Abstract
Objective
This study investigated the relationship between family functioning and performance on two tasks of emotion recognition (emotional prosody and face emotion recognition) and a cognitive control procedure (the Flanker task) following paediatric traumatic brain injury (TBI) or orthopaedic injury (OI).
Methods
A total of 142 children (75 TBI, 67 OI) were assessed on three occasions: baseline, 3 months and 1 year post-injury on the two emotion recognition tasks and the Flanker task. Caregivers also completed the Life Stressors and Resources Scale (LISRES) on each occasion. Growth curve analysis was used to analyse the data.
Results
Results indicated that family functioning influenced performance on the emotional prosody and Flanker tasks but not on the face emotion recognition task. Findings on both the emotional prosody and Flanker tasks were generally similar across groups. However, financial resources emerged as significantly related to emotional prosody performance in the TBI group only (p = 0.0123).
Conclusions
Findings suggest family functioning variables—especially financial resources—can influence performance on an emotional processing task following TBI in children.
Keywords: Children, traumatic brain injury, family functioning, emotional prosody, face emotion, social cognition
Introduction
Traumatic brain injury (TBI) is one of the most common injuries leading to disability in children [1, 2]. Among the myriad deficits, significant difficulties with social interaction are common following head injury and can become some of the most challenging, long-term difficulties faced by children and their families [3–11]. At the same time, TBI often drastically increases family burden and can result in long-term family dysfunction [12]. This latter finding is critical when considering social dysfunction following paediatric TBI because research with typically-developing children demonstrates a link between family context (such as discipline practices, parent–child attachment, parental socialization and the marital relationship) and the development of emotional regulation and social interaction [13–19].
Studies of childhood TBI survivors underscore the interactions between recovery of social skills, behavioural dysfunction and quality-of-life and the family environment [11, 12, 20–29]. For example, Yeates et al. [11, 28] showed that children sustaining a severe TBI who lived in stable family environments faired better in terms of social reasoning and behavioural outcomes both in the short-term (6 and 12 months post-injury) and long-term (an average of 4 years post-injury) when compared to children residing in families with limited resources or significant family turmoil. In a subsequent investigation, Taylor et al. [29] suggested that the interactions between family environment and recovery from TBI are actually reciprocal (e.g. disability following injury influences the family environment, but the family environment also influences the extent of disability).
Caregiver specific factors have also been associated with overall family burden as well as outcomes following paediatric TBI. A study by Wade et al. [30] indicated that parental social resources—described as the support from friends and/or the extent to which a spouse, friends or extended family could be counted on to help out—were crucial factors in reducing long-term family burden regardless of initial level of stress. Aitken et al. [31] investigated the relationship between a child’s quality-of-life following TBI and caregiver reported burden. The authors reported that those children with relatively lower quality of life scores following their TBI had caregivers with greater levels of burden at 3 and 12 months following injury and this pattern was especially pronounced in parents of children with unmet healthcare needs. These results not only indicate an interaction between quality-of-life following paediatric TBI and caregiver reported burden, but, along with the findings of Yeates et al. [11, 28] and Taylor et al. [29], suggest this relationship may be reciprocal.
The studies discussed above examined the relationship of family environmental factors (e.g. caregiver burden) and broad measures of recovery from paediatric TBI (e.g. performance on a task of social reasoning [11], ratings of externalizing/internalizing behaviours [28] or quality-of-life [31]). No studies have examined the relationship of family environment to other cognitive abilities that are thought to be important in the development of social interaction. For example, a foundational cognitive process posited to be important for successful social interaction is the ability to recognize the emotions of other people [32]. Previous research with adults and a few studies with children indicate difficulties recognizing emotions from voices and facial expressions are common in both the acute and chronic stages of recovery after closed head injury [33–42]. As such, researchers argue that difficulties with emotion recognition significantly contribute to deficits in social communication and social competence following TBI [34, 43, 44].
A recent study conducted by the authors [45] demonstrates the connection between family burden as it relates to SES and ability to recognize emotion for children recovering from TBI. Findings indicated difficulties with recognition of both emotion prosody and face emotion in the first 2 years following paediatric TBI. However, the patterns were different for these tasks and both procedures appeared influenced by environmental factors. On the emotional prosody task, children coming from low socioeconomic backgrounds who sustained a head injury consistently performed worse and demonstrated a slower recovery rate than matched orthopaedic injury (OI) controls. The performance of children from relatively higher socioeconomic circumstances in the closed head injury group initially lagged behind those in the OI group, but these children displayed a fast rate of recovery, eventually allowing their performance to surpass that of the OI controls. Conversely, children sustaining an OI always outperformed children with a TBI on the face emotion recognition task.
In summary, previous research demonstrates:
A likely link between emotion recognition and social cognition within typically-developing children.
Deficits in emotion recognition are likely following paediatric TBI.
Emotional recognition is related to environmental factors in children sustaining a TBI or OI.
Paediatric TBI increases caregiver burden and can increase family dysfunction.
Research indicates a link between family environment and broad measures of social/behavioural functioning.
Thus, the question remains, what is the connection between other aspects of the family environment such as caregiver perceived stressors and resources and emotional recognition following TBI? Exploring this connection is a necessary first-step toward a more thorough understanding of the relationship between the family environment and social outcomes after childhood head injury. To the authors’ knowledge, no studies have directly addressed this question.
Study purpose
The current study investigated the relationship between variables of family functioning (as indexed by a measure of caregiver social/financial stressors and resources) and the child’s performance on two tasks of emotion recognition (emotional prosody and face emotion recognition). The authors were particularly interested in whether specific variables within the broad domains of parental stress and resources (i.e. friends, finances, spouse, etc.) made independent contributions to the child’s emotion recognition skills. Additionally, the authors were interested in investigating if any obtained relationships were specific to emotional processing or more indicative of cognitive skills in general. Thus, this study examined the relationship between family functioning and performance on the Flanker task, which is a task of cognitive inhibition. This particular procedure was chosen because it is a relatively pure task of cognition and not likely to be significantly influenced by emotion processing skills. It was anticipated that it would provide a basis on which to interpret any findings by helping to determine if obtained results were specific to emotion recognition.
