Abstract
Aims
The current guidelines recommend reperfusion therapy in acute myocardial infarction (AMI) with ST-segment elevation or left bundle branch block (LBBB). Surprisingly, the right bundle branch block (RBBB) is not listed as an indication for reperfusion therapy. This study analysed patients with AMI presenting with RBBB [with or without left anterior hemiblock (LAH) or left posterior hemiblock (LPH)] and compared them with those presenting with LBBB or with other electrocardiographic (ECG) patterns. The aim was to describe angiographic patterns and primary angioplasty use in AMI patients with RBBB.
Methods and results
A cohort of 6742 patients with AMI admitted to eight participating hospitals was analysed. Baseline clinical characteristics, ECG patterns, coronary angiographic, and echocardiographic data were correlated with the reperfusion therapies used and with in-hospital outcomes. Right bundle branch block was present in 6.3% of AMI patients: 2.8% had RBBB alone, 3.2% had RBBB + LAH, and 0.3% had RBBB + LPH. TIMI flow 0 in the infarct-related artery was present in 51.7% of RBBB patients vs. 39.4% of LBBB patients (P = 0.023). Primary percutaneous coronary intervention (PCI) was performed in 80.1% of RBBB patients vs. 68.3% of LBBB patients (P< 0.001). In-hospital mortality of RBBB patients was similar to LBBB (14.3 vs. 13.1%, P = 0.661). Patients with new or presumably new blocks had the highest (LBBB 15.8% and RBBB 15.4%) incidence of cardiogenic shock from all ECG subgroups. Percutaneous coronary intervention was done more frequently (84.8%) in patients with new or presumably new RBBB when compared with other patients with blocks (old RBBB 66.0%, old LBBB 62.3%, new or presumably new LBBB 73.0%). In-hospital mortality was highest (18.8%) among patients presenting with new or presumably new RBBB, followed by new or presumably new LBBB (13.2%), old LBBB (10.1%), and old RBBB (6.4%). Among 35 patients with acute left main coronary artery occlusion, 26% presented with RBBB (mostly with LAH) on the admission ECG.
Conclusion
Acute myocardial infarction with RBBB is frequently caused by the complete occlusion of the infarct-related artery and is more frequently treated with primary PCI when compared with AMI + LBBB. In-hospital mortality of patients with AMI and RBBB is highest from all ECG presentations of AMI. Restoration of coronary flow by primary PCI may lead to resolution of the conduction delay on the discharge ECG. Right bundle branch block should strongly be considered for listing in future guidelines as a standard indication for reperfusion therapy, in the same way as LBBB.
Keywords: Acute myocardial infarction, Right bundle branch block, Left bundle branch block, Primary angioplasty, Reperfusion
Introduction
Left bundle branch block (LBBB) and right bundle branch block (RBBB) in acute myocardial infarction (AMI) patients are well known to carry the high mortality risk.1,2 Nevertheless, the guidelines of the European Society of Cardiology (ESC) list only LBBB as an indication for urgent reperfusion therapy.3 The American Heart Association (AHA)/American College of Cardiology (ACC) guidelines provide similar recommendations.4 Thus, the current guideline-recommended electrocardiographic (ECG) indications for reperfusion therapy in AMI include ST-segment elevation (STE) and LBBB of new or unknown onset. It is not well known whether also new or unknown onset RBBB should be an indication for reperfusion therapy, especially in the modern era of primary percutaneous coronary intervention (PCI). The aim of this analysis was to investigate the coronary angiographic (CAG) findings, reperfusion therapies used, and in-hospital outcomes of patients with AMI presenting with RBBB when compared with those presenting with LBBB or with other ECG patterns.
Methods
Patients
A total of 6742 consecutive patients with AMI routinely admitted to eight participating tertiary hospitals during the study period of 3 years (2006–08) were retrospectively analysed. The patients were included in this retrospective registry based on (i) diagnosis of AMI and (ii) coronary angiography. Patients with AMI, who did not undergo coronary angiography (n = 650, i.e. 8.8% from all AMI patients), are not subject of this analysis. Baseline characteristics studied (age, sex, diabetes, previous myocardial infarction, Killip class on admission, etc.) are listed in Table 1.
Table 1.
Patients baselines characteristics
| STEMI | STDMI | LBBB | RBBB | Other ECG | P-value* | P-value** | |
|---|---|---|---|---|---|---|---|
| n = 6742 | 3447 | 907 | 291 | 427 | 1670 | ||
| Mean age (years) | 64.5 (12.4) | 69.5 (10.7) | 72.1 (10.1) | 69.8 (11.3) | 65.6 (11.4) | 0.005 | <0.001 |
| Females (%) | 31.2 | 34.6 | 38.1 | 23.2 | 31.6 | <0.001 | <0.001 |
| Diabetes (%) | 24.0 | 36.8 | 45.7 | 36.3 | 31.7 | 0.013 | <0.001 |
| Previous MI (%) | 13.8 | 29.2 | 38.1 | 25.8 | 29.7 | <0.001 | <0.001 |
| Killip class (mean) | 1.44 (0.85) | 1.47 (0.83) | 1.86 (1.06) | 1.71 (1.01) | 1.23 (0.62) | 0.050 | <0.001 |
| Killip I (%) | 72.6 | 70.5 | 51.2 | 57.9 | 84.5 | 0.134 | <0.001 |
| Killip II (%) | 17.0 | 16.0 | 24.6 | 24.1 | 9.9 | ||
| Killip III (%) | 3.7 | 9.1 | 11.1 | 6.9 | 3.3 | ||
| Killip IV (%) | 6.7 | 4.4 | 13.1 | 11.1 | 2.3 | ||
| Old BBB (%) | – | – | 26.7 | 26.5 | – | 0.508 | – |
| Unknown BBB (%) | – | – | 57.5 | 60.8 | – | ||
| New BBB (%) | – | – | 15.8 | 12.7 | – | ||
| QRS mean (ms) | – | – | 133.7 (19.6) | 133.4 (18.9) | – | 0.811 | – |
| BBB disappeared (%) | – | – | 14.2 | 18.8 | – | 0.193 | – |
| Median duration of the hospital stay | 5 | 6 | 5 | 7 | 4 | 0.001 | <0.001 |
Continuous data are expressed as mean values (standard deviation), categorical data are expressed as relative frequencies (percentage).
