Abstract
Background
Obstructed labour is still a major cause of maternal and perinatal morbidity and mortality in Uganda, where many women give birth at home alone or assisted by non-skilled birth attendants. Little is known of how the community view obstructed labour, and what actions they take in cases where this complication occurs.
Objective
The objective of the study was to explore community members’ understanding of and actions taken in cases of obstructed labour in south-western Uganda.
Design
Grounded theory (GT) was used to analyse data from 20 focus group discussions (FGDs), 10 with women and 10 with men, which were conducted in eight rural and two urban communities.
Results
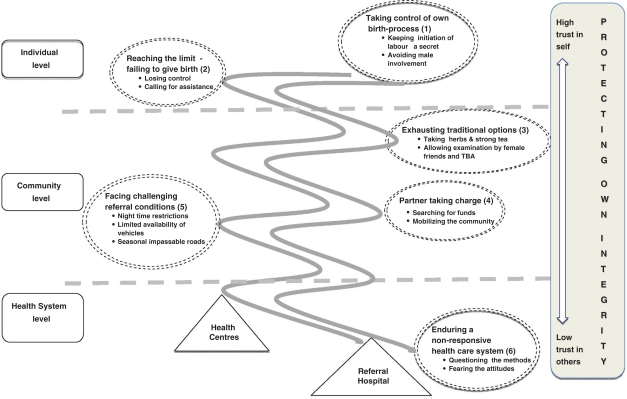
A conceptual model based on the community members’ understanding of obstructed labour and actions taken in response is presented as a pathway initiated by women's desire to ‘protecting own integrity’ (core category). The pathway consisted of six other categories closely linked to the core category, namely: (1) ‘taking control of own birth process’; (2) ‘reaching the limit – failing to give birth’ (individual level); (3) ‘exhausting traditional options’; (4) ‘partner taking charge’; (5) ‘facing challenging referral conditions’ (community level); and finally (6) ‘enduring a non-responsive healthcare system’ (healthcare system level).
Conclusions
There is a need to understand and acknowledge women's reluctance to involve others during childbirth. However, the healthcare system should provide acceptable care and a functional referral system closer to the community, thus supporting the community's ability to seek timely care as a response to obstructed labour. Easy access to mobile phones may improve referral systems. Upgrading of infrastructure in the region requires a multi-sectoral approach. Testing of the conceptual model through a quantitative questionnaire is recommended.
Keywords: obstructed labour, community members, understanding, actions, protecting own integrity, Uganda, Africa, maternal mortality, childbirth, delivery care, mobile phones, transport
The community's role in reducing maternal mortality in resource poor settings is often considered less important than that of obstetric healthcare services. However, research indicates that community involvement is an important component of healthcare interventions targeting maternal and new-born health (1–3).
One of the five major causes of maternal mortality is obstructed labour, which globally accounts for 8% of all maternal deaths (4). Although the causes of obstructed labour are wellknown (5–7), other factors influence the outcome; notably the delay by the pregnant woman or her family to make a decision to seek care [first delay], the difficulty of reaching the hospital once the decision has been taken [second delay] and delay in care at the referral unit [third delay] (8). Around 15%–20% of all deliveries are expected to require emergency obstetric care (9–13). In resource poor settings, the healthcare structure may not respond adequately to meet demands at this level. On the other hand, it is evident that the population do not adequately seek the services, even when required.
Whereas several studies have discussed the magnitude, causes and outcome of obstructed labour as well as the health system's response (14–18); not much has been reported on the community's understanding and management of obstructed labour. In Uganda, where the national figures of obstructed labour are high (19) and where most women prefer home births (20), maternal mortality due to obstructed labour is common. Recent studies reported that obstructed labour is the second largest direct cause (22%) of maternal mortality in the country (19, 21). In south-western Uganda the prevalence of obstructed labour in six hospitals was recently estimated to be around 10% (22). There exists a knowledge gap on the communities’ understanding and actions taken in cases of obstructed labour.
The objective of the study was to explore community members’ understanding of and actions taken in response to obstructed labour in south-western Uganda.
Methods
Grounded theory (GT) is commonly used to study phenomena about which little is known (23). To our knowledge, community members’ understanding of obstructed labour has previously not been highlighted in the literature. GT, with its’ specific feature of simultaneous data collection and analysis, enables the researcher to pursue new ideas emerging during data collection, which in our study was conducted by focus group discussions (FGDs) (24). Combining group interaction with the pursuit of new ideas through GT techniques such as: [1] the constant comparison of previous and new data; and [2] the distinct coding process described under the analysis section (23) provided us with excellent tools to explore this topic.
Setting
The study was conducted in rural villages and urban communities in Mbarara district, south-western Uganda from September 2008 to November 2009. Mbarara district had a 2010 mid-year projected population of 427,200 (25). More than 80% live in rural areas, and the majority depend on subsistence agriculture. The district is administratively divided into three counties, 17 sub-counties, and 755 villages. The villages are the lowest administrative unit in the district. The district is served by one government hospital (Mbarara), and four private hospitals (Mayanja Memorial, Community, Ruharo Mission, Holy Innocents) located in the municipality of Mbarara. The hospitals provide comprehensive emergency obstetric care, which includes surgery and blood transfusion. The rural areas are further served by 49 health centres, which are evenly distributed throughout the district. As opposed to the hospitals, these only provide basic obstetric services, i.e. assistance at low-risk deliveries. Mbarara hospital serves as a regional referral hospital and also the main teaching hospital for health sciences students of Mbarara University of Science and Technology.
