Abstract
A 43-year-old woman was diagnosed with an intravenous leiomyomatosis at a previous hospital and transferred to our hospital to undergo surgical treatment. Emergency one-stage operation for coincidental removal of intra-abdominal, right atrial, and intravenous masses were planned. Upon arriving at the operating room, she suffered a sudden onset of severe dyspnea and showed hemodynamic instability. Intraoperative TEE showed pulmonary embolization of a right atrial mass. Removal of the pulmonary artery mass and the intra-abdominal mass, and the cardiopulmonary bypass were performed without any complications.
Keywords: Pulmonary artery, Embolization, Leiomyomatosis
CASE REPORT
A 43-year-old woman diagnosed with intravenous leiomyomatosis at another hospital was transferred to our hospital. She had suffered from palpitation, dizziness, dyspnea, and chest pain for two weeks prior to admission into another hospital, and had experienced syncope three times on the day of admission to our hospital. No cardiac murmur was noted, and laboratory findings were unremarkable with the exception of anemia (Hemoglobin: 9.7 g/L). Cardiac and pelvic magnetic resonance imaging (MRI) taken at the previous hospital revealed multiple low attenuation masses in the uterus, involving both ovaries, the left gonadal vein, the left internal iliac vein, and the left renal vein, which extended into the inferior vena cava (IVC), and to the right atrium (RA) (Fig. 1). A trans-thoracic echocardiogram revealed a 4.8×1.8-cm hypermobile and echogenic mass in the RA connected to the mass in the IVC. Emergency one-stage operation was planned with a gynecologist, and upon being transferred to the operation room, the patient had a sudden onset of dyspnea and unstable blood pressure. Rapid endotracheal intubation was performed to maintain blood oxygen saturation. In transesophageal echocardiography (TEE), the echogenic mass in the RA and IVC was not seen. We suggested that the mass detached from the RA and migrated to the right ventricle or the pulmonary artery. We discovered an echogenic linear mass in the pulmonary artery between the arterial bifurcation and both main pulmonary arterial branches (Fig. 2). Trans-abdominal hysterectomy and left salphingo-oophorectomy were performed through median laparotomy, and the mass in the left gonadal and internal iliac veins was completely removed (Fig. 3A). Another mass in the pulmonary artery was also removed under conventional cardiopulmonary bypass without circulatory arrest (Fig. 3B). The RA was opened to confirm that there was no remnant mass in the RA and the IVC. The histologic study confirmed intravenous leiomyomatosis. The patient's postoperative course was uneventful, and she has received follow-up care for two years without any evidence of tumor recurrence.
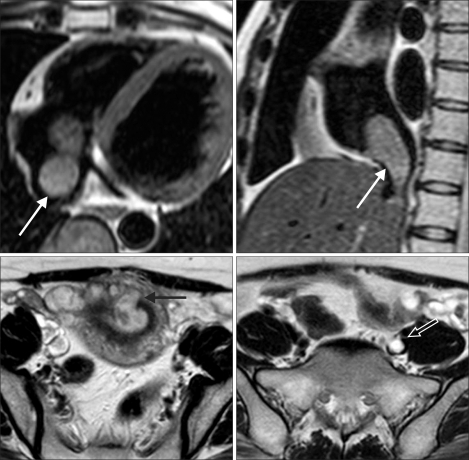
Fig. 1.
T2-weighted cardiac MRI showing a lobulated mass in the right atrium extended from the inferior vena cava (white arrows). T2-weighted pelvic MRI showing an endometrial mass (black arrow) invading the myometrium and extending into the left pelvic vein (hollow arrow).
Fig. 2.
Intraoperative trans-esophageal echocardiogram reveals no previous mass in the right atrium or the inferior vena cava, but a solid mass (white arrow) in the right pulmonary artery. RA=Right atrium; IVC=Inferior vena cava; RPA=Right pulmonary artery; PA=Pulmonary artery.
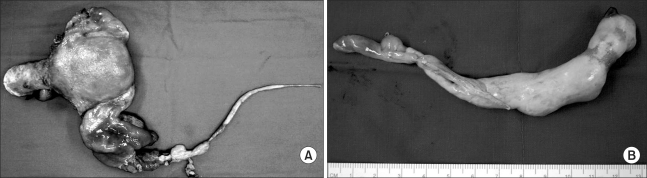
Fig. 3.
Gross findings of the masses removed from the inferior vena cava (A), and from the right pulmonary artery (B).
