Abstract
The relationship between intimate partner violence (IPV) and HIV risk is well documented, but few interventions jointly address these problems. We developed and examined the feasibility of an intervention to reduce HIV risk behaviors among 97 women seeking services for IPV from a community-based NGO in Johannesburg, South Africa. Two versions of the intervention (a 6-session group and a 1-day workshop) were implemented, both focusing on HIV prevention strategies integrated with issues of gender and power imbalance. Attendance was excellent in both intervention groups. Assessments were conducted at baseline, post-intervention and two-month follow-up to demonstrate the feasibility of an intervention trial. Women in both groups reported reductions in HIV misperceptions and trauma symptoms, and increases in HIV knowledge, risk reduction intentions, and condom use self-efficacy. The 6-session group showed greater improvements in HIV knowledge and decreases in HIV misperceptions in comparison to the 1-day workshop. The study demonstrated the feasibility and potential benefit of providing HIV prevention intervention to women seeking assistance for IPV.
Keywords: Intimate partner violence, HIV prevention, Women, Group intervention, South Africa
Introduction
Women who experience violence from an intimate partner have heightened susceptibility to HIV, and there is a clear need for integrated approaches to address these two public health problems [1]. Intimate partner violence (IPV) is defined as any behavior within an intimate relationship that causes physical, psychological or sexual harm, including physical aggression, psychological abuse, sexual coercion, or efforts to control the mobility or freedom of a partner [2]. IPV is common in women’s relationships in South Africa [3, 4], and physical and sexual assault are reported by large percentages of women across multiple South African provinces [5–7]. Concepts of masculinity that are rooted in gender inequality and the violence of post-Apartheid South Africa continue to fuel IPV [8–10]. In a study of men in Cape Town, 44% acknowledged abusing a female partner, with 66% using physical abuse and 34% using both physical and sexual abuse [11].
South Africa not only has one of the highest rates of IPV [2], but is also among the countries hardest hit by the HIV epidemic, with women comprising the majority of the estimated 5.4 million HIV infected adults (18.1% of the adult population) [12, 13]. Women’s vulnerability to HIV is both biological and social. Biologically, women have a higher risk of HIV acquisition per vaginal sex act, as compared with men [14, 15], which is exacerbated by the presence of reproductive tract infections, sexually transmitted and otherwise, which often go undiagnosed in women [16–18]. Socially, women are at greater risk of HIV because gender inequalities limit women’s ability to negotiate the terms of sex and to introduce risk reduction measures [19].
The most extreme form of gender inequality is IPV, which has been strongly associated with HIV risk and infection in women [1, 20, 21]. IPV contributes both directly and indirectly to HIV risk. In cases of sexual coercion and forced sex, women have little opportunity to refuse sex or negotiate the terms of sex, and unwanted sex may result in the tearing of vaginal and/or anal tissue, facilitating entry of the virus [22]. Indirectly, women who lack power and control in their relationships have difficulty practicing safe sex behaviors such as condom negotiation [23, 24], a situation that has been coined as “choice disability” [25]. IPV may also increase HIV risk behaviors through pathways such as depression and substance use [26].
Despite the high prevalence of IPV and its role in the spread of HIV in South Africa, little has been done to address the HIV risk of women who experience IPV. Traditional HIV prevention messages are often inappropriate for women because they assume a level of choice and control in relationships, which women in violent relationships do not have [27]. Several interventions addressing violence in the context of HIV prevention have been developed and tested in South Africa, with mixed results [28–32]. However, to our knowledge, there are no empirically-supported interventions that address HIV prevention for identified survivors of IPV, or that are delivered in IPV service agencies. Community-based organizations that provide services to IPV victims may be well placed to deliver HIV prevention services to these women. Women who seek out services are demonstrating a state of readiness to take action in their lives and relationships [33], which could be harnessed for introducing HIV prevention.
To address this gap, we developed an HIV prevention intervention with a specific focus on gender issues and power imbalance for women who had experienced IPV, and explored the feasibility of the intervention in this context. The study compared two versions of this intervention, a 6-session group intervention and 1-day workshop, both implemented in a community organization that provides direct services to IPV survivors. Two important issues to address with regard to the feasibility of the interventions were whether (1) women seeking services for IPV in a community-based, nongovernmental organization would attend group sessions, and if so (2) would feasibility differ for a multiple or single session intervention.
Methods
Procedures
Study participants were 97 women (age 18 or older) seeking abuse-related services, primarily IPV and/or sexual assault, at a Johannesburg based NGO (POWA: People Opposing Women Abuse). Women were recruited from January 2003 to March 2004 at five sites (two shelters and three drop-in clinics). Women seeking services were told of the study and given an informational brochure on the project in Zulu, Sotho or English.
Following provision of written informed consent, trained interviewers individually and privately administered a baseline assessment interview in Zulu, Sotho or English per participant request. Women were assigned to a 1-day workshop or a 6-session group intervention, based on preference, due to our concern that abused women in potentially controlling relationships may be prevented or at risk of violence from attending weekly group sessions or a full day session, depending on their unique circumstances. One block of participants containing one group of each intervention type (approximately n = 20; 10 per intervention group) was recruited at each of the five study sites.