This study is unique in several respects. First, it examined possible relationships between specific variables of caregiver functioning and a child’s performance on two tasks of emotion recognition. Second, the measure used allowed one to specifically examine the role that caregiver functioning (independent from other variables of family functioning) may play in moderating cognitive performance over time. Finally, the use of a relatively emotion-free measure of cognitive skills [46, 47] (i.e. the Flanker task) allowed for a true comparison of the influence of family factors on emotional processing beyond the impact of overall cognitive performance.
This study used growth curve modelling in order to examine change over time (i.e. baseline, 3 months and 1-year follow-ups). It was hypothesized that some relationships would be observed between family functioning and performance on the emotion recognition tasks and that these relationships would not occur in both the emotion recognition tasks and the Flanker measure.
Method
Participants
All procedures were approved by the institutional review boards of the participating organizations and complied with the NIH policies on human subjects. Participants with TBI secondary to a closed head injury or an OI were recruited from Dallas, Houston and Miami medical centres during or directly after hospital admission. Inclusion of the OI group was intended to control for risk factors pre-disposing children to injury and to equate for non-specific factors such as maturation or stress resulting from hospitalization.
The current investigation examined participants at three time points; baseline within 1 month after injury, 3 months and 1 year post-injury. A total of 142 children (75 children with TBI and 67 children with orthopaedic injuries) participated in the current study as part of a larger project examining neurobehavioural outcomes following paediatric TBI. General participant information, including race, gender and mother’s education can be found in Table I Due to scheduling difficulties not every child participated in each of the three evaluation time points (see Table II). Participants ranged in age from 7–17 years of age at the time of injury (see Table III).
Table I.
Participant demographics, including gender, race and mother’s education
| OI | TBI | χ2 | t | p | |
|---|---|---|---|---|---|
| Gender | |||||
| Males | 47 (70.15%) | 49 (65.33%) | 0.37 | 0.5404 | |
| Females | 20 (29.85%) | 26 (34.67%) | |||
| Race* | |||||
| White | 21 (31.34%) | 32 (42.67%) | 7.56 | 0.0228 | |
| Black | 23 (34.33%) | 11 (14.67%) | |||
| Other | 23 (34.33%) | 32 (42.67%) | |||
| Mother’s education | |||||
| M | 13.53 | 12.45 | 2.21 | 0.0285 | |
| SD | 2.68 | 2.99 | |||
| Range | 7–20 | 5–18 | |||
Groups are significantly different when p <0.05.
Table II.
Number of participants observed at each occasion and total number of participants involved in the study
| OI | TBI | |
|---|---|---|
| Number of observations by occasion | ||
| Baseline | 65 | 65 |
| 3 month | 54 | 68 |
| 12 month | 44 | 50 |
| Total participants involved in study | 67 | 75 |
Table III.
Participant statistics, including age of injury acquisition, Glasgow Coma Scale score and mechanism of injury
| OI | TBI | t | p | |
|---|---|---|---|---|
| Age of injury* | ||||
| M | 12.021 | 13.341 | −2.97 | 0.0035 |
| SD | 2.48 | 2.773 | ||
| Range | 7.053–16.556 | 7.102–17.216 | ||
| GCS | ||||
| M | 14.985 | 7.972 | ||
| SD | 0.122 | 4.434 | ||
| Range | 14–15 | 3–15 | ||
| Mechanism of injury | ||||
| Auto, truck, bus (driver/passenger) | 2 | 24 | ||
| Motorcycle/moped | 5 | 7 | ||
| RV, off road | 1 | 6 | ||
| Bicycle | 5 | 5 | ||
| Fall | 13 | 12 | ||
| Falling object | 1 | 0 | ||
| Sports/play | 32 | 4 | ||
| Hit by motor vehicle (pedestrian) | 3 | 12 | ||
| Other | 4 | 2 | ||
Groups are significantly different, p < 0.05.
Enrolment criteria for the TBI group included the lowest post-resuscitation Glasgow Coma Scale (GCS) [48] score recorded at the emergency centre. In this sample, 75 children had moderate-to-severe TBI. Moderate TBI was defined by GCS scores of 9–12 or by GCS scores of 13–15 with brain lesions (contusions, haematomas) indicated by computed tomographic (CT) scans. Severe TBI was defined by GCS scores of 3–8. See Table III for a description of the participants in terms of GCS score and mechanism of injury. The 67 hospitalized OI patients had mild-to-moderate orthopaedic injuries as defined by the Abbreviated Injury Scale [49]. All participants were English-speaking, had no previous hospitalization for head injury and did not have a diagnosis of mental retardation or a neurodevelopmental disorder (e.g. Autism).
Procedures
Testing commenced only after parental consent and child assent were obtained in accordance with institutional review board-approved guidelines at each medical centre. Children were assessed at three time points during the first year of follow-up: baseline (within 1 month), 3 months (±1 month) and 12 months (±2 months) post-injury. Possible moderating variables relating to age at injury, socioeconomic status (SES), gender and ethnicity were also collected on each child/family. For the current study, mother’s education alone was used as a proxy measure of SES because other approaches for estimating this variable (e.g. the Socioeconomic Composite Index [SCI]) [11, 28] rely on variables such as total family income. In the current study, the measure of TBI was financial resources (i.e. a variable of interest) and thus could not also be used to estimate SES for reasons of redundancy.
Measures
Life Stressors and Social Resources Inventory-Adult Form (LISRES-A)
The LISRES-A [50] measures the proximal family environment by the parent completing a self-report inventory (or structured interview if reading is not adequate to complete the self-report form). The LISRES-A was developed to evaluate an individual’s unique pattern of stressors and resources within and across life domains such as finances, spouse, work, friends, family and physical health [51]. The scales measuring life stressors evaluate circumstances within each domain that may cause stress. Social resources scales assess circumstances within these same domains (with the exception of physical health), which may also be sources of social support. For example, work stressors include items such as ‘Do you have conflicts with your supervisor? Is there constant pressure?’, whereas work resources include items such as ‘Are your co-workers friendly toward you? Is your work challenging?’ Questions regarding financial stress are concerned with particular issues such as ‘do you have enough money to pay for …’, and financial resources are assessed in terms of family income on an eight-point scale ranging from < $20 000 to > $60 000. It should be noted that, with the exception of the spouse and financial domains, research suggests that individuals who report a high level of stress within a domain do not necessarily report corresponding low levels of resources within that same domain [51].