STEMI, ST elevation myocardial infarction; STDMI, ST depression myocardial infarction; LBBB, left bundle branch block; RBBB, right bundle branch block; ECG, electrocardiogram; MI, myocardial infarction; BBB, bundle branch block; QRS, QRS complex on ECG.
*P-value only applies to the comparison of LBBB vs. RBBB.
**P-values for the comparison of all five groups (null hypothesis: all five groups have the same characteristics).
Electrocardiographic patterns
Electrocardiographic reading was done by the treating cardiologist. Electrocardiograms from all patients with RBBB have been reviewed once more at the time of this manuscript preparation by another independent cardiologist. The patients were divided into the following subgroups based on the first (admission) ECG:
ST-segment elevation acute myocardial infarction (STEMI, n = 3447, i.e. 51.1%): persistent STEs in at least two contiguous leads (≥2 mm in the chest leads or ≥1 mm in the extremity leads),
ST-segment depression acute myocardial infarction (STDMI, n = 907, i.e. 13.5%): horizontal or descending ST-segment depressions in at least two contiguous leads (≥2 mm in the chest leads or ≥1 mm in the extremity leads),
acute myocardial infarction with LBBB, irrespective of any ST-segment deviations were present on ECG (LBBB-MI, n = 291, i.e. 4.3%): QRS ≥120 ms and LBBB shape,
acute myocardial infarction with RBBB, irrespective of any ST-segment deviations were present on ECG (RBBB-MI, n = 427, i.e. 6.3%) with subgroups of RBBB alone (2.8%), RBBB + left anterior hemiblock (LAH) (3.2%), RBBB + left posterior hemiblock (LPH) (0.3%): QRS ≥120 ms and RBBB shape, electrical axis extreme left (> −45°) for LAH, respectively, extreme right (> +105°) for LPH. In all RBBB patients, a special care was taken to describe the presence or absence of STEs and all ECGs were once more analysed by an independent cardiologist.
acute myocardial infarction with other ECG (other ECG-MI, n = 1670, i.e. 24.8%): any other ECG patterns (negative T waves, small ST shifts not fulfilling the above criteria, non-specific or even negative ECG).
The information whether any bundle branch block (BBB) is old, new, or unknown origin and whether BBB persisted or disappeared during the hospital stay was collected. Analyses in this manuscript are done with all RBBB (including bifascicular blocks) as one patient group (i.e. RBBB ± LAH or LPH).
Coronary angiography, reperfusion therapy, outcomes
Coronary angiographic or autopsy data were analysed to estimate the number of diseased major coronary arteries, to identify the infarct-related artery, and to analyse TIMI flow in the infarct-related artery before and after percutaneous coronary intervention (PCI, whenever it was performed). Coronary angiography was described by the interventional cardiologist, who performed the procedure. Pre-discharge echocardiographic ejection fraction was registered. Reperfusion therapies used during the initial hospital stay and in-hospital mortality were analysed.
Statistical analysis
For continuous variables, mean values and standard deviations were calculated. After checking normality by the Shapiro–Wilk test, Student's t-test was used for testing of the hypotheses about the means when two groups (RBBB and LBBB) were compared. The analysis of variance was used for comparison of more than two groups. The Mann–Whitney test was used for the ordinal variables. Categorical data were tested with the Fisher's exact test and Pearson's χ2-test and adjusted residuals were used to identify significantly different subcategories. The multiple logistic regression and Cox's proportional hazards models were used to adjust the differences among groups for confounding factors. Following factors and covariates were entered into model: age, gender, indicators of diabetes, and previous MI, Killip class. Odds ratio (OR), hazard ratio (HR), and corresponding 95% confidence intervals (95% CI) are presented as effect estimates. All tests have been performed as two-sided on the level of significance 0.05. Statistical software Stata, release 9.2 (Stata Corp LP, College Station, TX, USA) was used for the analysis.
Results
Coronary angiographic findings
TIMI flow 0 (Figure 1) in the infarct-related artery was present in 51.7% of RBBB patients vs. 39.4% of LBBB patients [OR = 1.64 (95% CI 1.14–2.32), P = 0.023; adjusted OR 1.76 (95% CI 1.31–2.53), P = 0.005]. Nearly 80% of RBBB patients had a complete or subtotal occlusion of the infarct-related artery (TIMI flow 0-2 was present in 79.6% of RBBB AMI patients). Furthermore, the distribution of TIMI flow grades among RBBB patients closely resembled the pattern seen among ST elevation group and this angiographic similarity between STEMI and RBBB was more distinct than between STEMI and LBBB (Table 2).
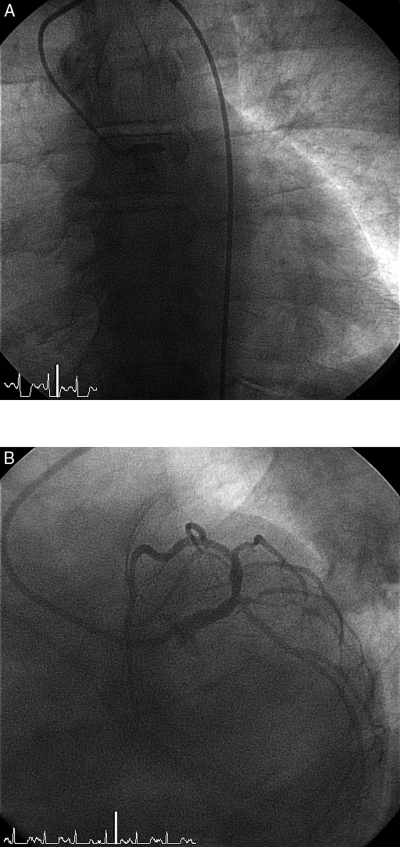
Figure 1.
