Abstract
Background
We evaluated the surgical results and predictors of long-term survival in patients who underwent coronary artery bypass grafting (CABG) at the time of an aortic valve replacement (AVR) due to aortic stenosis.
Materials and Methods
Between January 1990 and December 2009, 183 consecutive patients underwent CABG and concomitant aortic valve replacement for aortic stenosis. The mean follow-up period was 59.8±3.3 months and follow-up was possible in 98.3% of cases. Predictors of mortality were determined by Cox regression analysis.
Results
There were 5 (2.7%) in-hospital deaths. Follow-up of the in-hospital survivors documented late survival rates of 91.5%, 74.8%, and 59.6% at 1, 5, and 10 postoperative years, respectively. Age (p<0.001), a glomerular filtration rate (GFR) less than 60 mL/min (p=0.006), and left ventricular (LV) mass (p<0.001) were significant predictors of mortality in the multivariate analysis.
Conclusion
The surgical results and long-term survival of aortic valve replacement with concomitant CABG in patients with aortic stenosis and coronary artery disease were acceptable. Age, a GFR less than 60 mL/min, and LV mass were significant predictors of mortality.
Keywords: Aortic valve stenosis, Coronary artery disease, Coronary artery bypass surgery
INTRODUCTION
Aortic stenosis and coronary atherosclerosis can independently cause myocardial ischemia and the sequelae of myocardial ischemia including angina, myocardial infarction, and death. A review of the results of combined aortic valve replacement (AVR) and coronary artery bypass grafting (CABG) in several centers shows more variable mortality than that seen after isolated aortic valve replacement [1-6]. Therefore, the present study analyzed the surgical results and predictors of long-term survival in patients who underwent combined AVR and CABG for aortic stenosis and coronary artery disease.
MATERIALS AND METHODS
1) Patients
The present study examined the records of 183 patients who underwent combined AVR and CABG for aortic stenosis and co-existing coronary artery disease at our institution between January 1990 and December 2009. Data collection involved reviewing in-patient and out-patient medical records, and conducting telephone interviews. The study protocol was approved by the Institutional Review Board of the Asan Medical Center, Seoul, Korea. The requirement for informed patient consent was waived by the board because of the retrospective nature of the study.
2) Definitions
All patients underwent preoperative cardiac catheterization and echocardiography within 2 months prior to surgery. Coronary arteries with greater than 70% narrowing were considered significantly stenosed. Categorization of the extent of coronary artery disease (CAD) (one-, two-, or three-vessel disease) was based on the significant stenosis of major arteries (left anterior descending, left circumflex, or the right coronary artery) or branches thereof. Revascularization was considered incomplete if any major artery or one of the branches had a significant stenosis that was not revascularized with a bypass graft at the time of surgery. The severity of aortic stenosis was defined as mild, moderate, or severe by using the ACC/AHA guidelines for the management of patients with valvular heart disease [7]. Glomerular filtration rate (GFR) means the estimated GFR in this study [8].
Operative variables included completeness of myocardial revascularization, type of aortic prosthesis implanted, global ischemic time, total cardiopulmonary bypass time, and use of the internal thoracic artery. The selection of aortic valve prosthesis type was based on surgeon and patient preference. Operative mortality was defined as death prior to discharge or any death within 30 days following surgery. Major adverse cardiac events (MACE) included anticoagulation complication, thrombo-embolism including cerebrovascular attack, re-interventions for aortic valve or coronary artery, and infective endocarditis.
3) Statistical analysis
Categorical variables were presented as frequencies and percentages, and were compared using the chi-square test or Fisher's exact test. Continuous variables were expressed as mean±SD or medians with ranges, and were compared using the Student's unpaired t test or Mann-Whitney U test, as appropriate. Kaplan-Meier curves were employed to delineate overall survival, and log-rank tests were used to compare the differences in survival rates between groups. Stratified survival curves were plotted to explore unadjusted differences for variables of interest. For multivariate analyses, updated covariate Cox's proportional hazard regression models were used to examine the association of baseline characteristics with time to death. Variables with a probability value <0.05 in univariate analyses were candidates for the multivariable Cox models. Multivariate analyses involved a backward elimination technique and only variables with a p-value of <0.05 were used in the final model. Results were expressed as hazard ratios (HR) with 95% confidence intervals (CI). All reported p-values are two-sided, and p-values of less than 0.05 were considered to indicate statistical significance. SPSS version 14.0 was used for the statistical analysis.
