Abstract
Background
We examined socioeconomic and ethnic differences in use of lipid-lowering drugs after deregulation of simvastatin in the UK for adults with moderate or high risk of coronary heart disease.
Methods
3631 participants in the Whitehall II cohort study (mean age 62.7 years, 91% white) were informed of their risk of coronary heart disease, based on Framingham score, before deregulation (2002–2004). Use of prescribed lipid-lowering drugs and use of over-the-counter simvastatin were analysed as outcome variables, after deregulation (2005–2007).
Results
2451 participants were at high risk and 1180 at moderate risk. 20% moderate-risk and 44% high-risk participants reported using prescribed lipid-lowering drugs although no over-the-counter simvastatin was used. Prescribing rates did not differ between employment grades (an index of socioeconomic position), but was higher among South Asian high-risk compared with White high-risk participants (odds ratio 1.64, 95% CI 1.21 to 2.23). Of the high-risk participants, 44% recalled their increased coronary heart disease risk. South Asian high-risk participants were less likely to recall than White high-risk participants (odds ratio 0.65, 95% CI 0.46–0.93). Furthermore, high risk participants with middle (odds ratio 0.74, 95% CI. 0.61–0.89) and low (odds ratio 0.52, 95% CI 0.37–0.74) employment grades were less likely to recall than those with high grades.
Conclusion
Socioeconomic and ethnic differences in reported use of lipid-lowering drugs were small, but the use of these drugs in general was much lower than recommended and the participants did not utilise over-the-counter statins. Ethnic minorities and lower socioeconomic position groups were less likely to be aware of their increased coronary risk.
Keywords: statin, pharmacoepidemiology, cardiovascular risk, inequalities, socioeconomic position, ethnicity
Introduction
The way care is provided for chronic diseases has changed greatly over recent years. First, patients are encouraged to take a more active role in disease management and to share decision-making with their clinical team. Second, there have been shifts in the way care is provided, with an increasing number of access points for care1. In the UK, for example, the deregulation of simvastatin, which became available without prescription in August 2004, represented a major shift in the management of cardiovascular disease (CVD) risk and has not been repeated for any comparable aspect of chronic disease management. The National Service Framework for Coronary Heart Disease (2000) (NSF), Joint British Societies’ guidelines on prevention of cardiovascular disease in clinical practice (2005) and National Institute for Health and Clinical Excellence clinical guideline 67: lipid modification (2010) recommend that high-risk individuals with a 10-year CVD risk of ≥20% (equivalent to a 10-year coronary heart disease [CHD] risk of ≥15%) or with established CVD or diabetes be prescribed statins by clinicians. ‘Over the counter’ (OTC) statins were marketed for individuals at moderate-risk, i.e. those with “approximately 10–15% 10-year risk of a first major event of CHD”2. The stated rationale was that this was an attempt to increase choice through improved access to medicines3, although some identified a financial motive4.
This shift in the availability of simvastatin may be hypothesized to worsen health inequity, either because more affluent individuals would be more likely to purchase OTC statins or because awareness of one’s CHD risk may also influence purchasing, given evidence that recall of CHD-related information may be socially patterned5. Prior to deregulation, studies of social variations in statin use produced conflicting results: a cross-sectional analysis in four primary care trusts in England found some evidence of lower prescribing rates in areas with higher South Asian ethnicity and deprivation6; in contrast, a study of older British men found no evidence for a social class differences in statin use for secondary prevention7. The latter finding was replicated in analysis of the Health Survey for England and in a survey of 9,508 patients with angina in Scotland, although a prescribing bias toward the socioeconomically deprived was seen for some other CHD treatments8. To the best of our knowledge, there are no prospective cohort studies examining socioeconomic variations in use of lipid-lowering medications after deregulation, for both primary and secondary prevention.
Given the NSF’s objective to both improve population health overall and to reduce inequalities, we analysed data from the Whitehall II cohort study. Our principal aim was to examine the extent to which the use of lipid-lowering drugs, both prescribed and OTC, differed between socioeconomic and ethnic groups after deregulation, in adults with both moderate and high CHD risk. As a secondary objective, we analysed prospectively collected data on recall of personal CHD risk sent to participants and their GPs three years previously, given the likely contributory role of variation in recall of CHD risk to health inequalities.