As traditionally used in paediatric TBI studies [11, 28], the Family Stressors score is defined as the mean of the T-scores for five Stressors scales (Health, Work, Spouse, Extended Family, and Friends), whereas the Family Resources score is defined as the mean T-score for four Resource scales (Work, Spouse, Extended Family and Friends). The correlations between these sub-scales were low in this sample, indicating a high degree of independence. Since the authors were interested in examining specific family factors that may affect emotion recognition, analyses were conducted using these individual sub-scales plus the sub-scales of financial stressors and financial resources. Of note, the financial resources scale is better conceptualized as a measure of family income, but will continue to be referred to as financial resources scale to remain consistent with the actual instrument. The LISRES-A was administered to each participating parent at each time point. At baseline, the measure pertained to pre-injury status, whereas at each follow-up assessment responses evaluated post-injury status.
Scores for single-parent families or families in which the parent does not work are limited to the relevant scales. Further, it should be emphasized that the LISRES-A provides a measure of the parent’s perception of their own stressors and resources, and is not a direct measure of a child’s stressors or resources. Internal consistency is moderate-to-high for all LISRES-A scales, as is stability (except for work) over a 1-year interval.
Emotional prosody task [52–54]
Children listened to a digital recording of four semantically neutral sentences spoken with eight different emotional prosodic contours: happy, sad, angry, neutral, afraid, surprised, disgusted and sleepy. To identify the emotion expressed, the participant pointed to the name of the emotion printed beneath a picture of a cartoon face displaying the emotion. Each sentence was 3-seconds in duration and all 32 sentences were played in random order for each participant. The task proceeded based upon the response rate of each participant making sure that there was a minimum of 10 seconds between sentences. Performance was evaluated in terms of the number of sentences correctly identified. This task has been shown to be sensitive to changes in cortical volume following paediatric TBI [54].
Face emotion recognition [55]
This task evaluated a participant’s ability to recognize facial emotions. Participants sorted 24 photographs. Each photograph displayed one of six adults expressing one of four different facial emotions (e.g. anger, happiness, surprise or disgust). Children were instructed to sort the photographs into four groups—each group comprising six people expressing the same emotion (e.g. all happy). Importantly, the previous study [45] demonstrated that, regardless of group, most participants were able to correctly sort faces by facial identity and, thus, that data is not included in the present investigation. The task was scored for accuracy of recognizing the emotion displayed by sorting into the correct emotion group and completion time to sort the photographs was recorded. The reliability for this task for children with TBI was moderately high (internal consistency coefficient = 0.75).
Eriksen Flanker + No-Go task
In this task, initially developed by Eriksen and Eriksen [47] and subsequently modified by Bunge et al. [46], each child was told that a central arrow would appear with other symbols next to it. The child was asked to press a key corresponding to the direction of the arrow as quickly and accurately as possible except when the central arrow had an X next to it, in which case no key press was necessary. This task consisted of 112 trials in four randomized conditions; stimuli adjacent to the central arrow were (a) facilitation: two arrows pointing in the same direction as the central arrow; (b) interference: two arrows pointing in the direction opposite the central arrow leading to interference from conflicting stimuli; (c) baseline: central arrow flanked by two dashes, providing a measure of baseline performance under a neutral condition; and (d) no-go: central arrow flanked by two Xs, a measure of overriding a pre-potent response. For these analyses, the authors were mainly interested in a measure of reaction time during a cognitive task. Therefore, performance was analysed by evaluating reaction time during the interference condition while controlling for baseline reaction time.
Statistical analysis
The demographic data were compared using t-tests for continuous variables (e.g. age-at-injury, mother’s education), and a Chi-Square test for categorical variables (e.g. gender and ethnicity). Procedures for the growth curve modelling are described below.
For relevant measures, outliers were observed and removed from the analysis resulting in a minimal loss of data points. A Poisson distribution was assumed for the outcome, because the variable was the total number of correct trials and a generalized linear mixed model utilizing the Glimmix procedure in SAS was applied to the data. Linear and quadratic functions of time were also tested in the model in order to model the growth curve of task performance over time. However, the quadratic function of the effect of time was not significant, so only the intercept and slope were entered into the model. Age-at-injury, mother’s education (as an estimate of SES), gender, ethnicity and injury group were examined for effects on the intercepts and slopes of the recovery. The effects of gender and ethnicity were not significant and therefore not included in the model. In order to interpret the outcome, age was centred at the overall mean of age.
On the emotion recognition and cognitive tasks, we evaluated the relationships among group, specific family factors, and emotional prosody identification. The LISRES-A defines specific family stressors as the sub-domains of Health, Finances, Work, Spouse, Extended Family and Friends, while specific family resources are sub-domains of Finances, Work, Spouse, Extended Family and Friends. For this study, each of these sub-domains was looked at in turn to determine its relation to the child’s performance on the emotional prosody, face emotion recognition and Flanker tasks.
Results
Demographic variables
There was no significant difference for gender between group, but the OI group was comprised of a higher proportion of participants of African American ethnicity and a lower proportion of participants of Caucasian and other ethnicities, χ2 (2, n = 142) = 7.56, p = 0.0228. TBI participants, as a group, were 1.3 years older than OI participants at the time of injury, t(140) = −2.97, p = 0.0035, and estimated SES for the TBI participants was lower than for OI participants, t(135) = 2.21, p = 0.0285. Although attrition was modest, data indicated that the relationship between groups with regard to these variables remained relatively stable over the three occasions.
Emotional prosody
After controlling for SES, only the Finances subdomain showed relations with the child’s emotional prosody performance. Financial resources were significantly positively related to the total correct responses on the prosody task (i.e. more resources resulted in better performance). This relation also depended on age, F(1,157) = 4.31, p = 0.0394, with the relationship stronger for younger participants. This relation also depended on group, F(1,157) = 7.43, p = 0.0072, with a positive relationship existing only in the TBI group, t(157) = 5.04, p <0.0001 (Figure 1; Table IV).
Figure 1.