RESULTS
1) Preoperative clinical characteristics and operative variables
The mean age at surgery was 68.0±8.8 years and 60.7% of patients were male. Clinical follow up was complete in 98.4% of patients, with a mean follow-up duration of 59.8±3.3 months. The clinical details and results of cardiac catheterization and echocadiography are shown in Table 1. Mean cross-clamp time and cardiopulmonary bypass time were 104.3±42.5 minutes and 170.1±63 minutes, respectively. A total of 103 bioprostheses (56.3%) and 80 mechanical prostheses (43.7%) were used. Overall, 65% (n=119) of patients used an internal mammary artery graft. Among all of the patients in our study cohort were 40 (21.9%) patients who were considered incompletely revascularized. For all patients, the reason for incomplete revascularization was poor distal target or quality.
Table 1.
Preoperative clinical characteristics
Values represent mean±SD. Values in parentheses are percentages. NYHA=New York Heart Association functional class; COPD=Chronic obstructive pulmonary disease; Hx=History; MI=Myocardial infarction; A-fib=Atrial fibrillation; eGFR=Estimated glomerular filtration rate; CAD=Coronary artery disease.
2) Early outcomes
Significant postoperative morbidities occurred in 24 patients (Table 2). There were five cases of stroke and four cases of bleeding. Five (2.7%) in-hospital deaths occurred. Three patients died in the immediate postoperative period, and of these, two deaths occurred from low cardiac output and the other was secondary to a hemorrhagic diathesis and complications. The remaining two deaths were attributable to sepsis and postoperative atrioventricular block, respectively.
Table 2.
Mortality and significant postoperative morbidities
Values in parentheses are percentages.
3) Late outcomes
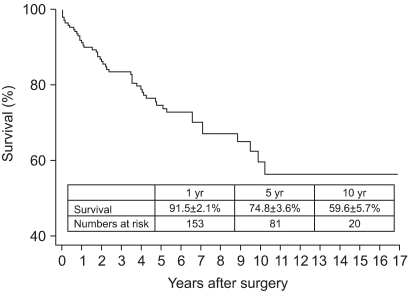
Late death occurred in 48 patients including 31 cardiac and 17 non-cardiac deaths. Non-cardiac deaths included cancer in 3 patients, infection in 3 patients, multiorgan failure in 3 patients, and accidents and other causes in 6 patients. Overall survival was 91.5±2.1% at 1 year, 74.8±3.6% at 5 years, and 59.6±5.7% at 10 years (Fig. 1).
Fig. 1.
Long-term survival rate.
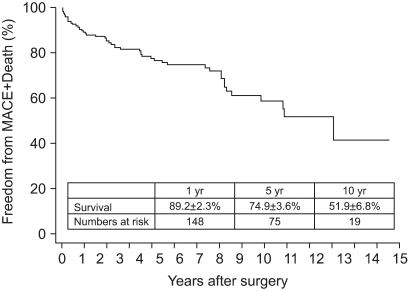
Three reoperations were performed. One patient underwent a redo-CABG because of the occlusion of a saphenous vein graft to the left anterior descending artery (LAD). The other two patients underwent redo-AVR because of prosthetic aortic valve failure (Fig. 2).
Fig. 2.
Freedom from Major adverse cardiac events (MACE) and mortality.
Univariate analysis identified older age, a GFR less than 60 mL/min, history of myocardial infarction (MI), presence of chronic obstructive pulmonary disease (COPD), left ventricular internal dimension of systole (LVIDs), end-systolic volume (ESV) and lower ejection fraction as factors associated with overall mortality. Multivariate analysis revealed that older age, a GFR less than 60 mL/min, and LVIDs were independent factors affecting long-term survival (Table 3).
Table 3.
Univariate and multivariate analysis for risk factors of mortality
Cox proportional hazard model (backward LR). AMI=Acute myocardial infarction; CI=Confidence Interval; eGFR=Estimated glomerular filtration rate; AMI=Acute myocardial infarction; NYHA IV=New York Heart Association functional class IV; LV=Left ventricle; LVIDs=Systolic left ventricular internal diameter; ESV=End-systolic volume; EDV=End-diastolic volume; EF=Ejection fraction.