Methods
Study population
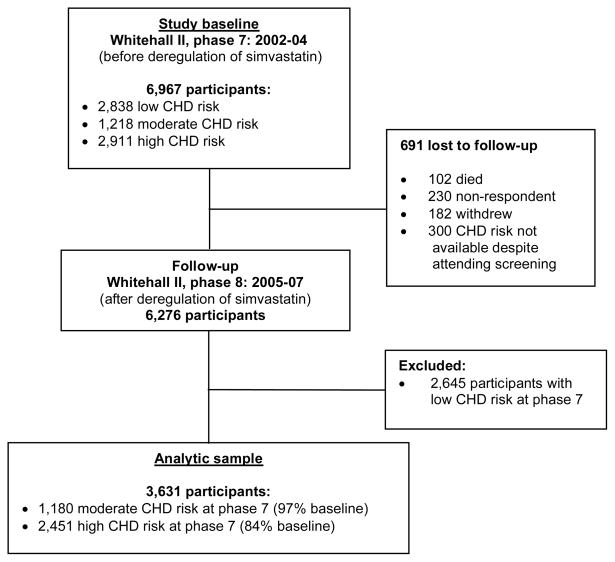
The Whitehall II study, established in 1985, is a longitudinal study to examine the socioeconomic gradient in health in British civil servants9. During the 2002–2004 data collection phase (the baseline for the present analysis), 6967 men and women aged 50 to 74 years underwent a clinical examination including assessment of their Framingham risk score. Between 2005 and 2007 (i.e. post-deregulation of simvastatin), participants were sent a health questionnaire including questions on use of lipid-lowering medications. The present analysis is limited to those participants who responded to this questionnaire and were at moderate (10–15%) or high (>15%) 10-year CHD risk, a total of 3,001 men and 630 women (Figure 1). Approval from the local Ethics Committee and written informed consent from each participant were obtained at each study phase.
Figure 1.
Flow chart showing numbers of participants at each phase of the study
Risk status
10-year absolute risk of CHD was determined using algorithms derived from the Framingham study10. All the items of the algorithm were measured according to standardised protocols. Age, sex and smoking status were self-reported. Oral glucose tolerance test was performed after an overnight fast, or for participants scheduled for afternoon clinics, after a light fat-free breakfast and an additional five hours’ fasting. Venous blood samples were taken at baseline and 2-hours after administration of a 75g glucose solution. Diabetes was defined by a fasting glucose ≥7.0 mmol/L, a 2-hour post load glucose ≥11.1 mmol/L, reported doctor diagnosed diabetes or use of diabetes medication. Systolic blood pressure was measured twice after 5min at rest with an Omron 907 automatic monitor and an average of 2 readings was taken. Blood cholesterol (HDL, LDL, total cholesterol) and glucose were measured in the same laboratories using identical methodology for all subjects. Left venticular hypertrophy (LVH) was identified on twelve-lead ECG with Minnesota codes by a single, blinded cardiologist using Eclipse 850 machines. Presence of CHD was ascertained through participant self-reporting and linkage to general practice and hospital records using NHS Number, name and date of birth, requesting specific diagnoses and hand-searching records whenever the participant reported any CVD-event, long-standing illness requiring treatment, hospital admission for chest pain or any medication or investigation suggestive of CVD. We defined moderate risk as 10-year estimated CHD risk between 10% and 15% and high risk as 10-year estimated CHD risk ≥15% or established CVD or diabetes. Participants were sent letters which informed them of their results and summarised whether they were “at increased risk of heart disease or angina”. Participants were told whether their blood pressure, blood cholesterol and blood glucose were “normal”, “slightly raised” or “raised” and whether their ECG was “normal” or “abnormal” and had changed since the previous screening. In the same envelope, unsealed, a similar letter was addressed to their GP; no results were sent directly to the GP.
Socioeconomic position and ethnicity
Socioeconomic position was assessed by British civil service grade of employment in 2002–2004 (or last grade prior to retirement) and was classified to high (administrative grades), intermediate (professional or executive grades) and low (clerical or support grades) position. Although mostly white collar, respondents across these three grades covered a wide range of socioeconomic positions and differed with respect to responsibility (from support staff, such as porters and telephonists, to senior executives), salary (from £7,387 to £87,620 per annum in August 1992) and social status. Ethnic group was observed at screening and classified as White Caucasian, South Asian, Afro-Caribbean, Chinese, Other or uncertain. Participants classified as Chinese or Other were grouped together in this study due to small numbers.