The 6-session intervention was delivered in 90 min weekly sessions (when necessary, given limited durations of stay in shelters, in three sessions a week over two weeks), for a total of nine intervention hours. The 1-day workshop had a six-hour curriculum, including a lunch/social period. A post intervention assessment was administered approximately 2 weeks following the intervention (2 months post baseline), and a follow-up assessment was administered 2 months following the post assessment (4 months post baseline).
Measures
Demographic Data
Participants provided data on their age, educational level, ethnicity, income, and marital/relationship status.
HIV Risk Behavior Knowledge [34, 35]
Practical understanding of HIV risk behavior was assessed using a 24-item true–false scale (α = 0.63).
HIV Misperceptions
An 8-item scale was developed to assess misperceptions regarding HIV (α = 0.66). Items asked how strongly the respondent agrees or disagrees with statements such as: “HIV affects only poor people” and “Traditional healers can cure AIDS.”
Risk Reduction Behavioral Intentions [34, 35]
Intention to perform HIV risk-reduction behaviors was assessed with a 7-item scale (α = 0.74).
Risk Reduction Self Efficacy
A 7-item scale was used to measure participant’s self efficacy to apply HIV risk reduction strategies (α = 0.82). The items were anchored on a 10-point scale ranging from “very sure I can’t” to “very sure I can”, and included questions about how confident they were that they could “talk with a partner about HIV”, “stay away from situations that might lead to unprotected sex”, and “put on a condom correctly”.
Trauma Symptoms [36]
The Trauma Symptom Checklist (TSC-40) was used to assess symptoms associated with traumatic experiences, including aspects of posttraumatic stress and other symptom clusters found in some traumatized individuals (α = 0.94). It includes 40 questions about the frequency of symptoms (e.g., flashbacks, sexual problems, uncontrollable crying) over the past 2 months. Responses are on a four-point scale, from “never” to “often”.
Intimate Partner Violence [37]
The Conflict Tactics Scale was used to measure women’s experiences of IPV. The measure includes 39 different descriptions of abuse that fall into five sub-scales: physical assault, sexual coercion, psychological aggression, negotiation, and injury. For each abuse descriptor, the participant was asked to report whether she had ever experienced it; and if so, how often in the last year.
Sexual Behavior Practices [35]
Participants self-reported: (1) number of lifetime partners; (2) number of partners in the past 2 months; (3) type of partner (main and other); (4) number of vaginal and anal intercourse occasions in the past 2 months; and (5) number of times condoms were used during intercourse in the past 2 months.
HIV Testing and Sexually Transmitted Infection (STI) Treatment History [38]
Participants were asked whether they had been tested for HIV, and if so, the results. They were also asked whether they ever received treatment for an STI, and if they had symptoms of or treatment for an STI in the past year and in the past 3 months.
Process Data
Participants had an opportunity to provide intervention feedback using a brief evaluation guide, which included six open-ended questions about aspects of the intervention that were most and least helpful, and how the intervention has impacted their perceptions and intentions. The feedback was provided individually in written form or in a group session, depending on participants’ preferences. When discussed orally, comments were recorded by a note taker.
Group facilitators provided feedback through weekly debriefing meetings of the study team. In these sessions, facilitators shared their insights into the conduct of the intervention, including their perceptions of participants’ experiences, aspects of the intervention that were easy or difficult to implement, and suggestions for changes in the intervention. Detailed notes were taken by the facilitator of the feedback sessions. All process data were reviewed by the study coordinator, and key themes were identified.
Intervention
Following formative qualitative research with POWA clients [39] and in collaboration with POWA counselors, we developed an intervention that was culturally tailored and socially appropriate for women seeking services at POWA. The primary goal of the intervention was to integrate HIV prevention strategies with issues of gender, power imbalance, and abuse. The intervention content focused on: (1) understanding abuse and trauma, including its association with HIV risk, (2) knowledge about HIV/AIDS and risk behaviors, (3) condom use, including strategies for over-coming barriers, (4) communication, negotiation and problem solving skills, (5) empowerment approaches that include economic independence and negotiating gender roles, and (6) violence, HIV risk and coping. A theme across all sessions was the position of women within society, and how gender norms and identities directly influence women’s lives. The approach was largely participatory, including discussions, role plays, hands-on exercises and small group work. The facilitators were careful to set a non-judgmental tone and built solidarity among the group members. Based on participant needs, groups were conducted in a mix of Zulu, Sotho and English.
All intervention sessions in both conditions were co-facilitated by African female group leaders, including both research staff from the University of Pretoria with expertise in HIV prevention and gender issues and POWA counselors experienced with providing services to abused women. Facilitators received a three-day training, which included an overview of the background areas (IPV and HIV) and the implementation of the intervention sessions. Facilitators were trained on an approach of “radical listening”, which focuses on external oppressive conditions that may have been internalized, so not to attribute problems to the individual [40]. Debriefing sessions following the training helped to reinforce material and address any questions or concerns prior to implementation. Monitoring and procedural protocols were established to ensure fidelity of field activities to study protocol.