Sampling of informants
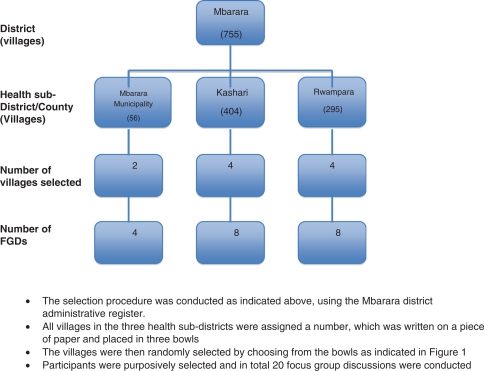
Using simple random sampling, 10 villages; eight rural and two urban, were selected as our study sites to ensure that both rural and urban villages were represented in the study (Fig. 1). Further, purposive sampling was used to identify key informants in each village, i.e. individuals familiar with the phenomenon being studied such as women in childbearing age, mothers-in-law, women leaders and grandmothers as well as male partners and male leaders. The purposive selection of informants consequently ensured that persons with varied knowledge regarding childbirth and prolonged labour were included in our study (26). The principal researcher Jerome Kabakyenga (JK) a public health specialist, and Phionah Kyomuhendo (PK) a social scientist, collaborated with the village leaders to identify informants. In total, 126 women and men participated in the 20 FGDs conducted. Sixty informants were women whose age ranged from 19 to 70 years with a mean age of 32.8 and 61 were men with an age range from 27 to 69 years and a mean age of 40.1. Table 1 shows the characteristics of the informants.
Fig. 1.
Selection of villages.
Table 1.
Characteristics of informants
| Characteristics | Women | Men |
|---|---|---|
| Number | 65 | 61 |
| Age group | ||
| <20 | 1 | 0 |
| 20–29 | 23 | 8 |
| 30–39 | 19 | 18 |
| 40–49 | 14 | 17 |
| 50–59 | 4 | 14 |
| 60–69 | 1 | 4 |
| 70+ | 1 | 0 |
| Mean age (years) | 32.8 | 40.1 |
| Age range (years) | 19–70 | 27–69 |
| Residence | ||
| Urban | 10 | 8 |
| Rural | 55 | 53 |
Data collection
A preliminary interview guide was developed and pretested by JK in the neighbouring Isingiro district. Due to simultaneous data collection and analysis (23) the guide that included topics such as perception of obstructed labour, decision process during care seeking in case of obstructed labour, selection of referral site and experience of skilled care at birth, was revised as new ideas emerged. However, all FGDs were initiated by asking the informants to discuss what their understanding of an obstructed labour was and what actions they took in case this complication occurred within their community. Probing was done according to what was discussed in the actual FGD but also according to ideas identified in the previous groups.
The FGDs had six to eight informants each to ensure group interaction (24). All FGDs were moderated by JK and assisted by PK. The discussions took place either in the living rooms of houses identified by PK or outside in the shade provided by big trees. Prior to initiating the FGD, the process was explained in detail. Individual verbal consent was sought from all informants and permission to use the tape recorder was requested. The equipment was tested to ensure its’ workability and to familiarise the informants with the situation. JK and PK conducted the FGDs, which lasted between 60 and 90 min in the local language ‘Runyankole’. The FGDs were transcribed verbatim and then translated to English.
Analysis
In line with GT (23), JK and PK conducted a brief discussion on their experiences of each FGD directly after the session ended to capture the initial interpretation and identify new ideas that needed to be pursued in the forthcoming FGDs. Coding of data was accomplished in the three stages suggested by Strauss and Corbin (23). Open coding, which entailed reading each transcript line by line to identify ideas and attach codes to these. Similar codes were pooled into categories and developed in terms of their characteristics and dimensions, i.e. ensuring a rich description of the category. An example illustrating this process is provided in Table 2.
Table 2.
Example of a coding process
| Codes | Category | Properties (characteristics) | Dimensions |
|---|---|---|---|
| Difficult finding transport Transport requires money Transport difficult to get at night Roads impassable during wet season | Facing challenging referral conditions | Type of transport Cost of transport availability of transport State of roads | Private – public Limited – extensive Night time –day time Wet season – dry season |
Axial coding included linking identified categories to each other and elaborating the conceptual model (Fig. 2) . Selective coding entailed refining of the categories, which was partly done through a comparison of the various data transcripts, but also by going back to the community for further information. Selective coding also included identification and labelling of the core category, the key aspect of the story being related (Fig. 2) . Data were jointly analysed by JK and KOP. Review and feedback during analysis and manuscript preparation was provided by Maria Emmelin (ME) and Per-Olof Östergren (P-OÖ). Quotations from data are referred to as ‘(FGD 1, W)’, i.e. discussion number one for women and ‘(FGD 1, M)’ discussion number one for male informants, based on the fact that FGDs are analysed at group level only (24).
Fig. 2.
Conceptual model of a pathway to obstructed labour as described by the community.
Ethical considerations
The study was granted formal ethics approval by Lund University and Uganda National Council of Science and Technology. Permission to conduct the study was obtained from the district and local leaders. Informants gave individual informed verbal consent prior to the start of each FGD.
Results
Based on the analysis of FGDs with women and men in the community, six categories, were identified, namely: (category 1) taking control of own birth process; (category 2) reaching the limit – failing to give birth; (category 3) exhausting traditional options; (category 4) partner taking charge; (category 5) facing challenging referral conditions; and (category 6) enduring the non-responsive healthcare system. The categories, as illustrated in the conceptual model (Fig. 2) , address aspects on individual level (categories 1, 2), community level (categories 3–-5) and healthcare system level (category 6). ‘Protecting own integrity, the core category, emerged as the concept that mirrors the community members’ frequent discussions around women's tendency to solitary withdrawal during childbirth. The core category was perceived as the key factor initiating the pathway that may lead to obstructed labour. Further, ‘protecting own integrity’, may, as indicated in the model, be reinforced by information and/or experience at the healthcare system level (category 6).
