Abstract
Objective This article presents a summary of findings from asthma studies focusing on immigration and acculturation-related factors. A study examining associations between these processes, family cohesion and social support networks, and asthma morbidity in a sample of Dominican and Puerto Rican caregivers residing in the mainland U.S., is also described. Methods Latino children with asthma (n = 232), ages 7–16 (49% female) and their caregivers completed interview-based questionnaires on immigration and acculturation-related processes, family characteristics, and asthma morbidity. Results The frequency of ED use due to asthma may be higher for children of caregivers born in Puerto Rico. Acculturative stress levels were higher for Puerto Rican born caregivers residing in the mainland U.S. Conclusion Asthma-related educational and intervention programs for Latino children and families should be tailored to consider the effects that the immigration and acculturation experience can have on asthma management. Specific family-based supports focused on decreasing stress related to the acculturation process, and increasing social and family support around the asthma treatment process may help to reduce asthma morbidity in Latino children.
Keywords: acculturation, asthma morbidity, immigration
Introduction
Pediatric Asthma Disparities: A Focus on Immigration-Related Factors
Pediatric asthma disparities in the United States are apparent. African American and Latino children are disproportionately affected by asthma, with greater disease prevalence and morbidity compared to their non-Latino White counterparts. Puerto Rican (PR) children who live on the mainland U.S. are particularly at risk, evidencing higher asthma prevalence and worse morbidity than children from any other Latino ethnic subgroup and children from African American and non-Latino White (NLW) backgrounds (Burchard et al., 2004; Lara, Akinbami, Flores, & Morgenstern, 2006). Children of Dominican descent also fare poorly in terms of asthma outcomes (Centers for Disease Control, 2005). Place of residence impacts asthma risk. Island PR children have higher lifetime asthma prevalence than PR children residing in the mainland U.S. (Cohen et al., 2007; Hunninghake, Weiss, & Celedón, 2006).
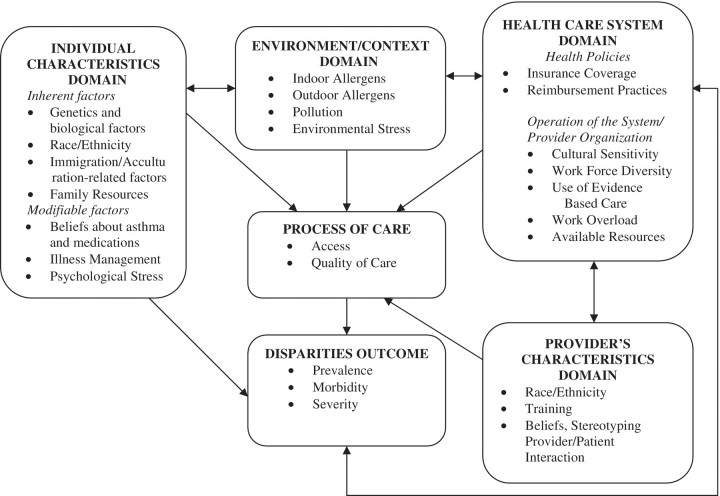
Asthma health disparities between Latino and NLW children appear to be multi-determined. A conceptual and empirically derived framework (Canino et al., 2006; Fig. 1) has been developed for understanding pediatric asthma disparities (in asthma prevalence, severity, and morbidity) as a result of a complex interaction of factors related to four main domains: the individual and family (e.g., genetics; Burchard et al., 2004; beliefs about controller medication use; McQuaid et al., 2009), the environment in which the child lives (e.g., exposure to allergens and irritants; Kattan et al., 2005; neighborhood stress; Koinis-Mitchell et al., 2007), the health-care system (e.g., insurance overage, consistent health care provider; Ortega et al., 2003), and provider characteristics (e.g., provider–patient interaction; Yoos et al., 2005).
Figure 1.
Conceptual framework of pediatric asthma health disparities. Reproduced from Canino et al. (2006). Asthma disparities in the prevalence, morbidity, and treatment of Latino children. Social Science and Medicine, 63, 2926–2937. Elsevier Limited.
Latinos are the largest U.S. ethnic minority group, totaling 12.6% of the population (U.S. Census Bureau, 2004). Little is understood about how processes related to immigration and acculturation affect asthma outcomes in Latino children. Latino families who immigrate to the mainland U.S. come from different geographical areas, and each area has its own unique relationship to the United States. For example, PR is a U.S. territory, although not an official state, whereas the Dominican Republic (DR) is a separate country. Families emigrate from their country of origin for a variety of historical, economic, political, and/or personal reasons, which may influence the timing of the immigration and the acculturation process. A family's immigration and acculturation experience may affect how they manage chronic illnesses such as asthma. For example, immigrant families may have varying levels of comfort and familiarity with the health care system process in the mainland, which may affect treatment behaviors.
In this article, we summarize assessment procedures and findings from pediatric asthma studies that examine Latino immigration and acculturation-related factors to determine their impact on asthma morbidity outcomes and to provide future directions for research. We then describe results from a study of Latino caregivers of children with asthma who currently reside in Rhode Island (RI), focusing on associations among immigration and acculturation-related factors, family characteristics relevant to the immigration experience (e.g., level of family cohesion), and asthma morbidity. We also discuss implications for future research based on our study findings. Immigration and acculturation-related processes are viewed as belonging within the individual domain of our health disparities model (Fig. 1), as these factors are associated with one's cultural background and family experience. Our review of results provides an empirical rationale for considering these important contributors to Latino children's asthma outcomes.
It is necessary to define immigration and acculturation, as these terms are not always used consistently (Alegria, Mulvaney-Day et al., 2007; Hunt, Schneider, & Comer, 2004). Immigration is the geographic mobility of individuals from one country to another (Alegria, Mulvaney-Day, et al., 2007; Alegria, Shrout et al., 2007). “Immigrants” are individuals who have moved from their country of origin to another country within their lifetime. Note that for PRs, who move from PR to the United States, this mobility is referred to as migration, because PR is a U.S. territory and PRs are U.S. citizens. “Immigration-related factors” (which in this article will include migration) can include place of birth (nativity), age of entry into the host country, and years residing in the host country.
Immigration factors can affect the process of adaptation to the host culture, a process referred to as acculturation. The extent to which immigrants acculturate may depend on differences in cultural characteristics between the country of origin and the host country. Acculturation can be defined as the change in one's norms, values, ideas, and behaviors that result from direct and continuous contact with a different culture (Duarte et al., 2008; Lara, Gamboa, Kahramanian, Morales, & Bautista, 2005). Acculturative stress refers to the distress that can develop during and as a result of the process of acculturation (Duarte et al., 2008).
Asthma Studies Examining Immigration and Acculturation-Related Factors
Immigration-related factors examined in the asthma literature include child and caregiver nativity (i.e., country of birth), and the amount of time the caregiver and/or child has resided in the United States. Preferred language is an example of an acculturation-related factor commonly assessed (Martin et al., 2007). In some cases, researchers (e.g., Martin et al., 2007) have simultaneously examined two or more of these factors (e.g., caregiver nativity and preferred language) as a measurement of “acculturation”.