In terms of MACE and death, univariate analysis identified a GFR less than 60 mL/min, New York Heart Association class IV, echocardiographic data including LV mass greater than 280 g, ESV, and EDV as significant factors. Multivariate analysis revealed that a GFR less than 60 mL/min, EDV, and LV mass greater than 280 g were also independent factors in MACE and death (Table 4).
Table 4.
Univariate and multivariate analysis for risk factors of major adverse cardiac events and mortality
Cox proportional hazard model (backward LR). CI=Confidence interval; eGFR=Estimated glomerular filtration rate; AMI=Acute myocardial infarction; NYHA IV=New York Heart Association functional class IV; LV=Left ventricle; LVIDs=Systolic left ventricular internal diameter; ESV=End-systolic volume; EDV=End-diastolic volume; EF=Ejection fraction.
DISCUSSION
The present study examined surgical and long-term clinical outcomes following combined AVR and CABG in patients with aortic stenosis and coronary artery disease. The outcomes and survival rates were acceptable. The operative mortality rate was 2.7%. This rate was similar to rates reported by others, which ranged from 3.4% to 6.5% [2,9-13], and which were no different from those for patients undergoing isolated AVR and not CABG [14-16]. In the current study, the 10-year cumulative survival rate was 59.6%, which was similar to rates reported by others (52% in [10] and 55% in [9,11]).
The present study included 18 patients (10.8%) with moderate aortic stenosis. It is broadly accepted that AVR should be performed in conjunction with CABG if aortic stenosis is severe or if the patient has symptoms. However, controversy exists regarding the treatment of asymptomatic patients with mild or moderate stenosis [17,18]. A recent study showed that AVR at the time of CABG for mild or moderate aortic stenosis appeared to convey a survival advantage on patients with moderate aortic stenosis but not on those with mild aortic stenosis [11,19,20].
1) Risk factors for long-term clinical outcomes
The present study found that older age had a negative effect on long-term survival, as reported elsewhere [3,10,12]. We found that in patients ≥70 years old, the 10-year survival rate was 24.5±10.7%, and that the rate decreased with greater age. This shorter life expectancy for patients older than 70 years should be taken into account when considering surgery in such patients.
We found that incomplete CABG revascularization did not influence late survival. An early study by Kobayashi and colleagues [21] showed that although extensive CAD negatively influenced early mortality, this did not negatively affect late survival. In addition, the number of diseased territories, the number of bypass grafts, incomplete revascularization, aortic stenosis, and aortic insufficiency did not predict late mortality in the cited study or our present work.
The present study found that survival was not affected by valve type (mechanical or bioprosthetic). These findings are consistent with previous studies showing satisfactory long-term results using either mechanical or bioprosthetic valves in AVR [22,23] and AVR-CABG [24,25] patients.
LV mass is proportional to the total force that contracting LV walls must receive at end-systole. As aortic stenosis becomes more severe, the measured values of LV mass, EDV, and LVID also become greater. These changes in the measured value mean LV hypertrophy (LVH). The results of the present study found that preoperative LVH might be a negative effect of both mortality and MACE, including mortality, because LVH caused problems with myocardial protection and remodeling due to scar change. Early surgery might therefore be a therapeutic option to further improve clinical outcomes and lessen operative risk [26,27].
The analysis of left ventricular function and its influence on long-term survival is complex in patients with both aortic valve disease and coronary disease. Segmental dysfunction secondary to myocardial infarction will not be improved by surgery and may theoretically have a more profound effect on risk than will generalized impairment of left ventricular function caused by aortic stenosis [9]. Previous studies [10,12,21] showed that a low EF increased the risk of undergoing AVR-CABG. However, EF was not found to influence long-term survival in the current study.
Several studies have documented ten-year cumulative survival rates similar (52% [10], 55% [9,11]) to the 59% from this study. Although this study contains younger patients with higher preoperative ejection fractions, several factors were also identified in this study as significant predictors of mortality.
