Abstract
Spontaneous pneumothorax is a common clinical problem in emergency care. However, the overall incidences of primary spontaneous pneumothorax has been reported from as low as 1.4% to 7.6%. The clinical findings of simultaneous bilateral spontaneous pneumothorax can be variable. Clinical presentation is variable, ranging from mild dyspnea to tension pneumothorax. Bilateral tension pneumothorax can defined as cases where no tracheal deviation is detected in chest X-ray, and symptoms may be equal bilaterally. Herein, we present a case with simultaneous bilateral tension pneumothorax, severely deteriorated (i.e. with loss of consciousness, cyanosis, and hemodynamically unstable), that was successfully treated with immediate large-size needle decompression.
Keywords: Pneumothorax
CASE REPORT
An 18-year-old male transferred to the emergency department presented loss of consciousness, cyanosis, and deteriorated vital signs. According to the rescue team transfer records, he called the control center himself because he was home alone. He complained of aggravating dyspnea after eating dinner and of sudden onset vomiting. During ambulance transfer, cyanosis was detected and supplemental oxygen was delivered by mask. The patient could not remember what happened after the arrival of the rescue team at his house and had no memory of his stay at the emergency room and intensive care unit (ICU).
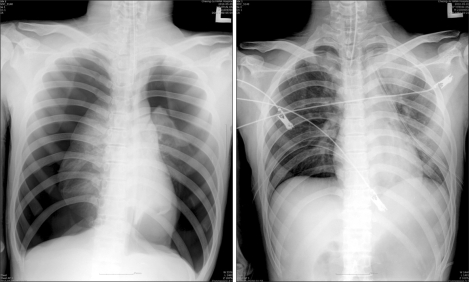
Upon arrival to the emergency room, the patient presented with a cyanotic lip, stupor or semi-comatose mental state, and severe tachyarrhythmia. The percutaneous oxygen saturation level was very low, in the undetectable range. Endotracheal intubation was performed immediately. After drawing blood for an emergency laboratory study and portable chest X-ray, cardiopulmonary resuscitation was performed for several minutes. After confirmation of bilateral tension pneumothorax (Fig. 1), a large bore needle (16 G) was inserted into the second intercostal space of the mid-clavicular line to decompress intrathoracic pressure. Immediately after insertion of the needle, percutaneously checked SaO2 increased dramatically to higher than 95%. Closed bilateral thoracostomy followed, using a 24 Fr chest tube. The patient was transferred to the ICU for close monitoring of the patient's mental state and other parameters related to tension pneumothorax. The ABGA results upon arrival and after insertion of the chest tube were a pH of 7.272, PCO2 of 56.1 mmHg, PO2 of 78.6 mmHg, and SaO2 78.6%, and a pH of 7.373, PCO2 of 42.7 mmHg, PO2 of 171.3 mmHg, and a SaO2 of 99.3%, respectively.
Fig. 1.
X-ray upon admission to the emergency room, showing simultaneous bilateral spontaneous pneumothorax, left. Post-tubing state, right.
Within several hours after admission into the ICU, the patient's mental state and vital signs were restored to within normal limits. Two hours after admission into the ICU, endotrachial intubation was removed and spontaneous breathing was maintained with an adequate SaO2 level. The possibility of hypoxic brain damage was evaluated by a neurosurgeon, who confirmed that there were no significant sequela.
On the second day at the hospital, bilateral pneumothorax recurred during the application of continuous negative wall suction (-18 CmH2O). High resolution lung computed tomography showed multiple bullae in bilateral upper lung fields. A wedge resection was performed using bilateral video assisted thoracic surgery (VATS).
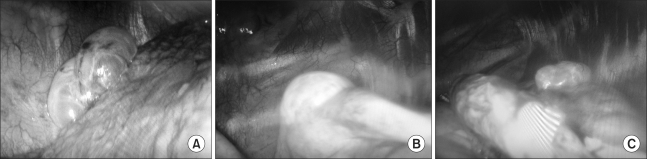
The operation was performed under general anesthesia with double-lumen endotracheal intubation. To avoid hemodynamic instability during the operation, the patient was positioned with the head elevated 30 degrees (Semifowler's position) and with the legs slightly elevated, with both upper arms extended. During the operation, to improve the operation field view, the operation table was tilted to the contralateral side (Fig. 2). A large bullae on the left lung and single giant bulla on right upper lung were resected with an Endo-GIA linear stapling device. One long thoracic drain (28 Fr) was inserted bilaterally into the thoracic cavity after mechanical abrasion of upper portion of the parietal pleura. The postoperative course was uneventful. For two years after the operation, there was no evidence of recurrence of pneumothorax on both sides (Fig. 3).
Fig. 2.
Endoscopic findings: giant bulla on right upper lobe (A), bulla on the left upper lobe (B), and another bulla on the left upper lobe (C).