Child and Caregiver Nativity
Among Mexican children, birth in Mexico is associated with a decreased probability for the development of asthma (Eldeirawi & Persky, 2007; Lara et al., 2006). In contrast, Among PR children residing in the Mainland U.S., asthma prevalence was higher for Island-born PR children with Island born-PR caregivers than for U.S.-Mainland born children with U.S.-Mainland born PR caregivers (Lara et al., 2006; Cohen et al., 2007).
Less research has focused on the role of caregiver birthplace in relation to pediatric asthma morbidity. Klinnert, Price, Liu, and Robinson (2003) compared asthma morbidity among Latino infants with U.S.-born and foreign-born caregivers primarily of Mexican origin. Although foreign-born Latino caregivers reported less illness severity in their children, their infants had higher numbers of ED visits than infants of U.S.-born Latino, NLW, or African American caregivers. Acclimating to a different health context may affect awareness of health care options and health care utilization in this sample.
Duration and Timing of U.S. Residence
The length of time children have lived in the United States and timing of U.S. residence during development may impact asthma risk. Among a sample of Mexican-American children living in the United States, children who had lived in the United States during their first year of life had a 2.39-fold increased risk of having asthma compared to children who had lived in Mexico during their first year of life (Eldeirawi & Persky, 2007). The potential protective effect of birth or residence in Mexico among Mexican-American children may diminish after extended residence in the United States, with increased risk of asthma after living 10 or more years in the United States (Eldeirawi & Persky, 2007). It is also possible that U.S.-born children may be more likely to see physicians during early life, which contributes to an asthma diagnosis bias for these children.
Acculturation
Other studies have referred to the immigration and acculturation process in various ways. Martin and colleagues (2007) measured Mexican American caregivers’ acculturation as a combination of caregiver nativity, the length of time of U.S. residence, and language preference. Lower caregiver acculturation was associated with less asthma prevalence in children. Although children of Mexico-born caregivers had lower asthma prevalence than children of U.S.-born caregivers, asthma rates among children of immigrants did not increase with increasing caregiver time spent in the United States. It is not clear how early environmental exposure and families’ support systems in the United States influenced these results. Klinnert and colleagues (Klinnert, Price, Liu, & Robinson, 2002) measured acculturation as caregiver nativity and language preference in a sample of predominately Mexican-American infants who lived in the United States. Infants with fewer biological asthma risks (e.g., caregiver asthma status) were more likely to have foreign-born caregivers who spoke Spanish. Overall, inconsistencies in the results across studies may be due, in part, to differences in how immigration and acculturation-related processes were defined and assessed.
Family Characteristics Also Matter
Family characteristics also may affect families’ immigration and acculturation experiences, and asthma morbidity. The level of social support families receive during and after immigration may minimize the potential feelings of isolation during the acculturation process (e.g., Alegria, Mulvaney-Day et al., 2007). Given the family plays an integral role in asthma management (McQuaid, Walders, Kopel, Fritz, & Klinnert, 2005), strong family ties and connections may help to alleviate stress associated with managing asthma when adapting to a new geographical location. Because of the centrality of the family in the Latino culture, family characteristics may be important in promoting positive psychosocial outcomes for Latino children growing up under conditions of adversity (Leidy, Guerra, & Toro, 2010). Within the Latino culture, “familismo” means placing the family before one's own personal needs (Sarkisian, Gerena, & Gerstel, 2006). Building on the concept of interconnectedness inherent in familismo, family cohesion has been associated with optimal psychosocial outcomes among Latino children (Tolan, Gorman-Smith, Huesmann, & Zelli, 1997). Studies have not investigated how family characteristics and the social support system may have a bearing on immigration factors and asthma outcomes among Latino families.
In summary, Latino families living in the United States have unique immigration and acculturation experiences that may affect their management of asthma and, subsequently, their child's asthma morbidity. For Mexican-American children, birth in their native county predicts better asthma outcomes relative to birth in the United States. For PR children, Island PR born children may be at greater risk for asthma compared to their counterparts born in mainland U.S. (Lara et al., 2006). In addition, length of residence in the United States and level of caregiver acculturation, are important to consider with regard to level of asthma risk (Martin et al., 2007).
Caribbean Latinos: Latino Ethnic Subgroups at Particular Risk?
There is a particular need to compare the immigration, acculturation, and asthma morbidity experiences of PR and Dominican children living in the mainland U.S., given that these children are at higher risk for poor asthma outcomes than children from other Latino subgroups, such as Mexicans (Lara et al., 2006). Both groups are Caribbean Latinos, with similar demographic profiles, yet PRs face fewer barriers to their mobility to the mainland U.S. and may be more highly acculturated due to their status as U.S. citizens and overall exposure to U.S. culture.
The Current Study
In the current study, we investigated immigration-related characteristics (e.g., caregiver nativity, caregiver country of upbringing) among a sample of Latino caregivers of Dominican or PR descent who have a child with asthma and currently reside in the mainland U.S. We assessed differences in children's level of asthma severity and morbidity (e.g., asthma-related functional limitation, ED visits due to asthma) in relation to these immigration-related factors. We expected that Latino children of DR and Island PR-born caregivers would have greater asthma severity and morbidity than Latino children of U.S.-mainland born caregivers. We further hypothesized that children of Island PR-born caregivers would have poorer asthma outcomes than their Dominican counterparts.
We also examined differences in levels of acculturative stress, and family characteristics/resources (e.g., family cohesion and involvement in social networks) based on caregiver immigration experiences. Given the increased frequency with which PR families travel back and forth to the mainland (Alegria et al., 2007) and previous evidence documenting the link between acculturative stress and ED use in this group (Koinis-Mitchell et al., 2007), we expect that PR born caregivers will experience higher levels of acculturative stress. Research examining family cohesion and social networks in children with asthma from these Latino subgroups has not been conducted to inform hypotheses concerning how these processes may differ based on caregivers’ immigration experiences, thus these questions are tested on an exploratory basis. Research including Latino children who are free of chronic illness has shown that family cohesion and social support has served as positive resources for Latino families exposed to increased levels of poverty (Leidy et al., 2010).
Finally, we examine the extent to which acculturative stress and family characteristics mediate the association between immigration and asthma morbidity. Consistent with a health disparities framework, a mediational approach is used as there is limited research identifying cultural and family-related explanatory mechanisms that underlie the association between immigration characteristics and morbidity in this group. These processes may serve as modifiable targets for family-based interventions focused on decreasing morbidity in Latino children with asthma (e.g., enhancing social support networks and asthma educational resources for newly immigrated families). In light of our conceptual model of asthma disparities in Latino children (Fig. 1; Canino et al., 2006), immigration-related processes and family characteristics may interact or exert a direct or indirect influence on the various other elements of the model to ultimately affect children's asthma outcomes (Canino et al., 2006). As a first step, we test these specific associations as one example of the many potential pathways of influence, whereby immigration-related factors and family/cultural characteristics can affect asthma outcomes.
Methods
Participants
Data for this study were collected as part of the Rhode Island–Puerto Rico Asthma Center (RIPRAC) project funded by the National Heart, Lung and Blood Institute (NHLBI) to examine factors contributing to asthma health disparities in Latino (Puerto Rican and Dominican) and NLW children from mainland RI and island PR. A detailed presentation of the RIPRAC study design and methods is presented elsewhere (see Canino et al., 2009). The examination of immigration-related factors and family characteristics from these data, which are the focus of the current study, have not been previously investigated.