The two versions of the intervention were implemented with similar content and delivery. The 1-day workshop represented a distillation of the 6-session intervention, but with less emphasis on skills building exercises.
Data Analysis
To examine the feasibility of conducting an intervention trial, we administered a series of standardized measures at three time points over the study period. Changes in psychosocial measures and traumatic symptoms were evaluated by comparing variables of interest before and after the intervention. Repeated-measures ANOVAs were used, in which intervention format (1 day workshop vs. 6 weekly sessions) served as the between-subjects variable, and time (baseline to post) served as the within-subjects variable. Two additional exploratory analyses were conducted. Sexual behavior was examined among a subgroup of women, specifically, only those who had engaged in unprotected sexual activity at baseline. To explore relationship termination as a potential HIV risk reduction strategy, logistic regression was used to determine whether intervention condition predicted relationship status post-intervention, while controlling for baseline relationship status. All analyses were repeated to evaluate changes from baseline to follow up.
Missing responses within a scale were replaced by the scale mean. Sexual risk responses were taken from the overall sexual behavior questions and were corroborated by responses to specific sexual behavior questions with main and other partners. Analyses were conducted using SPSS version 12.
Results
Sample Demographics
The 97 women who participated in the study had a mean age of 36 years. Almost all women (88%) had at least one biological child, with a mean of two children. The women were from a low socio-economic background, with 79% having less than a high school education, 77% earning less than R500 (about 80 USD at the time of the study) per month, and 81% having no formal employment. Ninety-four percent of the population was of African ethnicity. Approximately one-third reported Zulu as their mother tongue, and another one-third Sotho. About one-third of the women were residing at a POWA shelter, with the remainder receiving POWA services as drop-in clients.
As expected, experience of abuse by an intimate partner was high in the sample. In the past year, 63.6% of women had experienced physical assault; 75.3% psychological abuse; 55.7% sexual coercion; and 56.8% had some injury as a result of partner abuse. A history of sexual abuse was also common, with 81% reporting some type of sexual abuse in her lifetime. Over half reported sexual abuse as an adult, and 38 and 42% reporting abuse as a child or adolescent, respectively. At baseline, almost half of the respondents reported that they had tested for HIV, and of those, 17% said they received a positive diagnosis. Almost half the sample (49/97) reported that they had engaged in vaginal or anal sex in the previous 2 months. More than one-third reported having experienced a sexually transmitted infection (STI).
Forty-five women were allocated to the 6-session group, and 52 to the 1-day workshop (Fig. 1). Despite non-random assignment, women did not differ between conditions on baseline demographic or outcome measures, except mother tongue and HIV testing. Women in the 6-session group more likely to be raised speaking Zulu (60.5% vs. 25%, χ2 = 11.03, P<0.01), and among those who had tested for HIV, were more likely to report that they returned for their result (100% vs. 80%, χ2 = 6.21, P<0.05).
Fig. 1.
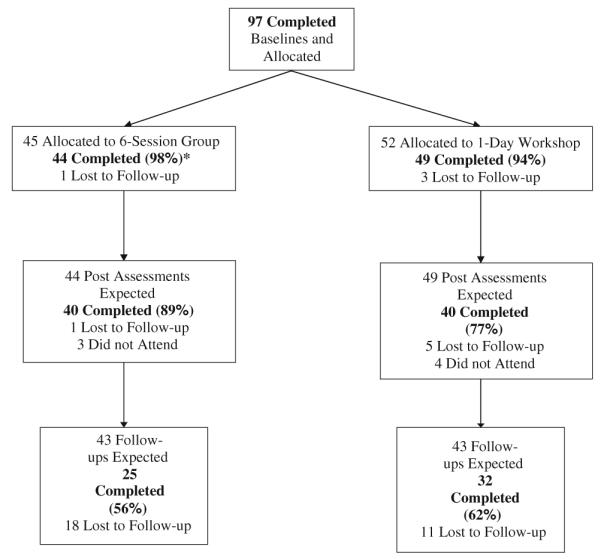
Recruitment flow chart. *: Individuals were considered to have completed the 6-session group if they attended 5 or more sessions; **: All percentages are calculated from the initial number allocated to each intervention
Attendance and Retention
Of those assigned to the 6-session group, 98% attended 5 or more of the 6-session groups; for the 1-day workshop, 94% attended both the morning and afternoon sessions. The large majority of participants (83%) completed the post assessment. However, more difficulties arose in locating participants at the follow-up (a 59% completion rate; Fig. 1). Women in the shelters tended to be less likely to complete the follow-up compared with women in the drop-in centers (47% vs. 65%, χ2 = 2.96, P = 0.085). Attrition did not differ by intervention condition.
Psychosocial and Trauma Indicators
Table 1 presents the means for the psychosocial variables (HIV knowledge, HIV misperceptions, risk reduction intentions, risk reduction self efficacy, and trauma symptoms) by intervention group and assessment point. In all psychosocial domains, individuals in both intervention conditions showed improvement over time at the post assessment (Table 2). These effects were maintained at follow-up, with the exception of HIV misperceptions and risk reduction intentions.
Table 1.
