Abstract
This study was conducted to investigate the clinical application of three-dimensional (3D) reconstructed computed tomography (CT) images in detecting and gaining information on esophageal foreign bodies (FBs). Two patients with esophageal FBs were enrolled for analysis. In both cases, 3D reconstructed images were compared with the FB that was removed according to the object shape, size, location, and orientation in the esophagus. The results indicate the usefulness of conversion of CT data to 3D images to help in diagnosis and treatment. Use of 3D images prior to treatment allows for rapid prototyping and surgery simulation.
Keywords: Esophageal surgery, Esophageal foreign body, Computed tomography
CASE REPORT
1) Case 1
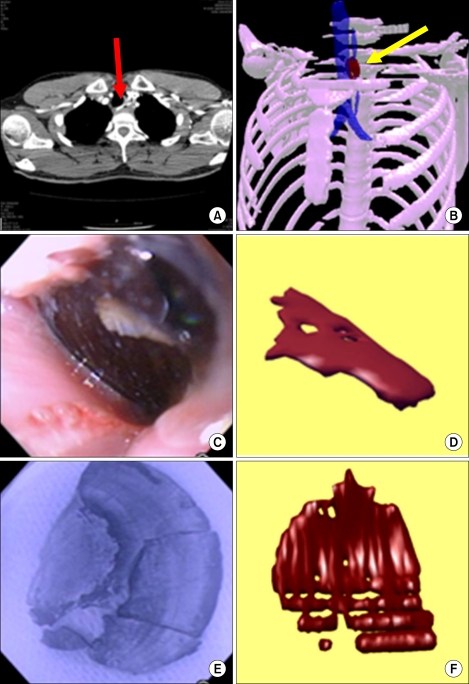
This 34-year-old male patient had an impacted Mytilus coruscus shell in the esophagus. The shell was extracted using flexible fiberoptic endoscopy. Prior to FB removal, the patients received a chest CT after contrast enhancement using a Toshiba Aquillion operating at 120 kVp and 62 mAs, with a slice thickness of 3 mm (Fig. 1).
Fig. 1.
Shell of Mytilus coruscus in case 1. (A) Axial CT image showing an esophageal foreign body (red arrow). (B) Three-dimensional reconstructed image showing the relationship with other structures (yellow arrow). (C) Endoscopic view of shell. (D) Rotation of the reconstructed image to mimic the endoscopic photograph. (E) Endoscope-mediated photograph of the extracted shell. (F) Reconstructed image rotated to mimic the foreign body.
2) Case 2
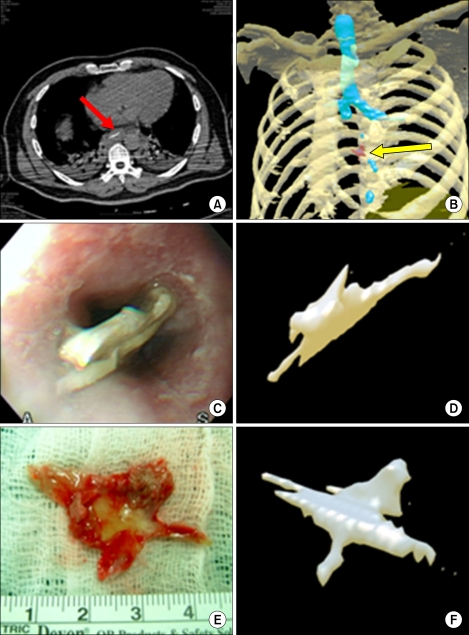
This 52-year-old male patient had a fish bone lodged in the espophagus. The fish bone was removed by open thoracotomy under general anesthesia. Prior to FB removal, the patient received a chest CT after contrast enhancement using a Siemens Navigator operating at 120 kVp and 90 mAs, with a slice thickness of 2 mm (Fig. 2).
Fig. 2.
Fish bone in case 2. (A) Axial CT showing an esophageal foreign body (red arrow). (B) Three-dimensional reconstructed image showing the relationship with other structures (yellow arrow). (C) Endoscopic view of fish bone. (D) Rotation of a reconstructed image to mimic the endoscopic photograph. (E) Extracted fish bone. (F) Reconstructed image rotated to mimic the foreign body.
