Abstract
Objectives
We examined health care disparities in Korean urban homeless people and individual characteristics associated with the utilization of health care.
Methods
We selected a sample of 203 homeless individuals at streets, shelters, and drop-in centers in Seoul and Daejeon by a quota sampling method. We surveyed demographic information, information related to using health care, and health status with a questionnaire. Logistic regression analysis was adopted to identify factors associated with using health care and to reveal health care disparities within the Korean urban homeless population.
Results
Among 203 respondents, 89 reported that they had visited health care providers at least once in the past 6 months. Twenty persons (22.5%) in the group that used health care (n = 89) reported feeling discriminated against. After adjustment for age, sex, marital status, educational level, monthly income, perceived health status, Beck Depression Inventory score, homeless period, and other covariates, three factors were significantly associated with medical utilization: female sex (adjusted odds ratio [aOR, 15.95; 95% CI, 3.97 to 64.04], having three or more diseases (aOR, 24.58; 95% CI, 4.23 to 142.78), and non-street residency (aOR, 11.39; 95% CI, 3.58 to 36.24).
Conclusions
Health care disparities in Seoul and Daejeon homeless exist in terms of the main place to stay, physical illnesses, and gender. Under the current homeless support system in South Korea, street homeless have poorer accessibility to health care versus non-street homeless. To provide equitable medical aid for homeless people, strategies to overcome barriers against health care for the street homeless are needed.
Keywords: Health care, Health care disparity, Health status, Homeless persons
INTRODUCTION
In the Republic of Korea (hereafter Korea), more than 5000 people are estimated to be homeless each year. The number of homeless people has increased in urban areas after the economic crisis in Korea. The main causes of homelessness were unemployment and recession [1]. The increased number of homeless people shocked Korean society and became a major social problem, including in the public health sector. The lifestyle of homelessness is hazardous to health. Homelessness, itself, can be recognized as a health risk factor [2]; it affects health through poor hygiene, lack of social support, and limitation of essential resources for life as a human being [3]. As a result, the health status of homeless people is generally poor, with increased prevalence of chronic diseases and increased mortality [4-9]. Common health problems of the homeless population include alcoholism; chronic diseases such as hypertension, diabetes, and hepatitis; and infectious diseases such as syphilis and tuberculosis. In Korea, similar findings have been identified; the estimated standardized mortality rate of male homeless people was about 2 times higher than that of the general male population during 1998 to 2005 [10].
Although poor health status in the homeless population is unquestioned, health care services, as a coping measure to prevent aggravation of poor health status, are not adequately provided in diverse settings [3]. Poor accessibility to health care for homeless people can be explained by financial and nonfinancial barriers [11]. To decrease the financial barriers, securing health services utilization through a social protection system is essential. A study done in the United States found that only 43% of homeless people who participated in the National Survey of Homeless Assistance Providers and Clients had health insurance. Having health insurance was associated with significantly higher probabilities of using ambulatory health care and inpatient hospitalization. Also, it was associated with lower probabilities of reporting barriers to needed care [12]. Among nonfinancial barriers, lack of transportation to health facilities, long waiting times in clinics, and the feeling of being stigmatized by health care professionals are frequently reported by homeless people [2,13].
Concerning the association of homelessness and health care, many studies have focused on the homeless population as a vulnerable group with regard to health care, but few studies have reported disparities in using health care within this population [14]. Although the fact that the entire homeless population is underserved in the health care sector is obvious, this knowledge is essential for targeting the most needy subgroup among homeless people. Among studies that documented health care disparities within the homeless population, the following variables have been found to be highly associated with disparities: health insurance status, race, age, physical health status, mental health status, and experience of violence [11,14,15].
In Korea, several studies have been performed to investigate the poor health status and deprived health care utilization of homeless people. However, prior studies have focused on the homeless population from a medical perspective [6,7,9]. Few studies have dealt with health security of the homeless population. Concerning health care utilization of the homeless, two studies presented exclusion experiences of homeless people in health care services [3,16]. Exclusion from health care includes discrimination, a feeling of being stigmatized, a poorly organized referral system from shelters to health care facilities, and poor quality care. Despite these findings about exclusion from health care services, factors associated with health care utilization by Korean homeless people have not been comprehensively explored. Moreover, health care disparities within the Korean homeless population have not previously been identified. In this study, we aimed to identify disparities in health care utilization of Korean urban homeless people using survey data to test the following hypothesis: Do health care disparities exist within the Korean urban homeless population?