Means for psychosocial and behavioral outcomes by study condition and assessment point
| Pre-intervention |
Post-intervention |
Follow up |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Mean | SD | N | Mean | SD | N | Mean | SD | |
| Psychosocial outcomes | |||||||||
| HIV Knowledge | |||||||||
| 1-Day workshop | 52 | 17.03 | 2.73 | 39 | 19.54 | 2.82 | 29 | 19.97 | 2.56 |
| 6-Session group | 44 | 16.05 | 3.84 | 40 | 20.63 | 2.98 | 23 | 21.17 | 1.72 |
| HIV Misperceptions | |||||||||
| 1-Day workshop | 52 | 6.23 | 3.15 | 39 | 6.41 | 2.93 | 29 | 5.35 | 3.46 |
| 6-Session group | 44 | 7.02 | 3.15 | 40 | 4.50 | 3.77 | 23 | 5.26 | 3.53 |
| Risk reduction intensions | |||||||||
| 1-Day workshop | 52 | 15.27 | 3.03 | 39 | 16.30 | 3.25 | 29 | 16.90 | 3.12 |
| 6-Session group | 44 | 14.98 | 2.93 | 40 | 17.15 | 3.26 | 23 | 15.26 | 3.40 |
| Risk reduction self efficacy | |||||||||
| 1-Day workshop | 51 | 56.73 | 15.14 | 39 | 62.26 | 15.95 | 28 | 65.61 | 9.96 |
| 6-Session group | 44 | 58.89 | 13.80 | 38 | 67.13 | 5.96 | 23 | 66.91 | 9.62 |
| Trauma symptomatology | |||||||||
| 1-Day workshop | 52 | 45.39 | 25.27 | 39 | 30.48 | 22.07 | 29 | 26.35 | 24.17 |
| 6-Session group | 44 | 47.72 | 24.55 | 39 | 36.93 | 27.91 | 23 | 30.77 | 24.51 |
| Behavioral outcomesa | |||||||||
| Proportion of unprotected sex | |||||||||
| 1-Day workshop | 18 | 0.60 | 0.50 | 18 | 0.33 | 0.49 | 10 | 0.30 | 0.48 |
| 6-Session group | 20 | 0.55 | 0.47 | 20 | 0.36 | 0.48 | 14 | 0.21 | 0.41 |
| Number of partners | |||||||||
| 1-Day workshop | 18 | 1.11 | 0.47 | 18 | 0.67 | 0.77 | 10 | 0.60 | 0.52 |
| 6-Session group | 20 | 1.15 | 0.49 | 20 | 0.80 | 0.77 | 14 | 0.50 | 0.52 |
Includes only those who engaged in sex at baseline
Table 2.
Repeated measures ANOVAs comparing pre-intervention to post-intervention and follow-up
| df | F (pre-post) |
F (pre-post by intervention) |
df | F (pre-FU) |
F (pre-FU by intervention) |
|
|---|---|---|---|---|---|---|
| Psychosocial outcomes | ||||||
| HIV Knowledge | (1, 76) | 80.70*** | 5.38* | (1, 50) | 111.5*** | 0.71 |
| HIV Misperceptions | (1, 76) | 4.59* | 9.40** | (1, 50) | 2.21 | 0.69 |
| Risk reduction intentions | (1, 76) | 11.49*** | 1.52 | (1, 50) | 3.14**** | 1.67 |
| Risk reduction self efficacy | (1, 73) | 10.04** | 0.15 | (1, 49) | 9.47** | 2.06 |
| Trauma symptomatology | (1, 76) | 16.08*** | 1.30 | (1, 50) | 24.64*** | 0.25 |
| Behavioral outcomesa | ||||||
| Proportion of unprotected sex | (1, 36) | 6.20* | 0.19 | (1, 22) | 6.23* | 0.44 |
| Number of partners | (1, 36) | 19.58*** | 0.28 | (1, 22) | 12.35** | 0.06 |
includes only those who engaged in sex at baseline
P<.05,
P<.01,
P ≤ .001,
P<.10
Comparing the two conditions, the 6-session group intervention showed significant improvement over the 1-day workshop in improving HIV knowledge and dispelling misperceptions at the post assessment (Table 2). However, at follow-up there were no differences between the conditions in any of the psychosocial domains.
Sexual Behavior Indicators
Table 1 presents the means for the behavioral variables (proportion of sex that was unprotected and number of sex partners) by intervention group and assessment point. Women in both intervention conditions had reduced these HIV risk behaviors at the post and follow-up assessments (Table 1). Comparing the two conditions, there were no significant differences in these behavioral variables (Table 2). However, logistic regression analysis showed that those in the 6-session group were less likely to be in a relationship at post than those in the 1-day workshop, after controlling for baseline relationship status (OR = 0.32, 95% CI = 0.12, 0.91, P<.05), although this difference was not maintained at the follow-up assessment.
Process Data
An increase in social support was an important outcome of the intervention. Participants expressed that they felt comforted to be in a group setting with other survivors of abuse who were seeking help. Some groups felt so strongly supported that they went on to form their own support groups that continued after the intervention. An interesting age dynamic occurred in the group, whereby the older women showed a great deal of support and compassion for younger members, encouraging and reassuring them as they made transitions out of abusive relationships.
