Abstract
Objectives
To review the existing epidemiological literature on suicide and alcohol related disorders and their social determinants in the U.S. Arctic, as it relates to U.S. government research and evaluation efforts, and to offer recommendations to boost research capacity in the U.S. Arctic and collaborations across the circumpolar arctic as part of global health initiatives. Study design: Synthetic literature review.
Methods
Published literature, federal and state reports on suicide and alcohol-related disorders, federal databases on research and program evaluation in the U.S Arctic were reviewed, with a focus on epidemiological trends over the past 50 years.
Results
Suicide and alcohol-related disorders play a significant role in health disparities t in the U.S. Arctic, with evidence of a disturbing prevalence trend over the past 50 years. Important variations exist in suicide rates across different regions of Alaska with different majority populations of Alaska Native cultural groups, and in selected key instances, within these regions, with immense implications for guiding effective prevention efforts. Consequences of alcohol abuse are severe and particularly significant in their impact upon Alaska Native people. Health related conditions associated with alcohol abuse are among leading causes of mortality.
Conclusions
Recommendations to boost research capacity in behavioural health in the U.S. Arctic are offered; specifically on strategies and methods of inquiry and analysis, distinctions between populations and communities in rural circumpolar contexts, future epidemiological and implementation research.
Keywords: Arctic, Alaska, Alaska Native, suicide, alcohol, U.S. Arctic research and research infrastructure
INTRODUCTION
Understanding the role behavioural and mental health conditions play in mortality and health outcomes is crucial to eliminating health disparities experienced in the U.S. Arctic. This paper reviews the epidemiology of suicide and alcohol use disorders to explore their role in health disparities and mortality in the U.S. Arctic, where in one five year period in the past decade, suicide was the eighth leading cause of death, while liver disease and cirrhosis the tenth (1). Nature of the complex relationship between suicide and alcohol disorders is beyond the scope of this review, which instead highlights what is different about them in the Arctic, in contrast to the U.S general population and their unique challenge for Alaska Native (AN) people.
During the second half of the 20th century, AN communities experienced shifts in diseases and health-related concerns, from devastating influenza and tuberculosis epidemics to behavioural health as major causes of illness and mortality, with suicide and alcohol use disorders emerging as major health problems (2). The U.S. government (USG) research investment in behavioural and mental health to guide its response is presented in this paper. We conclude with recommendations for boosting research and research capacity in the U.S. Arctic informed by the literature and experience of recent funded research efforts.
METHODS
Systematic literature searches were conducted with a focus on suicide and alcohol in the U.S. Arctic. No other limitations were set. Research published since 2000 was prioritized. MEDLINE, Web of Science, PUBMED, and PSYCINFO databases were supplemented by relevant additional sources cited in the articles identified in the databases. USG and State of Alaska reports from public health agencies further augmented this review, providing crucial data on epidemiology not published in the literature. NSF, SAMHSA, and NIH databases, including the NIH Reporter database provided listings of existing USG funded behavioural and mental health research projects.
RESULTS AND DISCUSSION
Suicide in the U.S. Arctic
In contrast to recent findings in Greenland of a seasonal increase in summer suicides (3), suicides in Alaska are evenly distributed across each month, with no apparent seasonal pattern (4). However, significant disparities exist in the rate of suicides in Alaska when compared to the U.S. general population, and within Alaska, where disparities emerge between ethnic groups, by age, and region. While the causes of these disparities remain poorly understood, their basic epidemiology provides important clues for potential effective interventions.
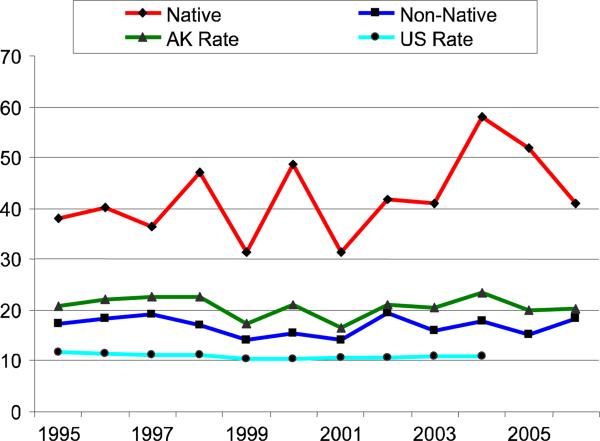
In 2004, there were 155 suicides in Alaska, resulting in the highest rate in the U.S., at 23.4/100,000, a rate more than double the U.S. rate of 11/100,000 (5). However, an important consideration in understanding Alaska suicide data is it involves inference from low base rate events within small populations. For this reason, estimates can vary enormously from year to year, requiring multi-year analyses to derive more stable estimates. Using this approach, the impact of sustained high rates of suicide in Alaska becomes evident (Figure 1), with suicide rates in Alaska from 1990 to 2005 consistently twice that of the general U.S. population (5).
Figure 1.
Suicide rates in Alaska 1990–2005
Note. Rates are per 100,000 age-adjusted to year 2005 population estimates per group.
Adapted from (5). Used with permission.
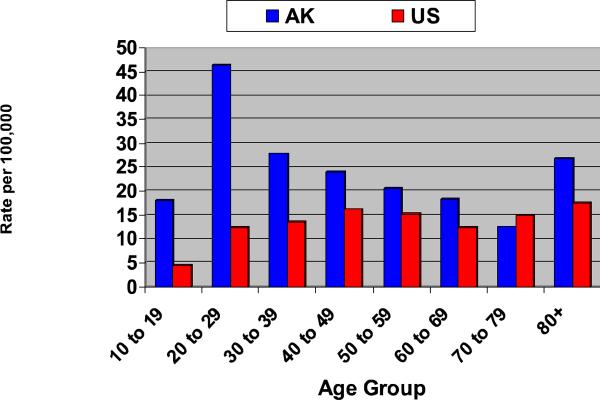
While suicide was the eighth leading cause of death in Alaska in 2001–2005 (1), it was the second leading cause of death under age 50; mean age at time of suicide is younger than for the U.S. general population (5). Figure 2 shows in Alaska, the highest rates of suicide occur at age 20–29, in contrast, in the U.S. general population, where the highest rates occur over age 80.