METHODS
I. Data Collection
The survey was conducted in two cities, Seoul and Daejeon, from April 1 to May 14, 2011. A questionnaire designed for this study was used. This study is a part of the "Fusion Study on Homeless in Korea" funded by the Brain Fusion Program of Seoul National University (hereafter SNU). To determine eligibility, we adopted a definition of homelessness from "law for welfare and self-supporting of homeless" established in 2011: "Homeless refers to a person without regular habitation who uses shelters for the homeless or places not appropriate for residence during a considerable period." Eligible individuals for the study were those who could communicate well with an investigator and offer information about their socioeconomic status, health care utilization, health security level, and other factors. Participants had to reside in the street, shelters, or drop-in centers in Seoul and Daejeon. Each participant provided information by interview with a questionnaire. The investigators who interviewed participants were staff members of shelters and drop-in centers or volunteer workers from a civil group. To improve the response rate and accuracy of responses, we educated interviewers on our survey design, the attitude of investigation, and the aim of each question. Homeless people who participated in this survey were rewarded with 5000 Korean Won (KRW) for their participation. The reasons why the two cities were picked as the survey area were to avoid making inferences from a single area and to evaluate comparability between two areas.
II. Measures
A. Demographic characteristics
All participants were asked to report their gender, marital status, birth date, educational level, religion, whether they had a job, income level, reason for being homeless, whether they recognized their current status as homelessness, and social security status.
B. Health status.
To measure current health status of participants, we adopted questions from European Quality of Life (EUROQOL) and the Community Health Survey (CHS) of the Korean Center for Disease Control [17]. In the set of questions developed by EUROQOL, perceived health status and quality of life are measured. In the set of questions developed for the CHS, current morbidity from chronic diseases using "experience of having a disease diagnosed by a doctor" is evaluated. The chronic diseases include hypertension, diabetes, stroke, tuberculosis, hepatitis, depression, arthritis, angina pectoris, and myocardial infarction.
C. Mental health status.
To assess the mental health status of participants, we adopted the Beck Depression Inventory (BDI) in our questionnaire. The BDI was developed by Beck to screen for depression and has been applied in community and clinical settings [15]. It consists of 21 questions that measure cognitive, emotional, and physical aspects of depression, and items in each question are presented as a Likert scale. We used the Korean edition translated by Lee and Song [18]. We classified participants using 22 points as a cutoff value [19]. In this classification, a person who scored more than 22 points on the BDI was included in the high-risk group for depression.
D. Access to health care and utilization.
We assessed accessibility and utilization of health care in the past 6 months using questions adopted from the questionnaire of the Korea Health Panel [18]. This set of questions asks the reason for visits to a health care provider in terms of disease entity: respiratory diseases, pulmonary tuberculosis, hepatobiliary diseases except hepatitis, hepatitis, gastrointestinal diseases, musculoskeletal diseases, dermatologic diseases, neurologic diseases, dental diseases, and others. Also, it assesses the health care facilities visited in the past 6 months (no use, free clinics for the homeless, community health centers, private clinics, public hospitals, teaching hospitals, charity hospitals, others), the number of visits to health care providers in the past 6 months (hospitalization, ambulatory care, emergency department), whether respondents experience the feeling of being discriminated against by health care professionals, and whether they perceive the discrimination as a determinant of differences in their course of treatment.
E. Health security.
In the section on health security, we asked all participants about their current status in securing health care. Also, participants were asked which system they joined (National Health Insurance or Medicaid), and whether they pay for a contribution to health insurance.
III. Sampling Methods
A sample size calculation is needed to determine the number of participants. For this, we used nationwide homelessness data from the Ministry of Welfare and Health [20]. In these data, 5463 people were estimated to have been homeless in 2009. Although civil groups have pointed out the underestimation of homelessness in these data, no alternative exists for estimating the number of homeless people who reside in the street, shelters, and drop-in centers. Using this value, 360 participants were deemed to be a representative sample of the Korean homeless population.
For selection of participants, a quota sampling method is considered more suitable for the Korean homeless population than random sampling. Random sampling can be used in a setting with accurate data on the study population. Homeless people are hard to follow, and no precise and nationwide statistical data have been collected on the homeless population in Korea until now. Although quota sampling has a weakness on representativeness, we used this sampling method. In quota sampling, a criterion is needed to allocate each quota. In 2009 data, the ratio of street versus non-street homeless was determined to be 1:2.5. Therefore, we segmented the study population into street homeless and non-street homeless using this ratio.