(A) Complete (100%) thrombotic occlusion of the left main coronary artery. Anterior view. (B) The same patient after primary percutaneous coronary intervention with stent implantation. Left inferior oblique (spider) view.
Table 2.
Angiographic findings, reperfusion therapy, and outcomes
| STEMI | STDMI | LBBB | RBBB | Other ECG | P-value* | P-value** | |
|---|---|---|---|---|---|---|---|
| n= 6742 | 3447 | 907 | 291 | 427 | 1670 | ||
| No signif. CAD (%) | 0.8 | 0.1 | 2.2 | 2.2 | 2.6 | 0.214a | <0.001a |
| 1-VD | 37.3 | 17.2 | 21.3 | 27.8 | 29.1 | ||
| 2-VD | 28.2 | 19.9 | 28.3 | 30.1 | 27.5 | ||
| 3-VD | 30.0 | 53.1 | 41.9 | 35.5 | 35.1 | ||
| LM disease | 3.7 | 9.7 | 6.3 | 4.4 | 5.7 | ||
| IRA—LMCA (% from IRAs) | 1.1 | 6.0 | 5.8 | 3.5 | 2.3 | 0.281 | <0.001 |
| IRA-LAD | 45.0 | 31.5 | 43.8 | 48.5 | 42.7 | ||
| IRA-LCX | 14.0 | 37.5 | 22.1 | 17.2 | 24.0 | ||
| IRA-RCA | 39.1 | 21.2 | 25.8 | 28.9 | 27.5 | ||
| IRA-bypass | 0.8 | 3.8 | 2.5 | 1.9 | 3.5 | ||
| No PCI done (% of all) | 10.8 | 38.2 | 31.7 | 19.9 | 32.5 | <0.001 | <0.001 |
| Pre-PCI TIMI flow 0 (% from PCIs) | 57.3 | 22.5 | 39.4 | 51.7 | 20.5 | 0.023 | <0.001 |
| TIMI-1 | 8.4 | 5.9 | 8.0 | 8.6 | 6.7 | ||
| TIMI-2 | 18.8 | 24.7 | 23.9 | 19.3 | 19.5 | ||
| TIMI-3 | 15.5 | 46.9 | 28.6 | 20.4 | 53.3 | ||
| Post-PCI TIMI flow 0-1 (% from PCIs) | 4.4 | 3.8 | 9.6 | 7.0 | 4.2 | 0.409 | <0.001 |
| TIMI-2 | 6.4 | 1.7 | 7.5 | 10.0 | 2.4 | ||
| TIMI-3 | 89.2 | 94.5 | 82.9 | 83.0 | 93.4 | ||
| Reperfusion—none (%) | 10.9 | 30.2 | 29.0 | 17.7 | 28.9 | 0.002 | <0.001 |
| TL (%) | 0.4 | 0.0 | 0.3 | 0.5 | 0.0 | ||
| Primary PCI (%) | 88.1 | 61.8 | 68.3 | 80.1 | 67.5 | ||
| Acute CABG (%) | 0.6 | 8.0 | 2.4 | 1.7 | 3.6 | ||
| Mean EF (%) | 46.3 (12.0) | 50.1 (13.5) | 37.5 (12.7) | 42.4 (14.2) | 53.4 (13.1) | <0.001 | <0.001 |
| In-hospital mortality (%) | 5.4 | 6.3 | 13.1 | 14.3 | 2.9 | 0.661 | <0.001 |
Continuous data are expressed as mean values (standard deviation), categorical data are expressed as relative frequencies (percentage).
STEMI, ST elevation myocardial infarction; STDMI, ST depression myocardial infarction; LBBB, left bundle branch block; RBBB, right bundle branch block; ECG, electrocardiogram; CAD, coronary artery disease; 1-VD, single vessel disease; 2-VD, two vessel disease; 3-VD, three vessel disease; LM, left main; IRA, infarct related artery; LMCA, left main coronary artery; LAD, left anterior descending; LCX, left circumflex; RCA, right coronary artery; PCI, percutaneous coronary intervention; TIMI, thrombolysis in myocardial infarction; TL, thrombolysis; CABG, coronary artery bypass grafting; EF, ejection fraction.
aNone of CAD (no signif., 1,2,3-vessel) and LM disease categories differs significantly (all P> 0.05) in the comparison of LBBB vs. RBBB; all categories differ significantly (all P< 0.001) among five compared groups.
*P-value only applies to the comparison of LBBB vs. RBBB.
**P-values for the comparison of all five groups (null hypothesis: all five groups have the same characteristics).
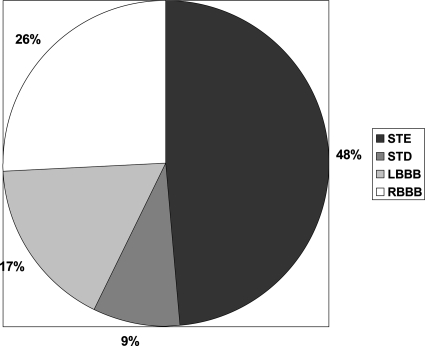
Left main coronary artery occlusion
Ninety-seven patients (1.4% of the entire study population) had left main, as the infarct-related, artery (Figure 2). In 35 of them, the left main coronary artery (LMCA) was functionally occluded (TIMI flow 0–2): most frequent ECG presentation pattern for LMCA occlusion was STE (n = 17), followed by RBBB [n = 9; with LAH in six patients (Figures 3 and 4) and without LAH in three patients], LBBB (n = 6), and ST-segment depression (n = 3). In other words, acute LMCA occlusion presents in 26% with RBBB, without STEs (Figure 5).