Figure 2.
Suicide rate by age group in Alaska and the United States 2003–2006
Note. Rates are per 100,000 age adjusted to year 2004 US general population.
Adapted from (5). Used with permission.
Suicide among Alaska Native people
Kraus (6) investigated changing patterns of suicidal behaviour among AN peoples from 1950–1970, discovering a disturbing trend of accelerating rates of suicide and emergence of youth suicide. Kraus also found rates of suicide remained stable until 1965, then doubled over the next five years. Almost all of this increase was accounted by suicides among 15- to 25-year-olds. During 1970–1974, the rate doubled again (7) and by 1983–1984, suicide rates for the AN population were 43/100,000 (8, 9), increasing again in 1986 to 67.6/100,000 (10).
Recent data indicate continuation of these disturbing trends. From 2001 through 2005, following a number of local, state, and tribal efforts in response to these rates, the average suicide rate among all AN people declined to 38.6/100,000, still in sharp contrast to 20.2/100,000 for all other ethnic groups in Alaska (1), and 10.84/100,000 for the U.S. general population (11). Overall, suicide rates among all AN people increased 500% since 1960 (12), and as indicated in Figure 1, annual suicide rates between 1990–2005 for all AN cultural groups remained 3 to 6 times higher than the U.S. general population, with the suicide rate of AN 10–19 four times that of their non-Native peers (4).
Across the circumpolar North, veritable epidemics of suicides have taken place among the indigenous communities of Greenland, Canada, and Alaska (13). One characteristic of youth suicide in these communities is its tendency to occur in epidemics or “clusters” (14). Clusters are series of suicides closely spaced in time and place, and etiologically linked (15, 16). For example, in a suicide “epidemic” documented in a Yup'ik village of 522 people, seven young men and one woman committed suicide in one year (17).
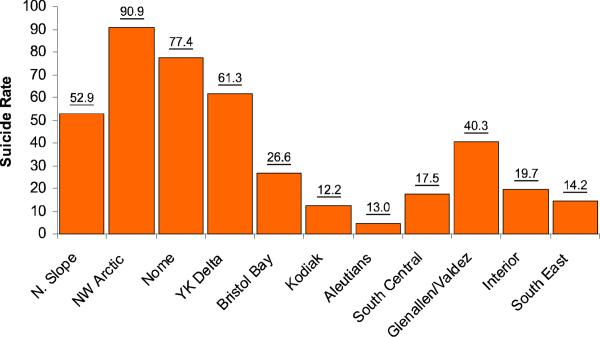
At the same time, important variation exists in suicide rates across different regions of Alaska with different majority populations of AN cultural groups. Figure 3 shows how between 2004–2006, suicide rates in Kodiak and the Aleutians, which have a mixed ethnicity White/Alutiq/Asian and Pacific Island population and an Aleut/Alutiq majority population respectively, were the lowest in the state. The highest rates were in the Northwest Arctic, Nome, Yukon-Kuskokwim Delta, and North Slope regions, which have Inupiaq and Yup'ik majority populations, with the highest rates exceeding 90/100,000. Looking at the data more closely, significant variation exists within these regions. For example, for 2001–2005, the Wade Hampton Census area, which is within the Yukon-Kuskokwim Delta, experienced higher suicide rates than Northwest Arctic (1), where in one community of approximately 650, from 2003–2006, there were 14 deaths by suicide, all under age 25. In another Wade Hampton community of similar size and composed of the same majority Yup'ik cultural group, a suicide had not occurred in over 30 years. This suggests suicide is not necessarily a problem uniformly across all AN cultural groups, or across all communities within regions where the majority of inhabitants are from the same AN cultural group. Identification of factors predictive of the low suicide rates found within specific groups and communities is an important priority for research. Solution of this puzzle has immense implications for guiding effective suicide prevention efforts in the U.S. Arctic, and elsewhere in the circumpolar north.
Figure 3.
Alaska suicide rates by Emergency Medical Service Region 2004–2006
Note. Rates are per 100,000 adjusted for each region to 2004 population.
Adapted from (5). Used with permission.
Subgroup analysis holds particular promise in understanding these phenomena. One recent study explored correlates of fatal versus nonfatal suicides among one regional subgroup of Inupiat (18). An earlier study explored temporal and geographic patterns in teen suicide in Alaska (19). These studies highlight the potential value of investigations that seek to untangle the differences in risk and protection among distinct cultural and cohort groups as explanatory mechanisms for suicide.
Alcohol use disorders in the U.S. Arctic
The context of alcohol use disorders in Alaska reveals a very complex picture and a number of trends. Overall consumption of alcoholic beverages was consistently about 1.2 higher in Alaska than the U.S. general population from 2000–2007, and consumption of distilled spirits in particular was 1.4 times higher (1). Rates of binge drinking are also higher, with an accompanying trend among high school youth to increase binge drinking over the high school years (20). In addition, Alaska has high rates of Fetal Alcohol Spectrum Disorders (FASD), with prevalence of 478/100,000, a rate nearly five times the U.S. general population (21).