With regard to addressing the intersection of HIV risk and abuse, a few themes were noteworthy. The sessions on abuse and HIV risk, and sexual communication and problem solving were well-liked and highly interactive. While it was relatively easy to find a suitable definition in Zulu and Sotho for “abuse,” doing so for “trauma” proved more difficult. For training purposes, trauma was defined as “a wound in one’s soul” and translated into local languages. In the context of discussing relevant terms related to sexual activity (e.g., masturbation, anal sex, and semen), interesting questions arose such as: “Why are specific sexual acts not discussed?” “Why are such terms considered taboo?” “How do social expectations influence sexuality and related practices?” Not surprisingly, the session on abuse, violence, HIV risk and coping was considered the most sensitive session. To develop adaptive strategies for coping with abuse and violence, and prevention of HIV, facilitators created an environment that allowed for disclosure and open emotional expression. Small group (2–3 women) and relaxation exercises were utilized before full group discussion to provide emotional intimacy and support. Women acknowledged internal (low self esteem, shame, depression) and external (stigma, revictimization in the criminal justice system) factors as barriers to adaptive coping. In addition, the intervention provided skill development related to communication and problem solving. The intervention explicitly addressed the possibility that implementing risk reduction strategies such as condom use, sexual assertiveness or communication about HIV/AIDS may place women at greater risk for violence from a partner. Examples of this include deciding whether or not to negotiate safer sex, availability of alternative solutions to provide safety, identification of unsafe situations that may lead to coercion or abuse, and empowerment strategies more likely to end rather than increase violence.
Comparing the two intervention formats, the facilitators preferred the 6-week intervention modality, as it provided more time to address participant questions and concerns and had a sense of continuity. The facilitators perceived that the multi-session format allowed more trust to develop, time to process issues and make important connections between abstract concepts and participants’ own life experiences, and provided an opportunity to utilize new skills and coping strategies developed in the group sessions.
Discussion
Women who have experienced or are currently experiencing IPV are at greater risk for HIV [20, 21, 41], and may benefit from appropriately tailored HIV prevention interventions. In particular, women who are actively seeking services for IPV may be in a particular state of “readiness” to accept and integrate new information and skills regarding HIV prevention. This study supports the feasibility of an HIV prevention intervention targeted to women seeking services for IPV in South Africa, and the acceptability of conducting an intervention research trial in collaboration with an NGO providing social services to these women.
This feasibility study provided an excellent opportunity to engage in a collaborative effort to address client concerns and research design dilemmas within a service agency. As noted, POWA staff and counselors were initially concerned whether women would attend group sessions, questioned if attendance at a multi-session intervention was possible within an abusive context, and were understandably reluctant to offer either a no treatment control condition or a comparison condition that did not address abuse and HIV. From the research perspective, it was unknown whether women seeking services for IPV would be interested in research participation, would be willing to complete research related assessments, and what issues would arise with regard to attrition in this context.
Attendance was exceptionally high at both the 6-session group (98% attended 5 or more of the 6 sessions) and the 1-day workshop (94% attended both morning and afternoon sessions). This serves as confirmation of women’s interest in the topic of HIV prevention, and the relevance to their lives and situations. Our retention of women for post assessments 2 weeks following the intervention was acceptable (83% completed a post assessment), but only 59% were able to be contacted to complete the follow up assessment 2 months later. Women in shelters were less likely to complete the follow-up assessment compared with women in the drop-in clinics, and it was frequently difficult to locate residents after they left the shelters. The mobility of this population is something that needs to be considered for future research studies.
Both versions of the group intervention suggested a positive impact on psychosocial outcomes. Post intervention, participants reported better HIV knowledge, fewer HIV misperceptions, more intentions to reduce HIV risk, better self efficacy to use condoms, and fewer trauma symptoms. Most of these effects remained when comparing the baseline to the follow-up period, suggesting that the interventions may have a longer term effect. Sexual risk behavior appeared to decline at post and follow-up; however, given the limited number of participants who engaged in risk behavior at baseline, this needs further assessment with a larger sample before proper conclusions can be drawn.
Comparing the two versions of the intervention at the post assessment, the 6-session group had greater impact on improving HIV knowledge and decreasing HIV misperceptions. In addition, participants in the 6-session group were more likely than their counterparts in the 1-day workshop to say that they were not in a relationship at the post assessment, controlling for their baseline relationship status. While these condition differences were not maintained at the follow-up assessment, this could be due to the lack of power as a consequence of attrition. The impact of a multi-session intervention, compared with a one-time intervention, may be attributable to the peer and social support developed during, and possibly maintained following, the group intervention. While social support can be a beneficial attribute in all group interventions, it may be particularly salient in an intervention for women coping with IPV. Survivors of abuse often face stigma from their families and communities, and have internalized shame about their experiences. A group intervention can help to address stigma and shame and may help women develop social support to constructively deal with their situations. Process data indicated that social support was an important by-product of the intervention.