Protecting own integrity
The main characteristic of ‘protecting own integrity’ was trust, ranging from [1] high trust in self to [2] low trust in others. The high trust in self appears to originate in traditions and expectations of society, i.e. socio-cultural beliefs, and previous positive experiences of managing childbirth at home, either alone or with minimal assistance in the final stage of labour. Personal pride, identified as another characteristic of high trust in self, implied women's strong determination to reveal the true state of their condition only when they had something to show for the efforts undertaken, i.e. the baby itself. The low trust in others emanates from a need for privacy, which in turn is linked to aspects such as shame of exposing themselves in an intimate manner and a desire to prevent information related to living conditions from being spread in the community. Labour marks the climax of a 9-month pregnancy period where trust in self gradually builds up. As long as the labour process progresses normally, a woman is considered to be well prepared to take control of it by herself (category 1) . If the labour should stall, the woman will reluctantly agree to seek assistance from the very same community members in whom she has declared her low trust in category 2 . Despite agreeing to explore options available in the community (category 3) , the woman in labour will exercise her own will regarding who should be involved or not. Trust in self is dented but still part of the process. Low trust in others also includes the partner. He is left with no other option but to take charge once the woman seems to be unable to withstand his interference (category 4) . Once being in charge, the partner faces a variety of challenges when trying to solve the emergency transport required at this stage (category 5). The difficulties faced are clearly related to high trust in self and consequent delay in admitting that assistance is required. Finally the low trust in others is further fuelled by hearsay about and/or own experience of a non-responsive healthcare system (category 6).
The conceptual model visualises how the high trust emanating from the woman on an individual level, gradually weakens as the pathway moves towards the community level and encounter the non-responsive healthcare system.
Taking control of own birth process
According to the informants, women take over the control of the birth process by keeping the onset of labour a secret, with a particular aim of hiding the truth from their partners whom they mistrust as they are considered fearful, ignorant and not helpful in the actual process of labour:
I hid in the room with no one, I did not even tell my husband … but when I pushed only one leg came out … I pleaded with those I had hidden from … because I had wanted them to hear the kid crying. At that moment, they tried everything to take me to the hospital. (FGD 1, W)
Intuitively men may deduce that labour has already started or about to start, however, when asked whether labour has commenced, women usually reply in affirmative that it has not and present a picture of normality by going about their usual chores. As indicated by the citation below, men are conscious of women's determination to avoid male involvement and that they would rather prefer timely information to seek the available nearby care:
… now considering that we live close to the hospital … the problem with women is that they do not tell us (men). She will get labour pains and not say anything …. (FGD 18, M)
Being in control of own delivery also implied that women decided if and when to call for assistance. Being able to manage all alone was regarded as the ultimate proof of being courageous as opposed to being a coward who required assistance.
Reaching the limit – failing to give birth
Choosing solitary confinement was done with the anticipation that the entire process of labour would be uneventful. The informants, however, demonstrated knowledge regarding the uniqueness of each labour's progress, by stating that ‘each labour runs its’ own course’ (FGD 13, W). The community's perception on the duration of the normal labour process varied from 3 hours to 2 days. The duration of labour was also linked to the understanding that labour pains need to be productive (successful childbirth) for a labour to progress normally:
Some labour pains may start with high intensity but without yielding any results. They are real but they don't yield results …. (FGD 9, W)
Even if the closest family member and partner may suspect that the labour is not progressing normally, i.e. one would have expected the baby to be born, the acceptance of failure by the woman herself is required. According to the community they label the condition of a stalled progress of labour ‘ascending pregnancy’ and/or that the ‘pregnancy is hung’. At this point a woman realises she is ‘losing control’ and start the process of calling for assistance. Losing control was described in terms of ‘getting weak’, ‘looking pale’, ‘loosing breath’ and ‘failing to push’ all signs of becoming exhausted. According to the informants this was a result of premature pushing. Letting go of the control, however, was not always a clear-cut decision. The partner's suggestion, as shown in the following citation, might not be acted on and the delay caused could be substantial:
My husband suggested that he calls other women to come and assist. I declined; telling him that it was too early I had just started labour … and I thought to myself since I delivered on my own for the first pregnancy. Then why should I call people to assist me on this pregnancy? … on the third day I told my husband to take me to hospital. (FGD 15, W)
Reaching the stage where the woman no longer has the energy to continue on her own, she acknowledges failure and hands over the responsibility to others by calling for assistance, a process that was conducted in several steps:
… she first tries to push on her own but if she fails, she sends one of her kids to go and call a friend. If she also fails, they call a traditional birth attendant …. (FGD 4, M)
Exhausting traditional options
Once women in labour accepted failure and opened up for assistance, the first people they would call were friends or close female family members, the mothers-in-law, however, were not referred to in this context. This again revealed the desire by the women in labour to still have reservations to who can come to her assistance at the time of need. According to the informants, the number of women assisting could range from one to several, and the advices given were many and varied as shown in the following citation:
We would give her herbs, checking using fingers, everyone would have checked where the kid has reached, brought every herb they know … given it to her … some will give her hot strong tea and others telling her push … others say that they have touched the kid's hair, leg, after putting fingers into her. (FGD 1, W)
The options for managing obstructed labour further depended on what was presumed to be the cause of the obstruction. In case the diagnosis was ‘a hung/stuck pregnancy’, originally caused by using herbs to prevent recurrent abortions, then herbs to ‘release’ the pregnancy were administered. Further, if the pregnancy was perceived to ‘ascend’, a phenomenon observed during contractions, herbs that would make it ‘descend’ were given to the woman.