Use of lipid-lowering drugs and awareness of cardiovascular risk after deregulation of statin use
At 2005–2007 follow-up, participants were asked to list any medications taken in the last fourteen days, state whether they were prescribed by a doctor or not, and asked “Have you ever been told that you have an increased risk of heart disease?”. In addition, cognitive ability was assessed using a standard 30-item Mini-Mental State examination (MMSE).
Statistical analysis
We used Fisher exact test and analysis of variance as appropriate to examine group differences in categorical and continuous variables. Use of prescribed lipid-lowering drugs (yes/no), use of OTC simvastatin (yes/no) and recall of cardiovascular risk (yes/no) were investigated as outcome variables in logistic regression models, specifying ethnicity and socioeconomic position as independent variables and adjusting for age, sex and MMSE score. The relationship between recall of risk and Framingham score was also explored using logistic regression. Interactions with sex were tested in all analyses and as none were significant at the p<0.05 level, results are presented for men and women combined. All analyses were conducted using Intercooled Stata 9 (StataCorp LP, College Station, Texas, USA), and statistical significance was inferred at a 2-tailed p<0.05.
Results
There were 1218 participants with moderate risk and 2911 participants with high risk at baseline. Of these, 1180 (96.6%) and 2451 (84.2%) respectively were available for follow-up, dropout being greater in the high-risk group (p=0.005 by Fisher’s exact test). Compared to the analytic sample, participants lost to follow-up were slightly older (63.5 vs 62.7 years, p=0.07), more likely to be women (31.3% vs 17.3%, p<0.001), non-white (17.7% vs 9.0%, p<0.001), and from the lowest employment grade (15.1% vs 9.5%, p<0.001). Baseline characteristics of the 3631 participants forming the analytic sample are shown in Table 1.
Table 1.
Sample characteristics by 10-year CHD risk category prior to deregulation of simvastatin (baseline). Figures are numbers (%) unless otherwise stated
| Moderate risk group (N = 1,180) | High risk group (N = 2,451) | |
|---|---|---|
| Mean age, years | 61.3 | 63.4 |
| Sex | ||
| Male | 1,070 (90.7) | 1,931 (78.8) |
| Female | 110 (9.3) | 520 (21.2) |
| Ethnicity | ||
| White | 1,127 (95.8) | 2,171 (88.7) |
| South Asian | 34 (2.9) | 186 (7.6) |
| Afro-Caribbean | 12 (1.0) | 70 (2.9) |
| Other | 4 (0.3) | 21 (0.9) |
| Employment grade | ||
| High | 625 (53.2) | 1,045 (44.5) |
| Intermediate | 481 (40.9) | 1,040 (44.3) |
| Low | 70 (6.0) | 265 (11.3) |
Use of prescribed lipid-lowering medications
236 (20.0%) participants with moderate risk and 1082 (44.1%) with high risk reported using a prescribed lipid-lowering drug (p<0.001). There were some ethnic differences in prescribed drug use (Table 2): among high risk participants, those of South Asian ethnicity were more likely to report using a prescribed drug than White participants, odds ratio 1.64 (95% CI 1.21 to 2.23; p=0.001). Age was positively associated with use (odds ratio 1.04, 95% CI 1.02 to 1.05; p<0.001 for each additional year).
Table 2.
Odds ratios (95% confidence intervals) for reported use of prescribed lipid-lowering drugs after deregulation of simvastatin by 10-year CHD risk category at baseline and adjusted for age and sex
| Moderate risk group (N = 1,180) | High risk group (N = 2,451) | |
|---|---|---|
| Ethnicity | ||
| White | 1.00 (reference) | 1.00 (reference) |
| South Asian | 2.44 (1.20, 4.95) p=0.01 | 1.64 (1.21, 2.23) p=0.001 |
| Afro-Caribbean | 0.37 (0.05, 2.86) p=0.34 | 0.92 (0.56, 1.51) p=0.75 |
| Other | 1.46 (0.15, 14.1) p=0.74 | 1.18 (0.50, 2.79) p=0.71 |
| Employment grade | ||
| High | 1.00 (reference) | 1.00 (reference) |
| Intermediate | 0.74 (0.55, 1.01) p=0.06 | 0.99 (0.83, 1.19) p=0.94 |
| Low | 0.89 (0.46, 1.75) p=0.74 | 1.06 (0.78, 1.43) p=0.70 |
Among the moderate risk participants, the corresponding odds ratio for South Asian versus White ethnicity was 2.44 (95% CI 1.20 to 4.95; p=0.01). Age was positively associated with use in this risk-group as well (odds ratio 1.03, 95% CI 1.00 to 1.06; p=0.03 for each additional year).