A key finding in this feasibility study is that women experiencing IPV did attend a group intervention. And, if offered a preference, our findings indicate that many will choose a multiple session intervention format and attend the large majority of the sessions. Facilitators indicated that the six-week modality had potential benefits over the one-day workshop, because it provided more time to address questions and concerns; led to more trust and support; and provided time to develop and implement new skills and coping strategies in the context of difficult issues. However, if future research suggested that a 1-day workshop can have similar effects, this would be important for the translation of research into practice.
While our study strongly supports the feasibility of this intervention, the design was limited by several factors with regard to drawing conclusions from our psychosocial and behavioral assessments and identified areas to consider in the conduct of a research trial. First, women were allowed to choose the intervention condition they participated in because we felt that women needed the option of choosing either a multi-day or full-day workshop, depending on perceived risks in their potentially violent relationships. Although we did not find any statistically significant differences between the two groups at baseline, it is reasonable to assume that women who self-selected the 1-day workshop were somehow different than those who self-selected the 6-session group, although this was not evident in the characteristics assessed in the study. We therefore run the risk of falsely attributing differences to our intervention conditions. Future research could be conducted using either a nonrandomized study design or randomization to an experimental or comparison intervention within the multiple and single session selection structure. Second, we were only able to perform exploratory analysis on behavioral outcomes with women who reported sexual activity at baseline and completed the post or follow-up assessments. Only 38 women met these conditions, limiting the power of our analysis and any potential conclusions. Third, the difficulty reaching women for the 2 month follow up assessment further reduced the number of respondents in our analysis, highlighting the challenges of medium- to long-term follow up of this population. After receiving abuse related services at the study site, shelters in particular, women may have relocated to different parts of the city or country in order to escape abusive partners. Additionally, those who returned to abusive relationships may have been fearful of returning for a follow-up assessment. Fourth, generalizability to the larger population of abused women in South Africa is limited as women in this study were seeking abuse related services and likely represent a more empowered group. And finally, our lack of a control condition made it impossible to separate the effect of the intervention from the over-time effect of being in services at the study NGO. Although this is a significant limitation of our study design, our collaborative team felt that including a waitlist or no treatment control condition would detract from our evaluation of the feasibility of implementing the two versions of our intervention in the service setting. In fact, our findings suggest that integrating HIV prevention into services offered to women experiencing IPV may actually maximize a window of opportunity for HIV prevention.
Individual behavioral interventions focused on HIV risk alone are likely insufficient to reduce sexual-risk behavior among women experiencing IPV. Women may fail to attend to risk-reduction messages given their preoccupation with personal safety and may lack the means to implement risk reduction due to the nature and consequences of IPV in their intimate relationships. Attempting to implement safe sex practices may even put women at greater risk, by serving as a trigger for physical or sexual violence. HIV prevention interventions for women who are currently or recently in violent relationships must therefore address the context of these relationships and sexual practices, and be mindful of women’s history of trauma and abuse. It is important that women in violent relationships develop HIV prevention skills that can be effectively and safely applied in their current unequal partnership, and that they have structural and institutional options available to them to support leaving the relationship if they choose. Integrating HIV prevention into ongoing services provided to abused women addresses these concerns, and findings from this study support the feasibility of such an approach. Intervention trials are needed to ascertain the efficacy and longer term impact of multi-component interventions that address HIV risk and IPV.
Acknowledgments
This research was supported by grants WAF 244 (01-016) (awarded to Kathleen Sikkema, Ph.D.) from the World AIDS Foundation, D43-TW05808 from the NIH Fogarty International Center, P30-MH62294 Center for Interdisciplinary Research on AIDS (CIRA), and P30-AI064518 (Duke Center for AIDS Research). The authors gratefully acknowledge our community collaboration with People Opposing Women Abuse (POWA) in Johannesburg.
Contributor Information
Kathleen J. Sikkema, Department of Psychology and Neuroscience, Duke University, Box 90086, Durham, NC 27708-0086, USA
Sharon A. Neufeld, School of Medicine, Yale University, New Haven, CT, USA; Department of Social and Developmental Psychology, University of Cambridge, Cambridge, UK
Nathan B. Hansen, School of Medicine, Yale University, New Haven, CT, USA
Rakgadi Mohlahlane, Centre for the Study of AIDS, University of Pretoria, Pretoria, South Africa.
Madri Jansen Van Rensburg, People Opposing Women Abuse, Johannesburg, South Africa.
Melissa H. Watt, Global Health Institute, Duke University, Durham, NC, USA
Ashley M. Fox, Mailman School of Public Health, Columbia University, New York, NY, USA
Mary Crewe, Centre for the Study of AIDS, University of Pretoria, Pretoria, South Africa.
