertension, others, and unknown cause. Patients were classified into two groups according to their maximum education level: Up to high school graduate or beyond college graduate. Plasma hemoglobin (Hb), serum albumin, serum cholesterol, blood urea nitrogen (BUN), creatinine, C-reactive protein (CRP), and weekly Kt/Vurea (total, renal, and peritoneal Kt/Vurea) were reviewed from laboratory reports. The Kt/Vurea is a dimensionless index that measures fractional urea clearance, which comprises a peritoneal and a residual renal component. In the analysis, patients were classified as low Hb (< 10.0 g/dL) vs high Hb (≥ 10.0 g/dL) group. Low albumin level was defined as serum albumin ≤ 4.0 g/dL and high CRP was defined as CRP ≥ 0.5 mg/dL. Plasma Hb, serum albumin and normalized protein equivalent of nitrogen appearance (nPNA) were checked for nutritional indices. The CRP was measured as an inflammatory marker. The funding organization had no role in the study design, data collection, data analysis, data interpretation, or writing the manuscript.
Survey instruments
The Modified Charlson comorbidity Index (MCCI) was used to quantify the severity of comorbidity. The MCCI has been commonly employed in the studies with ESRD patients and especially validated in the studies of HRQOL (9). The patients were grouped based on the MCCI scores as low (< 5) and high (≥ 6) comorbidity groups (10).
The Korean version of Beck's Depression Inventory (BDI) was used to evaluate depression in our patients. The BDI has been validated in various groups of patients and has been used in dialysis patients to evaluate depression (1). The BDI consisted of 21 self-reported items and each item is rated on the scale of 0-3, producing possible score range from 0 to 63 (0 to 4; no depression, 5 to 9; mild to moderate depression, 10 to 18; moderate to severe depression, 19 to 29; and severe depression, 30 to 63) (11). We set up a cut-off value of 19 to include patients with moderate to severe depression.
KDQOL-SF™ has been used to evaluate HRQOL of ESRD patients (12), and recently, Park et al. translated and validated the Korean version of KDQOL-SF™ (13). It takes less than 20 min to complete the questionnaire, which consists of a generic core of 36 items supplemented with 43 kidney-disease targeted items and one overall health rating item. The detailed explanation about the composition of KDQOL-SF™ is shown in our previous study (14). We used the Korean version of KDQOL-SF™ to measure HRQOL in maintenance PD patients. Instruments and scoring programs of KDQOL-SF™ can be found at http://www.gim.med.ucla.edu/kdqol/downloads/download.html.
Statistical analysis
Data were analyzed using SPSS 16.0 for Windows (SPSS Inc., Chicago, IL, USA). We used frequency analysis to evaluate the prevalence of depression. The Fisher's exact test was used to evaluate risk factors for depression including demographic and laboratory variables and to compare HRQOL scores between depressed and non-depressed patients. Then, we performed multiple logistic regression analysis to define independent risk factors for depression. The linear regression analysis was used to show the relationship between BDI score and each component score of KDQOL-SF™. We also used linear regression analysis to define variables associated with each component summary score of KDQOL-SF™. Then, we performed multiple linear regression analysis to define independent risk factors associated with impaired HRQOL. The results were given as mean ± SD and P < 0.05 was considered to be statistically significant.
Ethics statement
The institutional review board of Seoul National University Hospital approved the research protocol in September 2008 (IRB No. H-0807-053-251). All subjects gave written informed consent before study enrollment.