Analysis of socioeconomic groups revealed no difference in prescribed lipid-lowering drug use between employment grades in the moderate or high risk groups.
Use of over-the-counter simvastatin
Few participants reported using any OTC drugs: 40 (3.4%) in moderate risk group and 65 (2.7%) in high risk group (p=0.25 by Fisher’s exact test). All reported OTC drugs were Omega-3 fatty acid compounds; no participants reported use of OTC simvastatin.
Recall of CHD risk
248 (21.0%) of participants with moderate risk and 1,080 (44.1%) with high risk recalled being told they were at increased risk of heart disease (p<0.001). After adjusting for age, sex, and MMSE-score, better recall was associated with higher Framingham score (adjusted odds ratio per one unit increase in Framingham score 1.05, 95% CI 1.04–1.07; p<0.001).
Among moderate risk participants, there was no association between ethnicity, employment grade and recall of CHD risk, with the exception of participants of intermediate employment grade who were slightly less likely to recall this information than those with high employment grade (age, sex, and MMSE-score adjusted odds ratio 0.72, 95% CI 0.53 to 0.98; p=0.04) (Table 3). Age was inversely associated with likelihood of recall (odds ratio 0.94, 95% CI 0.92 to 0.98; p<0.001 for each additional year).
Table 3.
Odds ratio (95% confidence interval) for recall of CHD risk after deregulation of simvastatin by CHD risk category and adjusted for age, sex and memory score.*
| Moderate risk group (N = 1,180) | High risk group (N = 2,451) | |
|---|---|---|
| Ethnicity | ||
| White | 1.00 (reference) | 1.00 (reference) |
| South Asian | 1.00 (0.40 to 2.50), p=0.99 | 0.65 (0.46 to 0.93), p=0.02 |
| Afro-Caribbean | 0.39 (0.05 to 3.10), p=0.37 | 0.80 (0.45 to 1.42), p=0.45 |
| Other | - | 0.82 (0.32 to 2.14), p=0.69 |
| Employment grade | ||
| High | 1.00 (reference) | 1.00 (reference) |
| Intermediate | 0.72 (0.53 to 0.98), p=0.04 | 0.74 (0.61 to 0.89), p=0.001 |
| Low | 0.55 (0.25 to 1.22), p=0.14 | 0.52 (0.37 to 0.74), p<0.001 |
Empty cells indicate no participants in these categories.
Amongst high risk participants, South Asian participants were less likely to recall being told they were at increased risk than White participants (adjusted odds ratio 0.65, 95% CI 0.46 to 0.93; p=0.02). Furthermore, participants with intermediate (adjusted odds ratio 0.74, 95% CI 0.61 to 0.89; p=0.001) and low employment grade (adjusted odds ratio 0.52, 95% CI 0.37 to 0.74; p<0.001) were less likely to recall this information than those of high employment grade, demonstrating a socioeconomic gradient in recall (Table 3). There was no association with age in this risk-group.
Association of risk-recall with lipid-lowering drug use
After adjusting for age, sex, ethnicity and socioeconomic position, participants who recalled being told they were at increased risk of heart disease were significantly more likely to report use of prescribed lipid-lowering drugs in both moderate risk group (odds ratio 5.77, 95% CI 4.14 to 8.02; p<0.001) and in high risk group (odds ratio 3.60, 95% CI 3.02 to 4.30; p<0.001).
Discussion
Evidence from a well-characterised occupational cohort study of British men and women suggests that use of lipid-lowering drugs was low but did not vary by SEP. We found greater odds for high-risk South Asian patients to reported use of a prescribed drug which is consistent with advice current at the time to multiply estimated CVD risk by 1.4 in patients of South Asian origin to adjust for need11. Fewer participants overall recalled being told they were at increased risk of CHD than used medication and high-risk participants of South Asian origin and of lower socioeconomic position were less likely to recall being told their risk. Up to three years after deregulation, use of OTC simvastatin was not reported at all.