The present study focused on the 232 Latino child participants living in RI and their primary caregivers (PCGs). One hundred and one (43.5%) families self-identified as PR and 131 (56.5%) as Dominican. Child participants had physician-diagnosed asthma that was confirmed by study physicians through physical examination, lung function testing, and medical history. Children were between the ages of 7-16 (M = 10.6 years; SD = 2.4 years) and 51% were male. Seventy-seven percent were born in the mainland U.S., 12% in Island PR, and 11% in the DR.
Design and Procedures
Participant recruitment in RI occurred at several locations including the hospital-based ambulatory pediatric clinics, community primary care clinics, hospital-based asthma educational programs, health fairs and other community events, and schools. Efforts were made to recruit Latino families from a wide range of income levels to prevent group differences based largely on socioeconomic status (SES). Including the Mainland Latino families, three hundred and ninety-two families (51% PR, 49% DR) in RI were deemed eligible to participate in the study. Eighty-one percent of eligible Mainland-PR families, and, 86% of eligible Mainland-DR families enrolled. The most common reasons for non-enrollment were lack of time and interest, or failure to attend the enrollment session. Thirty-four percent of PR enrollees did not complete all of the assessments required for inclusion in the current report, relative to 18% of DR families (chi square = 11.5, p < .01). Most non-completers cited lack of time or interest in continuing in the protocol, or they became unreachable. There were no differences between families that completed the protocol versus those that did not regarding child age, gender, asthma severity level, and family poverty level.
Children with asthma and their PCGs participated in interview-based assessments. Questionnaires were administered by trained research assistants to children and their PCGs separately, in the lab or in participants’ homes. Research assistants were fluent in both English and Spanish, and interviews were conducted in either language based on participant preference.
Questionnaires were translated and adapted from English to Spanish using multi-stage methods employed previously by the RIPRAC study's Puerto Rican investigators and their colleagues (Canino & Bravo, 1994; Matías-Carrelo et al., 2003).
Written caregiver consent and child assent were obtained. The Institutional Review Board of a hospital in Providence, RI approved this study. To facilitate a review of the medical record (for determining asthma severity level), PCGs completed a release of information form. Families received payment for study participation.
Measures
Poverty Threshold
Socioeconomic status was identified by calculating an income-to needs ratio for each family by dividing yearly family income for that family size by the poverty threshold for a family of that size (U.S. Department of Health and Human Services, 2005). A family was considered at or below the poverty line if the ratio was less than or equal to 1. By this criterion, 58.6% of the families were identified as living below the poverty threshold.
Immigration-Related Characteristics
Immigration characteristics examined in this study included caregiver nativity and the caregiver's country of upbringing, defined as the country in which the caregiver lived most of the time until age 16 (Alegria, Takeuchi, et al., 2004).
Asthma Severity
Asthma severity ratings were made by study clinicians who utilized a visual worksheet to classify severity based on three criteria: reported symptom frequency, pre-albuterol FEV1, and current controller medication dose. The worksheet, which was derived from the established Global Initiative for Asthma (Global Initiative for Asthma, 2002) and NAEPP guidelines, has been described in a separate paper (Esteban et al., 2009). Asthma severity was classified as “mild intermittent,” “mild persistent,” “moderate persistent,” and “severe persistent.” Of the entire sample of RI children, 83% were classified as experiencing persistent levels of asthma severity.
Asthma Morbidity
Two indexes of child asthma morbidity were used in this study, asthma-related functional limitation and number of ED visits due to asthma in the previous year. Functional limitation due to asthma was assessed via PCG report on the Asthma Functional Severity Scale (Rosier et al., 1994). The AFSS is comprised of 6 items that assess frequency of asthma episodes, frequency of symptoms between episodes, degree of impairment during an episode, and degree of impairment during the intervals between episodes. A functional morbidity index score is the mean across items for the past year, with higher scores indicating greater levels of impairment. The AFSS has demonstrated good to excellent validity in U.S. Latino, African American and NLW children with asthma (Koinis-Mitchell et al., 2007). Internal consistency of the AFSS has been good to excellent, with Cronbach's α's ranging from .72 to .92 in previous studies (Koinis-Mitchell et al., 2007; Rosier et al., 1994). Alpha reliability of the measure in the RIPRAC study was adequate for the 12-month recall version in English and Spanish (α = .74 and .72, respectively). The AFSS includes an item requesting the PCG to report on number of asthma-related visits the child had in the previous year since study participation. Number of ED visits was treated as a dichotomous variable (1 = “one or more ED visits” and 0 = “no ED visits”; Koinis-Mitchell et al., 2007).
Acculturation-Related Factor and Family Characteristics/Resources
Measures assessed the PCG's level of acculturative stress, family cohesion, and social support networks.
Acculturative Stress
The Cultural Stress Scale (CSS) is a 26-item subscale of the Hispanic Stress Inventory (Cervantes, Padilla, & Salgado de Snyder, 1991). The CSS evaluates stresses associated with acculturation, including immigration stress, family/culture stress, and occupational/economic stress in the previous 12 months. Items are rated on 3-point scale (0 = rarely/never, 1 = sometimes, 2 = often) with possible scores ranging from 0 to 52. Internal consistency estimates exist for English and Spanish versions of the scale. Previous research demonstrated internal consistency exceeding α = .78 (Cervantes et al., 1991). In the RIPRAC study, internal consistency was excellent for both English (Cronbach's α = .91) and Spanish (Cronbach's α = .84) versions of the instrument.
Family Cohesion
Family cohesion was assessed by PCG report on the 7-item Family Pride scale (Gil & Vega, 1996; Olson, 1986). This scale taps the value of familism, a value deeply rooted in Latino cultures (Gil & Vega, 1996). Respondents indicate on 4-point Likert scales their level of agreement with statements examining family cultural values such as trust, loyalty and a general orientation toward family. Total scores range from 7 to 28, with lower values representing greater family cohesion. The scale has been used extensively in research with Latino families (Gil & Vega, 1996). Internal consistency in previous research (α = .87–.91; Gil & Vega, 1996) and in the current study (α = .91, English and .92, Spanish) is excellent.
Social Networks
Two items from the National Latino and Asian American Study (NLAAS), a large population-based survey of Latinos and Asian Americans (Alegria, Takeuchi, et al., 2004; Alegria, Vila, et al., 2004) were used to assess contact with family and friends (e.g., “How often do you talk on the phone or get together with friends/relatives?”). Only two items from the original scale were used in RIPRAC to minimize subject burden while providing exploratory information about the role of social contacts in asthma management. A dichotomous variable was computed that represented the frequency of contact with friends/family. If responses to either or both single item indicates contact with friends/family “most every day” or “a few times a week,” the summary variable is coded 1. Less frequent contact was coded as 0. Internal consistency of these items was rather low (Cronbach's α = .38) in this sample, however the scale was retained for exploratory purposes.