The informants further elaborated that when a traditional birth attendant or a wise woman was called to assist, she examines the position of the baby's head and thus determines whether the labour was progressing or not:
In case of a complication during labour a traditional birth attendant is called to assist and when she examines you and finds that you are not able to deliver with her assistance she advises you to be taken to hospital. (FGD 11, W)
Partner taking charge
The partners, usually the husbands, though in the vicinity of where the women give birth, only get involved when most of the options available locally to assist the women have been exhausted. This was interpreted as a process of actively taking over the decision making rather than passively being handed the responsibility:
It's your husband who takes care of everything because by that time you are very weak …. (FGD 9, W)
The components of this process, ‘searching for funds’ and ‘mobilising the community’, were related to the act of seeking care within the health system, a step that often proved to be complicated. According to the informants, most births occur in the community with no complications and obstructed labours would therefore find most women and their partners without any savings for referral purpose. The partners would initially approach friends and ask for financial support as indicated:
You can easily tell because if she has been giving birth from the village normally and now she has failed, you start thinking of what to do, you go and borrow from a friend. (FGD 4, M)
When close friends are unable to assist, the request for help is carried further to community members at large who then will comply, as they consider it their responsibility to assist a man who is in dire need of referring his wife due to a delivery that does not progress normally. In villages, which are remote and not accessible by vehicles assistance is provided by community members to carry the women on locally improvised stretchers to a place where vehicles can access:
When the husband comes and tells us that wife has failed to deliver, we cannot sit there doing nothing. You contribute money and transport the woman to hospital. If she has not over delayed we take her to the health centre. If they find that she is having severe complications the health centre refers her to Mbarara hospital. (FGD 2, M)
In case a vehicle has to be sourced from another village, the cost will be higher and unable to be met at the moment. In a situation like this, partners have no other option according to the informants but to resort to urgently seek loans from money lenders.
Facing challenging referral conditions
Informants regarded referral from the village to the hospital as a major undertaking to the family and to the community as a whole. However, the use of mobile phones had eased the communication between the villages and urban areas, which facilitated the connection between community members and vehicle drivers and/or owners. The availability of means to transport women with obstructed labour, however, depended on ‘time of the day’, ‘state of roads’ and the ‘location’ of the village.
Women whose labours were considered to be obstructed during daytime would find it easier and less costly to get means of transport as opposed to the women who faced a similar condition at night. Even when vehicles were identified they would come at an exorbitant cost. Informants explained that night travel is regarded as risky because of insecurity by robbers/thieves:
… me from my understanding most women start labour pains at night and when you call someone with a vehicle, so as to make things hard for you, they charge you very highly almost twice of what they charge during the day …. (FGD 14, M)
The location of the villages may also determine whether the women with obstructed labour can easily be transported to a place that provides comprehensive obstetric care. Informants indicated that some villages are inaccessible by virtue of their location in hilly areas, which makes access to these areas by vehicles difficult:
I called the traditional birth attendant (TBA) and she came and tried to assist by this time 3pm she was still trying. Then the TBA told me that the baby is in the pelvis and is stuck. She said the baby is big and cannot come out. The woman was already tired. We put her on a stretcher and brought her near the road. We waited for a vehicle, which we got in after an hour and then took her to Mbarara hospital. (FGD 16, M)
The informants also indicated that transporting women with obstructed labour from the villages to hospital depended on the state of the roads. During the rainy season some areas would be left with roads inaccessible to vehicles, which necessitated carrying the women on stretchers for long distances to reach the road:
In this village, the roads are bad, in the wet season, they are slippery, even a car cannot pass …. (FGD 12, M)
Enduring a non-responsive healthcare system
Mistrust towards the healthcare system emanated from past experiences by women who had given birth in health facilities or from relatives and/or friends who had accompanied women seeking care at health facilities. The informants focused particularly on ‘methods’ applied in treating the women and ‘attitudes’ exhibited by the healthcare workers. Furthermore, the physical state of health facilities, particularly the referral hospital was described as non-conducive for service seekers.
A major issue discussed among the informants was the rudeness of healthcare staff, particularly the midwives. According to the female informants, the rudeness was more hurtful as it was delivered by fellow women who should be familiar with the painful process of giving birth. It was further implied that the abusive environment was created to extract bribes from service seekers:
In the hospitals, midwives speak rudely. Even when you are there you are able to see that the way they treat women is not good. There are also a few who demand bribe …. (FGD 12, M)
Informants indicated that there is a belief in the villages that whenever women with any complicated labour are admitted in Mbarara hospital, which also serves as a teaching hospital, caesarean sections will be conducted on them for training purposes. This implied that caesarean sections were carried out on some women without justification:
What I commonly hear is that when there is training of health workers if you take a woman there, then she will be operated on, even if she was to deliver normally. (FGD 14, M)
The community, as described by the study informants, expected to find health facilities that could offer a favourable environment for maternal healthcare with basic supplies and drugs. The health centre level IVs, which were established to offer comprehensive emergency obstetric care services, however, end up referring all women with complications to hospitals. According to the informants this introduces another delay in the referral process for women with obstructed labour. Moreover the hospital has few overworked staff, is overcrowded and most of the time lack basic supplies. Attendants to women in labour are usually requested to purchase various supplies in town:
You cannot believe it when you arrive at the hospital, there are no delivery beds, people are so crowded … some women end up having child birth on the verandas and some may even lose their lives before seeing a doctor. (FGD 10, M)
Discussion
The major finding of this study was that women's desire to ‘protect their own integrity’, i.e. the core category of our conceptual model (Fig. 2) actually initiate a process that might end as an obstructed labour. This resembles the first step in the ‘three delays model’ described by Thaddeus and Maine (8), as the active decision to isolate one self does not facilitate the family's possibility to make a timely decision in case referral is required. Integrity, however, has another aspect, which is referred to as ‘formal relation to self’, where focus is more on what the individual determines as a valid decision. Calhoun (27) defines integrity as a social virtue and ‘a matter of a person's proper regard for their own best judgement’. The individual judgement may incidentally coincide with general opinion and practice in the community, as was the case in our study, where women's choice of solitary confinement appeared to be largely accepted. The protection of integrity, as described in our study, was clearly linked to trust in self and lack thereof in others. According to Hill and O'Hara (28), experts generally agree that trust is a mental state involving risk taking as it infer opening to others. Trust in self, on the other hand, points more to self-efficacy that is built through experiences, modelling, social persuasions and physiological factors as described by Bandura (29). By demonstrating faith in one's capability, women manage to protect themselves and their privacy.