The Alaska Behavioural Risk Factor Survey (BRFS) has tracked adult drinking in Alaska since 1991 (22). Overall prevalence of heavy alcohol use among Alaskans in 2007, defined on the BRFS as 2 or more drinks a day in men and one or more in women, was 6%, a rate similar to the U.S. general population. However, BRFS data from 2001 to 2007 shows a higher level in Alaska than the U.S. general population of episodic heavy drinking, or binge drinking, despite a declining trend over time. The weighted percentages of the state's population that engaged in binge drinking in Alaska over the past 30 days, defined as 5 or more drinks for men and four or more drinks for women were 21% in 1991, and 19% in 2007, compared to 16% in 2007 for the U.S. general population.
Aligned with this adult trend, youth binge drinking, as reported through the Alaska Youth BRFS, also displayed a steady consistent decline between 1995 and 2007, and is now at a level similar to that of the 2005 general U.S. youth population (1, 20). Youth who drink in Alaska appear to begin drinking in early to mid-teens (1, 23–25); with highest rates of binge drinking reported among 18–34 year-olds (22).
According to the 2003–2004 National Survey of Drug Use and Health (26), Alaskan men were two times as likely to binge drink than women. Among 18–25 year-old males, 39% reported binge drinking, 16% reported drinking five or more drinks for five or more days in the past 30 days, and 7% were in need of treatment services.
Physical and/or sexual abuse are the most common risk factors for alcohol use disorders in Alaska, including early substance use. Among a sample of 830 individuals from one detoxification facility in Alaska, 28% of women and 13% of men reported childhood physical abuse, and 31% of women and 6.5% of men reported childhood sexual abuse (27). In contrast, the aggregated prevalence rate of childhood sexual abuse across 25 North American population samples is 22.3% for women and 8.5% for men (28). When compared to the Alaska general population, this group reported earlier onset of alcohol use, more arrests, and more psychopathology: 80% met criteria for psychiatric disorder on the Brief Symptom Inventory, a screening measure of psychopathology (29).
In summary, the consequences of alcohol abuse in Alaska are severe. Alaska consistently has one of the highest rates of death in the U.S. from alcohol-related causes (30) with liver disease and cirrhosis as the 10th leading cause of death in the state (1), where the consequences of alcohol use disorders having a particularly significant impact upon AN people.
Alcohol use disorders among Alaska Native people
Alcohol use disorders among AN people have direct and substantial impacts upon mortality. Between 1999 and 2003 unintentional injuries were the third leading cause of death among AN peoples while suicide was the fourth, with males having twice as many unintentional non-fatal injuries than females (31). A large proportion of these injuries, suicides, and homicides were alcohol-related (1). Alcohol use disorders lead to a wide variety of nervous, digestive, and circulatory disorders, with AN people having the highest rate of death from these alcohol induced disorders of any ethnic group in Alaska. Rates from 2001–2005 were over three times the rate of all other ethnic groups, with the highest indicators in rural areas, where AN males had 17% higher death rate than females; in 2005, nearly 1 in 13 AN deaths were alcohol induced (30).
In one study, 61% of men and 37% of women screened had engaged in binge drinking in the past year (25). Reasons reported for drinking included reducing stress and trauma, sadness, depression, despair, and a sense of being caught between cultures. Alcohol use was consistently associated in focus group interviews with violent behavior, injury, and death. Deaths were viewed as clustered in families with multiple drinkers, and alcohol related suicide was also reported as a major problem. Among the 486 AN alcohol treatment inpatients that participated in the Collaborative Study on the Genetics of Alcoholism, in contrast to people of African-American, Hispanic, and Euro-American racial and ethnic backgrounds, ANs and Euro-Americans with alcoholism experienced higher rates of depression, while ANs with alcoholism, in contrast to all other ethnic groups, tended to have the earliest onset of the disorder, used medical and mental health professionals and Alcoholics Anonymous the least, and displayed the highest levels of co-occurring marijuana dependence (32). Relative absence of gender differences emerged in this AN sample on alcohol-related consequences, however women experienced greater prevalence of depression (33).
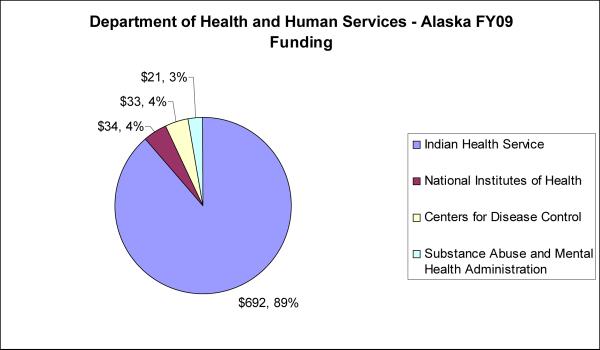
Behavioural and mental health research in the U.S. Arctic
In this section, we briefly describe U.S. government (USG) behavioural and mental health research funding to address this area of significant concern in the U.S. Arctic. The overall USG investment in all biomedical and behavioural health-related research, training, and services in the U.S. Arctic for 2009 (the most recent year complete data is available), was over $770 million USD in multiyear awards active that year through the Department of Health and Human Services (DHHS). Figure 4 indicates the relatively small proportion of this investment that is devoted to research. Most USG research funding in the U.S. Arctic is awarded on a peerreviewed competitive basis through the National Institutes of Health (NIH), with $34 million USD in multiyear awards active in 2009. Substantially smaller amounts fund research and evaluation as part of the Substance Abuse and Mental Health Services Administration (SAMHSA), Centers for Disease Control (CDC), and Indian Health Services (IHS) projects. In summary, research efforts account for only a small fraction of health-related programmatic funding in the U.S. Arctic, which is largely obligated for services; there is critical need for research resources, and in particular, research capacity-building programs. Of the $34 million USD NIH investment in arctic biomedical and behavioural health research, $15 million USD was devoted to behavioural and mental health research in total funding for multiyear awards that were active in 2009. The nature of this behavioural and mental health research portfolio in the U.S. Arctic is described in the next section.
