Abstract
We report a case of subcutaneous phaeohyphomycosis of foot, which is a mycotic disease that produces brown pigmented hyphae, pseudohyphae and yeast form in combination. The patient was immunocompetent and had injury 23 years before, and developed a non healing foot ulcer which was clinically suspected as tuberculous or carcinomatous etiology. Local wide excision was done and sent in formalin for histopathological examination. Microscopically pigmented septate, hyphae and yeast forms were identified on hematoxylin and eosin stained sections which were confirmed by special stains such as periodic acid-Schiff and Gomori's methenamine silver stains.
Keywords: Phaeohyphomycosis, post traumatic non healing chronic ulcer
INTRODUCTION
Phaeohyphomycosis is a term coined by Ajello et al.[1] It is a mycotic disease caused by melanin containing fungus, characterized by the presence of dematiaceous (dark-walled) septate hyphae, pseudohyphae and sometimes yeast or a combination of all these in tissue.[2,3]
It is a saprophyte found in soil, wood and plant material in tropical and subtropical areas. Subcutaneous infection results from invasive traumatic injury usually in immunocompromised individuals. Most of the time, diagnosis is unsuspected and delayed because of its rarity and varied presentation. We report a case of subcutaneous Phaeohyphomycosis of foot in immunocompetent patient presenting as a post traumatic chronic non healing ulcer of 2 years duration.
CASE REPORT
A 46 year old lady, resident of urban Delhi, presented with non healing ulcer over left foot since two years. She met a road traffic accident 23 years back and had avulsion injury of dorsum of left foot and had skin grafting over the dorsum of foot, with amputation of great toe. Apparently, it was healthy till 13 years and thereafter she started having recurrent breakdown of graft, which subsided after taking local wound care. She presented to our department with complaints of non-healing painful ulcer since 2 years, which was not responding to previous medications. She had no history of immunosuppressants or steroid medications in past. She was non- diabetic and had no other systemic or underlying disease. Enzyme-linked immunosorbent assay (ELISA) for Human immunodeficiency virus -1 and 2 (HIV-1 and HIV-2) were non-reactive and viral marker study was negative for hepatitis-B and hepatitis-C infection. Routine hematological and biochemistry tests were normal. Clinically, it was suspected as tubercular versus carcinomatous ulcer because of its longer duration. Local wide excision was done and tissue was sent for histopathological initially, and later for mycological examination after histopathological diagnosis of Phaeohyphomycosis. Excised tissue sections were stained with hematoxylin and eosin [Figure 1], Gomori's methenamine silver (GMS) stains [Figure 2] and periodic acid-Schiff [Figure 3]. Sections stained by hematoxylin and eosin showed dark brown pigmented hyphal elements along with yeast like spores surrounded by mixed inflammatory infiltrates, epitheloid cells, and multinucleated giant cells.
Figure 1.
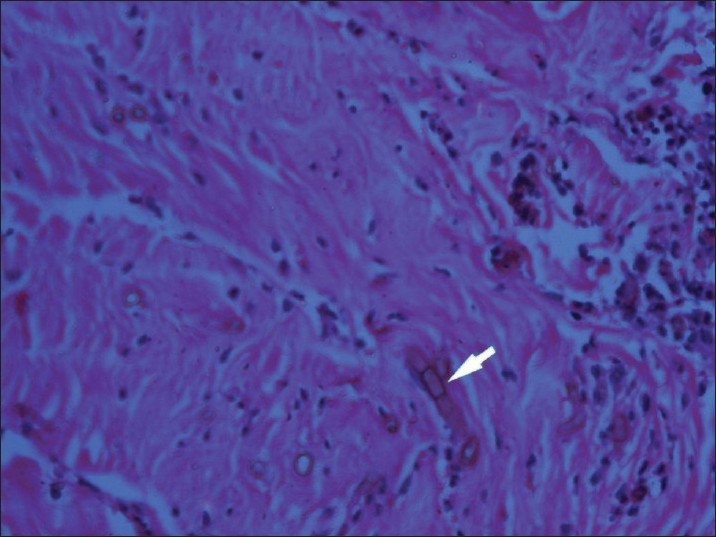
Pigmented septate hyphae with diffuse chronic inflammatory infiltrates (Hematoxylin and Eosin stain, ×40)
Figure 2.