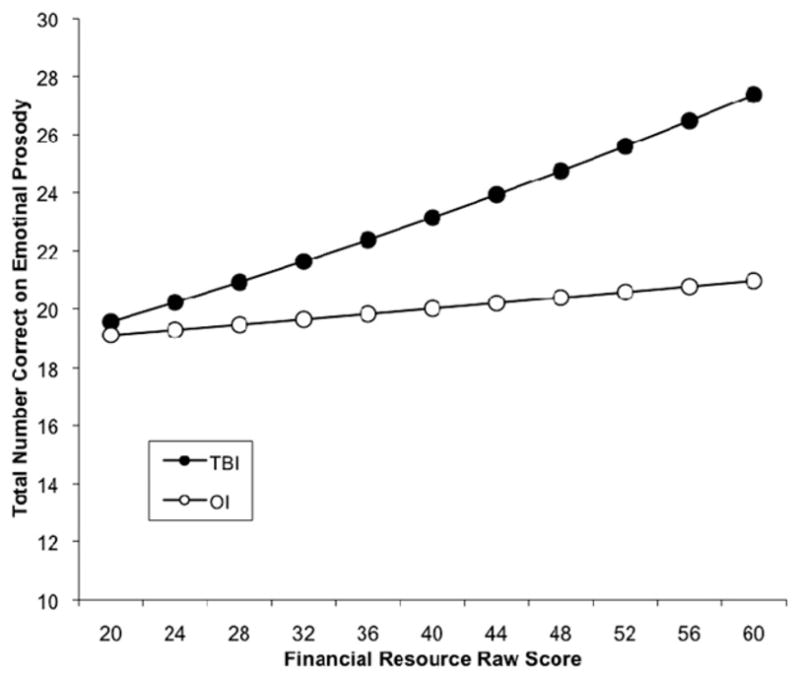
The relationship between Financial Resource raw scores and the total number of correct responses on the Emotional Prosody task was moderated by the type of injury to the participant. Orthopaedic control participants were not significantly affected by family resources, whereas those participants with TBI showed more improvement in task performance as family resources improved.
Table IV.
Results summary for the relation of LISRES-A to performance on the Emotional Prosody task
| Factors of LIRES-A | Predictors | Estimate | t | p |
|---|---|---|---|---|
| Financial stressor | ||||
| Group (OI vs TBI) | 0.0584 | 1.46 | 0.1453 | |
| Mother’s education | 0.0178 | 2.45 | 0.0154 | |
| Age | 0.0210 | 2.91 | 0.0041 | |
| Financial stressor | −0.0115 | −2.77 | 0.0063 | |
| Financial stressor*Age | 0.0038 | 2.67 | 0.0084 | |
| Interval | 0.0897 | 2.76 | 0.0065 | |
| Financial resource | ||||
| Group (OI vs TBI) | 0.0979 | 2.53 | 0.0123 | |
| Mother’s education | 0.0115 | 1.62 | 0.1068 | |
| Age | 0.0201 | 2.89 | 0.0045 | |
| Financial resource | 0.0084 | 5.04 | <0.0001 | |
| Financial resource*Group | −0.0061 | −2.73 | 0.0072 | |
| Financial resource*Age | −0.0009 | −2.08 | 0.0394 | |
| Interval | 0.0842 | 2.57 | 0.0110 | |
Interval is time since injury interval.
There was a significant negative relation between family financial stress and the number of correct responses made by the child on the prosody task (i.e. greater financial stress was associated with poorer performance). This depended on the child’s age, F(1,162) = 7.12, p = 0.008 (Table IV) with younger children showing the effect, but not older children. This relation did not change with group or time (Figure 2).
Figure 2.
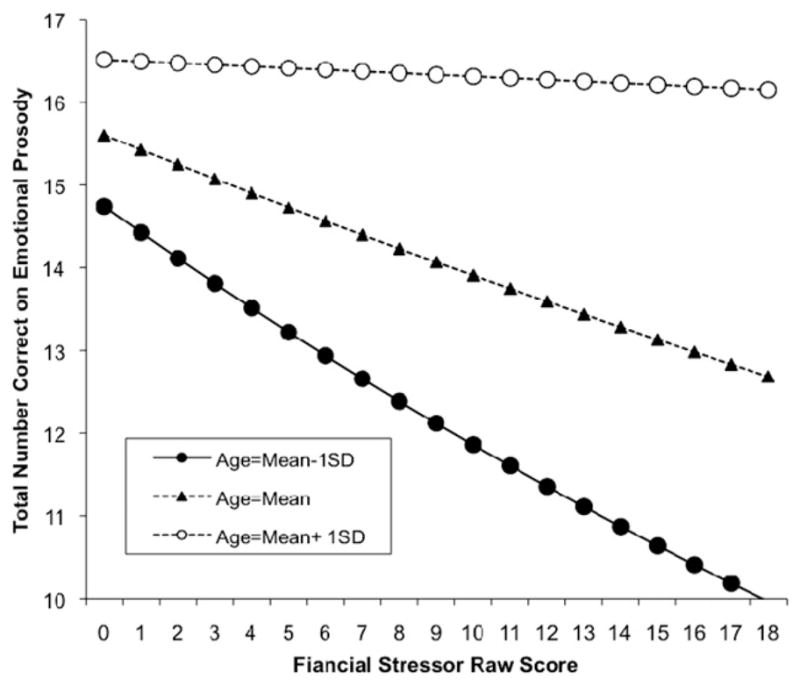
The relationship between Financial Stressor raw scores and the total number of correct responses on the Emotional Prosody task was moderated by age. Age categories are shown as standard deviations from the mean, with a positive deviation (i.e. older age) resulting in a much weaker negative relationship between financial stress and task performance.
Face emotion recognition
No significant relationships between face emotion recognition performance and any of the stressors or resources sub-domains of the LISRES-A were observed.
Flanker
SES as well as baseline reaction time were both controlled for in the analyses. Financial resources were negatively related to reaction time for both groups, F(1,121) = 4.20, p = 0.0426. Further, although not reaching statistical significance, financial stressors trended toward being positively related to reaction time on the Flanker, F(1,123) = 2.73, p = 0.1012. Because of the possible influence of cognitive inhibition on emotion recognition performance, this study re-analysed the initial emotional recognition data controlling for Flanker performance. The obtained results were essentially unchanged from the previous findings (i.e. Flanker performance did not alter the relationship between emotional recognition and family functioning variables for either the emotional prosody or face emotion recognition tasks).