IV. Statistical Analysis
After the survey, we could gather data on 247 participants. Two participants who did not provide demographic information were excluded from the analytic data set. In another 42 participants, responses to questions needed for this analysis were missing. Consequently, 203 responses were used in this analysis.
To test our main hypothesis, we analyzed relationships between measures related to socioeconomic status as independent variables and the utilization of health care in the recent 6 months with a univariate logistic regression. After that, to correct for other covariates, a multivariate logistic regression was performed. In this questionnaire, utilization data for health care for each homeless person were gathered separately for emergency services, inpatient services, and outpatient services. We surveyed the frequency of visits to health care facilities for each type of service. We summed all visits for each participant and distinguished these data as 0 or 1 or more. For example, if a participant had not visited any health care service in the recent 6 months, this person was classified in the 'not-used group'. Otherwise, the participant was classified in the 'used group'. The conventional p-value of 0.05 was used for all tests of significance.
Participants provided written informed consent. The study design and questionnaire were approved by the Institutional Review Board of Seoul National University.
RESULTS
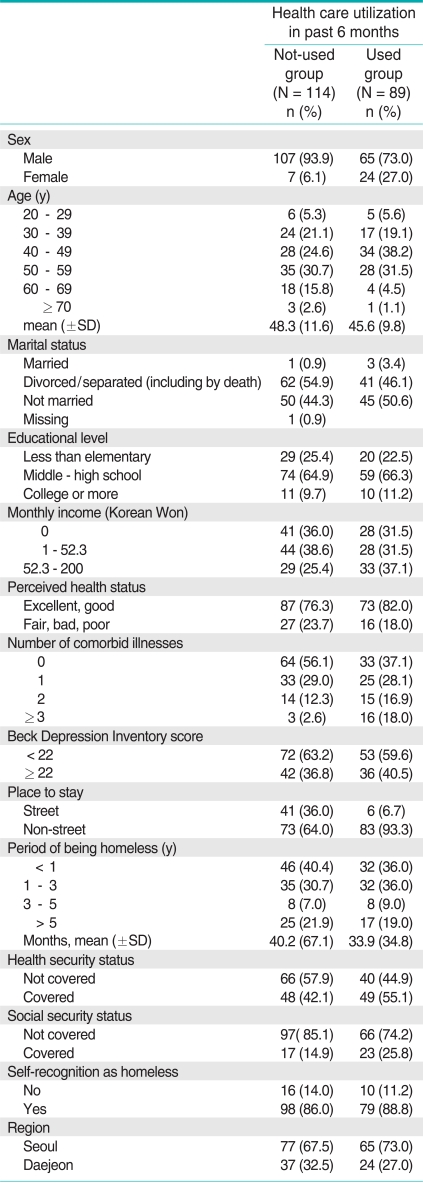
Characteristics of the 203 study participants are shown in Table 1. Descriptive analysis was performed to separate participants into a 'not-used group' versus a 'used group.' On average, participants in the not-used group reported a lifetime duration of homelessness of 40.2 months compared to 33.9 months in the used group. The difference in duration was not statistically significant in a t-test. In terms of "place to stay," 36% in the not-used group were street homeless, as were 6% in the used group. This difference had significance in the chi-square test (p < 0.000). In the health status section, 23.7% of not-used respondents answered that they recognized their health as 'fair', 'bad', 'poor'. Participant's chronic disease morbidity was estimated by disease diagnosis experience. We counted the number of morbidities of each participant and categorized them by number of comorbidities (0, 1, 2, 3, or more). In the notused group, 56.1% reported that they did not have any other diseases. In contrast, 37.1% of the used group reported no other diseases. Also, only 3% of the not-used group reported three or more other diseases compared to 16% of the used group. In the mental health section, 36.8% of the not-used group scored higher than 22 points on the BDI, as did 40.5% in the used group. The concordance rate between place to stay at present and place to stay in the last 6 months is noteworthy. Our questionnaire was designed to investigate the "place to stay" of each participant, separating "at present" and "in the last 6 months." From these data, we classified responses into street versus non-street and calculated a kappa coefficient. The kappa coefficient between street and non-street place to stay was 0.80 (95% CI, 0.70 to 0.90). So, we selected "place of stay at present" as a criterion to separate participants.