Data Analysis Plan
Associations among demographic, asthma severity, acculturation, immigration, family, and morbidity variables were examined using Pearson's correlations or analyses of variance (ANOVA). Chi-squared analyses were used to test for differences in asthma severity classification based on immigration experiences (caregiver nativity and country of upbringing). ANOVAs were conducted to assess group differences in asthma morbidity (functional limitation, ED utilization) in acculturative stress and in family characteristics (family cohesion and contact with social networks) by migration patterns. Linear regression analyses were conducted to examine the associations between caregiver nativity, acculturative stress, family processes, and asthma outcomes, and controlling for demographic variables found in preliminary analyses to be potential confounds. For models in which all paths were statistically significant, we tested for mediation using Sobel's product of coefficient tests to ascertain the extent to which acculturation and family processes explained the association between immigration patterns and asthma outcomes. An α-level of .05 was used for all statistical tests. Effect sizes for analyses of variance were expressed as partial omega squared (ω2), interpreted as small (.01), medium (.06), or large (.14) (Cohen, 1988).
Results
Table I contains demographic and asthma characteristics and immigration patterns of the sample stratified by RI Latino ethnic group. There were no group differences in child gender, age, poverty threshold, asthma severity, or asthma morbidity in the 12 months prior to study participation. Group differences were found in frequency of ED visits, with 47.5% of RI Puerto Rican families reporting their children had been to the ED for asthma at least once in the previous 12 months, as compared to 30.5% of RI Dominican families (χ2 = 7.0, p < .01).
Table I.
Demographic, Immigration, and Asthma Characteristics by Group
| RI Puerto Rican | RI Dominican | |
|---|---|---|
| Child characteristics | ||
| Mean age in years (SD) | 10.6 (2.4) | 10.6 (2.5) |
| Gender (% male) | 50 | 53 |
| Below poverty threshold (%) | 60 | 57 |
| Asthma severity (%) | ||
| Mild intermittent | 13 | 17 |
| Mild persistent | 29 | 19 |
| Moderate persistent | 33 | 31 |
| Severe persistent | 26 | 34 |
| One or more ED visits previous 12 months (%)* | 48 | 31 |
| Mean score, asthma functional limitation in previous year (SD) | 1.7 (0.8) | 1.6 (0.7) |
| Parent characteristics | ||
| Biological mother (%) | 91 | 92 |
| Country of birth (%)** | ||
| United States | 29 | 8 |
| Puerto Rico | 71 | 1 |
| Dominican Republic | 0 | 92 |
| Country of Upbringing (%)** | ||
| United States | 42 | 10 |
| Puerto Rico | 58 | 1 |
| Dominican Republic | 0 | 89 |
*p < .05; **p < .01.
Associations Among Demographic Characteristics, Immigration Variables, and Asthma Indicators
Preliminary analyses were undertaken to examine associations among demographic variables (child age, gender, and family poverty status), asthma severity, functional limitation, ED visits, and immigration-related factors. Results from these analyses informed which covariates to hold constant in subsequent analyses. Asthma severity and functional limitation did not vary as a function of any of the demographic or immigration variables. Frequency of ED visits was marginally related to caregiver nativity (χ2 = 5.87, p = .05), suggesting that more children of caregivers born in island PR (41%) or the DR (44%) had at least 1 ED visit in the previous year relative to children of caregivers born in the mainland U.S. (14.8%). Caregiver nativity and country of upbringing were unrelated to the other asthma and demographic variables.
Immigration-Related Factors, Asthma Severity, and Morbidity
Next, we examined differences in children's level of asthma severity and morbidity (functional limitation, ED utilization) based on families’ immigration experiences (caregiver nativity or country of upbringing). Results appear in Table II. No demographic characteristics were associated with either immigration variable or asthma severity, thus, none were included as covariates in this analysis. No differences in children's level of asthma severity emerged based on caregiver nativity or country of upbringing.
Table II.
Child Asthma Characteristics by Family Immigration Experiences
| United States | Puerto Rico | Dominican Republic | Group differences | Effect sizesa | |
|---|---|---|---|---|---|
| Caregiver nativity | |||||
| Child asthma severity (%) | χ2 = 3.0 | ||||
| Mild intermittent | 15 | 14 | 16 | ||
| Mild persistent | 26 | 27 | 20 | ||
| Moderate persistent | 31 | 34 | 30 | ||
| Severe persistent | 28 | 25 | 34 | ||
| Asthma related functional limitation,bM (SD) | 1.5 (0.8) | 1.7 (0.7) | 1.6 (0.7) | F (2,232) = 1.8 | ωp2 = .01 |
| 1 or more ED visits previous 12 monthsb (%) | 33 | 49 | 33 | F (2.232) = 3.5* | ωp2 = .02 |
| Parent country of upbringing | |||||
| Child asthma severity (%) | χ2 = 5.0 | ||||
| Mild intermittent | 15 | 12 | 17 | ||
| Mild persistent | 29 | 25 | 20 | ||
| Moderate persistent | 29 | 38 | 28 | ||
| Severe persistent | 27 | 25 | 35 | ||
| Asthma related functional limitationb, M (SD) | 1.5 (0.8) | 1.8 (0.7) | 1.6 (0.8) | F (2,231) = 2.1 | ωp2 = .01 |
| 1 or more ED visits previous 12 monthsb (%) | 37 | 48 | 33 | F (2,231) = 2.3 | ωp2 = .01 |
aPartial omega squared (ωp2), interpreted as small (.01), medium (.06) or large (.14) (Cohen, 1988).
bControlling for asthma severity.
*p < .05; **p < .01; ***p < .001.
In examining the relationship between immigration variables and asthma-related functional limitation, we controlled for asthma severity given it was significantly associated with both of these variables in preliminary analyses. No differences in asthma functional limitation emerged as a function of caregiver nativity [F(2,232) = 1.8, ns] or country of upbringing [F(2,231) = 2.1, ns].
ED visits for asthma, controlling for asthma severity, did vary as a function of caregiver nativity (F(2,232) = 3.5, p < .05). Post hoc tests indicated that a larger proportion of children with caregivers born in island PR had at least one ED visit in the previous 12 months relative to children of caregivers born in the DR (50% vs. 32%, respectively). ED visits did not vary as a function of caregiver country of upbringing [F(2,231) = 2.3, ns].
Immigration and Acculturation-Related Factors and Family Characteristics
Our next set of analyses examined differences in acculturative stress, family cohesion, and social networks based on families’ immigration experiences, controlling for poverty threshold (as poverty threshold was related to acculturative stress and family resources). Consistent with our health disparities framework, controlling for the effects of poverty allows us to identify whether there may be differences in these processes based on immigration experiences. Results appear in Table III.
Table III.