Discussion
The current study examined the relationships between caregiver-perceived stressors and resources, child performance on two emotion recognition tasks and child performance on a task of cognitive inhibition. Several interesting findings were observed providing modest support for the influence of family environment on emotion recognition skills after childhood TBI.
LISRES-A and emotion recognition
Financial resources and financial stress appeared to have the most significant relationships to emotion recognition performance. Specifically, there was a significant interaction between financial resources, group and child performance on the emotional prosody task, so that children with TBI exhibited significantly better performance at higher levels of perceived financial resources. This result was stronger in younger vs older children. Caregiver perceived financial stress was negatively related to the child’s performance on the emotional prosody task for both TBI and OI groups, but only for younger children.
It was striking that no relationships emerged between face emotion recognition and LISRES-A sub-scales. Previous research indicated that OI participants consistently outperformed their TBI peers on the face emotion recognition task [45]. However, despite there being a general relationship between estimated SES and face emotion recognition performance in a previous investigation [45], there were no significant group by LISRES-A sub-scale interactions on face emotion recognition. The previously observed relationship may have been driven by SES factors other than those elements specifically related to the family environment. It is also possible that the measure of caregiver functioning was not sensitive to environmental variables important in face emotion recognition and studies using other instruments would be able to detect effects not captured in the current study. Another possibility is that emotions expressed by voice cues are more directly linked to the family context.
LISRES-A and Flanker
This study also examined the relationship of family functioning to performance on the Flanker task in order to determine how specific the findings were on the emotion prosody task. When analysing the data by sub-domain of the LISRES, a significant negative relationship between financial resources and reaction time emerged for both groups. Although the authors did not necessarily expect to observe any relationships between caregiver-reported factors and Flanker performance, this finding makes intuitive sense and is consistent with previous research that indicates children from more financially stable backgrounds (i.e. higher SES) have a better trajectory of cognitive recovery after TBI [5, 28, 56]. A re-analysis of the emotion recognition data controlling for Flanker performance did not alter the pattern of findings on either the emotional prosody or face emotion recognition tasks.
Impact of financial stress
Family financial stress was negatively related to performance on the emotional prosody task, but only in younger children. This finding supports previous research, indicating that younger children are more susceptible to parental stress and perturbations in the family system when compared to older children and adolescents [57, 58].
Previous research has linked financial stability and income level to cognitive and behavioural outcomes via direct and indirect mechanisms [59]. Not surprisingly, financial stress as indicated by poverty status has been associated with the amount and quality of a child’s home environment as well as the types of stimulating experiences a child is exposed to [60]. The impact of financial status appears particularly relevant for younger children [59]. Given these studies, it is speculated that financial stress may be negatively related to the quantity and quality of educational opportunities available to the children involved in this study. Further, it is possible that financial stress, as measured in the current investigation, is measuring the broader category of parental stress, which may itself adversely affect a child’s performance on cognitive tasks such as emotional prosody [13, 17–19]. Whatever the mechanism, it does not appear to be unique with regard to children who sustain a TBI. It cannot be ruled out, however, that the relationship of financial stress to emotional prosody performance is related to the parental stress and family upheaval experienced by families following a traumatic event (e.g. the serious injury of a child).
Impact of financial resources
The positive relationship between financial resources (i.e. family income) and emotional prosody performance for the TBI group was the only significant group difference that emerged in the current investigation. This finding remained significant even after controlling for estimated SES and is consistent with previous research demonstrating that income and financial considerations are significant predictors of caregiver burden following brain injury. The fact that this relationship was not depleted by accounting for SES in the analysis highlights the importance of adequate financial resources beyond other variables typically associated with SES in facilitating positive outcome after brain injury [31, 61]. However, the variable of financial resources may, in this case, merely be a proxy for other environmental influences (e.g. aspects of family functioning or of the community in which the family lives) that are important for TBI outcome but not otherwise captured by the LISRES-A. For example, the greater the financial resources, the less stress the caregiver is under and the better the outcome for the child. This mechanism may be particularly important in the current sample given the relatively narrow range of financial resources measured by the LISRES-A.
Osberg et al. [61] argue that the increases in financial strain after paediatric TBI affect the family system in a negative manner by exacerbating overall family stress, eventually leading to greater family disruption. Work by Montgomery et al. [62] indicated that financial difficulties are experienced by at least 30% of families even up to 3 years post-injury and research with adults suggests that decreased family financial resources have a direct and deleterious impact on outcome as well as having an indirect/moderating effect on caregiver burden [63].
Although confined to a single emotion recognition task, the findings from this study suggest a model for reciprocal interactions between financial resources, caregiver burden and recovery from TBI. One could imagine a scenario whereby lower family resources have a direct impact on recovery by restricting access to rehabilitation services and/or appropriate environmental/educational modifications, but also have an indirect impact on recovery by exacerbating caregiver burden and increasing overall levels of family stress [63].
Juxtaposing the relationships between family functioning and emotional prosody and family functioning and Flanker performance further highlights the importance of financial resources to children with TBI. The lack of group effects on the Flanker task is in contrast to the significant impact of group on the relationship between financial resources and emotional prosody performance. Controlling for Flanker performance did not significantly change the relationship between financial resources and emotional prosody. If similar mechanisms accounted for both Flanker and emotional prosody performance, one may expect similar patterns of findings between family functioning and these procedures. Thus, the continued presence of the group by financial resources interaction with regard to emotional prosody indicates that reaction time alone cannot account for this relationship.
