Summary
Multiple CNS infections can coexist in advanced AIDS, but are most commonly reported in autopsy case studies. We now describe the case of an HIV+ individual, who was first diagnosed with CNS toxoplasmosis, confirmed by brain biopsy. After initiation of combined anti-retroviral therapy (cART) and successful treatment of CNS toxoplasmosis, he developed worsening neurological symptoms and was subsequently diagnosed with progressive multifocal leukoencephalopathy. Retrospective analysis of the MRI scans indicated that PML was already present early on but was interpreted as edema associated with CNS toxoplasmosis. Clinicians should be aware that multiple pathologies may coexist in the brain of immunosuppressed individuals and that PML may develop and worsen despite the use of cART.
Keywords: JC virus, progressive multifocal leukoencephalopathy, CNS toxoplasmosis, HIV, viral Infections, AIDS
Introduction
CNS opportunistic infections (OI) and tumors are frequent in advanced AIDS. In 1991, before the availability of combined anti-retroviral therapy (cART), CNS toxoplasmosis occurred in 72.2% and PML in 5.6% of HIV+ patients presenting with focal brain lesions 1. We describe the case of an HIV-1-infected man with concomitant brain diseases.
Case report
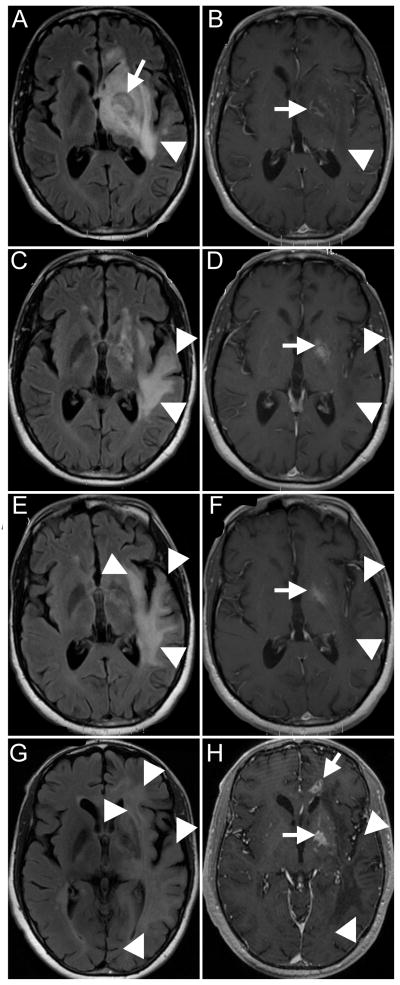
A 40-year-old untreated HIV+ man with CD4+ T-cell count of 7/ul (3%) and HIV plasma VL of 356,768 copies/ml presented to an outside hospital with 18 days history of fluctuating headache, right-sided weakness and fever. MRI of the brain showed a mass lesion in the left basal ganglia (figure, A, arrow) with surrounding hyperintense signal in fluid-attenuated inverse recovery (FLAIR) images, attributed to edema, extending in left temporal lobe (figure, A, arrowhead). There was ring enhancement in post-contrast T1-weighted image (figure, B, arrow). Because he was allergic to sulfa drugs, he was started on pyrimethamine and clindamycin for suspected CNS toxoplasmosis. Since he had a single brain lesion, a stereotactic brain biopsy was performed to rule out primary CNS lymphoma, which confirmed the diagnosis of toxoplasmosis.
Figure.
(A–B) MRI at the time of initial presentation. Fluid Attenuated Inverse Recovery image (FLAIR) (A) shows a toxoplasmosis lesion in the left basal ganglia (arrow), with surrounding hyperintense signal, attributed to edema (arrowhead). Post-gadolinium T1 image (B) shows ring enhancement around the toxoplasmosis lesion (arrow), and hypointense signal in the surrounding area (arrowhead). (C–D) MRI obtained one month after original presentation. FLAIR sequence (C) shows almost complete resolution of the left basal ganglia lesion (arrow), but progression of the white matter hyperintensities (arrowheads). Post-biopsy changes are seen in the left basal ganglia on T1 with gadolinium (D, arrow), which were also present on pre-contrast T1 images (not shown). There is no enhancement of the temporal lobe lesions (D, arrowheads). (E–F) Third MRI shows further progression of the hyperintense lesions on FLAIR (E, arrowheads), which where hypointense and did not enhance with contrast on T1 images (F, arrowheads). The original toxoplasmosis lesion is indicated by the arrow in F. (G–H) Last MRI shows again progression of the white matter lesions of PML on FLAIR (G, arrowheads), which remain hypointense on magnetization-prepared 180 degrees radio-frequency pulses and rapid gradient-echo T1 sequence (H, arrowheads). There is new contrast enhancement in the basal ganglia and in the anterior corpus callosum (H, arrows), suggestive of a recurrence of toxoplasmosis.