Strengths and Limitations
Our study benefits from using prospectively collected data, with detailed and repeated assessments of clinical need. Loss to follow-up is a potential limitation of the study. Although drop-out was greater among lower socioeconomic groups in common with most longitudinal studies, numbers were small such that there were no significant differences in sex, ethnicity, social position or cognitive ability between baseline participants and the analytic sample (all p-values >0.1). Furthermore, while those lost to follow-up are known to have greater mortality, we have previously shown that this association is unmodified by socioeconomic position, mitigating the likelihood of major attrition bias12. The lack of statistical significance for some analyses with non-White, non-South-Asian participants may reflect a Type II (false negative) error arising from low numbers; similarly, false positive errors can arise when multiple comparisons are made. Our findings regarding higher lipid-lowering drug use among high-risk South-Asian participants and socioeconomic differences in risk awareness among high-risk participants remain, however, statistically significant after Bonferroni correction for multiple testing.
Occupational cohorts such as Whitehall II are, by their nature, healthier than the general population and probably also more motivated and interested in their health. Although this may limit generalisability of our findings, the finding of low rates of recall of personal CHD risk in such a cohort is particularly pertinent. Medication use was self-reported and no register-based prescription data were available to validate this information. Although use of self-reports is reasonable given our interest in participants’ awareness of personal CHD risk, it may nevertheless be a source of bias especially if reporting accuracy differs between socioeconomic groups.
Comparison with other studies
Low prescribing rates relative to need are well recognized in CHD13. Some studies using clinical records report higher prescribing rates than found in our analysis, but do not usually take into account differences between prescribed therapy and actual compliance14.
Our finding of equitable lipid-lowering prescribing is largely in agreement with other UK studies7;8;15 and with a study limited to patients with pre-existing CHD using data up to 200514. Our findings contrast, however, with an ecological analysis using data between April 2004-March 2005, which found a positive association between increasing level of deprivation and volume of statin prescribed16. That study used data from the first year of the Quality and Outcomes Framework (a set of disease and treatment registers used in general practice), although registration data are not age/sex standardised and, as the authors acknowledge, are incomplete.
Our finding of a socioeconomic gradient in recall of cardiovascular risk must be placed in the context of other studies of the social patterning in physician communication, patients’ perception of health risks and patients’ engagement in chronic disease management. Self-management of chronic disease is known to be better among people of higher socioeconomic position (SEP)17 and has been suggested as a contributory factor to the socioeconomic gradient in health. In agreement with our findings, there is some pervious evidence that recall of CHD-related information may be socially patterned. For example, a study of a patients with known CHD found that African-American men were significantly less likely to be aware of their CHD diagnosis than White men when interviewed during a CHD-related admission5. This may be due to physician factors (for example, Schouten reports that doctors displayed less rapport with minority ethnic patients compared to White patients18 and Willems found that patients from lower social classes experienced a more directive and less participatory consultation than those from a higher social class19) or patient factors. Wardle has shown that individuals of lower socioeconomic position are more likely to believe that health is largely a matter of luck, as opposed to personal action, and that those of lower and middle socioeconomic position are less likely to think about the future often20. Lindbladh suggested that those with fewer resources are preoccupied with mitigating more immediately apparent material and social risks than risks to health and, given their material constraints, find it more costly and time consuming to process new information compared to the better-off who are more used to having explicit choices to make21.
Meaning of the study
Our findings carry several important implications. First, the stated rationale of deregulating simvastatin to widen availability appears to have had no impact on the problem of under-treatment. It may be that the high cost of OTC simvastatin (£8.16 for six tablets at today’s prices) is a strong disincentive to uptake. Alternative strategies to address the problem of under-treatment are known to be effective, such as computer-generated alerts or the multidisciplinary team approach22. Second, early controversy around deregulation, including fears of worsening health inequities, appear to have been unfounded, because the OTC product was not taken-up. Third, it appears that those at highest risk of CHD (South Asian patients and those of lower socioeconomic position) have the poorest recall of their risk status. Poor risk-awareness is likely to impact patients’ ability to participate in self-management of chronic disease, whether involving adherence to medication or lifestyle change, and may partly explain the worse outcomes experienced by South Asian patients and those of lower socioeconomic position23;24. Sometimes small adjustments in physician communication can be sufficient to achieve meaningful patient engagement. A study from Canada, for example, found that informing patients of their CVD risk tertile improved the effectiveness of statin therapy, with greater benefit seen in those with worse risk profiles25.