Immigration and Acculturation-Related Factors and Family Characteristics
| United States | Puerto Rico | Dominican Republic | Group differences | Effect sizesa | Post hoc | |
|---|---|---|---|---|---|---|
| Parent nativity | ||||||
| Acculturative stress,bM (SD) | 0.4 (0.3) | 0.5 (0.4) | 0.4 (0.3) | F (2,219) = 3.6* | ωp2 = .02 | PR > DR* |
| Family cohesion,bM (SD) | 22.9 (5.3) | 23.9 (4.8) | 25.8 (3.4) | F (2,232) = 9.2*** | ωp2 = .07 | US < DR*** |
| PR < DR* | ||||||
| Contact with social network,bM (SD) | 0.2 (0.4) | 0.3 (0.5) | 0.4 (0.5) | F (2,232) = 6.5** | ωp2 = .05 | US < DR** |
| Parent country of upbringing | ||||||
| Acculturative stress,bM (SD) | 0.5 (0.4) | 0.5 (0.3) | 0.4 (0.3) | F (2,218) = 1.6 | ωp2 = .01 | – |
| Family cohesion,bM (SD) | 23.0 (5.3) | 24.5 (4.4) | 25.7 (3.4) | F (2,231) = 8.1** | ωp2 = .06 | US < DR*** |
| Contact with social network,bM (SD) | 0.2 (0.4) | 0.3 (0.5) | 0.4 (0.5) | F (2,231) = 5.3** | ωp2 = .04 | US < DR** |
aPartial omega squared (ωp2), interpreted as small (.01), medium (.06), or large (.14) (Cohen, 1988).
bControlling for poverty level.
*p < .05; **p < .01; ***p < .001.
Acculturative Stress
The results from the ANOVA including acculturative stress showed significant group differences based on caregiver nativity, after controlling for poverty [F(2,219) = 3.57; p < .05]. Post hoc analyses showed significant group differences between island PR born caregivers and DR born caregivers. Island PR born caregivers reported the highest levels of acculturative stress and U.S. born caregivers reported the lowest levels. No significant group differences emerged in acculturative stress based on caregiver country of upbringing [F(2,218) = 1.62, ns].
Family Cohesion
The results from the ANOVA including family cohesion showed significant group differences based on caregiver nativity, after controlling for poverty [F(2,232) = 9.16; p < .001]. Post hoc analyses showed that significant group differences resided between DR-born caregivers and U.S. mainland-born caregivers, and between PR-born caregivers and DR-born caregivers. DR-born caregivers reported the highest levels of family cohesion and U.S. mainland-born caregivers reported the lowest levels of family cohesion.
The results from the ANOVA examining group differences in family cohesion based on country of upbringing was significant [F(2,227) = 8.08; p < .01]. Post hoc tests indicated a significant group difference between caregivers who spent the most time during childhood in the DR and those who spent most of the childhood in the mainland U.S. Caregivers who spent the most time during childhood in the DR reported the highest levels of family cohesion.
Contact with Social Networks
The results from the ANOVA including contact with social networks showed significant group differences based on caregiver nativity, after controlling for poverty [F(2,228) = 6.45; p < .05]. Post hoc analyses indicated differences between DR-born and mainland-born caregivers. DR-born caregivers reported the highest levels, and mainland U.S.-born caregivers reported the lowest levels of contact with social networks.
Contact with social networks varied significantly by caregiver's country of upbringing [F(2,231) = 5.27; p < .01]. Follow-up tests indicated that caregivers who spent the most time during childhood in the DR had significantly higher levels of contact with social networks than caregivers who spent most of the childhood in the mainland U.S.
Mediational Analyses
A series of six mediational analyses were conducted to explore whether associations between immigration variables (country of caregiver upbringing, caregiver nativity) and ED visits were mediated by acculturative stress, family cohesion, or social network contacts, while controlling for poverty threshold and asthma severity. This approach allows us to identify potential acculturation-related factors and family characteristics that contribute to asthma morbidity. For each mediational analysis, a series of linear regressions was conducted to test associations between (a) the IV (independent variable) and the mediator, (b) the mediator and the DV (dependent variable), and (c) the IV and the DV. According to Baron and Kenny (1986), for mediation to be present, the IV must be significantly associated with the DV, and this association must be reduced by the presence of the mediating variable. To statistically confirm mediation as recommended by MacKinnon and colleagues (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002) we then conducted Sobel's (1988) product of coefficients test for each mediation analysis, which determined whether the indirect pathway in each model (IV → Mediator → DV) was statistically significant. Analyses were conducted using ED visits as the dependent variable, as this was the only asthma outcome significantly associated with immigration and cultural processes in preliminary analyses.
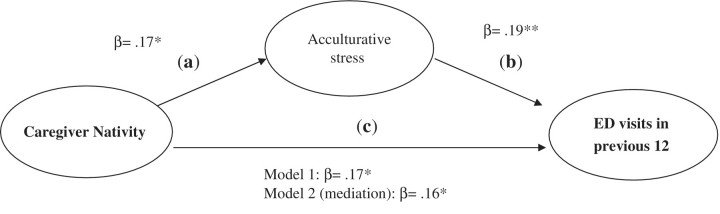
Prior to the analyses, effect coding was applied to the categorical migration variable. Values for caregiver nativity (PR, DR, or U.S. born) were assigned to make comparisons between U.S.- and PR or DR-born caregivers, and between PR and DR-born caregivers. Values for country of caregiver upbringing (U.S. mainland, island PR or DR) were assigned to compare island versus mainland, and PR versus DR. Figure 2 shows an example of the models tested, and displays results of the only model in which all paths were statistically significant. In this analysis, caregiver nativity (island PR vs. DR) significantly predicted cultural stress (path a, β = .17, p < .05), and ED visits (path c, β = .17, p < .05), and cultural stress predicted ED visits (path b, β = .18, p < .01). In the final model, the predictive power of caregiver nativity on ED visits was slightly reduced by the inclusion of cultural stress (β = .16, p < .05). The Sobel test of the indirect effect of nativity on ED visits was not significant (Z = 1.76, p = .08). These results suggest that caregiver immigration history and acculturative stress, though related processes, may operate independently of each other to effect frequency of ED visits in our sample.
Figure 2.
Mediation model: caregiver nativity, acculturative stress, and ED visits in previous 12 months.
An examination of the unique predictive variance of the two variables indicated that they predicted a modest but significant amount of variance in ED usage. Caregiver nativity alone accounted for 2.8% of unique variance in ED visit frequency [Fchange (2,218) = 3.35, p < .05], and the addition of cultural stress to the model contributed an additional 2.4% [Fchange(1,217) = 5.80, p < .05]. The entire model, including severity and poverty threshold covariates, accounted for 9.8% of the variance in ED visits [F(5,217) = 4.70, p < .001].
Discussion
Summary of Findings from the Current Study
The current study focused on the effects of immigration and acculturation-related factors and family characteristics on pediatric asthma morbidity (e.g., ED use) among a sample of Puerto Rican and Dominican families residing in the U.S. After controlling for severity, children of foreign-born caregivers (caregivers born in PR or DR) had a higher risk for an ED visit due to asthma in the previous year compared to children of U.S.-born caregivers. Children of Island PR born caregivers had a higher proportion of ED visits relative to children of DR born caregivers. Severity levels and asthma-related functional limitation did not appear to be different between the groups based on immigration-related factors.
Our recent work suggests that patterns of health care utilization differ based on place of residence, as rates of ED use were found to be higher among Island PR versus mainland PR children, despite the fact that severity rates were higher among mainland Latino children (Esteban et al., 2009). Families may be following health care utilization patterns established in their country of origin. Families may also be using the ED more often because of lack of preventive management, as they may not be aware of how to appropriately respond to symptoms. Less is known about why DR born families use the ED room more often than mainland-born, Latino families, as factors that account for patterns of health care utilization for asthma in the DR have not been studied in depth.