Childbirth has social and cultural meanings (30) and a childbearing woman constructs her perceptions of the birthing experience (31). As indicated in our conceptual model, ‘women taking control of own birth process’ as the labour is expected to progress normally without problems. Similarly Kyomuhendo (32) reported from a study carried out in western and central Uganda that pregnancy and childbirth are the key areas where women still command power and respect. Janssen (33) reported from Niger that childbirth was regarded as a private and solitary affair and from the Bariba tribe in Benin, Sargent (34) found that solitary childbirth was viewed as a test of endurance. Even in high-income countries, where most of the deliveries are institutionalised, personal control during childbirth has been found to be an important factor for women's satisfaction (35). However, in the Ugandan context, solitary or home births are fraught with life threatening risks to the woman and her unborn child, as the majority of women will find themselves without help if labour becomes obstructed.
‘Reaching the limit – failing to give birth’ describe the stage where women realise that they cannot manage on their own. Several studies report that traditional birth attendants are first summoned to assist in cases where labour becomes prolonged (36–38); however, in our study we found that women preferred initially calling their female friends. Research on home births have found that husbands and/or mothers-in-law are in control of the birthing process (39, 40). According to Neema (41), strong influence of mothers-in-law during childbirth process was still a significant factor in Mbarara district in the early 1990s. In our study, however, we found that mothers-in-law were actually not mentioned as a source of support. This finding could be related to the change in the social fabric where young couples have been forced to live far from their parents due to land pressure or to seek better opportunities elsewhere.
‘Exhausting traditional options’ is the concept used in our model to encompass all the available traditional methods to assist a woman with obstructed labour. Administering herbs appeared to be particularly useful when, as the community expressed it, the ‘pregnancy ascended’ or ‘was hung’. Herbs are commonly used during pregnancy or childbirth in Uganda, and a recent study by Kamatenesi (42) indicated that in the neighbouring district of Bushenyi, herbs were used in 80% of childbirths. A community study in Nigeria showed that women were aware of obstructed labour as a complication of childbirth and the alternative mode of treatment available to them was use of traditional drugs (43). The alarming aspect is that the community's referral to a pregnancy that is ‘ascending’ or ‘hung’ may allude to imminent rupture of the uterus, a complication of obstructed labour that require immediate referral to a health facility that provides comprehensive emergency obstetric care. Applying herbs to ‘release’ the pregnancy will, in case it is an obstructed labour, subject the woman and her unborn child to the risk of dying. Actions aiming at solving the problem of obstructed labour within the community may ultimately prolong the first delay (8).
Research in Uganda (39, 40) argue correctly that partners/husbands are regarded as heads of households and consequently mainly involved in making decisions if a delivery turns complicated. However, we have not identified studies reporting that women intentionally withhold information that the labour process has initiated, as reported in our study. It is likely that a ‘partner taking charge’ when the birth process has turned into an emergency, experience anxiety and find it difficult to coordinate actions required for referral. Even if a partner of a pregnant woman sub-consciously might be prepared for any eventuality, the ethical aspect of withholding information, which leads to further delay, is seriously questioned. Thwala et al. (44) reported from Swaziland that childbirth is culturally considered to be the women's affair, a perception held by many cultures in Africa. However, active male involvement in all stages of pregnancy and labour has been promoted as one important strategy to improve maternal and neonatal outcome (45).
The community further ‘Face challenging referral conditions’, which alludes to the second delay, which was described by Thaddeus and Maine (8). Despite the extensive distribution of mobile phones within the community, which facilitate communication with vehicle owners or drivers for transport as well as communication with the hospital in cases of obstructed labour, aspects such as time of day, seasonal road conditions and location of dwelling delay women reaching the healthcare system once the decision has been taken to refer. Moreover, complications during childbirths usually find families not well prepared in terms of resources required to pay for the transport. Studies have, similarly to ours, found that long distance, unavailability of vehicles and poor states of roads are barriers to women reaching a facility which offers comprehensive obstetric care (17, 39) (40). The referral consequently becomes a great challenge as a result of the women and their partners being found unprepared in terms of resources needed for the referral. The availability of mobile phones needs to be exploited to improve community involvement in health service utilisation and referral services. The challenges described by the community in our study require a multi-sectoral approach. It is therefore important that maternal mortality and associated factors are shared not only with the Ministry of Health but also transport and road construction ministries. In Uganda, a master of public health programme in safe motherhood admits journalists, lawyers and politicians (46). By making use of competent human resources in a variety of areas, combined efforts may develop strategies, which involve actors at the individual, community and health system levels (Fig. 2).