Figure 4.
U.S. Department of Health and Human Services health-related funding in the U.S. Arctic, FY2009.
NIH
The Fogarty International Centre (FIC) is the designated focal point for Arctic issues at the NIH, providing leadership and input to a wide range of groups, including the Polar Research Board of the National Academies of Science, the U.S. Arctic Research Commission (USARC), and the Arctic Policy Group at the Department of State. FIC, together with four NIH institutes (National Institute on Alcohol Abuse and Alcoholism (NIAAA), National Institute on Drug Abuse (NIDA), National Center for Research Resources (NCRR), and National Institute on Mental Health (NIMH)), and CDC and USARC, organized a 2009 strategy-setting meeting on Behavioural and Mental Health Research. One specific focus was on suicide and alcohol use disorders. Proceedings were published in a special issue of IJCH (34); the review and recommendations offered here are the authors and not a report from this conference.
A significant investment in health research in Alaska at the NIH has been through the NCRR Institutional Development Award (IdeA) Program. IdeA supports the Centers of Biomedical Research Excellence (COBRE), which strengthen institutional biomedical research capacity by developing new investigator capability through support of an interdisciplinary centre. The Center for Alaska Native Health Research (CANHR) at the University of Alaska Fairbanks, is the only IdeA centre in the Arctic, and originally focused genetic, nutritional, and psychosocial components of obesity among Yupik Alaska Native adults. The centre established a reputation for community engagement using a tribal community-based participatory research (CBPR) perspective. CANHR also provides infrastructure support for several independently funded NIH projects driven by CBPR community co-researcher interests, examining a variety of behavioural and mental health topics including stress and trauma, and preventive intervention research on alcohol abuse and suicide.
The National Institute on Minority Health and Health Disparities (NIMHD) leads the USG effort in health disparities research and research capacity building in minority health. Many projects promoted CBPR to foster sustainable community efforts to accelerate translational research toward the elimination of health disparities. Currently, CANHR has one CBPR initiative with rural Yup'ik Southwestern Alaska communities as partners. A partner community determined its highest priority health need was to address suicide and alcohol abuse and developed a complex multilevel cultural intervention reducing suicide risk and co-occurring underage drinking in youth. The work has now advanced to a multi-site prevention trial (35). The process involves partnership with local tribal governments, the Lower Yukon School District, and the Yukon Kuskokwim Health Cooperation, with direction from local community planning groups. Another NIMHD Centers of Excellence (COE) Program builds research capacities to increase the pool of investigators from minority populations through research training and development. COE supports one center in the U.S. Arctic, the Center Addressing Health Disparities through Research and Education (CAHDRE) at the University of Alaska Anchorage (UAA). CAHDRE establishes linkages to several existing programs that encourage and support members of minority groups to prepare for the health research professions, some of which are in behavioral health.
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) studies the causes and consequences of excessive alcohol consumption, and develops and validates effective treatment and prevention strategies. In addition, NIAAA's 2009–2013 Health Disparities Strategic Plan prioritizes research on American Indian and Alaska Native (AIAN) populations. NIAAA funded two recent projects at CANHR: one developed a culturally based alcohol use prevention program for rural Yup'ik 12–18 year-olds, and a second developed measures to assess variables related to alcohol abuse and suicide in AN adolescents. NIAAA is merging with the National Institute on Drug Abuse (NIDA), which has funded basic and applied research on drug abuse in the AN population since 1994.
National Science Foundation
The National Science Foundation (NSF) supports a wide array of social science research, some of which explores social and cultural determinants of health. In fiscal year 2009, total NSF Arctic Social Science Research budget was approximately $15 million (including $10 million from American Recovery and Reinvestment Act [ARRA] funds), with one current study exploring resiliency strategies used by circumpolar youth, critical to understanding effective substance abuse and suicide prevention strategies (36).
Services and evaluation research in the U.S. Arctic
SAMHSA, CDC, and IHS support clinical, surveillance and health services in the U.S. Arctic frequently delivered through state, community, and tribal agencies. These programs typically include evaluation research components and often serve as incubators for U.S. Arctic service delivery innovation. This evaluation research holds great potential for advancing our understanding of treatment and service delivery
SAMHSA
The Center for Mental Health Services (CMHS), one of three centres within SAMHSA, leads national efforts to improve prevention and mental health treatment services, and leads a suicide prevention initiative serving AIAN communities. The Garrett Lee Smith State/Tribal Suicide Prevention Grant Program has awarded 20 CMHS grants to tribes and/or tribal organizations, four of which are in Alaska, to develop and implement youth suicide prevention and early intervention strategies. The CMHS Native Aspirations contract provides training and technical assistance to 54 communities, including nine AN communities, to implement community-based prevention efforts to reduce violence, bullying, and suicide in youth. The Fetal Alcohol Spectrum Disorders (FASD) Center of Excellence launched in 2000 supports evidence-based interventions for FASD through education and training. It supports State of Alaska programs for brief intervention, referral, in-patient and outpatient chemical dependency treatment. Another SAMHSA project develops Regional Suicide Prevention Teams to deliver comprehensive community-based suicide prevention services for 15–24 year-olds, with a special emphasis on AN, gay, lesbian, bisexual and transgender youth, young veterans, and other youth at risk for institutional care and correctional facilities. An independent evaluation team from the Center for Behavioral Health Research and Services (CBHRS) at UAA is identifying system gaps, ways to connect youth with mental health services, and training needs for Alaska suicide prevention programs. SAMHSA also supports several dual diagnosis programs for substance abuse and psychiatric disorders in the U.S Arctic.