References
- 1.Coker AL. Does physical intimate partner violence affect sexual health? A systematic review. Trauma Violence Abuse. 2007;8(2):149–77. doi: 10.1177/1524838007301162. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization . World Report on Violence and Health. WHO; Geneva: 2002. [Google Scholar]
- 3.Jewkes R, Penn-Kekana L, Levin J, Ratsaka M, Schrieber M. “He must give me money, he musn’t beat me”: violence against women in three South African provinces. South African Medical Research Council; Pretoria, South Africa: 1999. [PubMed] [Google Scholar]
- 4.Kalichman SC, Simbayi LC. Sexual assault history and risks for sexually transmitted infections among women in an African township in Cape Town, South Africa. AIDS Care. 2004;16(6):681–9. doi: 10.1080/09540120410331269530. [DOI] [PubMed] [Google Scholar]
- 5.Hoffman S, O’Sullivan LF, Harrison A, Dolezal C, Monroe-Wise A. HIV risk behaviors and the context of sexual coercion in young adults’ sexual interactions: results from a diary study in rural South Africa. Sex Transm Dis. 2006;33(1):52–8. doi: 10.1097/01.olq.0000187198.77612.d8. [DOI] [PubMed] [Google Scholar]
- 6.Wood K, Jewkes R. Violence, rape, and sexual coercion: every-day love in a South African township. Gend Dev. 1997;5(2):41–6. doi: 10.1080/741922353. [DOI] [PubMed] [Google Scholar]
- 7.Jewkes R, Penn-Kekana L, Levin J, Ratsaka M, Schrieber M. Prevalence of emotional, physical and sexual abuse of women in three South African provinces. S Afr Med J. 2001;91(5):421–8. [PubMed] [Google Scholar]
- 8.Wood K, Maforah F, Jewkes R. “He forced me to love him”: putting violence on adolescent sexual health agendas. Soc Sci Med. 1998;47(2):233–42. doi: 10.1016/s0277-9536(98)00057-4. [DOI] [PubMed] [Google Scholar]
- 9.Wood K, Lambert H, Jewkes R. “Showing roughness in a beautiful way”: talk about love, coercion, and rape in South African youth sexual culture. Med Anthropol Q. 2007;21(3):277–300. doi: 10.1525/maq.2007.21.3.277. [DOI] [PubMed] [Google Scholar]
- 10.Ragnarsson A, Onya HE, Thorson A, Ekstrom AM, Aaro LE. Young males’ gendered sexuality in the era of HIV and AIDS in Limpopo Province, South Africa. Qual Health Res. 2008;18(6):739–46. doi: 10.1177/1049732308318373. [DOI] [PubMed] [Google Scholar]
- 11.Abrahams N, Jewkes R, Laubsher R. “I do not believe in democracy in the home”: men’s relationships with and abuse of women. South African Medical Research Council; Pretoria, South Africa: 1999. [Google Scholar]
- 12.UNAIDS 2008 . Report on the global AIDS epidemic. Geneva: 2008. [Google Scholar]
- 13.South African Department of Health . The national HIV and syphilis prevalence survey of South Africa. South African Department of Health; Pretoria, South Africa: 2007. [Google Scholar]
- 14.European Study Group on Heterosexual Transmission of HIV Comparison of female to male and male to female transmission of HIV in 563 stable couples. BMJ. 1992;304(6830):809–13. doi: 10.1136/bmj.304.6830.809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Turmen T. Gender and HIV/AIDS. Int J Gynaecol Obstet. 2003;82(3):411–8. doi: 10.1016/s0020-7292(03)00202-9. [DOI] [PubMed] [Google Scholar]
- 16.Atashili J, Poole C, Ndumbe PM, Adimora AA, Smith JS. Bacterial vaginosis and HIV acquisition: a meta-analysis of published studies. AIDS. 2008;22(12):1493–501. doi: 10.1097/QAD.0b013e3283021a37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martin HL, Richardson BA, Nyange PM, et al. Vaginal lactobacilli, microbial flora, and risk of human immunodeficiency virus type 1 and sexually transmitted disease acquisition. J Infect Dis. 1999;180(6):1863–8. doi: 10.1086/315127. [DOI] [PubMed] [Google Scholar]
- 18.Freeman EE, Weiss HA, Glynn JR, Cross PL, Whitworth JA, Hayes RJ. Herpes simplex virus 2 infection increases HIV acquisition in men and women: systematic review and meta-analysis of longitudinal studies. AIDS. 2006;20(1):73–83. doi: 10.1097/01.aids.0000198081.09337.a7. [DOI] [PubMed] [Google Scholar]
- 19.Gupta G. Gender, sexuality and HIV/AIDS: the what, the why, and the how. plenary address, XIIIth international AIDS conference; Durban, South Africa: 2000. [Google Scholar]
- 20.Maman S, Mbwambo JK, Hogan NM, et al. HIV-positive women report more lifetime partner violence: findings from a voluntary counseling and testing clinic in Dar es Salaam, Tanzania. Am J Public Health. 2002;92(8):1331–7. doi: 10.2105/ajph.92.8.1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dunkle KL, Jewkes RK, Brown HC, Gray GE, McIntryre JA, Harlow SD. Gender-based violence, relationship power, and risk of HIV infection in women attending antenatal clinics in South Africa. Lancet. 2004;363(9419):1415–21. doi: 10.1016/S0140-6736(04)16098-4. [DOI] [PubMed] [Google Scholar]
- 22.HRW Deadly delay: South Africa’s efforts to prevent HIV in survivors of sexual violence. Hum Rights Watch. 2004;16(3):75. [Google Scholar]