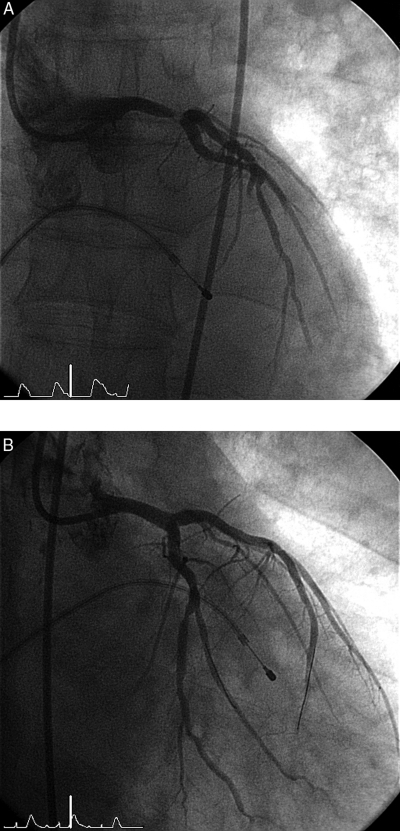
Figure 2.
(A) Subtotal (99%) left main coronary artery occlusion. Anterior view. (B) The same patient after primary percutaneous coronary intervention with two stents (kissing technique) implantation. Right inferior oblique view.
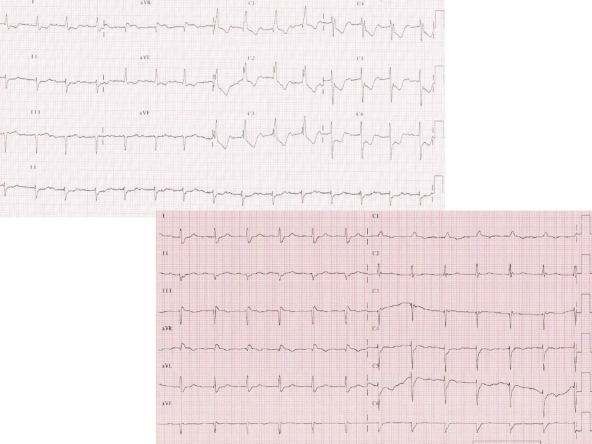
Figure 3.
Electrocardiography from two patients admitted in Killip class II-III with acute 100% occlusion of the left main coronary artery (A) and proximal dominant right coronary artery (B).
Figure 4.
Electrocardiographic from a 66-year-old male acute myocardial infarction patient with cardiogenic shock, subtotal left main coronary artery occlusion, and TIMI flow 2. Again, ST-segment elevation in V4–V5 is not typical and can easily be overlooked, while the dominant feature of this Electrocardiography is wide QRS complex deformed by RBBB + LAH.
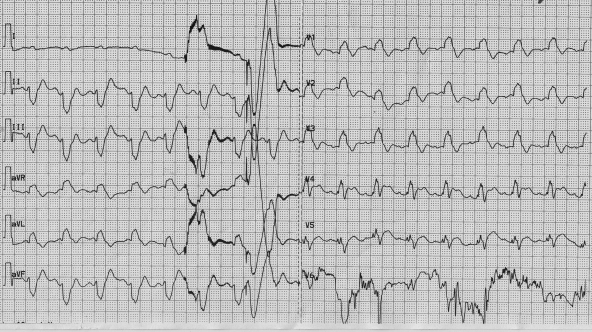
Figure 5.
Electrocardiographic findings among patients with acute myocardial infarction caused by the left main coronary artery occlusion.
Reperfusion therapies
Primary PCI was performed in 80.1% of RBBB patients vs. 68.3% of LBBB patients [OR = 1.88 (95% CI 1.33–2.64), P< 0.001; adjusted OR = 1.71 (95% CI 1.19–2.45), P = 0.004]. This difference was caused by the fact that fewer LBBB patients had CAG findings suitable for primary PCI (see Table 2 for details). In STEMI patients primary PCI was performed in 88.1%.
In-hospital outcomes
Despite the fact that RBBB patients were younger, had less frequent diabetes, less severe CAG findings, and less previous AMIs than LBBB patients, RBBB was related with a similar mortality as LBBB [14.3 vs. 13.1%, HR = 1.17 (95% CI 0.72–1.90), P = 0.630; adjusted HR = 1.33 (95% CI 0.80–2.21), P = 0.268] and was more than twice the mortality of STEMI [5.4%, HR = 2.11 (95% CI 1.45–3.07), P< 0.001; adjusted HR = 1.80 (95% CI 1.21–2.68), P = 0.004] and STDMI [6.3 %, HR = 2.49 (95% CI 1.70–3.64), P < 0.001; adjusted HR = 1.44 (95% CI 0.92–2.27), P = 0.108], respectively (Table 2).
Relation between in-hospital mortality and duration of the hospital stay
Even after taking the length of hospital stay into account, the conclusions concerning in-hospital mortality remain unchanged. We have tried the logistic regression model with length of hospital stay as a covariate and Cox's model. The overall test is significant (P-value for the comparison of all five groups P< 0.001). The comparison RBBB vs. LBBB yields P = 0.686, so the adjustment for length of stay brings only very small shift compared with the P-value presented in Table 2. The P-values for other contrasts involving RBBB group are: RBBB vs. STEMI P< 0.001, RBBB vs. STDMI P = 0.014, RBBB vs. other ECG P< 0.001. In fact, the median duration of hospital stay among the deceased patients was short (2 days for RBBB and 2.5 days for LBBB), confirming the clinical experience that vast majority of fatalities occurs within initial 48–72 h after hospital admission.