In conclusion, evidence from the Whitehall II study suggests that sub-optimal prescribing remains an issue and that making drugs available for self-purchase is an ineffective response to the problem. Given that controversy is likely to persist regarding the need to self-purchase treatment in a health care system which is based on the premise of universal access to health care according to clinical need, free at the point of delivery, other solutions should be found that are attuned to social differences in CHD risk, perception of risk and in doctor-patient communication and that avoid creating new inequities in disease management.
WHAT IS ALREADY KNOWN ON THIS TOPIC
The deregulation of simvastatin in the UK in 2004 meant that statins became available without prescription for people with moderate cardiovascular disease risk.
Ethnic and socioeconomic differences in use of lipid-lowering drugs before deregulation of simvastatin in 2004 were small in the UK, but it has been unclear whether deregulation increased such differences in medication use.
WHAT THIS STUDY ADDS
In the Whitehall II study of British civil servants, the use of lipid-lowering drugs remained socially equitable after recent changes in availability in the UK.
However, reported use of lipid-lowering drugs was much lower than expected given the clinical need for intervention in all socioeconomic and ethnic groups.
Availability of over-the-counter simvastatin was not taken-up in this population.
Few high CHD risk individuals were aware of their risk, with those most at risk being less likely to be aware.
Acknowledgments
Funding: The Whitehall II study is funded by Medical Research Council; British Heart Foundation; Wellcome Trust; Health and Safety Executive; Department of Health; Agency for Health Care Policy Research, UK; John D and Catherine T MacArthur Foundation Research Networks on Successful Midlife Development and Socioeconomic Status and Health; National Heart, Lung and Blood Institute and National Institute on Aging, NIH, US. IF is funded by an MRC Clinical Research Training Fellowship; TC by HEFCE and ESRC; MGM by an MRC Research Professorship; RR by a NIHR Public Health Career Scientist Award and by the NIHR UCLH/UCL Comprehensive Biomedical Research Centre and MK by HEFCE. MK was also supported by the Academy of Finland, the BUPA Foundation and the EU OSH ERA research programme.
thanks to the Whitehall II participants and staff, particularly Aida Sanchez, Thérèse Butler, Stephanie Smith, Geoffrey Reading and Dimple Shah for their assistance in preparing this paper.
Footnotes
Competing interests: All authors declare that the answer to the questions on your competing interest form [http://bmj.com/cgi/content/full/317/7154/291/DC1] are all No and therefore have nothing to declare.
Contributors: IF (guarantor for the paper) and TC formulated the initial hypotheses and with MK designed the study and the analytic protocols. All authors contributed to the interpretation of results and writing the paper, and approved the final manuscript.
Ethical approval: Ethical approval for the Whitehall II study was obtained from the University College London Medical School committee on the ethics of human research.
Reference List
- 1.Department of Health, England. Choosing Health: making healthy choices easier. 2004. [Google Scholar]
- 2.Johnson & Johnson MSD Consumer Pharmaceuticals. Zocor Heart-Pro 10mg tablets, summary of product characteristics. UK: 2004. [Google Scholar]
- 3.Department of Health, England. Press release. 2004 http://www.dh.gov.uk/en/Publicationsandstatistics/Pressreleases/DH_4082004.