The category ‘Enduring a non-responsive healthcare system’ emerged from the informants’ dislike of methods applied at the referral hospital as well as the attitudes experienced in encounters with healthcare workers. The latter were described as unwelcoming and authoritarian, and this negatively affected the integrity of women seeking obstetric emergency care, also reported by other researchers (39, 40). Caesarean sections are feared in most low-income countries because of cultural and social reasons (47–50). According to the perceptions of community members in our study, the frequent use of caesarean section was associated with training medical students. This corresponds to findings reported by Awonyika (47) from Nigeria who indicated that this belief was caused by inadequate information given by healthcare workers. Even if there is no time to explain prior to a surgery, information needs to be given once the woman is in a condition to absorb it. The risk is otherwise that negative feedback to the community will reinforce the process of ‘protecting own integrity’, as indicated in our model (Fig. 2).
Lack of supplies in hospitals further enhances the mistrust of women and their partners towards the healthcare system. By the time a referred woman and her next of kin reach a hospital, they have spent all funds available and little or nothing is left to buy the materials required by the labour ward. Public hospitals in Uganda are expected to be stocked with adequate supplies and also be free of charge but this is hardly the case. Amooti-Kaguna and Nuwaha, Merchant, Neema (39–41) have reported similar findings of inadequate supplies in Ugandan hospitals. The health system has not been able to adjust itself to the increased demands expected from a very rapidly rising population.
The mistrust in the health system, which traditionally has been regarded as a place for managing complicated labours, fortifies the negative feedback to the individual women and the community members. Eventually this may contribute to continued low use of maternity services and consequently high levels of maternal/neonatal morbidity and mortality.
Methodological considerations
Simple randomisation of rural and urban communities ensured that various parts of the district and consequently various set-ups of healthcare systems were represented in the study. The purposive selection of study informants, however, guaranteed that individuals familiar with the research topic were given an opportunity to voice their opinions. Though childbirth is largely taken as women's responsibility in Uganda, conducting FGDs with men alongside those of women provided us with an opportunity for data comparison. Views that were identified as being salient in women FGDs were probed for in subsequent FGDs with men and vice versa, thereby giving us an opportunity to validate our findings. All of the above are inherent methodological aspects of GT ensuring credibility of the findings presented. The research team, which consisted of maternal healthcare specialists as well as social scientists, looked at data through different lenses and questioned each other's interpretation until consensus was reached.
Conclusions and implications
There is urgent need to educate women, men and communities on the risks of having home or solitary childbirths which are not assisted by skilled attendants. Keeping partners unaware of an on-going childbirth process should be avoided as it reduces the possibility of timely action. The perception that childbirth is a woman's affair leaving men as bystanders needs to be changed through promoting male involvement in all stages; pregnancy, labour, childbirth, and postpartum. Establishment of women's groups where issues related to male involvement and optimal management of childbirth in the community can be discussed might be a way forward.
Having fully functional health centres offering comprehensive obstetric services closer to communities and streamlined referral system can help to create trust between women, families and the healthcare system. Women's integrity can be protected through having health workers who are compassionate, caring and therefore being able to support women during pregnancy, labour and child birth. Mobile phones have improved the community's’ ability to communicate in cases of obstructed labour, but challenges related to infrastructure require a multi-sectoral approach. Further testing of the conceptual model presented is recommended.
Acknowledgements
This study was funded by grants from Global Health Research Initiative (GHRI) and Swedish International Development Cooperation Agency (Sida). We extend our thanks to all women and men who participated in the study and their openness in the discussions. All authors (JK, P-OÖ, ME, PK, KOP) participated in the different phases of the study. JK was the principal investigator. JK and KOP participated in the conception and design of the study. JK and PK did primary data collection. JK and KOP conducted data analysis. JK wrote the first draft whereas the other authors (P-OÖ, ME, PK, KOP) made interpretations, reviews, and contributions towards developing the final manuscript.
Conflict of interest and funding
The authors have not received benefits from industry or elsewhere to conduct the study.
References