RESULTS
Baseline characteristics
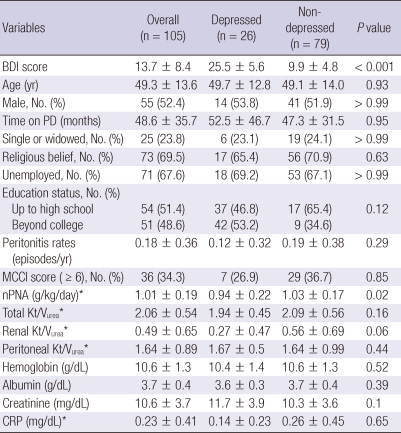
Table 1 shows baseline demographic characteristics of the subjects. Total 105 patients were included in the study. The mean age was 49 yr and male was slightly dominant (52.4%). The average duration of PD was 48.6 ± 35.7 months. Eighty-six patients (81.9%) were on continuous ambulatory peritoneal dialysis (CAPD) modality, ten patients (9.5%) on automated peritoneal dialysis (APD) method, and another 9 patients (8.6%) were on intermittent peritoneal dialysis (IPD) method. Most patients were married (76.2%) and about two-thirds of patients had religious belief. Only 34 subjects (32.4%) were employed at the time of study. Thirty-eight (36.2%) patients experienced ≥ 1 episodes of peritonitis during their dialysis period, and 15 of them had ≥ 2 episodes of peritonitis. The average peritonitis rate was 0.18 ± 0.36 episodes/year. Diabetes mellitus (32.4%) was the most common cause of ESRD, followed by glomerulonephritis (29.5%) and hypertension (3.8%). Among 101 patients with available weekly Kt/Vurea data, total (peritoneal + renal) Kt/Vurea and renal Kt/Vurea were 2.06 ± 0.54 and 0.49 ± 0.65, respectively.
Table 1.
Baseline characteristics of study population
*Data were analyzed without missing data and extreme values. BDI, Beck's Depression Inventory; MCCI, Modified Charlson's Comorbidity Index; nPNA, normalized protein equivalent of nitrogen appearance; CRP, C-reactive protein.
Prevalence of depression in PD patients
The mean BDI score was 13.7 ± 8.4 in our patients. Twenty-six of 105 (24.8%) patients had moderate to severe depression with a cut-off value of 19. When we set up a cut-off value to 10 to detect mild to severe depression, the prevalence of depression increased to the value of 66.7% (70 of 105 patients). The mean BDI score of depressive patients was 25.5 ± 5.6, which was significantly higher than that of non-depressed patients (9.9 ± 4.8, P < 0.001, Table 1).
Residual renal function as an independent risk factor for depression
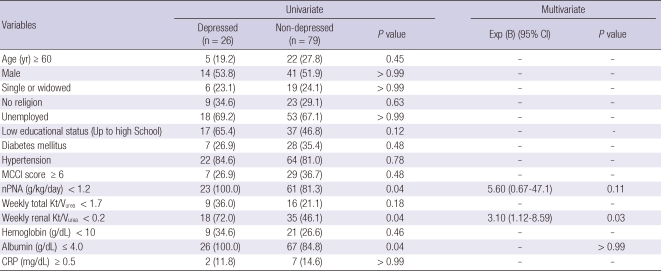
We evaluated demographic and clinical variables that were associated with depression (Table 2). In univariate analysis, lower weekly renal Kt/Vurea (< 0.2), lower nPNA (< 1.2 g/kg/day) and lower serum albumin level (≤ 4.0 g/dL) were associated with depression (P < 0.05). However, neither weekly total Kt/Vurea nor peritoneal Kt/Vurea was associated with depression. Demographic variables including age, gender, marital status, religious status, work status and education level did not show significant association with depression. Neither peritonitis rate nor CRP level was associated with depression. When we performed multivariate logistic regression analysis, lower renal Kt/Vurea (< 0.2) was the only independent risk factor associated with depression (OR = 3.1, 95% CI [1.12-8.59], P = 0.03).
Table 2.
Variables associated with Beck's Depression Inventory score
MCCI, Modified Charlson's Comorbidity Index; nPNA, normalized protein equivalent of nitrogen appearance; CRP, C-reactive protein.