DISCUSSION
Intravenous leiomyomatosis is a benign intravascular proliferation of smooth muscle cells originating from the intrauterine venules and reaching the right heart [1]. The uncommon benign tumor usually arises from either the uterine venous wall or uterine leiomyoma [2], and although it is histologically benign, it can cause fatal cardiovascular complications such as cardiac failure, pulmonary embolization, or sudden death [3]. In previously reported cases describing intracardiac involvement, the tumor extended to the right atrium in 30% of cases, and to the right ventricle in 70% of cases [3,4]. Extension or embolization into the pulmonary artery or lung metastasis is a very rare complication constituting less than 5% of the reported cases [5]. However, when it occurs, the course of the patient can be fatal, and urgent surgical correction is imperative.
Ariza and colleagues described the first successful two-stage removal of an intracaval mass, with delayed laparotomy after resection of the intracardiac portion of a tumor in 1982 [6]. Since then, a staged operation has been performed in many cases (radical resections of intracavocardiac tumors and intrapelvic components in separate operations), but more recently, a one-stage approach by median sternotomy with cardiopulmonary bypass with or without hypothermic circulatory arrest, and a separate laparotomy has been performed successfully [1,3,4]. The advantages of the one-stage resection include avoiding risks of tumor embolism, tumor progression, or hemodynamic complications in the interval between the two stages of two-staged operations. In addition, because both abdominal and thoracic cavities are opened, the tumor can be removed completely, and vascular reconstruction and bleeding control may be more easily performed [7]. However, in hemodynamically unstable patients, the longer operative time may not be appropriate, and a two-stage operation may be beneficial.
Since incomplete resection of the tumor may causes recurrence, gathering detailed preoperative information regarding tumor localization, size, and extent by using abdominal ultrasound, echocardiogram, computed tomography, magnetic resonance imaging, and venography is required [8]. Transesophageal echocardiography should also be performed to detect possible changes in the location and size of the tumor, as occurred in this case.
In conclusion, intracardiac leiomyomatosis should be considered in a female patient presenting with an extensive mass in the right side of the heart, and urgent surgical removal should be performed to avoid possible fatal complications, even if the patient is asymptomatic. As the tumor may move or detach from the central venous system even during operation, intraoperative TEE is considered a very important diagnostic tool.
References
- 1.Rispoli P, Santovito D, Tallia C, Varetto G, Conforti M, Rinaldi M. A one-stage approach to the treatment of intravenous leiomyomatosis extending to the right heart. J Vasc Surg. 2010;52:212–215. doi: 10.1016/j.jvs.2010.02.018. [DOI] [PubMed] [Google Scholar]
- 2.Nam MS, Jeon MJ, Kim YT, Kim JW, Park KH, Hong YS. Pelvic leiomyomatosis with intracaval and intracardiac extension: a case report and review of the literature. Gynecol Oncol. 2003;89:175–180. doi: 10.1016/s0090-8258(02)00138-5. [DOI] [PubMed] [Google Scholar]
- 3.Uchida H, Hattori Y, Nakada K, Iida T. Successful one-stage radical removal of intravenous leiomyomatosis extending to the right ventricle. Obstet Gynecol. 2004;103:1068–1070. doi: 10.1097/01.AOG.0000127947.14387.01. [DOI] [PubMed] [Google Scholar]
- 4.Harris LM, Karakousis CP. Intravenous leiomyomatosis with cardiac extension: tumor thrombectomy through an abdominal approach. J Vasc Surg. 2000;31:1046–1051. doi: 10.1067/mva.2000.104601. [DOI] [PubMed] [Google Scholar]
- 5.Lo KW, Lau TK. Intracardiac leiomyomatosis. Case report and literature review. Arch Gynecol Obstet. 2001;264:209–210. doi: 10.1007/s004040000115. [DOI] [PubMed] [Google Scholar]
- 6.Ariza A, Cerra C, Hahn IS, Shaw RK, Rigney B. Intravascular leiomyomatosis of the uterus. A case report. Conn Med. 1982;46:700–703. [PubMed] [Google Scholar]
- 7.Zhang C, Miao Q, Liu X, et al. Intravenous leiomyomatosis with intracardiac extension. Ann Thorac Surg. 2010;89:1641–1643. doi: 10.1016/j.athoracsur.2009.09.044. [DOI] [PubMed] [Google Scholar]
- 8.Kocica M, Vranes MR, Kostic D, et al. Intravenous leiomyomatosis with extension to the heart: rare or underestimated? J Thorac Cardiovasc Surg. 2005;130:1724–1726. doi: 10.1016/j.jtcvs.2005.08.021. [DOI] [PubMed] [Google Scholar]