Bundle branch block onset time
Patients with BBBs were further divided according to the BBB onset time (Table 3): new or presumably new BBB (as this is the currently accepted indication for reperfusion therapy in LBBB) vs. BBB known to be old. Group of patients with new or presumably new RBBB (despite having the lowest mean age from all BBB subgroups) had high Killip class on admission (15.4% presenting with cardiogenic shock). TIMI flow 0 in the infarct-related artery was found in significantly more patients with new or presumably new RBBB (55%) than in other three subgroups (old RBBB 34.9%, old LBBB 28%, new or presumably new LBBB 41.1%). Percutaneous coronary intervention was performed in 84.8% of patients with new or presumably new RBBB, more than in other three subgroups (old RBBB 66%, old LBBB 62.3%, new or presumably new LBBB 73%). The most striking are mortality differences between these four subgroups: in-hospital mortality was highest (18.8%) among patients presenting with new or presumably new RBBB, followed by new or presumably new LBBB (13.2%), old LBBB (10.1%), and old RBBB (6.4%).
Table 3.
Bundle branch block onset time
| LBBB old | LBBB new or unknown onset | RBBB old | RBBB new or unknown onset | P-value | |
|---|---|---|---|---|---|
| % from all patients | 1.1 | 3.2 | 1.7 | 4.6 | |
| Mean age (years) | 71.1 (10.0) | 71.4 (10.1) | 72.2 (9.9) | 69.3 (11.5) | 0.004 |
| Killip class (mean) | 1.68 (0.98) | 1.94 (1.10) | 1.45 (0.77) | 1.88 (1.10) | 0.001 |
| Killip IV (%) | 8.8 | 15.8 | 4.3 | 15.4 | 0.011 |
| BBB disappeared (%) | 1.6 | 19.4 | 6.8 | 23.2 | <0.001 |
| Pre-PCI TIMI flow 0 (% from PCIs) | 28.0 | 41.1 | 34.9 | 55.0 | <0.001 |
| No PCI done (% of all) | 37.7 | 27.0 | 34.0 | 15.2 | <0.001 |
| Reperfusion—none (%) | 33.3 | 24.3 | 31.9 | 12.5 | <0.001 |
| Primary PCI (%) | 62.3 | 73.0 | 66.0 | 84.8 | |
| Mean EF (%) | 37.3 | 37.8 | 43.4 | 41.5 | 0.003 |
| In-hospital mortality (%) | 10.1 | 13.2 | 6.4 | 18.8 | 0.015 |
Disappearence of bundle branch block during the hospital stay
In 87 patients, the BBB (present on the admission ECG) disappeared during the hospital stay. Almost all these patients had BBB of new or unknown onset and they mostly presented to hospital with acute heart failure (mean Killip class was 1.93, cardiogenic shock was present in 19%, 86% were treated by primary PCI, which was successful in 98%). Left bundle branch block disappeared in 32 patients and their mortality was 6.2%. Right bundle branch block disappeared in 55 patients and their mortality was 12.7%.
Bifascicular blocks
Patients, in whom RBBB was combined with either LAH or LPH tended to be older, had higher incidence of diabetes, had lower ejection fraction, more frequent occurrence of three-vessel disease and LAD as an infarct-related artery, and had slightly higher mortality (Table 4).
Table 4.
Right bundle branch block with/without left anterior/posterior hemiblock
| RBBB alone | RBBB + LAH | RBBB + LPH | P-value | |
|---|---|---|---|---|
| % from all patients | 2.8 | 3.2 | 0.3 | |
| Mean age (years) | 68.4 (11.6) | 71.0 (11.2) | 70.8 (9.0) | 0.119 |
| Female (%) | 22.4 | 25.4 | 23.5 | 0.827 |
| Diabetes (%) | 30.9 | 36.1 | 29.4 | 0.588 |
| Previous MI (%) | 22.4 | 26.0 | 47.1 | 0.089 |
| Killip class (mean) | 1.69 (0.98) | 1.59 (0.93) | 1.41 (0.80) | 0.414 |
| Killip I (%) | 57.6 | 36.9 | 70.6 | 0.754 |
| Killip II (%) | 26.5 | 21.1 | 23.5 | |
| Killip III (%) | 5.3 | 7.2 | 0.0 | |
| Killip IV (%) | 10.6 | 7.8 | 5.9 | |
| No signif. CAD (%) | 2.1 | 2.5 | 0.0 | 0.935 |
| 1-VD | 28.5 | 27.5 | 17.7 | |
| 2-VD | 30.5 | 26.2 | 29.4 | |
| 3-VD | 34.7 | 39.4 | 52.9 | |
| LM disease | 4.2 | 4.4 | 0.0 | |
| IRA—LMCA (% from IRAs) | 3.8 | 5.0 | 0.0 | 0.006 |
| IRA-LAD | 39.4 | 51.4 | 38.5 | |
| IRA-LCX | 16.7 | 20.0 | 23.0 | |
| IRA-RCA | 40.1 | 19.3 | 38.5 | |
| IRA-bypass | 0.0 | 4.3 | 0.0 | |
| Pre-PCI TIMI flow 0 (% from PCIs) | 53.5 | 48.5 | 44.5 | 0.870 |
| TIMI-1 | 8.5 | 9.7 | 0.0 | |
| TIMI-2 | 17.1 | 21.6 | 22.2 | |
| TIMI-3 | 20.9 | 20.2 | 33.3 | |
| Post-PCI TIMI flow 0-1 (% from PCIs) | 6.4 | 3.7 | 22.2 | 0.205 |
| TIMI-2 | 8.8 | 11.1 | 0.0 | |
| TIMI-3 | 88.8 | 85.2 | 77.8 | |
| No PCI done (% of all) | 18.7 | 20.1 | 52.9 | 0.008 |
| Reperfusion—none (%) | 18.0 | 17.7 | 47.1 | 0.014 |
| TL (%) | 0.0 | 0.0 | 0.0 | |
| Primary PCI (%) | 81.3 | 79.9 | 47.1 | |
| Acute CABG (%) | 0.7 | 2.4 | 5.8 | |
| Mean EF (%) | 44.9 (13.5) | 42.1 (13.4) | 41.2 (18.0) | 0.189 |
| In-hospital mortality (%) | 10.5 | 14.8 | 17.7 | 0.438 |
Right bundle branch block and ST-segment elevations
ST-segment elevations (as defined in the methods section) were recognizable on electrocardiograms of 226 (53%) RBBB patients, while in 201 (47%) of patients presenting with AMI and RBBB no STEs could be found. TIMI flow 0-2 was found on emergent coronary angiography among 135 (67%) patients with RBBB and no STEs and 205 (91%) of those who had RBBB and STEs.