In both cases, the axial CT data were saved in DICOM file format. To reconstruct the 3D images, 3D-Doctor 4.0 software (Able Software, USA) was used. The captured images were edited with GIMP. The outer surfaces of the FB, skin, bones including vertebrae, inner surface of the trachea, and esophagus were drawn in all frames after detection of the outlines. The 3D images were then created. The esophageal lumen was not fully distended and esophageal images were not perfect. The 3D images and photographs were compared with respect to the shape and location of each FB in the esophagus. After rotation of the 3D images, they looked similar in shape and orientation to the photographs of the FBs that had been removed.
DISCUSSION
Esophageal FBs should be detected and extracted as early as possible. Delays can produce life-threatening complications such as esophageal perforation and mediastinitis [1]. The best means of extracting an esophageal FB is debatable. Although the flexible fiberoptic endoscope is a very popular tool for FB extraction, the rigid esophagoscope is equally safe and represents a good tool in the hands of an experienced surgeon. If endoscopy fails, an open thoracotomy is the method of last resort.
In Asian countries, fish bone impaction is a very common cause of emergency room visits [2,3]. Since fish bones and shells tend to be calcium-rich, they are visible upon routine X-ray examination, if sufficiently large in size. Typically, X-ray examination is followed by a neck or chest CT. Nevertheless, small FBs can still be overlooked. Use of a flexible fiberoptic endoscope can often allow both a definitive diagnosis and extraction of the FB. In the present cases, prompt extraction of the rigid and sharp-edged FBs is necessary, since they can cause erosion and laceration of the esophageal mucosa if left untreated. Endoscopic extraction is not risk-free, and problems that arise can demand emergency surgery [2,4]. Rapid knowledge of an esophageal FB, specifically, its composition (i.e., hard or soft), shape, size, location, and orientation, is vital for a surgeon in tailoring the safest and most effective treatment. Our patients were successfully treated under endoscopy or by thoracotomy with full knowledge about the FB. At the time of the treatment, the CT data had not been converted to 3D images. The 3D reconstructions were made retrospectively, as was the comparison of these image reconstructions with actual photographs. The time required for making the reconstructed image was less than 30 minutes once the chest CT had been acquired, it took even less time when skilled personnel was involved. This shows another example of the practical value of CT reconstruction from the clinical point of view. Therefore, while the present data was not instrumental in the treatment of the patients from which the data was drawn, the potential of CT reconstruction for future cases was confirmed.
In the case of the shell FB, photographs of the shell that was removed were taken without inclusion of a ruler and the images were distorted due to endoscope angles, so measurements were not possible. For this FB, the 3D reconstructed images were helpful in determining the shape, size, and the relative location of the shell, and its orientation in the esophagus. Rotation of the 3D images could be performed to mimic the endoscopic images and to be used in simulation of surgical procedures if needed.
Endoscopic extraction of the fish bone FB caused esophageal laceration. As a result, the patient was required to fast for 7 days until a second endoscopy confirmed healing. In this patient, real photographs and 3D images were available and were used for comparisons of FB size, location (in the 3D image only), and orientation. The measured size was not the same, but was close. The shape in the 3D images was very similar to that in the real FB photograph. The 3D image was rotated to match the endoscopic view of the FB; the accuracy of the result indicates the potential of the approach as a simulation method. Information concerning the distance from a target point to the FB is available with one mouse click. Since CT is calibrated data, the 3D images can always be used for measuring distance.
A 3D reconstructed image from CT data can be converted into a real touchable physical model through rapid prototype (RP) technology. Before operations for cardiac anomaly or bone-destroying cancer surgery, the use of RP can generate a surgical simulation or allow a bone defect to be measured to make implants or flaps [4,5]. Patients with a vessel anomaly, vascular tumor, or stabbing injury can also benefit from the 3D reconstruction technique [6,7].
The use of 3D reconstruction is progressing to whole-body virtual endoscopy. Organs with hollow spaces occupied by fluid or air are the best candidates for virtual endoscopy. The technique has been adapted in the screening for polyps or other space-occupying lesions of the large intestine [8].