After controlling for poverty, Island PR born caregivers reported the highest levels of acculturative stress and U.S. born caregivers (either PR or DR) reported the lowest levels. It may be that stress associated with the acculturation process complicates effective asthma management; however, the nature of this relationship bears further examination in future research. Further, caregivers who were Dominican-born and raised reported the highest levels of family cohesion; and U.S. born caregivers reported the lowest levels of family cohesion. Caregivers born and raised in the DR also reported higher levels of contact with social networks than their U.S. born or PR born counterparts. In the context of the results indicating differences in ED rates by caregiver nativity, these findings suggest important family resources that can be drawn upon when facing stress related to asthma management. These results may be explained, in part, by where DR families tend to reside within specific neighborhoods in the Greater Providence urban area. Within this urban setting, enclaves of families from the DR live in close proximity to one another (Uriarte, Carrion, Jones, Carithers, & Carlos Gorlier, 2002). This may influence the nature of family connectedness and social support received on a daily basis. In contrast, PR families tend to be more widely dispersed throughout the city and may experience more travel back and forth to PR, which may fragment or inhibit the level of social support received.
Results from mediational analyses suggest that caregiver nativity and cultural stress may operate independently in their association with frequency of ED visits for this sample. Further, hierarchical regression analyses indicated that both nativity and cultural stress accounted for a unique portion of the variance in ED visit frequency. Although families may experience higher or lower levels of acculturative stress, depending on immigration history, it is not clear if this stress may influence the decision process to use the ED.
There are a host of other factors both related to and unrelated to the immigration and acculturation experience that may affect families’ use of the ED for asthma, many of which were beyond the scope of this study to examine. For example, the timing of a family's move to a new country and child's diagnosis of asthma may influence how the family fares with asthma management. Additionally, health care system factors may play a role (Canino et al., 2006), as families who are unfamiliar with the health care system in their new host country may have difficulty connecting with a consistent health care provider. Finally, barriers to preventative medication use and beliefs about medications should be considered as contributors of morbidity in PR children, as Island PR families with public health insurance report many more health care system barriers, such as obtaining asthma medications, than mainland U.S. Latino families (McQuaid et al., 2009).
Where do we go from here? Future Directions for Research
Several limitations of this study and the studies reviewed above should be considered and addressed in future research. First, the immigration and acculturation experience tends to be narrowly defined. Along with nativity, results overall suggest that acclimating to a different context (e.g., Mainland U.S.) may have an impact on the asthma outcomes of Latino children. More studies need to include a range of immigration-related factors including how child and caregiver nativity, length of stay in the U.S. over time, and processes related to acculturation (e.g., preferred language, comfort level with mainland norms) may increase or mitigate risk for developing asthma and morbidity among children of different Latino ethnic subgroups. Our measure of social support was limited to a two-item assessment that examined the extent to which caregivers actually utilize the supports that are available to them. Although this subscale did yield significant results in its relation with asthma morbidity, results are preliminary and should be interpreted with caution given the low internal consistency of the measure. Assessment of social networks should be studied more carefully, with a more psychometrically sound measure in future research. Moreover, associations among these processes need to be examined over time using longitudinal designs. Cross-sectional approaches, such as the one used in our study, pose limitations for testing important causal associations and do not allow for the examination of temporal associations between processes and multiple pathways of influence in the variables studied (Maxwell & Cole, 2007). For example, in future longitudinal research, it would be important to test whether caregiver nativity (at Time 1) influenced acculturative stress (at Time 2), and subsequently, whether stress related to acculturation affected increased asthma morbidity (at Time 3) in children from specific Latino ethnic subgroups.
The sample sizes in the studies reviewed above (including our study) are small. This may have contributed to the number of nonsignificant findings generated from our study. Further, with regard to our study, although ANOVA results from our study indicated significant group differences on acculturative stress, family cohesion, and contact with social networks across Latino ethnic groups based on caregivers’ nativity, a comparison of the group means of these groups suggests that the differences are small, and therefore, the clinical import of the results should be interpreted with caution. In addition, the studies tend to only include specific Latino ethnic subgroups. This makes it difficult to generalize results beyond these specific groups. Investigating these associations among subgroups of Latinos from different countries of origin (e.g., Mexico, DR, Cuba) may help disentangle the effects of environmental and immigration-related factors. For example, exposure to farm environments in early life may lower the risk for the development of asthma (Riedler, Eder, Oberfeld, & Schreuer, 2000). This may be particularly relevant for Mexican-born children and caregivers, who may have more exposure to farm environments during their early growth. Further, studies with larger samples that categorize Latino subgroups by caregiver nativity and ethnic background (e.g., PR ethnicity born in U.S., DR ethnicity born in U.S., PR ethnicity born in PR, DR ethnicity born in DR) may provide further specificity in how ethnic background, caregiver nativity and an interaction of the two can influence children's asthma morbidity.
What can be Learned from Research Examining Mental Health Outcomes in Latino Immigrants?
Among Latinos, findings in the realm of mental health disparities have given rise to the discussion of the Immigrant Paradox. This term refers to “the relatively good health and longer life span of foreign-born Latinos when expectations (based on their socioeconomic status) suggest far greater morbidity and mortality than observed” (Cagney, Browning, & Wallace, 2007). Data indicate that Latino immigrants have better mental health than their U.S.-born counterparts and Non-Latino Whites (Alegria, Mulvaney-Day et al., 2007). Findings from NLAAS (National Latino and Asian American Study), a study on the prevalence of psychiatric disorders among US Latinos, have shown that foreign nativity is associated with better mental health outcomes for some Latino groups (e.g., Mexicans) but not others (e.g., Puerto Ricans; Alegria, Shrout et al., 2007). As immigrants participate actively in American life; however, they become more similar to U.S.- born individuals in that their mental health may decline with more integration with American cultures, values, and lifestyles (Alegria, Shrout et al., 2007).
The “immigrant paradox,” evident in the adult mental health literature, is not reflected by some of the results of pediatric asthma studies. Data thus far indicate that overall, Latino children do worse in terms of asthma prevalence or morbidity than their non-Latino white counterparts. Upon closer inspection, we learn that level of asthma risk and morbidity may be worse for children of foreign-born than U.S.-born Latino caregivers. Among children of foreign-born caregivers, children of PR and DR-born immigrants may be more at risk than children of Mexican-born immigrants in terms of asthma prevalence. However, risk for morbidity may be worse overall for children of PR and DR-born caregivers who immigrate to the mainland U.S.
Timing of immigration and duration of residence in the host country are important factors to consider in future asthma research, as it has been shown in the mental health literature that Latino immigrants who arrive to the U.S. before the age of six are more similar in their mental health status to U.S.-born Latinos (Alegria, Shrout, et al., 2007). This may explain, in part, the contradictory findings in the asthma literature (in the studies that include PRs) that do not support the immigrant paradox. It may be that many caregivers in these samples arrived to the U.S. at an early age, and their child's health is affected by more exposure to the U.S. mainland. Moreover, the interaction between genetic predisposition, acculturation, and immigration is important to consider in furthering knowledge of why Latino immigrants from specific subgroups may be more at risk.