- 23.Karim AQ. Barriers to preventing human immunodeficiency virus in women: experiences from KwaZulu-Natal, South Africa. J Am Med Womens Assoc. 2001;56(4):193–6. [PubMed] [Google Scholar]
- 24.Karim QA, Karim SS, Soldan K, Zondi M. Reducing the risk of HIV infection among South African sex workers: socioeconomic and gender barriers. Am J Public Health. 1995;85(11):1521–5. doi: 10.2105/ajph.85.11.1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Andersson N, Cockcroft A, Shea B. Gender-based violence and HIV: relevance for HIV prevention in hyperendemic countries in southern Africa. AIDS. 2008;22(s4):S73–86. doi: 10.1097/01.aids.0000341778.73038.86. [DOI] [PubMed] [Google Scholar]
- 26.Fuentes CM. Pathways from interpersonal violence to sexually transmitted infections: a mixed-method study of diverse women. J Womens Health (Larchmt) 2008;17(10):1591–603. doi: 10.1089/jwh.2008.0885. [DOI] [PubMed] [Google Scholar]
- 27.Maman S, Campbell J, Sweat MD, Gielen AC. The intersections of HIV and violence: directions for future research and interventions. Soc Sci Med. 2000;50(4):459–78. doi: 10.1016/s0277-9536(99)00270-1. [DOI] [PubMed] [Google Scholar]
- 28.Jewkes R, Nduna M, Levin J, et al. A cluster randomized-controlled trial to determine the effectiveness of Stepping Stones in preventing HIV infections and promoting safer sexual behaviour amongst youth in the rural Eastern Cape, South Africa: trial design, methods and baseline findings. Trop Med Int Health. 2006;11(1):3–16. doi: 10.1111/j.1365-3156.2005.01530.x. [DOI] [PubMed] [Google Scholar]
- 29.Wechsberg WM, Luseno WK, Lam WK, Parry CD, Morojele NK. Substance use, sexual risk, and violence: HIV prevention intervention with sex workers in Pretoria. AIDS Behav. 2006;10(2):131–7. doi: 10.1007/s10461-005-9036-8. [DOI] [PubMed] [Google Scholar]
- 30.Jewkes R, Nduna M, Levin J, et al. Impact of stepping stones on incidence of HIV and HSV-2 and sexual behaviour in rural South Africa: cluster randomised controlled trial. BMJ. 2008;337:a506. doi: 10.1136/bmj.a506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kalichman SC, Simbayi LC, Cloete A, et al. Integrated gender-based violence and HIV risk reduction intervention for South African men: results of a Quasi-Experimental Field Trial. Prev Sci. 2009;10(3):260–9. doi: 10.1007/s11121-009-0129-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pronyk PM, Hargreaves JR, Kim JC, et al. Effect of a structural intervention for the prevention of intimate-partner violence and HIV in rural South Africa: a cluster randomised trial. Lancet. 2006;368(9551):1973–83. doi: 10.1016/S0140-6736(06)69744-4. [DOI] [PubMed] [Google Scholar]
- 33.Cluss PA, Chang JC, Hawker L, et al. The process of change for victims of intimate partner violence: support for a psychosocial readiness model. Womens Health Issues. 2006;16(5):262–74. doi: 10.1016/j.whi.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 34.Sikkema KJ, Heckman T, Kelly JA, et al. HIV risk behaviors amony women living in low-income, inner-city housing developments. Am J Public Health. 1996;86(8):1123–8. doi: 10.2105/ajph.86.8_pt_1.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sikkema KJ, Kelly JA, Winett RA, et al. Outcomes of a randomized community-level HIV prevention intervention for women living in 18 low-income housing developments. Am J Public Health. 2000;90(1):57–63. doi: 10.2105/ajph.90.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Briere J. Psychometric review of the trauma symptom checklist-40. In: Stamm BH, editor. Measurement of stress, trauma and adaptation. Sidran Press; Lutherville, MD: 1996. [Google Scholar]
- 37.Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised conflict tactics scales (CTS2): development and preliminary psychometric data. J Fam Issues. 1996;17(3):283–316. [Google Scholar]
- 38.NIMH-Multisite-HIV-Prevention-Trial The NIMH multisite HIV prevention trial reducing HIV sexual risk behavior. Science. 1998;280:1889–94. doi: 10.1126/science.280.5371.1889. [DOI] [PubMed] [Google Scholar]
- 39.Fox AM, Jackson SS, Hansen NB, Gasa N, Crewe M, Sikkema KJ. In their own voices: a qualitative study of women’s risk for intimate partner violence and HIV in South Africa. Violence Against Women. 2007;13(6):583–602. doi: 10.1177/1077801207299209. [DOI] [PubMed] [Google Scholar]
- 40.Wood GG, Roche SE. An emancipatory principle for social work with survivors of male violence. Affilia J Women Soc Work. 2001;16(1):66–79. [Google Scholar]
- 41.Dunkle KL, Jewkes RK, Brown HC, et al. Prevalence and patterns of gender-based violence and revictimization among women attending antenatal clinics in Soweto, South Africa. Am J Epidemiol. 2004;160(3):230–9. doi: 10.1093/aje/kwh194. [DOI] [PubMed] [Google Scholar]