Discussion
Outcomes of acute myocardial infarction patients with bundle branch block
Historically, the mortality of patients with AMI and RBBB before the thrombolytic era reached 77%.5 A more recent study from Denmark still revealed the highest mortality of AMI among patients with BBB (left or right): 33.3% patients died in-hospital and 54.8% were dead at 1 year.6 In the study of Dubois et al.,7 patients with BBB (both left and right) had more complications and higher Killip class on admission. Both in-hospital mortality (32 vs. 10%, P < 0.001) and 3-year mortality (37 vs. 18%, P < 0.001) were higher among patients with complete BBB. In one study of 1238 consecutive patients with AMI,8 RBBB was found in 10.9% of patients. It was newly diagnosed in 37.8%, was known to be old in 34.1%, and in 28.1% the time of RBBB origin could not be established. Right bundle branch block patients had 1-year mortality 40.7 vs. 17.6% mortality in patients without RBBB (P< 0.001). Mortality was significantly higher for new RBBB (43.1%, P< 0.001) than for old (15.5%) and indeterminate (15.3%) RBBB. For isolated RBBB vs. bifascicular block, early mortality was 14.4 vs. 40.6%, and 1-year mortality was 30.2 vs. 54.2% (P< 0.05 for both). Multivariate analysis showed an independent prognostic value of RBBB for early and 1-year mortality.
Bundle branch block onset time
In the usual clinical reality (at the time of decision for urgent CAG procedure), BBB frequently cannot be securely established as new or old. Thus, patients without information about previous ECG are described as ‘BBB of unknown origin’ and were evaluated together with patients in whom previous ECG did not show BBB.
Right bundle branch block in the guidelines
The ESC and AHA/ACC guidelines3,4 were discussed in the introduction part. These guidelines surprisingly do not list new (or unknown) onset RBBB as an indication for reperfusion therapy. Interestingly, the guidelines of the American College of Emergency Physicians for the management of patients with suspected AMI or unstable angina9 recommend reperfusion therapy in presence of any type of BBB. This recommendation is based on the GISSI10 and ISIS-2 studies.11 Also the Czech Society of Cardiology guidelines from 200912 recommend primary PCI strategy for all patients with new (or presumably new) BBB (left or right).
Bundle branch blocks and thrombolysis
The absolute mortality reduction from thrombolysis was greatest among patients presenting with any BBB (−4.9%), followed by anterior STE (−3.7%), ST elevation ‘other’ (−2.8%), ST depression (−1.4%), and ST elevation inferior (−0.9%).13 The analysis of the GUSTO 1 and TAMI 9 cohorts14 found that left anterior descending (LAD) artery infarcts account for 54% of all new BBBs and among anterior infarcts RBBB was more common (13%) than LBBB (7%). Thrombolytic therapy reduced mortality among patients with both BBBs (left and right).
Bundle branch blocks and primary percutaneous coronary intervention
Kurisu et al. 15 in patients with anterior myocardial infarction found significantly higher 30-day mortality in patients with RBBB compared with those without RBBB (14.0 vs. 1.9%, P< 0.01). The study of Kleeman et al.16 found that patients presenting with RBBB had higher in-hospital (26 vs. 11%, P< 0.001) and post-discharge (19 vs. 9.2%, P< 0.001) mortality than patients without RBBB. After adjustment for differences in baseline characteristics, RBBB remained an independent predictor of increased mortality. Sakakura et al.17 retrospectively analysed a group of 25 patients with AMI caused by the LMCA occlusion. The in-hospital mortality was 60%. Logistic regression analysis found RBBB as an independent predictor of mortality. Hirano et al. 18 found that 37% of patients with AMI caused by the LMCA occlusion present with RBBB, while only 3% with LBBB. We have shown that acute LMCA occlusion presents in 26% only with RBBB without STEs (Figure 5) being in close accordance both to previously mentioned reports and with Hirano et al., who found that in 30% of LMCA occlusions no STE could be found on the admission ECG, while RBBB with left axis deviation (frequently accompanied by ST-elevation in aVR) is typical for this catastrophic type of AMI. Another study19 found RBBB even in 52% of patients with acute occlusion of the LMCA.
In the PAMI trials,20 patients with LBBB (1.6%) on presenting electrocardiogram were compared with patients who had RBBB (3.1%) or no BBB (95.3%). In-hospital mortality was highest with LBBB 14.6%, followed by RBBB 7.4% and no BBB 2.8% (P < 0.0001).