In summary, our study includes a focus on caregiver immigration and acculturation on pediatric asthma morbidity, which has been previously understudied. Findings show that specific stresses related to the acculturation process itself, as well as family attributes and resources that are drawn upon during this time (e.g., family networks, social support), should be considered in future work examining immigration factors and asthma outcomes in children. Future research should also identify the potential protective effect that higher levels of family cohesion and social support may have for Latino children's asthma management in the context of poverty. Our inclusion of both Puerto Rican and Dominican groups provides a useful, first-step analysis of the factors that may distinguish families’ immigration and acculturation experience to the mainland, and in turn, how these experiences may affect children's asthma outcomes.
Results from our study and from those studies reviewed above suggest that a variety of immigration-related indicators (caregiver nativity, child nativity, timing of migration, length of stay in host country and mainland) and factors related to the acculturation process (levels of acculturative stress, language preference, level of social support, family resources) are needed to capture how these experiences may affect asthma management and outcomes of morbidity. Qualitative approaches that examine perceptions of asthma treatment and health care use prior to family's arrival to the mainland may inform interventions that are amenable to where families are in their trajectory of immigration and acculturation. More guided supports (e.g., education about how to effectively navigate the health care system, psychological services to help decrease stress levels related to acculturation, support in connecting families from similar backgrounds with one another, support in how to find interpreter services) may be needed for families who recently immigrate to the mainland and have a child with asthma.
Funding
Funds for this study were provided by grant # U01-Hl072438-01 from the National Heart Lung and Blood Institute (to G. K. F., G. C., PIs); and grant # 5P60 MD002261-02 from the National Center for Minority Health and Health Disparities (to G. C., P. I.).
Conflicts of interest: None declared.
Footnotes
*The methods of this study are based on a study first reported in Canino, G., McQuaid, E. L., Alvarez, M., Colon, A., Esteban, C., Febo, V., et al. (2009). Issues and methods in disparities research: The Rhode Island-Puerto Rico Asthma Center. Pediatric Pulmonology, 44(9), 899–908.
References
- Alegria M, Canino G, Stinson F S, Grant B F. Nativity and DSM-IV psychiatric disorders among Puerto Ricans, Cuban Americans, and non-Latino Whites in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2006;67:56–65. doi: 10.4088/jcp.v67n0109. [DOI] [PubMed] [Google Scholar]
- Alegria M, Mulvaney-Day N, Woo M, Torres M, Gao S, Oddo V. Correlates of past-year mental health service use among Latinos: Results from the National Latino and Asian American Study. American Journal of Public Health. 2007;97:76–83. doi: 10.2105/AJPH.2006.087197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Shrout P E, Woo M, Guarnaccia P, Sribney W, Vila D, Polo A, Cao Z, Mulvaney Day N, Torres M, Canino G. Understanding differences in past year psychiatric disorders for Latinos living in the US. Social Science & Medicine. 2007;65:214–230. doi: 10.1016/j.socscimed.2007.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Takeuchi D, Canino G, Duan N, Shrout P, Meng X L, Vega W, Zane N, Vila D, Woo M, Vera M, Guarnaccia P, Aguilar-gaxiola S, Sue S, Escobar J, Lin K-M, Gong F. Considering context, place and culture: the National Latino and Asian American Study. International Journal Methods and Psychiatric Research. 2004;13:208–220. doi: 10.1002/mpr.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Vila D, Woo M, Canino G, Takeuchi D, Vera M, Febo V, Guarnaccia P, Aguilar-Gaxiola S, Shrout P. Relevance and equivalence in the NLAAS instrument: Integrating etic and emic in the development of cross-cultural measures for a psychiatric epidemiology and services study of Latinos. International Journal of Methods and Psychiatric Research. 2004;13:270–288. doi: 10.1002/mpr.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burchard E G, Avila P C, Nazario S, Casal J, Torres A, Rodriguez-Santana J R, Toscano M, Sylvia J S, Alioto M, Salazar M, Gomez I, Fagan J K, Salas J, Lilly C, Matallana H, Ziv E, Castro R, Selman M, Chapela R, Sheppard D, Weiss S T, Ford J G, Boushey H A, Rodriguez-Cintron W, Drazen J M, Silverman E K Genetics of Asthma in Latino Americans (GALA) Study. Lower bronchodilator responsiveness in Puerto Rican than in Mexican subjects with asthma. American Journal of Respiratory and Critical Care Medicine. 2004;169:386–392. doi: 10.1164/rccm.200309-1293OC. [DOI] [PubMed] [Google Scholar]
- Cagney K A, Browning C R, Wallace D M. The Latino paradox in neighborhood context: The case of asthma and other respiratory conditions. American Journal of Public Health. 2007;97:919–925. doi: 10.2105/AJPH.2005.071472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canino G, Bravo M. The adaptation and testing of diagnostic and outcome measures for cross-cultural research. International Review of Psychiatry. 1994;6:281–286. [Google Scholar]
- Canino G, Koinis-Mitchell D, Ortega A, McQuaid E, Fritz G, Alegria M. Asthma disparities in the prevalence, morbidity and treatment of Latino children. Social Science and Medicine. 2006;63:2926–2937. doi: 10.1016/j.socscimed.2006.07.017. [DOI] [PubMed] [Google Scholar]
- Canino G, McQuaid E L, Alvarez M, Colon A, Esteban C, Febo V. Issues and methods in disparities research: The Rhode Island-Puerto Rico asthma center. Pediatric Pulmonology. 2009;44:899–908. doi: 10.1002/ppul.21075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control. Asthma - United States, 2003. 2005. Centers for Disease Control. [Google Scholar]
- Cervantes R, Padilla A, Salgado de Snyder W. The Hispanic Stress Inventory: A culturally relevant approach to psychological assessment. Psychological Assessment. 1991;3:438–447. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- Cohen R T, Canino G J, Bird H R, Shen S, Rosner B A, Celedon J C. Area of residence, birthplace, and asthma in Puerto Rican children. Chest. 2007;131:1331–1338. doi: 10.1378/chest.06-1917. [DOI] [PubMed] [Google Scholar]
- Duarte C S, Bird H R, Shrout P E, Wu P, Lewis-Fernandez R, Shen S, Canino G. Culture and psychiatric symptoms in Puerto Rican children: Longitudinal results from one ethnic group in two contexts. Journal of Child Psychology and Psychiatry. 2008;49:563–572. doi: 10.1111/j.1469-7610.2007.01863.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eldeirawi K M, Persky V W. Associations of physician-diagnosed asthma with country of residence in the first year of life and other immigration-related factors: Chicago asthma school study. Annals of Allergy, Asthma,& Immunology. 2007;99:236–243. doi: 10.1016/S1081-1206(10)60659-X. [DOI] [PubMed] [Google Scholar]