Table 1.
Characteristics of the study sample (n = 203)
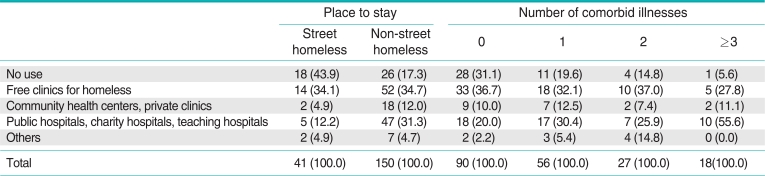
Table 2 shows the results for the question "which health care provider did you visit most in the past 6 months?" among participants. Among the street homeless, the most frequent answer was "no use" (43.9%), and after that, "others" (22.2%) and "public hospitals, charity hospitals, teaching hospitals" (12.2%). Among the non-street homeless, "free clinics for the homeless" (34.7%) and "public hospitals, charity hospitals, teaching hospitals" (31.3%) were the most common answers. We also compared the main type of visited health facilities for each subgroup classified by the number of comorbid illnesses. Participants who had fewer than two illnesses mainly visited "free clinics for the homeless"; those with more than three illnesses mainly visited "public hospitals, charity hospitals, teaching hospitals."
Table 2.
Most frequently visited health care facilities in past 6 months (n = 191)
In questions asking about participants' feeling of being discriminated against in health care services, 20 persons (22.5%) in the group that had used health care (n = 89) reported a feeling of being discriminated against. Among them, 11 persons stated that this kind of discrimination influenced their treatment. We distinguished persons who responded that they felt discriminated against by health care services based on the type of health facility. Among these persons, eight persons (42%) visited "free clinics for the homeless," five persons (26%) visited "public hospitals," and three persons (16%) visited "others." One person did not answer this question.
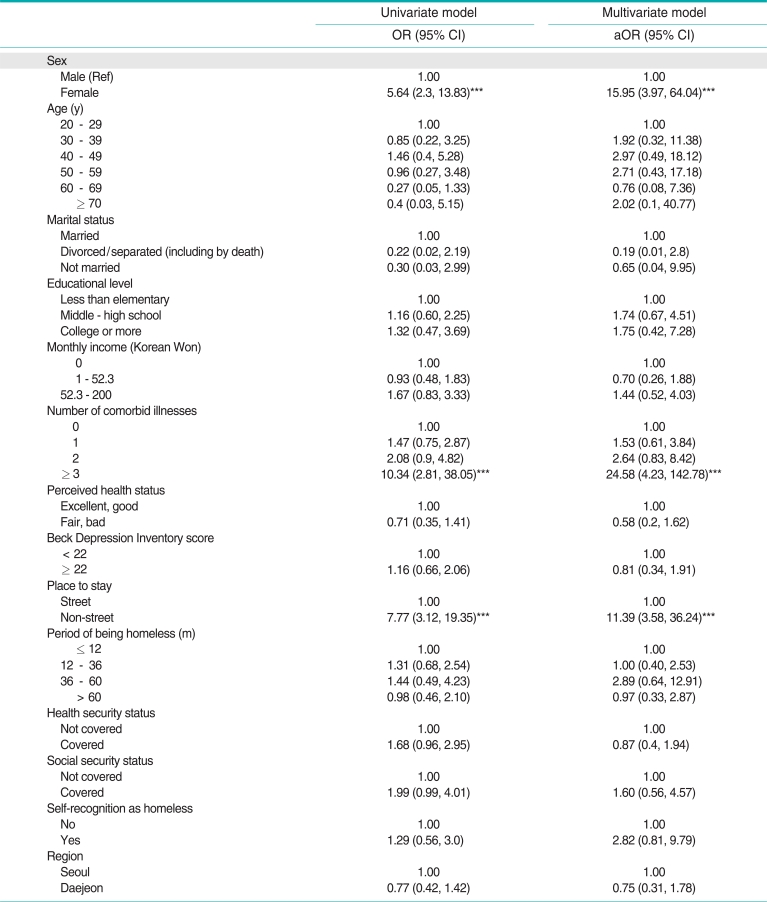
As shown in Table 3, three factors were found to be significantly associated with medical utilization in a univariate analysis. After correction for other covariates, the same three variables were still significantly associated with medical utilization: female gender (adjusted odds ratio (aOR, 15.95; 95% CI, 3.97 to 64.04], having three or more diseases (aOR, 24.58; 95% CI, 4.23 to 142.78), and non-street place to stay (aOR, 11.39; 95% CI, 3.58 to 36.24). The following factors were associated with a trend toward medical utilization but did not reach significance at the p < 0.05 level: educational level (middle-high school, college or more), monthly income (52.3 to 200 KRW), social security recipient, and persons who recognized themselves as homeless.