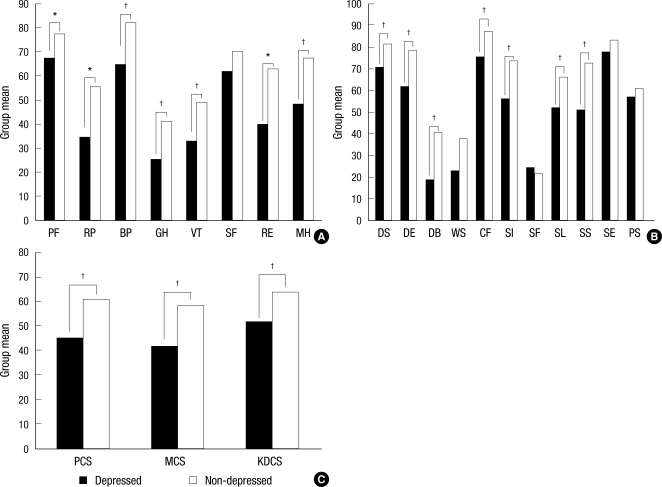
Impaired HRQOL in depressed patients
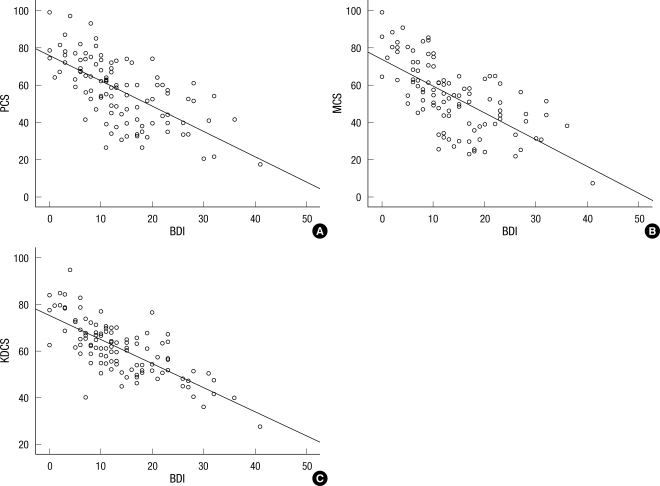
Each component summary of KDQOL: physical component summary (PCS), mental component summary (MCS), kidney dialysis component summary (KDCS) and subscales were evaluated and compared between depressed and non-depressed groups (Fig. 1). Among SF-36 domains, depressed patients showed significantly lower scores in physical function (PF), role physical (RP), bodily pain (BP), general health (GH), vitality (VT), role emotional (RE) and mental health (MH) domains (P < 0.05). All subscales of PCS showed significant difference between groups. Among disease-specific KDCS domains, depressed patients showed significantly lower scores in symptom/problem (DS), effects of kidney disease (DE), burden of kidney disease (DB), cognitive function (CF), quality of social interaction (SI), sleep (SL) and social support (SS) domains (P < 0.05). However, scores related to patient satisfaction domains (staff encouragement [SE] and patients satisfaction [PS]) were not different between groups. The mean ± SD for PCS, MCS, and KDCS in depressed group were lower compared to those in non-depressed group (45.2 ± 14.1 vs 61.2 ± 16.8, 41.8 ± 14.2 vs 58.3 ± 17.5 and 51.7 ± 10.8 vs 64.1 ± 10.5, respectively, P < 0.001). When we performed linear regression analysis, the BDI score was negatively correlated with each component summary score and its association was statistically significant (P < 0.001, Fig. 2).
Fig. 1.
Comparison of KDQOL-SF™ scores between depressed and non-depressed patients. *P < 0.05; †P < 0.01. (A) SF-36 domain scores (PF, Physical function; RP, Role physical; BP, Bodily pain; GH, General health; VT, Vitality; SF, Social function; RE, Role Emotional; MH, Mental health). (B) Disease-specific domain scores (DS, Symptom problem; DE, Effects of kidney disease; DB, Burden of kidney disease; WS, Work status; CF, Cognitive function; SI, Quality of social interaction; SF, Sexual function; SL, Sleep; SS, Social support; SE, Staff encouragement; PS, Patient satisfaction). (C) Composite summary scores (physical component summary [PCS], mental component summary [MCS], and kidney disease component summary [KDCS]).