- Esteban C A, Klein R B, McQuaid E L, Fritz G K, Seifer R, Kopel S J, Rodriguez-Santana J, Colon A, Alvarez M, Koinis Mitchell D, Ortega A N, Martinez-Nieves B, Canino G. Conundrums in childhood asthma severity, control, and health care use: Puerto Rico versus Rhode Island. Journal of Allergy and Clinical Immunology. 2009;124:238–244.e235. doi: 10.1016/j.jaci.2009.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gil A, Vega W. Two different worlds: Acculturation stress and adaptation among Cuban and Nicaraguan families. Journal of Social and Personal Relationships. 1996;13:435–456. [Google Scholar]
- Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. 2002 Retrieved from the Global Initiative for Asthma website: http://www.ginasthma.org. [Google Scholar]
- Holguin F, Mannino D M, Anto J, Mott J, Ford E S, Teague W G, Redd S C, Romieu I. Country of birth as a risk factor for asthma among Mexican Americans. American Journal of Respiratory and Critical Care Medicine. 2005;171:103–108. doi: 10.1164/rccm.200402-143OC. [DOI] [PubMed] [Google Scholar]
- Hunninghake G M, Weiss S T, Celedón J C. State of the art: Asthma in Hispanics. American Journal of Respiratory and Critical Care Medicine. 2006;173:143–163. doi: 10.1164/rccm.200508-1232SO. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt L M, Schneider S, Comer B. Should “acculturation” be a variable in health research? A critical review of research on US Hispanics. Social Science & Medicine. 2004;59:973–986. doi: 10.1016/j.socscimed.2003.12.009. [DOI] [PubMed] [Google Scholar]
- Kattan M, Stearns S C, Crain E F, Stout J W, Gergen P J, Evans R, III, Visness C M, Gruchalla R S, Morgan W J, O'Connor G T, Mastin J P, Mitchell H E. Cost-effectiveness of a home-based environmental intervention for inner-city children with asthma. Journal of Clinical Immunology. 2005;116:1058–1063. doi: 10.1016/j.jaci.2005.07.032. [DOI] [PubMed] [Google Scholar]
- Klinnert M D, Price M R, Liu A H, Robinson J L. Unraveling the ecology of risks for early childhood asthma among ethnically diverse families in the Southwest. American Journal of Public Health. 2002;92:792–798. doi: 10.2105/ajph.92.5.792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klinnert M D, Price M R, Liu A H, Robinson J L. Morbidity patterns among low-income wheezing infants. Pediatrics. 2003;112:49–57. doi: 10.1542/peds.112.1.49. [DOI] [PubMed] [Google Scholar]
- Koinis-Mitchell D, McQuaid E, Seifer R, Kopel S, Esteban C, Canino G, Garcia-Coll C, Klein R, Fritz G. Multiple urban and asthma-related risks and their association with asthma morbidity in children. Journal of Pediatric Psychology. 2007;32:582–595. doi: 10.1093/jpepsy/jsl050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara M, Akinbami L, Flores G, Morgenstern H. Heterogeneity of childhood asthma among Hispanic children: Puerto Rican children bear a disproportionate burden. Pediatrics. 2006;117:43–53. doi: 10.1542/peds.2004-1714. [DOI] [PubMed] [Google Scholar]
- Lara M, Gamboa C, Kahramanian M I, Morales L S, Bautista D E. Acculturation and Latino health in the United States: A review of the literature and its sociopolitical context. Annual Review of Public Health. 2005;26:367–397. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leidy M, Guerra N G, Toro R. The impact of positive parenting and family cohesion on social competence among children of immigrant Latino parents: A mixed methods study. Journal of Family Psychology. 2010;24:252–260. doi: 10.1037/a0019407. [DOI] [PubMed] [Google Scholar]
- MacKinnon D P, Lockwood C M, Hoffman J M, West S G, Sheets V. A comparison of methods to test the significance of the mediated effect. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin M A, Shalowitz M U, Mijanovich T, Clark-Kauffman E, Perez E, Berry C A. The effects of acculturation on asthma burden in a community sample of Mexican American schoolchildren. American Journal of Public Health. 2007;97:1290–1296. doi: 10.2105/AJPH.2006.092239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matías-Carrelo L, Chavez L M, Negrón G, Canino G, Aguilar-Gaxiola S, Hoppe S. The Spanish translation and cultural adaptation of five outcome measures. Culture, Medicine and Psychiatry. 2003;27:291–313. doi: 10.1023/a:1025399115023. [DOI] [PubMed] [Google Scholar]
- Maxwell S E, Cole D A. Bias in cross-sectional analyses of longitudinal mediation. Psychological Methods. 2007;12:23–44. doi: 10.1037/1082-989X.12.1.23. [DOI] [PubMed] [Google Scholar]
- McQuaid E, Walders N, Kopel S, Fritz G, Klinnert M. Pediatric asthma management in the family context: The family asthma management system scale. Journal of Pediatric Psychology. 2005;30:492–502. doi: 10.1093/jpepsy/jsi074. [DOI] [PubMed] [Google Scholar]
- McQuaid E L, Vasquez J, Canino G, Fritz G K, Ortega A N, Colon A, Klein R B, Kopel S J, Koinis-Mitchell D, Esteban C, Seifer R. Beliefs and barriers to medication use in parents of Latino children with asthma. Pediatric Pulmonology. 2009;44:892–898. doi: 10.1002/ppul.21074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson D H. Circumplex Model VII: Validation studies and FACES III. Family Process. 1986;25:337–351. doi: 10.1111/j.1545-5300.1986.00337.x. [DOI] [PubMed] [Google Scholar]
- Ortega A, McQuaid E, Canino G, Ramirez R, Fritz G, Klein R. Association of psychiatric disorders and different indicators of asthma in island Puerto Rican children. Social Psychiatry and Psychiatric Epidemiology. 2003;38:220–226. doi: 10.1007/s00127-003-0623-6. [DOI] [PubMed] [Google Scholar]
- Riedler J, Eder W, Oberfeld G, Schreuer M. Austrian children living on a farm have less hay fever, asthma and allergic sensitization. Clinical & Experimental Allergy. 2000;30:194–200. doi: 10.1046/j.1365-2222.2000.00799.x. [DOI] [PubMed] [Google Scholar]
- Rosier M J, Bishop J, Nolan T, Robertson C F, Carlin J B, Phelan P D. Measurement of functional severity of asthma in children. American Journal of Respiratory and Critical Care Medicine. 1994;149:1434–1441. doi: 10.1164/ajrccm.149.6.8004295. [DOI] [PubMed] [Google Scholar]
- Sobel M E. Direct and indirect effects in linear structural equation models. 1988 In J. S. Long (Ed.), Common problems/proper solutions: Avoiding error in quantitative research (pp. 46–64). Beverly Hills, CA: Sage. [Google Scholar]
- Uriarte M, Carrion E, Jones C, Carithers N, Carlos Gorlier J. Latinos in Rhode Island: A scan of issues affecting the Latino population in Rhode Island. Providence, RI: The Rhode Island Foundation; 2002. [Google Scholar]
- U.S. Census Bureau. Projected Population of the United States, by Race and Hispanic Origin: 2000 to 2050. Retrieved from U.S. Census Bureau; 2004. http://www.census.gov/ipc/www/usinterimproj/ [Google Scholar]
- U.S. Department of Health and Human Services. The 2005 HHS Poverty Guidelines. Washington, DC: U.S. Department of Health and Human Services; 2005. [Google Scholar]