Right bundle branch block and ST-segment shifts/Q waves
Some authors2,21 request for the diagnosis of AIM with RBBB other ECG changes (e.g. ST-segment elevations) to be present, while this is not the case for LBBB (where it is generally accepted that LBBB masks ST-segment shifts). Right bundle branch block is thought not to mask the repolarization phase changes or Q waves, therefore other ECG changes have to be present to conclude the diagnosis of AIM. However, others22 warn before this ‘clear-cut’ opinion pointing out that minor ST elevations in the anterior leads (V1–V4) can be missed due to compensation by pseudo-normalization of the negative T waves. Our experience showed that even in large infarcts (caused by left main or proximal LAD coronary artery occlusion) bifascicular block (RBBB + LAH or rarely RBBB + LPH) may occur without typical STEs and thus a large life threatening AMI might be missed when ST elevations are required. Authors of this study repeatedly experienced mistakes in the clinical decision making in the real life practice, when patients with ischaemic symptoms and new or presumably new RBBB (but without STEs) were neither referred to urgent coronary angiography ± PCI nor treated by thrombolysis, sometimes with catastrophic consequences. This bad experience was the actual trigger for this study.
It has been also shown that interpretation of Q-waves can be tricky in the presence of RBBB.23 Gussak et al.24 showed that RBBB after myocardial infarction shortened Q wave duration, thus enabling false-negative diagnosis of inferior myocardial infarction. Also the term ‘RBBB-dependent Q-wave’ was introduced by Rosenbaum et al.,25 who described appearance of new Q waves in leads V1–V2 that disappeared after restoration of normal conduction. Thus false-positive and false-negative diagnosis of myocardial infarction can be made when describing ECG with RBBB in suspicion of myocardial infarction.
Study limitations
The main study limitation is a retrospective character of analysis. However, all participating centres enrol AMI patients to their own or nationwide registries, thus minimizing the risk of losing a subject from analysis. Another limitation relates to the fact that coronary angiography analysis was not performed in a core lab and by blinded manner. However, we have analysed ‘real life’ data similar to other registries published and this is not a comparison of different treatment approaches.
Conclusions
Acute myocardial infarction with new or presumably new RBBB on the admission ECG is frequently related with complete occlusion of the infarct-related artery and with primary PCI treatment when compared with AMI + LBBB. In-hospital mortality of patients with AMI and new or presumably new RBBB (especially when the block is bifascicular) is highest from all ECG presentations of AMI. Restoration of coronary flow by primary PCI may lead to resolution of RBBB on the discharge ECG.
New or presumably new RBBB (±LAH or LPH) should be listed in future guidelines as a standard indication (possibly class I, level C) for reperfusion therapy, in the same way as LBBB, i.e. irrespective of the presence or absence of ST-segment denivelations.
Funding
This study was partially supported by the Charles University Prague research project nr. MSM0021620817. Funding to pay the Open Access publication charges for this article was provided by the Charles University Prague (Third Faculty of Medicine, MSM0021620817).
Conflict of interest: none declared.
References
- 1.Ross JC, Dunning AJ. Right bundle branch and left axis deviation in acute myocardial infarction. Br Heart J. 1970;32:847–851. doi: 10.1136/hrt.32.6.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wong CK, Stewart RAH, Gao W, French JK, Raffel C, White HD for the Hirulog and Early Reperfusion or Occlusion (HERO-2) Trial Investigators. Prognostic differences between different types of bundle branch block during the early phase of acute myocardial infarction: insights from the Hirulog and Early Reperfusion or Occlusion (HERO)-2 trial. Eur Heart J. 2006;27:21–28. doi: 10.1093/eurheartj/ehi622. [DOI] [PubMed] [Google Scholar]
- 3.Van de Werf F, Bax J, Betriu A, Blomstrom-Lundqvist C, Crea F, Falk V, Filippatos G, Fox K, Huber K, Kastrati A, Rosengren A, Steg PG, Tubaro M, Verheugt F, Weidinger F, Weis M, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Aguirre FV, Al-Attar N, Alegria E, Andreotti F, Benzer W, Breithardt O, Danchin N, Di Mario C, Dudek D, Gulba D, Halvorsen S, Kaufmann P, Kornowski R, Lip GY, Rutten F. Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J. 2008;29:2909–2945. doi: 10.1093/eurheartj/ehn416. [DOI] [PubMed] [Google Scholar]
- 4.Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC, Jr, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK. ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction. A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2004;44:671–719. doi: 10.1016/j.jacc.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 5.Gould L, Venkataraman K, Mohhamad N, Gomprecht RF. Prognosis of right bundle-branch block in acute myocardial infarction. JAMA. 1972;219:502–503. [PubMed] [Google Scholar]
- 6.Terkelsen CJ, Lassen JF, Nørgaard BL, Gerdes JC, Jensen T, Gøtzsche LB, Nielsen TT, Andersen HR. Mortality rates in patients with ST-elevation vs. non-ST-elevation acute myocardial infarction: observations from an unselected cohort. Eur Heart J. 2005;26:18–26. doi: 10.1093/eurheartj/ehi002. [DOI] [PubMed] [Google Scholar]