- 4.OTC statins: a bad decision for public health. Lancet. 2004;363(9422):1659. doi: 10.1016/S0140-6736(04)16284-3. [DOI] [PubMed] [Google Scholar]
- 5.Sanderson BK, Raczynski JM, Cornell CE, et al. Ethnic disparities in patient recall of physician recommendations of diagnostic and treatment procedures for coronary disease. Am J Epidemiol. 1998;148(8):741–749. doi: 10.1093/oxfordjournals.aje.a009695. [DOI] [PubMed] [Google Scholar]
- 6.Ward PR, Noyce PR, St Leger AS. Are GP practice prescribing rates for coronary heart disease drugs equitable? A cross sectional analysis in four primary care trusts in England. J Epidemiol Community Health. 2004;58(2):89–96. doi: 10.1136/jech.58.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ramsay SE, Morris RW, Papacosta O, et al. Secondary prevention of coronary heart disease in older British men: extent of inequalities before and after implementation of the National Service Framework. J Public Health. 2005;27(4):338–343. doi: 10.1093/pubmed/fdi053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murphy NF, Simpson CR, MacIntyre K, et al. Prevalence, incidence, primary care burden and medical treatment of angina in Scotland: age, sex and socioeconomic disparities: a population-based study. Heart. 2006;92(8):1047–1054. doi: 10.1136/hrt.2005.069419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marmot MG, Brunner EJ. Cohort Profile: The Whitehall II Study. Int J Epidemiology. 2005;34:251–256. doi: 10.1093/ije/dyh372. [DOI] [PubMed] [Google Scholar]
- 10.Anderson KM, Wilson PW, Odell PM, et al. An updated coronary risk profile. A statement for health professionals. Circulation. 1991;83(1):356–362. doi: 10.1161/01.cir.83.1.356. [DOI] [PubMed] [Google Scholar]
- 11.British Heart Foundation. JBS Guidelines on the Prevention of Cardiovascular Disease in Clinical Practice: Risk Assessment. 2006. [Google Scholar]
- 12.Ferrie JE, Kivimaki M, Singh-Manoux A, et al. Non-response to baseline, non-response to follow-up and mortality in the Whitehall II cohort. Int J Epidemiol. 2009 doi: 10.1093/ije/dyp153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Capewell S, Unal B, Critchley JA, et al. Over 20,000 avoidable coronary deaths in England and Wales in 2000: the failure to give effective treatments to many eligible patients. Heart. 2006;92(4):521–523. doi: 10.1136/hrt.2004.053645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DeWilde S, Carey IM, Richards N, et al. Trends in secondary prevention of ischaemic heart disease in the UK 1994 2005: use of individual and combination treatment. Heart. 2008;94(1):83–88. doi: 10.1136/hrt.2006.111757. [DOI] [PubMed] [Google Scholar]
- 15.Reid FD, Cook DG, Whincup PH. Use of statins in the secondary prevention of coronary heart disease: is treatment equitable? Heart. 2002;88(1):15–19. doi: 10.1136/heart.88.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ashworth M, Lloyd D, Smith RS, et al. Social deprivation and statin prescribing: a cross-sectional analysis using data from the new UK general practitioner ‘Quality and Outcomes Framework’. J Public Health (Oxf) 2007;29(1):40–47. doi: 10.1093/pubmed/fdl068. [DOI] [PubMed] [Google Scholar]
- 17.Goldman DP, Smith JP. Can patient self-management help explain the SES health gradient? Proc Natl Acad Sci. 2002;99(16):10929–10934. doi: 10.1073/pnas.162086599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schouten BC, Meeuwesen L. Cultural differences in medical communication: a review of the literature. Patient Educ Couns. 2006;64(1–3):21–34. doi: 10.1016/j.pec.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 19.Willems S, De Maesschalck S, Deveugele M, et al. Socio-economic status of the patient and doctor-patient communication: does it make a difference? Patient Educ Couns. 2005;56(2):139–146. doi: 10.1016/j.pec.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 20.Wardle J, Steptoe A. Socioeconomic differences in attitudes and beliefs about healthy lifestyles. J Epidemiol Community Health. 2003;57(6):440–443. doi: 10.1136/jech.57.6.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lindbladh E, Hampus Lyttkens C. Polarization in the reaction to health-risk information: a question of social position? Risk Analysis. 2003;23(4):841–855. doi: 10.1111/1539-6924.00361. [DOI] [PubMed] [Google Scholar]
- 22.Hanlon JT, Schmader KE, Ruby CM, et al. Suboptimal prescribing in older inpatients and outpatients. J Am Geriatr Soc. 2001;49(2):200–209. doi: 10.1046/j.1532-5415.2001.49042.x. [DOI] [PubMed] [Google Scholar]
- 23.Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993;88(4 Pt 1):1973–1998. doi: 10.1161/01.cir.88.4.1973. [DOI] [PubMed] [Google Scholar]
- 24.Balarajan R. Ethnicity and variations in mortality from coronary heart disease. Health Trends. 1996;28:45–51. [Google Scholar]
- 25.Grover SA, Lowensteyn I, Joseph L, et al. Patient knowledge of coronary risk profile improves the effectiveness of dyslipidemia therapy: the CHECK-UP study: a randomized controlled trial. Arch Intern Med. 2007;167(21):2296–2303. doi: 10.1001/archinte.167.21.2296. [DOI] [PubMed] [Google Scholar]