Table 3.
Factors associated with health care utilization in the past 6 months (n = 203)
OR: odds ratio, CI: confidence interval, aOR: adjusted odds ratio.
+p < 0.1, *p < 0.05, **p < 0.01, ***p < 0.001.
DISCUSSION
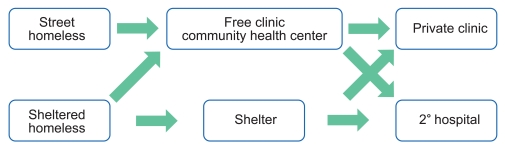
In this study, we analyzed data from a cross-sectional survey of homeless adults in two cities. From this analysis, we can conclude that health care disparities exist within the homeless population. Health care disparities among the homeless population have been described in other studies [12,14,15]. Socioeconomic status of the homeless was consistently found to influence their utilization of health care. In a multivariate analysis, three variables were highly associated with health care utilization among homeless people: female gender, three or more comorbid illnesses, and main place to stay. The variable "main place to stay" (street vs. non-street) was newly identified as a factor influencing utilization in this study. Contrary to the other identified variables, main place to stay negatively influenced homeless people who face a poorer status. This result can be explained by the current homeless support system in Korea. Figure 1 is a scheme expressing the current health care referral system for the homeless. As shown in Figure 1, non-street homeless people (mostly shelter homeless) can use health facilities through a transfer note issued by the shelter. A person who has obtained a transfer note can visit private clinics and public hospitals in the delivery network. In contrast, street homeless must visit free clinics or community health centers to be referred to the higher delivery system.
Figure 1.
Current health care referral system for the homeless.
Concerning the high concordance rate between the main place to stay at present and within 6 months, we can first conclude that the main place to stay for each homeless person becomes permanent. This may cause a vicious cycle of poor health and homelessness. Long-term fixed residency in the street may deprive an individual of the chance to use appropriate health care services. Also, residential type is a very important issue regarding the protection of homeless people and their freedom to choose their own shelter or house. Although this result may support the shelterization of all homeless, compulsory policy implementation can raise human rights issues, but unlike other variables, this variable is a changeable one and it is also related to the social norms or solutions to the homeless issue. This finding emphasizes the need for more equitable health care service provision within the homeless population based on need. Second, female homeless people were found to be more likely than male homeless people to use health care services. This result is consistent with prior studies [21-24]. Because we did not measure diseases and health care services that are specific to women, this result was not corrected for these diseases. To explain this finding, several factors such as differences in somatic morbidities, a higher frequency of mental distress versus males, and health-reporting behavior have been suggested in prior studies [25-27]. As shown in the multivariate analysis, this result was adjusted for the BDI screening result, perceived health status, and the number of estimated comorbidities. The higher odds ratio of using health care services among female homeless people may suggest the possibility of other unique factors related to homelessness. Third, in a multivariate analysis, those with three or more comorbid illnesses were more likely to have received health care services in the prior 6 months versus those who had fewer than three comorbid illnesses. This finding is consistent with a study that analyzed a representative homeless population in the United States [12]. In that study, comorbid illness status was highly associated with the use of ambulatory care by homeless people. This result can be explained by the need factor in a behavioral model for vulnerable populations [28]. In this model of access to health care, the need factor includes perceptions and evaluated need. The variable we measured to estimate morbidity in this survey can be recognized as quasi-morbidity. In further investigations, this result should be confirmed by "real" morbidity.
Our study demonstrates disparities in utilization of health care among homeless people. Disparities in using health care services among homeless people should be considered when developing a more equitable support system for the homeless population. Street homeless use health care much less than non-street homeless. The current medical referral system for homeless people is more focused on non-street homelessness, although the entire homeless group is underserved in health care. To increase health care accessibility of the street homeless, a policy that supports the most vulnerable subgroup in a vulnerable population is needed. A higher probability of using health care in women compared to men was revealed in this study, a finding consistent with prior studies. A homeless person who has three or more chronic diseases has a higher odds ratio of utilizing health care. In conclusion, health disparities in the Seoul and Daejeon homeless populations exist in terms of the main place to stay, physical illnesses, and gender.