- 1.Morrison J, Tamang S, Mesko N, Osrin D, Shrestha B, Manandhar M, et al. Women's health groups to improve perinatal care in rural Nepal. BMC Pregnancy Childbirth. 2005 Mar 16;5:6. doi: 10.1186/1471-2393-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Manandhar DS, Osrin D, Shrestha BP, Mesko N, Morrison J, Tumbahangphe KM, et al. Effect of a participatory intervention with women's groups on birth outcomes in Nepal: cluster-randomised controlled trial. Lancet. 2004 Sep 11–17;364:970–9. doi: 10.1016/S0140-6736(04)17021-9. [DOI] [PubMed] [Google Scholar]
- 3.Rosato M, Laverack G, Grabman LH, Tripathy P, Nair N, Mwansambo C, et al. Community participation: lessons for maternal, newborn, and child health. Lancet. 2008 Sep 13;372:962–71. doi: 10.1016/S0140-6736(08)61406-3. [DOI] [PubMed] [Google Scholar]
- 4.WHO. Geneva: World Health Organization; 2005. The World health report: 2005: make every mother and child count. Available from: http://www.who.int/whr/2005/en/index.html [cited 15 October 2011] [DOI] [PubMed] [Google Scholar]
- 5.Neilson JP, Lavender T, Quenby S, Wray S. Obstructed labour. Br Med Bull. 2003;67:191–204. doi: 10.1093/bmb/ldg018. [DOI] [PubMed] [Google Scholar]
- 6.Konje JC, Ladipo OA. Nutrition and obstructed labor. Am J Clin Nutr. 2000 Jul;72(1 Suppl):291S–7S. doi: 10.1093/ajcn/72.1.291S. [DOI] [PubMed] [Google Scholar]
- 7.AbouZahr C. Global burden of maternal death and disability. Br Med Bull. 2003;67:1–11. doi: 10.1093/bmb/ldg015. [DOI] [PubMed] [Google Scholar]
- 8.Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Soc Sci Med. 1994 Apr;38:1091–110. doi: 10.1016/0277-9536(94)90226-7. [DOI] [PubMed] [Google Scholar]
- 9.Olsen OE, Ndeki S, Norheim OF. Complicated deliveries, critical care and quality in emergency obstetric care in Northern Tanzania. Int J Gynaecol Obstet. 2004 Oct;87:98–108. doi: 10.1016/j.ijgo.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 10.Olsen OE, Ndeki S, Norheim OF. Availability, distribution and use of emergency obstetric care in northern Tanzania. Health Pol Plan. 2005 May;20:167–75. doi: 10.1093/heapol/czi022. [DOI] [PubMed] [Google Scholar]
- 11.Hossain J, Ross SR. The effect of addressing demand for as well as supply of emergency obstetric care in Dinajpur, Bangladesh. Int J Gynaecol Obstet. 2006 Mar;92:320–8. doi: 10.1016/j.ijgo.2005.09.029. [DOI] [PubMed] [Google Scholar]
- 12.Douangphachanh X, Ali M, Outavong P, Alongkon P, Sing M, Chushi K. Availability and use of emergency obstetric care services in public hospitals in Laos PDR: a systems analysis. Biosci Trends. 2010 Dec;4:318–24. [PubMed] [Google Scholar]
- 13.UNICEF, WHO, UNFPA. New York: United Nations Children's Fund; Guidelines for monitoring the availability and use of obstetric services. 1997 October. Available from: http://www.childinfo.org/files/maternal_mortality_finalgui.pdf [cited 5 March 2011] [Google Scholar]
- 14.Konje JC, Obisesan KA, Ladipo OA. Obstructed labor in Ibadan. Int J Gynaecol Obstet. 1992 Sep;39:17–21. doi: 10.1016/0020-7292(92)90774-d. [DOI] [PubMed] [Google Scholar]
- 15.Melah GS, El-Nafaty AU, Massa AA, Audu BM. Obstructed labour: a public health problem in Gombe, Gombe State, Nigeria. J Obstet Gynaecol. 2003 Jul;23:369–73. doi: 10.1080/01443610310001119510. [DOI] [PubMed] [Google Scholar]
- 16.Gessessew A, Mesfin M. Obstructed labour in Adigrat Zonal Hospital, Tigray Region, Ethiopia. Ethiop J Health Dev. 2003;17:175–80. Available from: http://ajol.info/index.php/ejhd/article/viewFile/9837/31302 [cited 5 March 2011]. [Google Scholar]
- 17.Nwogu-Ikojo EE, Nweze SO, Ezegwui HU. Obstructed labour in Enugu, Nigeria. J Obstet Gynaecol. 2008 Aug;28:596–9. doi: 10.1080/01443610802281682. [DOI] [PubMed] [Google Scholar]
- 18.Ali AA, Adam I. Maternal and perinatal outcomes of obstructed labour in Kassala hospital. doi: 10.3109/01443611003672096. Sudan. J Obstet Gynaecol 2010 May; 30: 376–7. [DOI] [PubMed] [Google Scholar]
- 19.Mbonye AK, Asimwe JB, Kabarangira J, Nanda G, Orinda V. Emergency obstetric care as the priority intervention to reduce maternal mortality in Uganda. Int J Gynaecol Obstet. 2007 Mar;96:220–5. doi: 10.1016/j.ijgo.2006.12.017. [DOI] [PubMed] [Google Scholar]
- 20.UBOS, Macro International Inc. Calverton, Maryland, USA: UBOS and Macro International Inc; 2007. Uganda Demographic and Health Survey 2006. Available from: http://www.measuredhs.com/pubs/pub_details.cfm?ID=681&srchTp=advanced [cited 5 March 2011]. [Google Scholar]
- 21.Orach CG. Maternal mortality estimated using the Sisterhood method in Gulu district, Uganda. Trop Doct. 2000 Apr;30:72–4. doi: 10.1177/004947550003000205. [DOI] [PubMed] [Google Scholar]
- 22.Kabakyenga JK. Ostergren PO, Turyakira E, Mukasa PK, Pettersson KO. Individual and health facility factors and the risk for obstructed labour and its adverse outcomes in south-western Uganda. BMC Pregnancy Childbirth. 2011;11:73. doi: 10.1186/1471-2393-11-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Strauss A, Corbin J. Basics of qualitative research: techniques and procedures for developing grounded theory. 2nd ed. London: Sage Publications, Inc; 1998. [Google Scholar]
- 24.Barbour R, Kitzinger J. Developing focus group research: politics, theory, and practice. London: Sage Publications; 1999. [Google Scholar]
- 25.Mbarara District Local Government. Mbarara: Mbarara District Local Government; Five-year rolled District Development Plan 2011/2012–2015/2016. Unit P; 2011 March. [Google Scholar]