CDC
The Arctic Investigations Program (AIP) CDC field station in Anchorage, AK coordinates disease surveillance, conducts public health research, works to improve laboratory diagnosis, and evaluates prevention strategies in the Arctic and Sub-Arctic, with special focus on indigenous populations. Under this aegis, AIP has provided significant support to circumpolar suicide research and conferences. In addition, the CDC Arctic Fetal Alcohol Spectrum Disorders Regional Training Center (Arctic FASDRTC) at CBHRS adds to the SAMHSA FASD efforts through programs focused on enhancing awareness, resource development, and dissemination of FASD prevention strategies, and includes two FASD education needs assessments.
IHS
The Alaska Tribal Health System (ATHS) provides single-payer, free-of-charge medical services, including mental health and substance abuse services to AN people. Primary funding is provided through HIS compacting to regional tribal health organizations Medicare, Medicaid, private insurance, grants, and other sources account for another 40% of total health-related revenue. Opportunities exist for behavioral and mental health research through the Native American Research Centers for Health (NARCH) program, an IHS and the NIH National Institute of General Medical Sciences (NIGMS) joint initiative. NARCH builds research infrastructure, representing significant opportunity to meet research needs of AN communities.
Strategies to boost behavioural and mental health research in the U.S. Arctic
Existing epidemiological literature indicates significant disparities in health outcomes associated with suicide and alcohol use disorders within the U.S. Arctic in contrast to the U.S. general population, and that these disparities are experienced most severely by AN people. Despite this fact that, there is a dearth of research on the determinants of suicide and alcohol abuse in Alaska and other Arctic communities, even less research on protective factors, and extremely limited research on evidence based practices for the U.S. Arctic and AN people.
For AN and other indigenous Arctic people, the solutions to these problems require development of sustained, trusting, collaborative, and non-exploitive research relationships. Research in particular with small, remote, extended kinship-based AN communities holds the potential to inform work with other Arctic indigenous groups, with application to other culturally distinct, indigenous, and rural populations. The following recommendations to boost research capacity and research in behavioural and mental health in the U.S Arctic are based in the existing epidemiological literature and research efforts in the U.S. Arctic.
Boosting research capacity
There are three NIH-funded programs at the University of Alaska focused on increasing research capacity in the U.S. Arctic. In addition to the IdeA program COBRE at CANHR, the Alaska Institutional Development Award for Biomedical Research Excellence (INBRE) program funded through NCRR targets chemical agents (especially contaminants in subsistence foods) and zoonotic and vector-borne microbial agents of disease. The Alaska Basic Neuroscience Program (ABNP), a Specialized Neuroscience Research Program (SNRP) grant, funded through the National Institute of Neurological Disorders and Stroke (NINDS), National Institute of Mental Health (NIMH), and NCRR strives to expand and stimulate basic neuroscience research with a focus on neuroprotection and adaptation at the cellular and molecular level. At the Alaska Native Tribal Health Consortium, a second SNRP award funds the Alaska Native Stroke Registry (ANSR). COBRE, INBRE, and SNRP focus on improving infrastructure for biomedical research and training in Alaska, providing important opportunities for early career scientists to engage in research in Alaska. Despite the extent of behavioural health concerns in the U.S. Arctic, no research capacity-building program emphasizes unmet behavioural health research needs. The logistical complexities of work in the arctic, and the remoteness and distance of the U.S. Arctic from other U.S. research institutions all pose significant challenges that research capacity-development grants in behavioural health research would be uniquely suited to address. In particular, such infrastructure grants could provide a catalyst for more coordinated and effective implementation for a number of existing evaluation studies, and enhance the competitiveness of investigators. Because of the relative remoteness of the U.S Arctic, distance learning and telemedicine tools are well developed in Alaska. These hold significant promise as capacity-development tools linking arctic researchers with outside research expertise, and can be extensively utilized as teaching, training, and mentoring.
Boosting research studies
Expanding research to develop contextually relevant and effective solutions to address the behavioural and mental health concerns of circumpolar residents is a critical need. However, increasing research on these topics will require better alignment between priorities of local communities and tribal organizations with researchers and funding agencies. Currently, there is a disconnect between the research priorities and methods of the funding communities and local stakeholders, which are more interested in solutions and the applied aspects of intervention research, while the research funding community often appears to local interests as more interested in underlying genetic and environmental determinants of disease. While research from both perspectives is important, there is pressing need to establish and maintain open communication to better inform these differences in priorities. On-going dialogue between communities through their tribal and state leadership, local and international arctic researchers, and representatives from key USG agencies is needed.
Research strategies
The literature, context, and existing research environment in the U.S. Arctic point to seven specific strategies to boost behavioural and mental health research in the U.S. Arctic.
Data collection methods and analysis
Although epidemiological data in Alaska has improved, significant gaps in our understanding of basic prevalence, risk, and protective factors persist, thus an analysis of existing data is needed to explore gaps and provide methods to address them. Given past negative experiences with research (37), new research initiatives in Alaska will require extensive consultations and collaboration with AN communities and leadership using CBPR models. This necessity, borne out of historical events, along with logistical challenges of research in Alaska, will require a significant investment in research resources in order to implement the types of rigorous, methodologically sophisticated protocols used in contemporary epidemiological research. Experience has demonstrated how NIH research infrastructure grants can provide crucial support critical to the intensive nature of this work. Such investment has enormous potential to address a substantial health disparity in the U.S. and in other international circumpolar settings. Methodological advances in robust, sophisticated approaches for the analysis of small sample data sets are needed for this research, as is the case in other rural research settings and in research with small at-risk populations.