CONCLUSION
The surgical results and long-term survival rates were acceptable for patients undergoing a combined CABG for aortic stenosis and coronary artery disease. Multivariate analysis found that older age, a GFR less than 60 mL/min, and greater LVIDs were independent variables affecting long-term survival in such patients.
References
- 1.Varadarajan P, Kapoor N, Bansal RC, Pai RG. Survival in elderly patients with severe aortic stenosis is dramatically improved by aortic valve replacement: results from a cohort of 277 patients aged or > =80 years. Eur J Cardiothorac Surg. 2006;30:722–727. doi: 10.1016/j.ejcts.2006.07.028. [DOI] [PubMed] [Google Scholar]
- 2.Richardson JV, Kouchoukos NT, Wright JO, Karp RB. Combined aortic valve replacement and myocardial revascularization: results in 220 patients. Circulation. 1979;59:75–81. doi: 10.1161/01.cir.59.1.75. [DOI] [PubMed] [Google Scholar]
- 3.He GW, Grunkemeier GL, Starr A. Aortic valve replacement in elderly patients: influence of concomitant coronary grafting on late survival. Ann Thorac Surg. 1996;61:1746–1751. doi: 10.1016/0003-4975(96)00143-9. [DOI] [PubMed] [Google Scholar]
- 4.Grimard BH, Larson JM. Aortic stenosis: diagnosis and treatment. Am Fam Physician. 2008;78:717–724. [PubMed] [Google Scholar]
- 5.Tjang YS, van Hees Y, Korfer R, Grobbee DE, van der Heijden GJ. Predictors of mortality after aortic valve replacement. Eur J Cardiothorac Surg. 2007;32:469–474. doi: 10.1016/j.ejcts.2007.06.012. [DOI] [PubMed] [Google Scholar]
- 6.Jones M, Schofield PM, Brooks NH, et al. Aortic valve replacement with combined myocardial revascularisation. Br Heart J. 1989;62:9–15. doi: 10.1136/hrt.62.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bonow RO, Carabello BA, Chatterjee K, et al. 2008 focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1998 guidelines for the management of patients with valvular heart disease). Endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2008;52:e1–e142. doi: 10.1016/j.jacc.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 8.Jin R, Grunkemeier GL, Brown JR, Furnary AP. Estimated glomerular filtration rate and renal function. Ann Thorac Surg. 2008;86:1–3. doi: 10.1016/j.athoracsur.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 9.Lytle BW, Cosgrove DM, Loop FD, et al. Replacement of aortic valve combined with myocardial revascularization: determinants of early and late risk for 500 patients, 1967-1981. Circulation. 1983;68:1149–1162. doi: 10.1161/01.cir.68.6.1149. [DOI] [PubMed] [Google Scholar]
- 10.Lytle BW, Cosgrove DM, Goormastic M, Loop FD. Aortic valve replacement and coronary bypass grafting for patients with aortic stenosis and coronary artery disease: early and late results. Eur Heart J. 1988;9(Suppl E):143–147. doi: 10.1093/eurheartj/9.suppl_e.143. [DOI] [PubMed] [Google Scholar]
- 11.Pereira JJ, Balaban K, Lauer MS, Lytle B, Thomas JD, Garcia MJ. Aortic valve replacement in patients with mild or moderate aortic stenosis and coronary bypass surgery. Am J Med. 2005;118:735–742. doi: 10.1016/j.amjmed.2005.01.072. [DOI] [PubMed] [Google Scholar]
- 12.Shahian DM, O'Brien SM, Filardo G, et al. The Society of Thoracic Surgeons 2008 cardiac surgery risk models: part 3--valve plus coronary artery bypass grafting surgery. Ann Thorac Surg. 2009;88:S43–S62. doi: 10.1016/j.athoracsur.2009.05.055. [DOI] [PubMed] [Google Scholar]
- 13.Morell VO, Daggett WM, Pezzella AT, Moran JM, Bitran D. Aortic stenosis in the elderly: result of aortic valve replacement. J Cardiovasc Surg (Torino) 1996;37:33–35. [PubMed] [Google Scholar]