Fig. 2.
Relationship between Beck's Depression Index (BDI) score and each component summary score of KDQOL-SF™. (A) Physical component summary (PCS) and BDI scores (r2 = 0.42, P < 0.001). (B) Mental component summary (MCS) and BDI scores (r2 = 0.435, P < 0.001). (C) Kidney disease component summary (KDCS) and BDI scores (r2 = 0.536, P < 0.001).
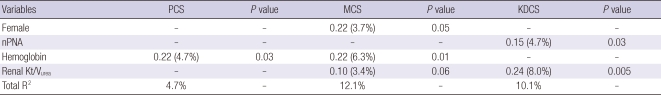
Residual renal function as an independent risk factor for impaired HRQOL
We evaluated the relationship between clinical variables and each component summary of KDQOL: PCS, MCS, and KDCS (Table 3). In univariate analysis, the nPNA level (β = 0.15, P = 0.03) and weekly renal Kt/Vurea (β = 0.24, P = 0.005) were closely related to KDCS, whereas plasma Hb was associated with both PCS (β = 0.22, P = 0.03) and MCS (β = 0.22, P = 0.01). Female patients were more likely to have better quality of life in MCS dimension than male patients with marginal statistical significance (β = 0.22, P = 0.05). Patients with lower weekly renal Kt/Vurea showed lower MCS score with marginal statistical significance (β = 0.10, P = 0.06). When we performed multiple linear regression analysis, weekly renal Kt/Vurea was the only independent risk factor associated with KDCS (β = 0.24, P = 0.02). On the other hand, weekly peritoneal Kt/Vurea, which reflects peritoneal solute removal, did not correlate with any of HRQOL dimensions. Plasma Hb was the independent risk factor for both PCS (β = 0.22, P = 0.03) and MCS (β = 0.26, P = 0.01), whereas female gender was another independent risk factor for HRQOL in MCS dimension (β = 0.22, P = 0.03).
Table 3.
Regression models to explain variables associated with each component summary score of KDQOL-SF™ [as Standardized Regression Coefficient β (Partial R2) and Total R2]*
*β denotes the relative importance of the explaining variable: the higher the β coefficient, the higher the contribution of that variable in the regression equation. Partial R2 symbolizes the explained variance of the dependent variable accounted for by the variable. Total R2 is the percentage of the total variation of the HRQOL score that is explained by the independent risk factors together. PCS, Physical Component Summary; MCS, Mental Component Summary; KDCS, Kidney Dialysis Component Summary; nPNA, normalized protein equivalent of nitrogen appearance.
DISCUSSION
In this single-center, cross-sectional study, we evaluated the prevalence of depression among maintenance PD patients and revealed associated factors with depression and HRQOL. Among our patients, 26 (24.8%) patients showed moderate to severe depression. Lower weekly renal Kt/Vurea and the nutritional indices were closely related to depression and HRQOL. Among them, lower RRF was the independent risk factor for depression and impaired HRQOL in our PD patients.
Depression and associated factors have been studied widely among dialysis patients. However, very few have been focused on the depression in PD population. In our study, about one-fourth of patients were found to have depression defined by BDI score over 19. This is slightly less than the prevalence of depression in maintenance HD patients in our previous study (51 of 160 subjects, 31.9%) (14). The exact comparison is beyond our scope because they were not analyzed at the same time with proper adjustment. However, some remarks can be made on the present analysis. At first, previous studies showed that patients on PD were more likely to preserve RRF than HD population (7, 15). According to our study, depressed patients showed lower RRF. Therefore, RRF must have some implication in the prevalence of depression according to dialysis modality. Further research should be done to reveal their association. Second, we clinically evaluated depression using the cut-off value of BDI score 19, and therefore, we might not have precisely diagnosed 'pathologic' depression. According to the previous study, however, cut-off scores ranging from ≥ 14 to 16 compare well with diagnostic assessments of depression in dialysis patients (16). Therefore, although our BDI criteria may have underestimated the prevalence of depression, those who were detected as 'depressed' are a high-risk group of patients who need an active management.