Epidemiological research on suicide
The differences in suicide rates between 20–29 year old AN and non-AN adults raise important unanswered questions regarding the underlying aetiology. While important differences have been suggested, little progress has been made in understanding the particular explanatory variables responsible for such differences. This level of understanding has important implications for informing prevention and treatment. Study of protective factors holds particular promise to advance understanding of differences at the community level.
Epidemiological research on alcohol use disorders
There have been a number of USG funded research studies on alcohol use disorders in Alaska; however, actual prevalence and incidence of use and abuse remains poorly described, particularly in rural indigenous settings. Several projects have examined prevention and treatment approaches; however, there is a need for research on the co-morbidities between alcohol use disorders and suicide, and approaches utilizing culturally tailored alcohol use disorder prevention and treatment strategies.
Distinguishing populations from communities
In the epidemiological data, important distinctions emerge regarding prevalence of suicide and alcohol use disorders and their resulting health disparities in the U.S. Arctic, and among AN people, in contrast to the general U.S. population. Though suicide and alcohol are often identified as AN problems in lay discourse, rates between Native and non-native rural populations often vary little, while rates between different Native groups and between different communities within the same Native and regional population group can vary enormously. Discovery of the explanatory variables for these differences holds enormous implications for prevention and treatment.
Systematic implementation research
A number of USG agencies have been funding behavioural and mental health prevention and treatment services in the U.S. Arctic for decades. The results of these investments suggest current methods are not working, as the anticipated declines in suicide and alcohol abuse rates have not materialized. Recognizing that program impact may take a number of years to become evident, systematic assessments of the implementation of prevention and treatment services are needed. These implementation studies would benefit from close collaboration with tribal and other local organizations that provide and manage services to communities, and close collaboration among local researchers with outside researchers knowledgeable in implementation research. Projects should examine differences in services implementation as they interact with population and community differences.
Rigorous examination of promising existing arctic strategies
Alaska has promising treatment and prevention strategies for suicide and alcohol use disorders (23, 24, 35, 38, 39) that utilize multi-level models of intervention at the individual, family and community levels (40). Research of these approaches provides an alternative to continuing to import potentially poorly suited intervention models untested in arctic contexts. Careful adaptation research of intervention models untested in arctic contexts is also needed. These studies also provide models for collaborative approaches for research with communities as partners in the research process (24,39), a development that has been well received in Alaska.
Linkages with the international circumpolar research community
Research on suicide and alcohol abuse in the U.S. Arctic is often conducted in isolation from similar efforts across the circumpolar North, and is rarely informed by innovative and important work outside the U.S. and North America. Yet suicide and alcohol related disorders present a shared societal and research concern across the entire arctic (41). Regular circumpolar research exchanges, along with bilateral and multilateral collaborations in suicide and alcohol research will boost U.S. Arctic research capacity and improve the health of arctic people.
Conclusions
Why would the USG make such significant investments in arctic research, given its small population size and remote location? Clearly, the magnitude of the disparities in health suggested by the existing data on suicide and alcohol use indicates existence of a serious long-term unaddressed public health crisis. A crisis of such proportions constitutes a key USG priority for solution-focused research. Implications of successful research strategies in the U.S. Arctic that develop solutions to this crisis also extend well beyond the arctic. Research in the U.S. Arctic is characterized by the same barriers found in many other areas of global health research, including limited research, health care, professional, and transportation infrastructure. Additionally, research in AN settings involves, as a crucial part of the work, a government-to-government research relationship, often with tribal entities. Current global health research, training, and capacity building activities are inadequate to meet this need. Research in the U.S. Arctic can inform global health research.
Acknowledgements
This article is dedicated to Gerald V. Mohatt, who started work on this paper, but passed away during the early preparation of this manuscript. For the past 30 years, Jerry was a champion of Arctic research, the health of people living in the Arctic, and the rights of Indigenous people. Jerry served as founding director of the Center for Alaska Native Health Research. His contribution to circumpolar research has been immense, and he will be missed by all of us whose lives he touched. Work on this manuscript was supported in part by National Center for Minority Health Disparities [R24 MD001626], National Institute of Neurological Disease and Stroke [01 NS0406904-04Revised, U01NS048069-04S1; U01NS048069-04S2], National Science Foundation [ARC-0756211], and National Center for Research Resources [P20RR061430] awards to the second author.
Footnotes
Conftict of interest statement Mohatt and Allen have no financial or personal relationships with people and/or organisations that could potentially influence the results or interpretation of the work being submitted. Levintova is an employee of the National Institutes of Health Fogarty International Center and has no conflicts of interest with the publication of this manuscript. The statements in this manuscript are of the authors alone and do not represent a position of U.S. government.