Several limitations of this study should be noted. To set eligibility, we adopted a definition of homelessness from law. According to the definition, "homeless" can include various settings. For clear-cut separation, we only surveyed three subgroups of the homeless population: street, shelter, and drop-in center. Although homeless people face diverse situations, only these three subgroups of the homeless population were studied. The sample used for analysis was not selected by a probability sampling method. Moreover, the eligibility criteria may have excluded homeless people in poorer status from our study, thus causing selection bias. Individual characteristics and information related to using health care services were determined on the basis of self-report. Although it is subjective, prior research that validated homeless persons' self-reports of health care utilization found that they were only slightly less accurate in their reporting than the population at large [29]. Although a survey is an easier way to obtain information related to accessibility, perceived health need has its own limitations in terms of subjectivity [30]. For accurate investigation of health care utilization and disparities, an analysis should be performed based on the medical records of the homeless population [31]. Qualitative methods can be utilized to identify the barriers that hinder use of health care services by homeless people.
The questionnaire used in this survey included a question asking the number of visits to health care facilities. However, the sample size was not sufficient to be analyzed by a counted-number analysis method such as the Poisson regression model. Therefore, we cannot analyze the information on the frequency of use of medical services. The total frequency of visiting health facilities was summed and classified to 0 or 1 or more. For example, people who had only one hospitalization were not distinguished from those with several. Further study with a larger sample of homeless people should be made to confirm our results. In addition, the designed questionnaire was not fully applicable to homeless women, which limited the interpretation of information related to homeless women. Finally, the cross-sectional study design that we used limits the ability to assess the causal relationships between individual characteristics and utilization of health care services.
Footnotes
The authors have no conflicts of interest with the material presented in this paper.
This article is available at http://jpmph.org/.
References
- 1.Ha SK, Lee SW. IMF and the crisis of the marginalized urban sector in Korea. J Contemp Asia. 2001;31(2):196–213. [Google Scholar]
- 2.Lewis JH, Andersen RM, Gelberg L. Health care for homeless women. J Gen Intern Med. 2003;18(11):921–928. doi: 10.1046/j.1525-1497.2003.20909.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jeong WO, Kim SM, Nam KC, Jang KS, Jun HG, Jung EI, et al. Homeless human rights report. Seoul: National Human Rights Commission of Korea; 2005. pp. 335–361. (Korean) [Google Scholar]
- 4.Hwang SW. Is homelessness hazardous to your health? Obstacles to the demonstration of a causal relationship. Can J Public Health. 2002;93(6):407–410. doi: 10.1007/BF03405026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hibbs JR, Benner L, Klugman L, Spencer R, Macchia I, Mellinger A, et al. Mortality in a cohort of homeless adults in Philadelphia. N Engl J Med. 1994;331(5):304–309. doi: 10.1056/NEJM199408043310506. [DOI] [PubMed] [Google Scholar]
- 6.Song HJ, Cho CH, Kang JH, Hwang WS, Han HK. Health status and behavior of homeless in Seoul. J Korean Acad Fam Med. 2000;21(3):357–366. (Korean) [Google Scholar]
- 7.Yoo IS, Lee SW. Study on actual state and disposition of homeless patients in an emergency center. J Korean Soc Emerg Med. 2002;13(2):169–174. (Korean) [Google Scholar]
- 8.Kim DH, You EY, Jung SK, Rhee JE, Suh GJ, Youn YK. The clinical analysis of the homeless visiting emergency medical centers. J Korean Soc Emerg Med. 2002;13(3):294–299. (Korean) [Google Scholar]
- 9.Park HS, Lyu SJ. A study on the health status among the homeless in shelters. J Korean Acad Community Health Nurs. 2004;15(4):655–665. (Korean) [Google Scholar]