- 7.Dubois C, Pierard LA, Smeets JP, Foidart G, Legrand V, Kulbertus HE. Short and long-term prognostic importance of complete bundle-branch block complicating acute myocardial infarction. Clin Cardiol. 1988;11:292–296. doi: 10.1002/clc.4960110504. [DOI] [PubMed] [Google Scholar]
- 8.Melgarejo-Moreno A, Galcerá-Tomás J, Garcia-Alberola A, Valdés-Chavarri M, Castillo-Soria FJ, Mira-Sánchez E, Gil-Sánchez J, Allegue-Gallego J. Incidence, clinical characteristics, and prognostic significance of right bundle-branch block in acute myocardial infarction. A study in the thrombolytic era. Circulation. 1997;96:1139–1144. doi: 10.1161/01.cir.96.4.1139. [DOI] [PubMed] [Google Scholar]
- 9.American College of Emergency Physicians. Clinical policy: critical issues in the evaluation and managent of adult patients presenting with suspected acute myocardial infarction or unstable angina. Ann Emerg Med. 2000;35:521–544. doi: 10.1067/mem.2000.106387. [DOI] [PubMed] [Google Scholar]
- 10.GISSI (Gruppo Italiano per lo Studio della Streptochinasi nell'Infarto miocardico) Effectivness of intravenous thrombolytic treatment in acute myocardial infarction. Lancet. 1986;1:397–402. [PubMed] [Google Scholar]
- 11.ISIS-2 (Second International Study of Infarct Survival) Collaborative Group. Randomised trial of intraveous streptokinase, oral aspirin, both or neither among 17 187 cases of suspected acute myocardial infarction: ISIS-2. Lancet. 1988;2:349–360. [PubMed] [Google Scholar]
- 12.Widimský P, Hlinomaz O, Kala P, Jirmář R. Diagnostika a léčba akutního infarktu myokardu s elevacemi ST. Cor Vasa. 2009;51:724–740. [Google Scholar]
- 13.Fibrinolytic Therapy Trialists Collaborative Group. Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Lancet. 1994;343:311–322. [PubMed] [Google Scholar]
- 14.Newby KH, Pisano E, Krucoff MW, Green C, Natale A. Incidence and clinical relevance of the occurrence of bundle-branch block in patients treated with thrombolytic therapy. Circulation. 1996;94:2424–2428. doi: 10.1161/01.cir.94.10.2424. [DOI] [PubMed] [Google Scholar]
- 15.Kurisu S, Inoue I, Kawagoe T, Ishihara M, Shimatani Y, Hata T, Nakama Y, Kijima Y, Kagawa E. Right bundle-branch block in anterior acute myocardial infarction in the coronary intervention era: acute angiographic findings and prognosis. Int J Cardiol. 2007;116:57–61. doi: 10.1016/j.ijcard.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 16.Kleemann T, Juenger C, Gitt AK, Schiele R, Schneider S, Senges J, Darius H, Seidl K MITRA PLUS Study Group. Incidence and clinical impact of right bundle branch block in patients with acute myocardial infarction: ST elevation myocardial infarction versus non-ST elevation myocardial infarction. Am Heart J. 2008;156:256–261. doi: 10.1016/j.ahj.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 17.Sakakura K, Kubo N, Hashimoto S, Ikeda N, Funayama H, Hirahara T, Sugawara Y, Yasu T, Ako J, Kawakami M, Momomura S. Determinants of in-hospital death in left main coronary artery myocardial infarction complicated by cardiogenic shock. J Cardiol. 2008;52:24–29. doi: 10.1016/j.jjcc.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 18.Hirano T, Tsuchiya K, Nishigaki K, Sou K, Kubota T, Ojio S, Kawasaki M, Minatoguchi S, Fujiwara H, Ueno K, Hosokawa H, Morita N, Nagano T, Suzuki T, Watanabe S. Clinical features of emergency electrocardiography in patients with acute myocardial infarction caused by left main trunk obstruction. Circ J. 2006;70:525–529. doi: 10.1253/circj.70.525. [DOI] [PubMed] [Google Scholar]
- 19.Kurisu S, Inoue I, Kawagoe T, Ishihara M, Shimatani Y, Nakamura S, Yoshida M, Mitsuba N, Hata T. Electrocardiographic features in patients with acute myocardial infarction associated with left main coronary artery occlusion. Heart. 2004;90:1059–1060. doi: 10.1136/hrt.2003.026799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guerrero M, Harjai K, Stone GW, Brodie B, Cox D, Boura J, Grines L, O'Neill W, Grines C. Comparison of the prognostic effect of left versus right versus no bundle branch block on presenting electrocardiogram in acute myocardial infarction patients treated with primary angioplasty in the primary angioplasty in myocardial infarction trials. Am J Cardiol. 2005;96:482–488. doi: 10.1016/j.amjcard.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 21.Thygesen K, Alpert JS, White HD Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction. Universal definition of myocardial infarction. Eur Heart J. 2007;28:2525–2538. doi: 10.1093/eurheartj/ehm355. [DOI] [PubMed] [Google Scholar]
- 22.Di Chiara A. Right bundle branch block during the acute phase of myocardial infarction: modern redefinitions of old concepts. Eur Heart J. 2006;27:1–2. doi: 10.1093/eurheartj/ehi552. [DOI] [PubMed] [Google Scholar]
- 23.Gussak I, Wright RS, Kopecky SL. Should we revise our diagnostic methods for Q-wave myocardial infarction in the presence of right bundle branch block? Am Heart J. 2000;140:10–11. doi: 10.1067/mhj.2000.106913. [DOI] [PubMed] [Google Scholar]
- 24.Gussak I, Zhou SH, Rautaharju P, Bjerregaard P, Stocke K, Osada N, Yokoyama Y, Miller M, Islam S, Chaitman BR. Right bundle branch block as a cause of false-negative ECG classification of inferior myocardial infarction. J Electrocardiol. 1999;32:279–284. [PubMed] [Google Scholar]
- 25.Rosenbaum MB, Girotti LA, Lazzari O, Halpern MS, Elizari MV. Abnormal Q waves in right sided chest leads provoked by onset of right bundle branch block in patients with anteroseptal infarction. Br Heart J. 1982;47:227–232. doi: 10.1136/hrt.47.3.227. [DOI] [PMC free article] [PubMed] [Google Scholar]