Depression can affect medical outcomes through a variety of mechanism. It can alter patient's ability to utilize medical care or change the behavior (17). Depression also increases hospitalization and mortality rates (18-20). One interesting study examined the effect of sertraline hydrochloride, an anti-depressant, in PD patients with clinical depression (21). After 12-week of treatment period, sertraline hydrochloride not only improved BDI score but also improved HRQOL and symptoms related to depression among PD patients. Therefore, the diagnosis and treatment of clinical depression in chronic PD patients are enormously important to improve their HRQOL. In our practice, however, referral to the psychiatric department is rarely done because either patients deny their depressed mood or refuse to visit psychiatry office or few practitioners have an interest in patients' mood. If we appropriately treat these patients with medication, it is more likely to improve their HRQOL and medical outcome.
This is the first study in Korea to demonstrate that RRF and nutritional status are important factors for depression and HRQOL in PD patients. In the previous study, Kim et al. analyzed depression in PD patient for the first time in Korea (22). They used Korean Center for Epidemiologic Studies Depression (CES-D) to evaluate depression. However, the prevalence of depression in their study was 75%, which is too much higher than the value (20%-30%) reported in many other studies (1, 23). In addition, they focused on the psychosocial issue such as stress and sense of hopelessness as risk factors for depression. They did not include either RRF or nPNA as potential variables. Since the number of incident PD patients is increasing every year and the average life span of dialysis patients has increased, we think our study is valuable because we emphasized the impact of depressive mood on HRQOL and evaluated its related factors.
In our study, lower weekly renal Kt/Vurea was the independent risk factor for depression and impaired HRQOL in PD patients. To the best of our knowledge, there is no study performed on the relationship between depression and RRF in PD population. One study compared weekly total Kt/Vurea between depressed and non-depressed patients and showed there was no statistically significant difference between groups (n = 43 vs n = 38, 1.8 ± 0.1 vs 1.9 ± 0.1, P > 0.05) (24). However, current concept of dialysis adequacy has been changed since a number of studies showed that RRF is more important than peritoneal clearance in the prognosis of PD patients (25, 26). Therefore, the result of our study implicates that preservation of renal function is important to decrease depressive symptoms other than increasing the dialysis dose. Meanwhile, the preservation of RRF has been suggested to improve HRQOL in both hemodialysis and peritoneal dialysis patients. In the CHOICE study, Shafi et al. demonstrated that preserved residual urine output was associated with better survival and QOL, lower inflammation and less erythropoietin use in hemodialysis patients (27). In addition, Termorshuizen et al. demonstrated in their 2-yr prospective study that RRF was more important than peritoneal clearance for PD patient survival and HRQOL (25). They used residual glomerular filtration rate (rGFR) to show RRF as an important determinant of HRQOL. However, when they repeated the same analysis with weekly renal Kt/Vurea instead of rGFR, the beneficial effect was restricted to the bodily pain and sleep disorder dimension. In our study, weekly renal Kt/Vurea was an independent risk factor for KDCS, not PCS or MCS dimension. Further large-scale, prospective studies are warranted to demonstrate the effect of RRF preservation on the maintenance or improvement of HRQOL in PD patients.