- 10.Lee TJ, Rho DM, Nam KC, Jeong WO, Ju YS, Kim SM, et al. Evaluation on homeless support and improvement. Seoul: Korea Institute for Health and Social Affairs (KIHASA); 2009. pp. 109–137. (Korean) [Google Scholar]
- 11.Hwang SW, Ueng JJ, Chiu S, Kiss A, Tolomiczenko G, Cowan L, et al. Universal health insurance and health care access for homeless persons. Am J Public Health. 2010;100(8):1454–1461. doi: 10.2105/AJPH.2009.182022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285(2):200–206. doi: 10.1001/jama.285.2.200. [DOI] [PubMed] [Google Scholar]
- 13.Wen CK, Hudak PL, Hwang SW. Homeless people's perceptions of welcomeness and unwelcomeness in healthcare encounters. J Gen Intern Med. 2007;22(7):1011–1017. doi: 10.1007/s11606-007-0183-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Teruya C, Longshore D, Andersen RM, Arangua L, Nyamathi A, Leake B, et al. Health and health care disparities among homeless women. Women Health. 2010;50(8):719–736. doi: 10.1080/03630242.2010.532754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brown RT, Kimes RV, Guzman D, Kushel M. Health care access and utilization in older versus younger homeless adults. J Health Care Poor Underserved. 2010;21(3):1060–1070. doi: 10.1353/hpu.0.0344. [DOI] [PubMed] [Google Scholar]
- 16.Shim MY. A study on the exclusion of the homeless from the public health service and the development of the state of lethargy [dissertation] Seoul: Sogang University; 2007. (Korean) [Google Scholar]
- 17.Korea Centers for Disease Control and Prevention (KCDC) 2010 community health survey questionnaire guideline. Seoul: KCDC; 2010. pp. 75–105. (Korean) [Google Scholar]
- 18.Lee YH, Song JY. A study of the reliability and the validity if the BDI, SDS, and MMPI-D scales. Korean J Clin Psychol. 1991;10(1):98–113. (Korean) [Google Scholar]
- 19.Shin MS, Kim ZS, Park KB. The cut-off score for the Korean version of beck depression inventory. Korean J Clin Psychol. 1993;12(1):71–81. (Korean) [Google Scholar]
- 20.Yoon HY. Research about the factors of prolonging duration of homelessness [dissertation] Seoul: University of Seoul; 2007. (Korean) [Google Scholar]
- 21.Koopmans GT, Lamers LM. Gender and health care utilization: the role of mental distress and help-seeking propensity. Soc Sci Med. 2007;64(6):1216–1230. doi: 10.1016/j.socscimed.2006.11.018. [DOI] [PubMed] [Google Scholar]
- 22.Green CA, Pope CR. Gender, psychosocial factors and the use of medical services: a longitudinal analysis. Soc Sci Med. 1999;48(10):1363–1372. doi: 10.1016/s0277-9536(98)00440-7. [DOI] [PubMed] [Google Scholar]
- 23.Choi SH, Cho Y. Sex differentials in the utilization of medical services by marital status. Korea J Popul Stud. 2006;29(2):143–166. (Korean) [Google Scholar]
- 24.Corney RH. Sex differences in general practice attendance and help seeking for minor illness. J Psychosom Res. 1990;34(5):525–534. doi: 10.1016/0022-3999(90)90027-2. [DOI] [PubMed] [Google Scholar]
- 25.Verbrugge LM. The twain meet: empirical explanations of sex differences in health and mortality. J Health Soc Behav. 1989;30(3):282–304. [PubMed] [Google Scholar]
- 26.Lahelma E, Martikainen P, Rahkonen O, Silventoinen K. Gender differences in illhealth in Finland: patterns, magnitude and change. Soc Sci Med. 1999;48(1):7–19. doi: 10.1016/s0277-9536(98)00285-8. [DOI] [PubMed] [Google Scholar]
- 27.Hankin BL, Abramson LY. Development of gender differences in depression: an elaborated cognitive vulnerability-transactional stress theory. Psychol Bull. 2001;127(6):773–796. doi: 10.1037/0033-2909.127.6.773. [DOI] [PubMed] [Google Scholar]
- 28.Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273–1302. [PMC free article] [PubMed] [Google Scholar]
- 29.Gelberg L, Siecke N. Accuracy of homeless adults' self-reports. Med Care. 1997;35(3):287–290. doi: 10.1097/00005650-199703000-00008. [DOI] [PubMed] [Google Scholar]
- 30.Cunningham PJ, Hadley J, Kenney G, Davidoff AJ. Identifying affordable sources of medical care among uninsured persons. Health Serv Res. 2007;42(1 Pt 1):265–285. doi: 10.1111/j.1475-6773.2006.00603.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hu SI, Kim MG, Lee SH, Kim SJ. Policy options to tackle unmet health needs. Seoul: KIHASA; 2009. pp. 15–20. (Korean) [Google Scholar]