References
- 1.Hull-Jilly DMC, Casto LD. State epidemiologic profile on substance use, abuse and dependency. Section of Prevention and Early Intervention Services, Division of Behavioral Health, Alaska Department of Health and Social Services; Juneau (AK): 2008. Internet. [cited 2010 Oct 1]. Available from: http://www.hss.state.ak.us/dph/ipems/injury_prevention/Assets/SEOW-2001-2005.pdf. [Google Scholar]
- 2.Fortuine R. Chills and fever: Health and disease in the early history of Alaska. University of Alaska Press; Fairbanks, (AK): 1989. [Google Scholar]
- 3.Björkstén KS, Kripke DF, Bjerregaard P. Accentuation of suicides but not homicides with rising latitudes of Greenland in the sunny months. BMC Psychiatry. 2009;9:20. doi: 10.1186/1471-244X-9-20. Internet. [10 pages]: [cited 2010 Oct 1]. Available from: http://www.biomedcentral.com/content/pdf/1471-244x-9-20.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Perkins R, Sanddal TL, Howell M, Sanddal ND, Berman A. Epidemiological and follow-back study of suicides in Alaska. Int J Circumpolar Health. 2009 Jun;68(3):212–23. doi: 10.3402/ijch.v68i3.18334. [DOI] [PubMed] [Google Scholar]
- 5.Alaska Injury Prevention Center. Critical Illness and Trauma Foundation, Inc. American Society for Suicidology . Alaska suicide follow-back study final report. Alaska Department of Health and Social Services; Juneau (AK): 2007. Internet. [cited 2010 Oct 1]. Available from: http://www.hss.state.ak.us/suicideprevention/pdfs_sspc/sspcfollowback2-07.pdf. [Google Scholar]
- 6.Kraus RF. Suicidal behavior in north Alaskan Eskimo. Alaska Medicine. 1974;16:2–6. [Google Scholar]
- 7.Kraus RF, Buffler PA. Sociocultural stress and the American Native in Alaska: An analysis of changing patterns of psychiatric illness and alcohol abuse among Alaskan Natives. Culture, Medicine and Psychiatry. 1979;3(2):111–51. doi: 10.1007/BF00052965. [DOI] [PubMed] [Google Scholar]
- 8.Kettl PA, Bixler EO. Suicide in Alaska natives, 1979–1984. Psychiatry: Journal for the Study of Interpersonal Processes. 1991;54(1):55–63. doi: 10.1080/00332747.1991.11024530. [DOI] [PubMed] [Google Scholar]
- 9.Kettl PA, Bixler EO. Alcohol and suicide in Alaska Natives. American Indian and Alaska Native Mental Health Research. 1993;5(2):34–45. doi: 10.5820/aian.0502.1993.34. [DOI] [PubMed] [Google Scholar]
- 10.Andereggen DL, Zangri A, Vigue M. Alaska Bureau of Vital Statistics annual report 1986–1987. Alaska Department of Health and Social Services; Juneau (AK): 1990. [Google Scholar]
- 11.Centers for Disease Control . WISQARS. National Center for Injury Prevention and Control, Centers for Disease Control; 2009. [cited 2009 July 14]; Available from: National Center for Injury Prevention and Control, Centers for Disease Control http://webappa.cdc.gov/sasweb/ncipc/mortrate.html. [Google Scholar]
- 12.Brems C. Substance use, mental health, and health in Alaska: Emphasis on Alaska Native people. Arctic Medical Research. 1996;55:135–47. [PubMed] [Google Scholar]
- 13.Bjerregaard P, Young TK. The circumpolar Inuit: Health of a population in transition. Munksgaard; Copenhagen, Denmark: 1998. [Google Scholar]
- 14.Ward JA, Fox J. A suicide epidemic on an Indian reserve. The Canadian Psychiatric Association Journal / La Revue de l'Association des psychiatres du Canada. 1977;22(8):423–6. doi: 10.1177/070674377702200804. [DOI] [PubMed] [Google Scholar]
- 15.Bechtold DW. Cluster suicide in American Indian adolescents. Am Indian Alsk Native Ment Health Res. 1988;1(3):26–35. doi: 10.5820/aian.0103.1988.26. [DOI] [PubMed] [Google Scholar]
- 16.Middlebrook DL, LeMaster PL, Beals J, Novins DK, Manson SM. Suicide prevention in American Indian and Alaska Native communities: A critical review of programs. Suicide Life-Threat. 2001 Spr;31:132–49. doi: 10.1521/suli.31.1.5.132.24225. [DOI] [PubMed] [Google Scholar]
- 17.Doak B, Nachmann B. Violent deaths among young adults in southwest Alaska villages: A subgroup of a longitudinal cohort study. Alaska Native Medical Center; Anchorage (AK): 1987. [Google Scholar]
- 18.Wexler L, Hill R, Bertone-Johnson E, Fenaughty A. Correlates of Alaska Native fatal and nonfatal suicidal behaviors 1990–2001. Suicide Life-Threat. 2008 Jun;38(3):311–20. doi: 10.1521/suli.2008.38.3.311. [DOI] [PubMed] [Google Scholar]
- 19.Gessner BD. Temporal trends and geographic patterns of teen suicide in Alaska, 1979–1993. Suicide Life-Threat. 1997 Fal;27(3):264–73. Empirical Study. [PubMed] [Google Scholar]
- 20.Alaska Department of Education and Early Development and Alaska Department of Health and Social Services . 2007 Youth Risk Behavior Survey results. Alaska Department of Education and Early Development and Department of Health and Social Services; Juneau (AK): 2007. Internet. [cited 2009 August 8]. Available from: http://www.hss.state.ak.us/dph/chronic/school/pubs/YRBS-ALL.pdf. [Google Scholar]
- 21.Schoelhorn J, Podvin D. Fetal Alcohol Syndrome prevalence in Alaska: New findings from the FAS Surveillance Project. Family Health Dataline. 2002;8(2):1–5. [Google Scholar]
- 22.Alaska Department of Health and Social Services . Health risks in Alaska among adults: Behavioral Risk Factor Survey 2007 annual report. Alaska Department of Health and Social Services; Juneau (AK): 2007. [Google Scholar]