On the other hands, nutritional indices including nPNA, serum albumin, and plasma Hb were also demonstrated as important factors associated with depression and HRQOL. Nutritional status, usually evaluated by the Subjective Global Assessment and serum albumin, has been reported to be closely associated with depression and HRQOL (28-30). Recently published data showed that depression can cause a chronic inflammatory state in the body system, which can increase the cardiovascular risk and mortality in dialysis patients. They suggested that depression may be related to a high mortality rate and it should be understood in the context of the malnutrition-inflammation-atherosclerosis (MIA) syndrome (24). Our study result is in the concordance with the previous study results. However, we could not demonstrate the relationship with depression and inflammatory marker such as CRP level. We assume that it may be related to the small sample size. Only 65 patients were included with available CRP data. Besides, most of our patients showed normal range of CRP level (0.23 ± 0.41 mg/dL). Future study is needed to disclose mechanism underlying the MIA syndrome and depression.
There are some limitations to our study. At first, this is a single-center, observational study with a small-size population. The result of our study should be confirmed in the large-scale, multi-center study in the future. Second, the result may be biased because not all the PD patients in our center were enrolled in our study. Those who refused to enroll in the study could have more depressive symptoms that prevented them from actively engage in the study. At last, there were many missing data, especially for nPNA and CRP, which must have led to the biased results. Although there are some limitation in the study design and patient enrollment, this study is invaluable to reveal RRF as an important determinant of HRQOL in PD patients.
In conclusion, depression is the prevalent psychological problem among maintenance PD patients. Lower RRF is an independent risk factor associated with depression and HRQOL in PD patients. The clinicians should be aware of clinical importance of RRF in the management of PD patients.
ACKNOWLEDGMENTS
The authors would like to appreciate Professor Sehyun Kim at Graduate School of East West Medical Science, Kyung Hee University and Hye Ja Park, RN, PhD at CHA University for permission to use the Korean version of KDQOL-SFTM 1.3. We also would like to express heartfelt thanks to Bong-Jin Hahm, MD, PhD at the Department of Psychiatry, Seoul National University College of Medicine for his clinical guidance and help in assessment of depression and HRQOL in our patients.
Footnotes
This study was supported by a grant from Fresenius Medical Care Korea Ltd (06-2008-36).
References
- 1.Finkelstein FO, Finkelstein SH. Depression in chronic dialysis patients: assessment and treatment. Nephrol Dial Transplant. 2000;15:1911–1913. doi: 10.1093/ndt/15.12.1911. [DOI] [PubMed] [Google Scholar]
- 2.Kimmel PL. Psychosocial factors in dialysis patients. Kidney Int. 2001;59:1599–1613. doi: 10.1046/j.1523-1755.2001.0590041599.x. [DOI] [PubMed] [Google Scholar]
- 3.Sumanathissa M, De Silva VA, Hanwella R. Prevalence of major depressive episode among patients with pre-dialysis chronic kidney disease. Int J Psychiatry Med. 2011;41:47–56. doi: 10.2190/PM.41.1.e. [DOI] [PubMed] [Google Scholar]
- 4.Lew SQ, Piraino B. Quality of life and psychological issues in peritoneal dialysis patients. Semin Dial. 2005;18:119–123. doi: 10.1111/j.1525-139X.2005.18215.x. [DOI] [PubMed] [Google Scholar]