Virtual endoscopy has not been attempted frequently for esophagus procedures, since flexible fiberoptic endoscopy is quick and convenient. In contrast, virtual esophagoscopy requires pretreatment with a gas-forming formula and motility-decreasing injections that distend the esophageal lumen to allow full examination of the esophagus. The gas-forming medicine might not be suitable for patients with an esophageal FB because of the danger of leakage of the medicine through damaged esophageal mucosa [9].
Until now, virtual endoscopy has not been tried in patients with esophageal FB. This study retrospectively assessed 3D reconstructions of chest CT images of esophageal FBs. The reconstructions were able to accurately indicate the shape, size, location, and orientation of the FB in the esophagus in two patients. The type of material comprising an FB cannot be determined in the absence of information concerning the ingested material. On the other hand, endoscopy is superior to 3D reconstruction in identifying the composition of an FB. The information in a 3D reconstructed image can be quickly converted into an RP, which can be used to simulate an extraction procedure such as flexible fiberoptic endoscopy or open surgery. Future refinements could see the use of robotic simulated surgery. Finally, the present CT data was acquired in 2- or 3-mm-thick slices. Use of slices of 1 mm thickness or less would provide finer detail, and the resulting 3D reconstruction would even more realistically mimic the FB.
References
- 1.Young CA, Menias CO, Bhalla S, Prasad SR. CT features of esophageal emergencies. Radiographics. 2008;28:1541–1553. doi: 10.1148/rg.286085520. [DOI] [PubMed] [Google Scholar]
- 2.Chang MY, Chang ML, Wu CT. Esophageal perforation caused by fish vertebra ingestion in a seven-month-old infant demanded surgical intervention: a case report. World J Gastroenterol. 2006;12:7213–7215. doi: 10.3748/wjg.v12.i44.7213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hirasaki S, Inoue A, Kubo M, Oshiro H. Esophageal large fish bone (Sea Bream Jawbone) impaction successfully managed with endoscopy and safely excreted through the intestinal tract. Intern Med. 2010;49:995–999. doi: 10.2169/internalmedicine.49.3262. [DOI] [PubMed] [Google Scholar]
- 4.Cheng HT, Wu CI, Tseng CS, et al. The occlusion-adjusted prefabricated 3D mirror image templates by computer simulation: the image-guided navigation system application in difficult cases of head and neck reconstruction. Ann Plast Surg. 2009;63:517–521. doi: 10.1097/SAP.0b013e31819349b9. [DOI] [PubMed] [Google Scholar]
- 5.Sannomiya EK, Silva JV, Brito AA, Saez DM, Angelieri F, Dalben Gda S. Surgical planning for resection of an ameloblastoma and reconstruction of the mandible using a selective laser sintering 3D biomodel. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:e36–e40. doi: 10.1016/j.tripleo.2008.01.014. [DOI] [PubMed] [Google Scholar]
- 6.Cho SH, Lee HC, Park CW. CT angiography with 3D reconstruction for the initial evaluation of penetrating neck injury with retained knife. Otolaryngol Head Neck Surg. 2007;136:504–505. doi: 10.1016/j.otohns.2006.08.015. [DOI] [PubMed] [Google Scholar]
- 7.Choi EY, Yoon YW, Kwon HM, et al. A case of pulmonary artery intimal sarcoma diagnosed with multislice CT scan with 3D reconstruction. Yonsei Med J. 2004;45:547–551. doi: 10.3349/ymj.2004.45.3.547. [DOI] [PubMed] [Google Scholar]
- 8.Nelson NJ. Virtual colonoscopy accepted as primary colon cancer screening test. J Natl Cancer Inst. 2008;100:1492–1499. doi: 10.1093/jnci/djn403. [DOI] [PubMed] [Google Scholar]
- 9.Panebianco V, Grazhdani H, Iafrate F, et al. 3D CT protocol in the assessment of the esophageal neoplastic lesions: can it improve TNM staging? Eur Radiol. 2006;16:414–421. doi: 10.1007/s00330-005-2851-5. [DOI] [PubMed] [Google Scholar]