- 14.Kirklin JW, Kouchoukos NT. Aortic valve replacement without myocardial revascularization. Circulation. 1981;63:252–253. doi: 10.1161/01.cir.63.2.252. [DOI] [PubMed] [Google Scholar]
- 15.Miller DC, Stinson EB, Oyer PE, Rossiter SJ, Reitz BA, Shumway NE. Surgical implications and results of combined aortic valve replacement and myocardial revascularization. Am J Cardiol. 1979;43:494–501. doi: 10.1016/0002-9149(79)90005-5. [DOI] [PubMed] [Google Scholar]
- 16.Mihaljevic T, Nowicki ER, Rajeswaran J, et al. Survival after valve replacement for aortic stenosis: implications for decision making. J Thorac Cardiovasc Surg. 2008;135:1270–1278. doi: 10.1016/j.jtcvs.2007.12.042. discussion 8-9. [DOI] [PubMed] [Google Scholar]
- 17.Lester SJ, Heilbron B, Gin K, Dodek A, Jue J. The natural history and rate of progression of aortic stenosis. Chest. 1998;113:1109–1114. doi: 10.1378/chest.113.4.1109. [DOI] [PubMed] [Google Scholar]
- 18.Hochrein J, Lucke JC, Harrison JK, et al. Mortality and need for reoperation in patients with mild-to-moderate asymptomatic aortic valve disease undergoing coronary artery bypass graft alone. Am Heart J. 1999;138:791–797. doi: 10.1016/s0002-8703(99)70198-5. [DOI] [PubMed] [Google Scholar]
- 19.Smith WT, Ferguson TB, Ryan T, Landolfo CK, Peterson ED. Should coronary artery bypass graft surgery patients with mild or moderate aortic stenosis undergo concomitant aortic valve replacement? A decision analysis approach to the surgical dilemma. J Am Coll Cardiol. 2004;44:1241–1247. doi: 10.1016/j.jacc.2004.06.031. [DOI] [PubMed] [Google Scholar]
- 20.Ahmed AA, Graham AN, Lovell D, O'Kane HO. Management of mild to moderate aortic valve disease during coronary artery bypass grafting. Eur J Cardiothorac Surg. 2003;24:535–539. doi: 10.1016/s1010-7940(03)00469-x. discussion 9-40. [DOI] [PubMed] [Google Scholar]
- 21.Kobayashi KJ, Williams JA, Nwakanma L, Gott VL, Baumgartner WA, Conte JV. Aortic valve replacement and concomitant coronary artery bypass: assessing the impact of multiple grafts. Ann Thorac Surg. 2007;83:969–978. doi: 10.1016/j.athoracsur.2006.10.027. [DOI] [PubMed] [Google Scholar]
- 22.Elayda MA, Hall RJ, Reul RM, et al. Aortic valve replacement in patients 80 years and older. Operative risks and long-term results. Circulation. 1993;88:II11–II16. [PubMed] [Google Scholar]
- 23.Glower DD, White WD, Hatton AC, et al. Determinants of reoperation after 960 valve replacements with Carpentier-Edwards prostheses. J Thorac Cardiovasc Surg. 1994;107:381–392. discussion 92-3. [PubMed] [Google Scholar]
- 24.Medalion B, Lytle BW, McCarthy PM, et al. Aortic valve replacement for octogenarians: are small valves bad? Ann Thorac Surg. 1998;66:699–705. doi: 10.1016/s0003-4975(98)00691-2. discussion-6. [DOI] [PubMed] [Google Scholar]
- 25.Magovern JA, Pennock JL, Campbell DB, et al. Aortic valve replacement and combined aortic valve replacement and coronary artery bypass grafting: predicting high risk groups. J Am Coll Cardiol. 1987;9:38–43. doi: 10.1016/s0735-1097(87)80079-7. [DOI] [PubMed] [Google Scholar]
- 26.Kang DH, Park SJ, Rim JH, et al. Early surgery versus conventional treatment in asymptomatic very severe aortic stenosis. Circulation. 2010;121:1502–1509. doi: 10.1161/CIRCULATIONAHA.109.909903. [DOI] [PubMed] [Google Scholar]
- 27.Brown ML, Pellikka PA, Schaff HV, et al. The benefits of early valve replacement in asymptomatic patients with severe aortic stenosis. J Thorac Cardiovasc Surg. 2008;135:308–315. doi: 10.1016/j.jtcvs.2007.08.058. [DOI] [PubMed] [Google Scholar]