Limitations and future directions
These findings are limited by certain considerations. First, the findings are restricted to two tasks of emotion recognition. These results cannot be generalized to other measures of emotional recognition or more directly related to social cognition. It could be the case that other emotional recognition tasks may yield a different pattern of findings in either the auditory or the visual domains. Second, although a striking impact of group was noted with regard to perceived financial resources, this was a singular result with regard to group. Third, caregiver distress and resources were used as a proxy measure of overall family functioning. Results that are more robust may have been obtained if we were able to incorporate other measures of family functioning. Fourth, even though emotion recognition is hypothesized to be a component of social cognition, the present findings do not necessarily generalize to other, more ecologically valid measures of social skill interaction. It is possible that family environment would have a larger impact on more complex social skills tasks. Finally, the estimate of financial resources was based on a single numeric scale of self-reported family income on the LISRES-A. As this scale only assesses financial resources in terms of income different results may be obtained if a more thorough measure of financial resources was used. For example, a scale that not only evaluated income but availability of medical coverage, savings, etc. may have provided a more complete picture of the role of financial resources in recovery from TBI.
In conclusion, these findings provide some support for the role of environmental factors in influencing the trajectory of recovery of emotion recognition skills following TBI. Specifically, they suggest that care-giver perceived stressors and resources are related to a child’s performance on a measure of emotional prosody as well as on a measure of cognitive inhibition after TBI. These results highlight the importance of financial resources in recovery from TBI and suggest that financial considerations may have wide-ranging implications for long-term outcomes following closed head injury. However, they also suggest that other processes related to social cognition (i.e. factors not related to emotion recognition) may better explain the link between the family environment and recovery of social interaction skills following TBI in children.
Acknowledgments
This work was supported by NINDS grant # NS21889 to HSL and by a NICHD T32 Fellowship to ATS.
Footnotes
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.Kraus JF. Epidemiological features of brain injury in children: occurrence, children at risk, causes and manner of injury, severity, and outcomes. In: Broman SH, Michel ME, editors. Traumatic head injury in children. New York: Oxford University Press; 1995. pp. 22–39. [Google Scholar]
- 2.Langlois JA, Kegler SR, Butler JA, Gotsch KE, Johnson RL, Reichard AA. Traumatic brain injury-related hospital discharges. MMWR Surveillance Summaries. 2003;52:1–18. [PubMed] [Google Scholar]
- 3.Channon S, Pellijeff A, Rule A. Social cognition after head injury: Sarcasm and theory of mind. Brain and Language. 2005;93:123–134. doi: 10.1016/j.bandl.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 4.Cicerone KD, Tanenbaum LN. Disturbance of social cognition after traumatic orbitofrontal brain injury. Archives of Clinical Neuropsychology. 1997;12:173–188. [PubMed] [Google Scholar]
- 5.Hanten G, Wilde EA, Menefee DS, Li X, Vasquez C, Swank P, Hunter JV, Lane S, Chu Z, Ramos MA, et al. Correlates of social problem solving during the first year after traumatic brain injury in children. Neuropsychology. 2008;22:357–370. doi: 10.1037/0894-4105.22.3.357. [DOI] [PubMed] [Google Scholar]
- 6.Janusz JA, Kirkwood MW, Yeates KO, Taylor HG. Social problem-solving skills in children with traumatic brain injury: Long-term outcomes and prediction of social competence. Child Neuropsychology. 2002;8:179–194. doi: 10.1076/chin.8.3.179.13499. [DOI] [PubMed] [Google Scholar]
- 7.Milders M, Fuchs S, Crawford JR. Neuropsychological impairments and changes in emotional and social behaviour following severe traumatic brain injury. Journal of Clinical and Experimental Neuropsychology. 2003;25:157–172. doi: 10.1076/jcen.25.2.157.13642. [DOI] [PubMed] [Google Scholar]
- 8.Snodgrass C, Knott F. Theory of mind in children with traumatic brain injury. Brain Injury. 2006;20:825–833. doi: 10.1080/02699050600832585. [DOI] [PubMed] [Google Scholar]
- 9.Turkstra LS, McDonald S, DePompeii R. Social information processing in adolescents: Data from normally developing adolescents and preliminary data from their peers with traumatic brain injury. Journal of Head Trauma Rehabilitation. 2001;16:469–483. doi: 10.1097/00001199-200110000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Yeates KO, Bigler ED, Dennis M, Gerhardt CA, Rubin KH, Stancin T, Taylor HG, Vannatta K. Social outcomes in childhood brain disorder: A heuristic integration of social neuroscience and developmental psychology. Psychological Bulletin. 2007;133:535–556. doi: 10.1037/0033-2909.133.3.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yeates KO, Swift E, Taylor HG, Wade SL, Drotar DD, Stancin T, Minich NM. Short-and long-term social outcomes following pediatric traumatic brain injury. Journal of the International Neuropsychological Society. 2004;10:412–426. doi: 10.1017/S1355617704103093. [DOI] [PubMed] [Google Scholar]
- 12.Wade SL, Taylor HG, Yeates KO, Drotar DD, Stancin T, Minich NM, Schluchter M. Long-term parental and family adaptation following pediatric brain injury. Journal of Pediatric Psychology. 2006;31:1072–1083. doi: 10.1093/jpepsy/jsj077. [DOI] [PubMed] [Google Scholar]
- 13.Cornell AH, Frick PJ. The moderating effects of parenting styles in the association between behavioral inhibition and parent-reported guilt and empathy in preschool children. Journal of Clinical Child and Adolescent Psychology. 2007;36:305–318. doi: 10.1080/15374410701444181. [DOI] [PubMed] [Google Scholar]