- 5.Paniagua R, Amato D, Vonesh E, Guo A, Mujais S Mesican Nephrology Collaborative Study Group. Health-related quality of life predicts outcomes but is not affected by peritoneal clearance: the ADEMEX trial. Kidney Int. 2005;67:1093–1104. doi: 10.1111/j.1523-1755.2005.00175.x. [DOI] [PubMed] [Google Scholar]
- 6.Korean Society of Nephrology; ESRD Registry committee. Renal replacement therapy in Korea: insan memorial dialysis registry 2005. Korean J Nephrol. 2006;25:S425–S457. [Google Scholar]
- 7.Lysaght MJ, Vonesh EF, Gotch F, Ibels L, Keen M, Lindholm B, Nolph KD, Pollock CA, Prowant B, Farrell PC. The influence of dialysis treatment modality on the decline of remaining renal function. ASAIO Trans. 1991;37:598–604. [PubMed] [Google Scholar]
- 8.Hiroshige K, Yuu K, Soejima M, Takasugi M, Kuroiwa A. Rapid decline of residual renal function in patients on automated peritoneal dialysis. Perit Dial Int. 1996;16:307–315. [PubMed] [Google Scholar]
- 9.Van Manen JG, Korevaar JC, Dekker FW, Boeschoten EW, Bossuyt PM, Krediet RT NECOSAD-Study. Adjustment for comorbidity in studies on health status in ESRD patients: which comorbidity index to use? J Am Soc Nephrol. 2003;14:478–485. doi: 10.1097/01.asn.0000043902.30577.c9. [DOI] [PubMed] [Google Scholar]
- 10.Beddhu S, Bruns FJ, Saul M, Seddon P, Zeidel ML. A simple comorbidity scale predicts clinical outcomes and costs in dialysis patients. Am J Med. 2000;108:609–613. doi: 10.1016/s0002-9343(00)00371-5. [DOI] [PubMed] [Google Scholar]
- 11.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 12.Hays RD, Kallich JD, Mapes DL, Coons SJ, Carter WB. Development of the kidney disease quality of life (KDQOL) instrument. Qual Life Res. 1994;3:329–338. doi: 10.1007/BF00451725. [DOI] [PubMed] [Google Scholar]
- 13.Park HJ, Kim S, Yong JS, Han SS, Yang DH, Meguro M, Han CW, Kohzuki M. Reliability and validity of the Korean version of Kidney Disease Quality of Life instrument (KDQOL-SF) Tohoku J Exp Med. 2007;211:321–329. doi: 10.1620/tjem.211.321. [DOI] [PubMed] [Google Scholar]
- 14.Park HC, Yoon HB, Son MJ, Jung ES, Joo KW, Chin HJ, Oh KH, Lim CS, Kim YS, Ahn C, Han JS, Kim S, Hahm BJ, Oh YK. Depression and health-related quality of life in maintenance hemodialysis patients. Clin Nephrol. 2010;73:374–380. doi: 10.5414/cnp73374. [DOI] [PubMed] [Google Scholar]
- 15.Moist LM, Port FK, Orzol SM, Young EW, Ostbye T, Wolfe RA, Hulbert-Shearon T, Jones CA, Bloembergen WE. Predictors of loss of residual renal function among new dialysis patients. J Am Soc Nephrol. 2000;11:556–564. doi: 10.1681/ASN.V113556. [DOI] [PubMed] [Google Scholar]
- 16.Craven JL, Rodin GM, Johnson L, Kennedy SH. The diagnosis of major depression in renal dialysis patients. Psychosom Med. 1987;49:482–492. doi: 10.1097/00006842-198709000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Fine A. Compliance with CAPD prescription is good. Perit Dial Int. 1997;17:343–346. [PubMed] [Google Scholar]
- 18.Chilcot J, Davenport A, Wellsted D, Firth J, Farrington K. An association between depressive symptoms and survival in incident dialysis patients. Nephrol Dial Transplant. 2011;26:1628–1634. doi: 10.1093/ndt/gfq611. [DOI] [PubMed] [Google Scholar]
- 19.Lopes AA, Bragg J, Young E, Goodkin D, Mapes D, Combe C, Piera L, Held P, Gillespie B, Port FK Dialysis Outcomes and Practice Patterns Study. Depression as a predictor of mortality and hospitalization among hemodialysis patients in the United States and Europe. Kidney Int. 2002;62:199–207. doi: 10.1046/j.1523-1755.2002.00411.x. [DOI] [PubMed] [Google Scholar]