- 23.Mohatt GV, Rasmus SM, Thomas L, Allen' J, Hazel' K, Hensel C. “Tied together like a woven hat:” Protective pathways to Alaska Native sobriety. Harm Reduct J. 2004 Nov 17;1:10. doi: 10.1186/1477-7517-1-10. Internet. [12 pages]; [cited 2010 Oct 1]. Available from: http://www.harmreductionjournal.com/content/pdf/1477-7517-1-10.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mohatt GV, Hazel KL, Allen J, Stachelrodt M, Hensel C, Fath R. Unheard Alaska: Culturally anchored participatory action research on sobriety with Alaska natives. Am J Community Psychol. 2004;33(3):263–73. doi: 10.1023/b:ajcp.0000027011.12346.70. [DOI] [PubMed] [Google Scholar]
- 25.Seale JP, Shellenberger S, Spence J. Alcohol problems in Alaska Natives: Lessons from the Inuit. Am Indian Alsk Native Ment Health Res. 2006;13(1):1–31. doi: 10.5820/aian.1301.2006.1. [DOI] [PubMed] [Google Scholar]
- 26.Office of Applied Statistics: Substance Abuse and Mental Health Services Administration (US) 2004 state estimates of substance use and mental health (from the 2003–2004 National Surveys on Drug Use & Health) Substance Abuse and Mental Health Services Administration; Washington DC: 2008. Internet. [cited 2009 August 8]. Available from: http://www.oas.samhsa.gov/2k4State/appB.htm. [Google Scholar]
- 27.Brems C, Johnson ME, Neal D, Freemon M. Childhood abuse history and substance use among men and women receiving detoxification services. Am J Drug Alcohol Abuse. 2004;30(4):799–821. doi: 10.1081/ada-200037546. [DOI] [PubMed] [Google Scholar]
- 28.Gorey KM, Leslie DR. The prevalence of child sexual abuse: Integrative review adjustment for potential response and measurement biases. Child Ab Negl. 1997 Apr;21(4):391–8. doi: 10.1016/s0145-2134(96)00180-9. [DOI] [PubMed] [Google Scholar]
- 29.Johnson ME, Brems C, Mills ME, Fisher DG. Psychiatric symptomatology among individuals in alcohol detoxification treatment. Addict Behav. 2007;32(8):1745–52. doi: 10.1016/j.addbeh.2006.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alaska Bureau of Vital Statistics . Data and Statistics. Alaska Department of Health and Social Services; Juneau (AK): 2009. Internet. [cited 2009 August 2]. Available from: http://www.hss.state.ak.us/dph/bvs/data/default.htm. [Google Scholar]
- 31.Day G, Provost E, Lanier A. Alaska Native morality update: 1999–2003. Alaska Native Epidemiology Center; Alaska Native Tribal Health Consortium; Anchorage (AK): 2006. [cited 2009 August 2]. Available from: www.anthc.org/cs/chs/epi/pubs.cfm. [Google Scholar]
- 32.Hesselbrock MN, Hesselbrock VM, Segal B, Schuckit MA, Bucholz K. Ethnicity and psychiatric comorbidity among alcohol- dependent persons who receive inpatient treatment: African Americans, Alaska Natives, Caucasians, and Hispanics. Alcohol Clin Exp Res. 2003 Aug;27(8):1368–73. doi: 10.1097/01.ALC.0000080164.21934.F9. [DOI] [PubMed] [Google Scholar]
- 33.Parks CA, Hesselbrock MN, Hesselbrock VM, Segal B. Gender and reported health problems in treated alcohol dependent Alaska natives. J Stud Alcohol. 2001 May;62(3):286–93. doi: 10.15288/jsa.2001.62.286. [DOI] [PubMed] [Google Scholar]
- 34.Levintova M, Zapol WI, Engmann N, editors. Circumpolar Health Supplements. 2010. Behavioral and mental health research in the Arctic: strategy setting meeting 2010; p. 5. [DOI] [PubMed] [Google Scholar]
- 35.Allen J, Mohatt G, Fok CC, Henry D, PA Team Suicide prevention as a community development process: understanding circumpolar youth suicide prevention through community level outcomes. Int J Circumpolar Health. 2009 Jun;68(3):274–91. doi: 10.3402/ijch.v68i3.18328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ulturgasheva O, Wexler L, Kral M, Allen J, Mohatt GV, Nystad K. CIPA Team Navigating international, community-based participatory health research: Indigenous culture, social change, and negotiating pathways to adulthood in five circumpolar communities. Journal of Community Engagement and Scholarship. in press. [PMC free article] [PubMed] [Google Scholar]
- 37.Manson S. Barrow alcohol study: Emphasis on its ethical and procedural aspects. Am Indian Alsk Native Ment Health Res. 1989;2(3):5–6. special issue. [Google Scholar]
- 38.Mohatt GV, Rasmus SM, Thomas L, Allen J, Hazel K, Marlatt GA. Risk, resilience, and natural recovery: A model of recovery from alcohol abuse for Alaska Natives. Addiction. 2008;103(2):205–15. doi: 10.1111/j.1360-0443.2007.02057.x. [DOI] [PubMed] [Google Scholar]
- 39.Allen J, Mohatt GV, Rasmus SM, Hazel KL, Thomas L, Lindley S, PA Team The Tools to Understand: Community as Co-Researcher on Culture-Specific Protective Factors for Alaska Natives. J Prev Interv Community. 2006;32(1):41–59. doi: 10.1300/J005v32n01_04. [DOI] [PubMed] [Google Scholar]
- 40.Petraitis J, Flay BR, Miller TQ. Reviewing theories of adolescent substance use: Organizing pieces in the puzzle. Psychological Bull. 1995;117(1):67–86. doi: 10.1037/0033-2909.117.1.67. [DOI] [PubMed] [Google Scholar]
- 41.Timonen M. Special editorial. Int J of Circumpolar Health. 2009;68(8):202–3. doi: 10.3402/ijch.v68i3.18337. [DOI] [PubMed] [Google Scholar]