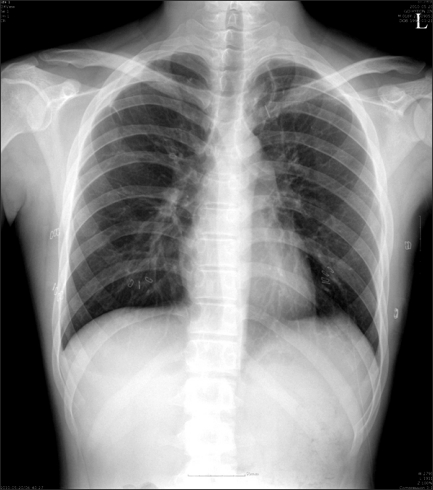
Fig. 3.
X-ray at discharge.
DISCUSSION
The incidence of simultaneous bilateral primary spontaneous pneumothorax has been reported to be as low as 1.4% to 7.6%. Simultaneous bilateral primary spontaneous pneumothorax can result in a severely deteriorated condition, usually requiring intubation or resuscitation. The reported causes of bilateral pneumothorax include trauma, tumor, and iatrogenic causes [1-3]. Other more rare causes have been reported, including catamenial pneumothorax, sarcoidosis, pregnancy, and radiation [4].
Simultaneous spontaneous bilateral tension pneumothorax is defined as when no tracheal shift occurs and when the degree of bilaterally lung collapse is similar in a chest X-ray. Patients with simultaneously developed bilateral tension pneumothorax may deteriorate rapidly, and immediate decompression is recommended. A vicious cycle may occur, leading to a deteriorated condition, with a chain reaction consisting of lowered venous return, lowered preload, lowered cardiac output and so on. The patient under study experienced a critically life threatened state, loss of consciousness, cyanosis, and tachyarrhythmia.
Clinical findings of spontaneous pneumothorax may vary from absence of symptoms to tension penumothorax. The treatment methods include needle aspiration, percutaneous catheter drainage, and tube thoracostomy [1-4]. Indication for surgical management of pneumothorax include continuous air leakage after insertion of chest tube, recurring pneumothorax on the same side, simultaneous bilateral pneumothorax, pneumothorax developed after pneumonectomy, and having an occupational cause [2,4].
At present, Video-Assisted Thoracic Surgery (VATS) is the most frequently used form of surgery for treating pneumothorax [3]. Kim et al. reported a series of 66 patients that were randomized to treatment with either transaxillary minithoracotomy (TAMT) or VATS. The conclusion was that VATS presented no advantages over TAMT. There were several advantages to performing a bilateral single stage operation. First, a smaller incision was required when compared with TAMT, which generally resulted in less pain. Postoperative pain was usually related to several complications. Second, the cosmetic effect is superior to that of TAMT. Finally, most procedures are possible (mechanical pleurodesis, chemical pleurodesis, etc.).
Prospective studies of simultaneous bilateral spontaneous pneumothorax management are rare. Generally, cases of bilateral pneumothorax require definitive surgical therapy to reduce the risk of recurrence [3,5]. This can be done either through VATS or open thoracotomy, depending on the surgeon's preference. Mechanical pleurodesis should be performed to reduce the recurrence rate.
Primary spontaneous pneumothorax frequently affects young, tall, and thin males. Our case presented the rare clinical situation of simultaneous bilateral tension pneumothorax, and a decision was made to treat with immediate large size needle decompression at the emergency room by a properly trained doctor. The procedure was a critical step which restored this patient from life-threatening tension pneumothorax.
References
- 1.Lee SC, Cheng YL, Huang CW, et al. Simultaneous bilateral primary spontaneous pneumothorax. Respirology. 2008;13:145–148. doi: 10.1111/j.1440-1843.2007.01168.x. [DOI] [PubMed] [Google Scholar]
- 2.Rivas de Andrés JJ, Jiménez López MF, Molins López-Rodó L, et al. Guideline for the diagnosis and treatment of spontanesous pneumothorax. Arch Bronconeumol. 2008;44:437–448. doi: 10.1016/s1579-2129(08)60077-4. [DOI] [PubMed] [Google Scholar]
- 3.Kim ES, Sohn ST, Kang JY. Simultaneous bilateral spontaneous pneumothorax. Korean J Thorac Cardiovasc Surg. 2006;39:475–478. [Google Scholar]
- 4.Shields TW. General thoracic surgery. 6th ed. New York: Williams & Wilkins; 2005. pp. 794–805. [Google Scholar]
- 5.Lewis RL. Simultaneous bilateral spontaneous pneumothorax; a case report. Curr Surg. 2002;59:99–100. doi: 10.1016/s0149-7944(01)00608-0. [DOI] [PubMed] [Google Scholar]