- 14.Kochanska G. Children’s temperament, mother’s discipline, and security of attachment: Multiple pathways to emerging internalization. Child Development. 1995;66:597–615. [Google Scholar]
- 15.Du Rocher TD, Shamir H, Cummings EM. Marital conflict, children’s representations of family relationships, and children’s dispositions towards peer conflict strategies. Social Development. 2004;13:171–192. [Google Scholar]
- 16.Kochanska G. Toward a synthesis of parental socialization and child temperament in early development of conscience. Child Development. 1993;64:325–347. [Google Scholar]
- 17.Eisenberg H, Cumberland A, Spinrad TL. Parental socialization of emotion. Psychological Inquiry. 1998;9:241–273. doi: 10.1207/s15327965pli0904_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Frick PJ, Morris AS. Temperament and developmental pathways to conduct problems. Journal of Clinical Child and Adolescent Psychology. 2004;33:54–68. doi: 10.1207/S15374424JCCP3301_6. [DOI] [PubMed] [Google Scholar]
- 19.Morris AS, Silk JS, Steinberg L, Myers SS, Robinson LR. The role of the family context in the develpment of emotion regulation. Social Development. 2007;16:361–388. doi: 10.1111/j.1467-9507.2007.00389.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anderson VA, Catroppa C, Dudgeon P, Morse S, Haritou F, Rosenfeld JV. Understanding predictors of functional recovery and outcome 30 months following early childhood head injury. Neuropsychology. 2006;20:42–57. doi: 10.1037/0894-4105.20.1.42. [DOI] [PubMed] [Google Scholar]
- 21.Anderson VA, Catroppa C, Haritou F, Morse S, Rosenfeld JV. Identifying factors contributing to child and family outcome 30 months after traumatic brain injury in children. Journal of Neurology, Neurosurgery and Psychiatry. 2005;76:401–408. doi: 10.1136/jnnp.2003.019174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ganesalingam K, Yeates KO, Ginn MS, Taylor HG, Dietrich A, Nuss K, Wright M. Family burden and parental distress following mild traumatic brain injury in children and its relationship to post-concussive symptoms. Journal of Pediatric Psychology. 2008;33:621–629. doi: 10.1093/jpepsy/jsm133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kinsella G, Ong B, Murtagh D, Prior M, Sawyer M. The role of the family for behavioral outcome in children and adolescents following traumatic brain injury. Journal of Consulting and Clinical Psychology. 1999;67:116–123. doi: 10.1037//0022-006x.67.1.116. [DOI] [PubMed] [Google Scholar]
- 24.Max JE, Castillo CS, Robin DA, Lindgren SD, Smith WL, Sato Y, Mattheis PJ, Stierwalt JAG. Predictors of family functioning after traumatic brain injury in children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:83–90. doi: 10.1097/00004583-199801000-00021. [DOI] [PubMed] [Google Scholar]
- 25.Schwartz L, Taylor HG, Drotar DD, Yeates KO, Wade SL, Stancin T. Long-term behavior problems following pediatric traumatic brain injury: Prevalence, predictors, and correlates. Journal of Pediatric Psychology. 2003;28:251–263. doi: 10.1093/jpepsy/jsg013. [DOI] [PubMed] [Google Scholar]
- 26.Taylor HG, Wade SL, Stancin T, Yeates KO, Drotar DD, Minich N. A prospective study of short-and long-term outcomes after traumatic brain injury in children. Behavior and Achievement Neuropsychology. 2002;16:15–27. doi: 10.1037//0894-4105.16.1.15. [DOI] [PubMed] [Google Scholar]
- 27.Taylor HG, Yeates KO, Wade SL, Drotar DD, Klein SK. Influences on first-year recovery from traumatic brain in children. Neuropsychology. 1999;13:76–89. doi: 10.1037//0894-4105.13.1.76. [DOI] [PubMed] [Google Scholar]
- 28.Yeates KO, Taylor HG, Drotar DD, Wade SL, Klein S, Stancin T, Schatschneider C. Preinjury family environment as a determinant of recovery from traumatic brain injuries in school-age children. Journal of the International Neuropsychological Society. 1997;3:617–630. [PubMed] [Google Scholar]
- 29.Taylor HG, Yeates KO, Wade SL, Drotar DD, Stancin T, Burant C. Bidirectional child–family influences on outcomes of traumatic brain injury in children. Journal of the International Neuropsychological Society. 2001;7:755–767. doi: 10.1017/s1355617701766118. [DOI] [PubMed] [Google Scholar]
- 30.Wade SL, Stancin T, Taylor HG, Drotar DD, Yeates KO, Minich NM. Interpersonal stressors and resources as predictors of parental adaptation following pediatric traumatic injury. Journal of Consulting and Clinical Psychology. 2004;72:776–784. doi: 10.1037/0022-006X.72.5.776. [DOI] [PubMed] [Google Scholar]
- 31.Aitken ME, McCarthy ML, Slomine BS, Ding R, Durbin DR, Jaffe KM, Paidas CN, Dorsch AM, Christensen JR, MacKenzie EJ, et al. Family burden after traumatic brain injury in children. Pediatrics. 2009;123:199–206. doi: 10.1542/peds.2008-0607. [DOI] [PubMed] [Google Scholar]
- 32.Lemerise EA, Arsenio WF. An integrated model of emotion processes and cognition in social information processing. Child Development. 2000;71:107–118. doi: 10.1111/1467-8624.00124. [DOI] [PubMed] [Google Scholar]
- 33.Allerdines MD, Alfano DP. Neuropsychological correlates of impaired emotion recognition following traumatic brain injury. Brain and Cognition. 2006;60:193–217. doi: 10.1016/j.bandc.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 34.Watts AJ, Douglas AM. Interpreting facial expression and communication competence following severe traumatic brain injury. Aphasiology. 2006;20:707–722. [Google Scholar]
- 35.Croker V, McDonald S. Recognition of emotion from facial expression following traumatic brain injury. Brain Injury. 2005;19:787–799. doi: 10.1080/02699050500110033. [DOI] [PubMed] [Google Scholar]
- 36.Green REA, Turner GR, Thompson WF. Deficits in facial emotion perception in adults with recent traumatic brain injury. Neuropsychologia. 2004;42:133–141. doi: 10.1016/j.neuropsychologia.2003.07.005. [DOI] [PubMed] [Google Scholar]
- 37.Henry JD, Phillips LH, Crawford JR, Ietswaart M, Summers F. Theory of mind following traumatic brain injury: The role of emotion recognition and executive dysfunction. Neuropsychologia. 2006;44:1623–1628. doi: 10.1016/j.neuropsychologia.2006.03.020. [DOI] [PubMed] [Google Scholar]