The patient improved clinically, and a second MRI done 4 weeks later showed almost complete resolution of the basal ganglia lesion on FLAIR (figure, C, arrow) and post-biopsy changes on post-contrast T1 images (figure, D, arrow). However, there was increase in the surrounding hyperintense signal in FLAIR images in the left temporal, parietal and frontal lobe (figure, C, arrowheads) which appeared hypointense in post-contrast T1 images (figure, D, arrowheads). The patient was started on cART with tenofovir/emtricitabine and raltegravir and anti-toxoplasmosis medications were continued. A third MRI performed 2 weeks later showed extension of the white matter abnormalities in the same lobes (figure, E–F, arrowheads) and post-biopsy changes on post-contrast T1-images (figure, F, arrow). While the right-sided weakness had subsided, the patient had developed expressive aphasia. Two months after the initial presentation, his CD4+ T-cell count had increased to 53/ul (6%) and plasma HIV VL had decreased to 1762 copies/ml. A lumbar puncture was performed, and quantitative PCR demonstrated a very high JC virus load (45 million copies/ml), establishing the diagnosis of PML. Eight weeks after onset of cART, the plasma HIV VL was < 75 copies/ml, but the CD4+ T-cell count decreased to 24/ul (3%). The patient developed severe expressive and receptive aphasia, right homonymous hemianopia, right hemiparesis, and disinhibition. A last MRI performed 3.5 months after disease onset showed that the PML lesions were present in almost the entire left hemisphere, the right parietal lobe, with isolated foci in the right frontal lobe and the left cerebellar peduncle (figure, G–H, arrowheads). There was no contrast enhancement in the PML lesions (figure, H, arrowheads). Interestingly, there was again new contrast enhancement at the site of the left basal ganglia lesion and in the anterior part of the left corpus callosum (figure, H, arrows). Mirtazapine 15 mg qhs and mefloquine 250 mg once a day for the first three days, followed by once weekly thereafter, were added as experimental treatments for PML 2–3. Despite these medications, he continued to worsen, developed pneumonia and passed away 5 months after initial presentation. No post mortem exam was performed.
Discussion
We report an HIV+ patient with concomitant toxoplasmosis and PML. Multiple CNS OI can co-exist in AIDS patients 1, 4, but are most commonly reported in autopsy case studies 5–6.
Indeed, lesions of PML were likely already present in the left temporal lobe, adjacent to the edema caused by toxoplasmosis. Interestingly, serial MRIs showed increase of the surrounding hyperintensities and disappearance of the original lesion on FLAIR after treatment for toxoplasmosis. Since the repeat imaging was suggestive of PML, lumbar puncture was done, which showed JCV DNA in CSF, confirming the diagnosis. PML progressed despite treatment with cART, with good control of HIV replication in the blood, but with only limited immunologic response, as measured by the CD4+ T cell count. It is possible that a lag in recovery of the immune system allowed PML to spread. In addition, a new contrast-enhancing lesion in the corpus callosum was seen on the last MRI which is suggestive of recurrent toxoplasmosis. Alternatively, worsening of PML may have been caused by an immune reconstitution inflammatory syndrome (IRIS). However, this is less likely because of the absence of contrast enhancement in PML lesions on MRI, and the modest increase in CD4+ T cell count, which was subsequently followed by a decrease. In contrast with our case, an HIV-negative immunosuppressed patient has recently been reported in whom the MRI showed hyperintense white matter lesions consistent with PML, but brain biopsy showed typical features of PML in combination with ruptured toxoplasmosis cysts 7.
Clinicians should be aware that multiple pathologies may coexist in the brain of immunosuppressed individuals and that PML may develop and worsen despite the use of cART.
Acknowledgments
Dr Koralnik has received a research grant from Biogen Idec, has been a consultant advisor for Bristol Myers Squibb, Ono pharmaceuticals, Merck Serono, Alnylam and Antisense and is funded by NIH grants R01 NS 041198 and 047029 and K24 NS 060950.
Footnotes
The authors have no conflict of interest.
Disclosure
Dr Gheuens is funded by NIH grant T32 AI07387-21 and is a fellow of the Clinical Investigator Training Program: Beth Israel Deaconess Medical Center – Harvard/MIT Health Sciences and Technology, in collaboration with Pfizer Inc. and Merck & Co.
Dr Cheeseman reports no disclosures.
References
- 1.Ammassari A, Cingolani A, Pezzotti P, et al. AIDS-related focal brain lesions in the era of highly active antiretroviral therapy. Neurology. 2000;55:1194–1200. doi: 10.1212/wnl.55.8.1194. [DOI] [PubMed] [Google Scholar]
- 2.Brickelmaier M, Lugovskoy A, Kartikeyan R, et al. Identification and characterization of mefloquine efficacy against JC virus in vitro. Antimicrob Agents Chemother. 2009;53:1840–1849. doi: 10.1128/AAC.01614-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elphick GF, Querbes W, Jordan JA, et al. The human polyomavirus, JCV, uses serotonin receptors to infect cells. Science. 2004;306:1380–1383. doi: 10.1126/science.1103492. [DOI] [PubMed] [Google Scholar]
- 4.Lima MA, Katz-Brull R, Lenkinski RE, Nunez R, Feinrider D, Koralnik IJ. Remission of progressive multifocal leukoencephalopathy and primary central nervous system lymphoma in an HIV-infected patient. Eur J Neurol. 2007;14:598–602. doi: 10.1111/j.1468-1331.2007.01820.x. [DOI] [PubMed] [Google Scholar]
- 5.Martinez AJ, Sell M, Mitrovics T, et al. The neuropathology and epidemiology of AIDS. A Berlin experience. A review of 200 cases. Pathol Res Pract. 1995;191:427–443. doi: 10.1016/S0344-0338(11)80730-2. [DOI] [PubMed] [Google Scholar]
- 6.Zelman IB, Mossakowski MJ. Opportunistic infections of the central nervous system in the course of acquired immune deficiency syndrome (AIDS). Morphological analysis of 172 cases. Folia Neuropathol. 1998;36:129–144. [PubMed] [Google Scholar]
- 7.Desmond R, Lynch K, Gleeson M, Farrell M, Murphy P. Progressive multifocal leukencephalopathy and cerebral toxoplasmosis in a patient with CLL. Am J Hematol. 2010;85:607. doi: 10.1002/ajh.21589. [DOI] [PubMed] [Google Scholar]