- 26.Dahlgren L, Emmelin M, Winkvist A, editors. Umea: Umea University; 2004. Qualitative methodology for international public health. [Google Scholar]
- 27.Calhoun C. Standing for something. J Philos. 1995 May 2005;92:235–60. Available from: http://links.jstor.org/sici?sici=0022-362X%28199505%2992%3A5%3C235%3ASFS%3E2.0.CO%3B2-G [cited 5 March 2011] [Google Scholar]
- 28.Hill C, O'Hara E. A cognitive theory of trust. University of Washington Law Review; 2006. Available from: http://lawreview.wustl.edu/inprint/84-7/HillOHara.pdf [cited 10 June 2011]
- 29.Bandura A. Self-eficacy: toward a unifying theory of behaviour change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 30.Callister LC. Cultural meanings of childbirth. J Obstet Gynecol Neonatal Nurs. 1995 May;24:327–31. doi: 10.1111/j.1552-6909.1995.tb02484.x. [DOI] [PubMed] [Google Scholar]
- 31.Campbell JC, Bunting S. Voices and paradigms: perspectives on critical and feminist theory in nursing. ANS Adv Nurs Sci. 1991 Mar;13:1–15. doi: 10.1097/00012272-199103000-00004. [DOI] [PubMed] [Google Scholar]
- 32.Kyomuhendo GB. Low use of rural maternity services in Uganda: impact of women's status, traditional beliefs and limited resources. Reprod Health Matters. 2003 May;11:16–26. doi: 10.1016/s0968-8080(03)02176-1. [DOI] [PubMed] [Google Scholar]
- 33.Janssen G. Solitary births in Tera Niger: a local quest for safety. In: Mirjam de Bruijn RvD, Gewald J., editors. Strength beyond structure: social and historical trajectories of agency in Africa. Leiden: Brill; 2007. pp. 240–82. [Google Scholar]
- 34.Sargent C. Obstetrical choice among urban women in Benin. Soc Sci Med. 1985;20:287–92. doi: 10.1016/0277-9536(85)90243-6. [DOI] [PubMed] [Google Scholar]
- 35.Goodman P, Mackey MC, Tavakoli AS. Factors related to childbirth satisfaction. J Adv Nurs. 2004 Apr;46:212–9. doi: 10.1111/j.1365-2648.2003.02981.x. [DOI] [PubMed] [Google Scholar]
- 36.Bergstrom S, Goodburn E. The role of traditional birth attendants in the reduction of maternal mortality. In: Lerberghe VDBaWV., editor. Safe motherhood strategies: a review of the evidence. Antwerp: ITG Press; 2001. pp. 77–95. [Google Scholar]
- 37.Starrs AM. Safe motherhood initiative: 20 years and counting. Lancet. 2006 Sep 30;368:1130–2. doi: 10.1016/S0140-6736(06)69385-9. [DOI] [PubMed] [Google Scholar]
- 38.Kamal IT. The traditional birth attendant: a reality and a challenge. Int J Gynaecol Obstet. 1998 Dec;63:43–52. doi: 10.1016/s0020-7292(98)00183-0. [DOI] [PubMed] [Google Scholar]
- 39.Amooti-Kaguna B, Nuwaha F. Factors influencing choice of delivery sites in Rakai district of Uganda. Soc Sci Med. 2000 Jan;50:203–13. doi: 10.1016/s0277-9536(99)00275-0. [DOI] [PubMed] [Google Scholar]
- 40.Merchant N. Edmonton: Alberta; 2010. Decision-making related to pregnancy and childbirth in Kabarole District, Western Uganda. Available from: http://hdl.handle.net/10048/1640 [cited 14 August 2011] [Google Scholar]
- 41.Neema S. Copenhagen: University of Copenhagen; 1994. Mothers and midwives: maternity care options in Ankole Southwestern Uganda. Available from: http://worldcat.org/oclc/51207146 [cited 15 June 2011] [Google Scholar]
- 42.Kamatenesi-Mugisha M, Oryem-Origa H. Medicinal plants used to induce labour during childbirth in western Uganda. J Ethnopharmacol. 2007 Jan 3;109:1–9. doi: 10.1016/j.jep.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 43.Asowa-Omorodion FI. Women's perceptions of the complications of pregnancy and childbirth in two Esan communities, Edo state, Nigeria. Soc Sci Med. 1997 Jun;44:1817–24. doi: 10.1016/s0277-9536(96)00291-2. [DOI] [PubMed] [Google Scholar]
- 44.Thwala SB, Jones LK, Holroyd E. Swaziland rural maternal care: ethnography of the interface of custom and biomedicine. Int J Nurs Pract. 2011 Feb;17:93–101. doi: 10.1111/j.1440-172X.2010.01911.x. [DOI] [PubMed] [Google Scholar]
- 45.Okechukwu OE, Adegbenro CO, Moses OO, Amos OT, Olanrenwaju OA. Men's involvement in safe motherhood. J Turkish-Germany Gynecol Assoc. 2007;8:240–6. [Google Scholar]
- 46.Uganda Christian University. Mukono: Uganda Christian University; 2011. Master of public health leadership – save the mothers. Available from: http://www.ucu.ac.ug/content/view/151/43 [cited 15 August 2011]. [Google Scholar]
- 47.Awoyinka BS, Ayinde OA, Omigbodun AO. Acceptability of caesarean delivery to antenatal patients in a tertiary health facility in south-west Nigeria. J Obstet Gynaecol. 2006 Apr;26:208–10. doi: 10.1080/01443610500508311. [DOI] [PubMed] [Google Scholar]
- 48.Fasubaa OB, Ogunniyi SO, Dare FO, Isawumi AI, Ezechi OC, Orji EO. Uncomplicated caesarean section: is prolonged hospital stay necessary? East Afr Med J. 2000 Aug;77:448–51. [PubMed] [Google Scholar]
- 49.Loto OM, Adewuya AO, Ajenifuja OK, Orji EO, Owolabi AT, Ogunniyi SO. The effect of caesarean section on self-esteem amongst primiparous women in South-Western Nigeria: a case-control study. J Matern Fetal Neonatal Med. 2009 Sep;22:765–9. doi: 10.3109/14767050902801660. [DOI] [PubMed] [Google Scholar]
- 50.Parkhurst JO, Rahman SA. Life saving or money wasting? Perceptions of caesarean sections among users of services in rural Bangladesh. Health Pol. 2007 Mar;80:392–401. doi: 10.1016/j.healthpol.2006.03.015. [DOI] [PubMed] [Google Scholar]