- 20.Hedayati SS, Bosworth HB, Briley LP, Sloane RJ, Pieper CF, Kimmel PL, Szczech LA. Death or hospitalization of patients on chronic hemodialysis is associated with a physician-based diagnosis of depression. Kidney Int. 2008;74:930–936. doi: 10.1038/ki.2008.311. [DOI] [PubMed] [Google Scholar]
- 21.Atalay H, Solak Y, Biyik M, Biyik Z, Yeksan M, Uguz F, Guney I, Tonbul HZ, Turk S. Sertraline treatment is associated with an improvement in depression and health-related quality of life in chronic peritoneal dialysis patients. Int Urol Nephrol. 2010;42:527–536. doi: 10.1007/s11255-009-9686-y. [DOI] [PubMed] [Google Scholar]
- 22.Kim JA, Lee YK, Huh WS, Kim YG, Kim DJ, Oh HY, Kang SA, Kim Moon, Kim HW, Kim JH. Analysis of depression in continuous ambulatory peritoneal dialysis patients. J Korean Med Sci. 2002;17:790–794. doi: 10.3346/jkms.2002.17.6.790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cukor D, Peterson RA, Cohen SD, Kimmel PL. Depression in end-stage renal disease hemodialysis patients. Nat Clin Pract Nephrol. 2006;2:678–687. doi: 10.1038/ncpneph0359. [DOI] [PubMed] [Google Scholar]
- 24.Ko GJ, Kim MG, Yu YM, Jo SK, Cho WY, Kim HK. Association between depression symptoms with inflammation and cardiovascular risk factors in patients undergoing peritoneal dialysis. Nephron Clin Pract. 2010;116:c29–c35. doi: 10.1159/000314548. [DOI] [PubMed] [Google Scholar]
- 25.Termorshuizen F, Korevaar JC, Dekker FW, van Manen JG, Boeschoten EW, Krediet RT NECOSAD Study Group. The relative importance of residual renal function compared with peritoneal clearance for patient survival and quality of life: an analysis of the Netherlands Cooperative Study on the Adequacy of Dialysis (NECOSAD)-2. Am J Kidney Dis. 2003;41:1293–1302. doi: 10.1016/s0272-6386(03)00362-7. [DOI] [PubMed] [Google Scholar]
- 26.Maiorca R, Brunori G, Zubani R, Cancarini GC, Manili L, Camerini C, Movilli E, Pola A, d'Avolio G, Gelatti U. Predictive value of dialysis adequacy and nutritional indices for mortality and morbidity in CAPD and HD patients. A longitudinal study. Nephrol Dial Transplant. 1995;10:2295–2305. doi: 10.1093/ndt/10.12.2295. [DOI] [PubMed] [Google Scholar]
- 27.Shafi T, Jaar BG, Plantinga LC, Fink NE, Sadler JH, Parekh RS, Powe NR, Coresh J. Association of residual urine output with mortality, quality of life, and inflammation in incident hemodialysis patients: the Choices for Healthy Outcomes in Caring for End-Stage Renal Disease (CHOICE) Study. Am J Kidney Dis. 2010;56:348–358. doi: 10.1053/j.ajkd.2010.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bakewell AB, Higgins RM, Edmunds ME. Quality of life in peritoneal dialysis patients: decline over time and association with clinical outcomes. Kidney Int. 2002;61:239–248. doi: 10.1046/j.1523-1755.2002.00096.x. [DOI] [PubMed] [Google Scholar]
- 29.Manns B, Johnson JA, Taub K, Mortis G, Ghali WA, Donaldson C. Quality of life in patients treated with hemodialysis or peritoneal dialysis: what are the important determinants? Clin Nephrol. 2003;60:341–351. doi: 10.5414/cnp60341. [DOI] [PubMed] [Google Scholar]
- 30.Merkus MP, Jager KJ, Dekker FW, Boeschoten EW, Stevens P, Krediet RT The Necosad Study Group. Quality of life in patients on chronic dialysis: self-assessment 3 months after the start of treatment. Am J Kidney Dis. 1997;29:584–592. doi: 10.1016/s0272-6386(97)90342-5. [DOI] [PubMed] [Google Scholar]