- 38.Hopkins MJ, Dywan J, Segalowitz SJ. Altered electrodermal response to facial expression after closed head injury. Brain Injury. 2002;16:245–257. doi: 10.1080/02699050110103346. [DOI] [PubMed] [Google Scholar]
- 39.Ietswaart M, Milders M, Crawford JR, Currie D, Scott CL. Logitudinal aspects of emotion recognition in patients with traumatic brain injury. Neuropsychologia. 2008;46:148–159. doi: 10.1016/j.neuropsychologia.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 40.Lew HL, Poole JH, Chiang JYP, Lee EH, Date ES, Warden D. Event-related potential in facial affect recognition: Potential clinical utility in patients with traumatic brain injury. Journal of Rehabilitation Research and Development. 2005;42:29–34. doi: 10.1682/jrrd.2004.05.0056. [DOI] [PubMed] [Google Scholar]
- 41.McDonald S, Flanagan S, Rollins J, Kinch J. TASIT: A new clinical tool for assessing social perception after traumatic brain injury. Journal of Head Trauma and Rehabilitation. 2003;18:219–238. doi: 10.1097/00001199-200305000-00001. [DOI] [PubMed] [Google Scholar]
- 42.Spell LA, Frank E. Recognition of nonverbal communication of affect following traumatic brain injury. Journal of Nonverbal Behavior. 2000;24:285–300. [Google Scholar]
- 43.Bornhofen C, McDonald S. Treating deficits in emotion perception following traumatic brain injury. Neuropsychological Rehabilitation. 2008;18:22–44. doi: 10.1080/09602010601061213. [DOI] [PubMed] [Google Scholar]
- 44.Hornak J, Rolls ET, Wade D. Face and voice expression identification in patients with emotional and behavioral changes following ventral frontal lobe damage. Neuropsychologia. 1996;34:247–261. doi: 10.1016/0028-3932(95)00106-9. [DOI] [PubMed] [Google Scholar]
- 45.Schmidt AT, Hanten GR, Li X, Orsten KD, Levin HS. Emotion recognition following pediatric traumatic brain injury: Longitudinal analysis of emotional prosody and facial expression. Neuropsychologia. doi: 10.1016/j.neuropsychologia.2010.05.029. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bunge SA, Dudukovic NM, Thomason ME, Vaidya CJ, Gabrieli JDE. Immature frontal lobe contributions to cognitive control in children: Evidence from fMRI. Neuron. 2002;33:1–11. doi: 10.1016/s0896-6273(01)00583-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Eriksen BA, Eriksen CW. Effects of noise letters upon the identification of a target letter in a non-search task. Perception and Psychophysics. 1974;16:143–149. [Google Scholar]
- 48.Teasdale G, Jennett B. Assessment of coma and impaired consciousness: A practical scale. Lancet. 1974;2:81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 49.Copes WS, Lawnick M, Champion HR, Sacco WJ. A comparison of Abbreviated Injury Scale: 1980 and 1985. Journal of Trauma. 1988;28:78–86. doi: 10.1097/00005373-198801000-00011. [DOI] [PubMed] [Google Scholar]
- 50.Moos RH, Moos BS. LISRES-A: Life Stressors and Social Resources Inventory - Adult Form Manual. Odessa: Psychological Assessment Resources, Inc; 1994. [Google Scholar]
- 51.Moos RH, Fenn CB, Billings AG. Life stressors and social resources: An integrated assessment approach. Social Science Medicine. 1988;27:999–1002. doi: 10.1016/0277-9536(88)90291-2. [DOI] [PubMed] [Google Scholar]
- 52.Adolphs R. The neurobiology of social cognition. Current Opinion in Neurobiology. 2001;11:231–239. doi: 10.1016/s0959-4388(00)00202-6. [DOI] [PubMed] [Google Scholar]
- 53.Adolphs R, Tranel D. Intact recognition of emotional prosody following amygdala damage. Neuropsychologia. 1999;37:1285–1292. doi: 10.1016/s0028-3932(99)00023-8. [DOI] [PubMed] [Google Scholar]
- 54.Levin HS. Neuroplasticity and brain imaging research: Implications for rehabilitation. Archives of Physical Medicine and Rehabilitation. 2006;87(12 Suppl):1. doi: 10.1016/j.apmr.2006.09.010. [DOI] [PubMed] [Google Scholar]
- 55.Adolphs R, Tranel D, Damasio H. Emotion recognition from faces and prosody following temporal lobectomy. Neuropsychology. 2001;15:396–404. doi: 10.1037//0894-4105.15.3.396. [DOI] [PubMed] [Google Scholar]
- 56.Hanten G, Li X, Newsome MR, Swank P, Chapman SB, Dennis M, Barnes MA, Ewing-Cobbs L, Levin HS. Oral reading and expressive language after childhood traumatic brain injury: Trajectory and correlates of change over time. Topics in Language Disorders. 2009;29:236–248. [Google Scholar]
- 57.Bronfenbrenner U. Ecology of the family as a context for human development: Research perspectives. Developmental Psychology. 1986;22:723–742. [Google Scholar]
- 58.Rudolph KD, Hammen C. Age and gender as determinants of stress exposure, generation, and reactions in youngsters: A transactional perspective. Child Development. 1999;70:660–677. doi: 10.1111/1467-8624.00048. [DOI] [PubMed] [Google Scholar]
- 59.Yeung WJ, Linver MR, Brooks-Gunn J. How money matters for young children’s development: Parental investment and family processes. Child Development. 2002;73:1861–1879. doi: 10.1111/1467-8624.t01-1-00511. [DOI] [PubMed] [Google Scholar]
- 60.Bradley RH, Corwyn RF, McAdoo HP, Coll CG. The home environments of children in the United States part I: Variations by age, ethnicity, and poverty status. Child Development. 2001;72:1844–1867. doi: 10.1111/1467-8624.t01-1-00382. [DOI] [PubMed] [Google Scholar]
- 61.Osberg JS, Brooke MM, Baryza MJ, Rowe K, Lash M, Kahn P. Impact of childhood brain injury on work and family finances. Brain Injury. 1997;11:11–24. doi: 10.1080/026990597123773. [DOI] [PubMed] [Google Scholar]
- 62.Montgomery V, Oliver R, Reisner A, Fallat ME. The effect of severe traumatic brain injury on the family. The Journal of Trauma: Injury, Infection, and Critical Care. 2002;52:1121–1124. doi: 10.1097/00005373-200206000-00016. [DOI] [PubMed] [Google Scholar]
- 63.Nabors N, Seacat J, Rosenthal M. Predictors of caregiver burden following traumatic brain injury. Brain Injury. 2002;16:1039–1050. doi: 10.1080/02699050210155285. [DOI] [PubMed] [Google Scholar]