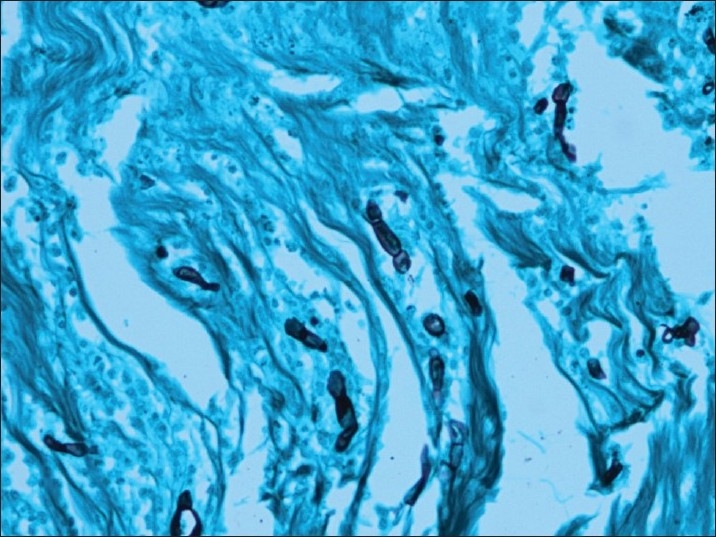
Dark pigmented fungal hyphae (Gomori's methenamine silver stain, ×40)
Figure 3.
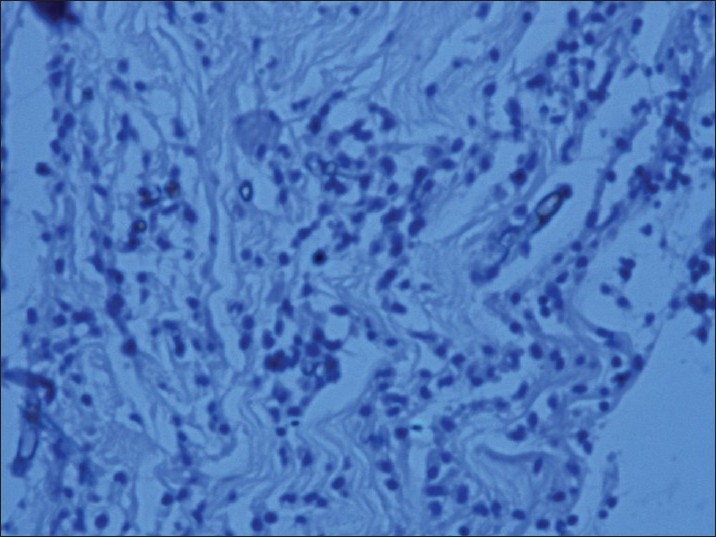
Pigmented septate fungal hyphae (Periodic acid-Schiff stain, ×40)
Special staining by periodic-acid-Schiff and GMS stains demonstrated numerous darkly pigmented, septate, hyphal fragments admixed with yeast like spores consistent with the diagnosis of Phaeohyphomycosis. Histopathological examination of serial sections and margins of ulcer tissue have shown no evidence of dysplasia or carcinomatous changes. Ziehl-Nielsen staining was done for acid fast bacilli and it was negative for tubercle bacilli. Since wide excision biopsy was sent in formalin, no ulcer tissue was left to perform mycological study to find out species. However, swab cultures and tissues taken from post-operative resected margins were sent for mycological examination. Direct Potassim hydroxide - KOH (10%) mount was prepared and no hyphae or budding yeast cells were seen. Tissue was sub cultured on three culture media – SDA (Sabouraud's Dextrose Agar) with gentamycin, SDA without gentamycin and PDA (Potato Dextrose Agar), and incubated for three weeks at 37°C and 22°C and no growth was seen. At present, she is on antifungal treatment with tab itraconazole 400 mg daily for 3 weeks with tapering dosage to 200 mg daily for 2 weeks and final dose of 100 mg daily for 1 month. Open raw area was grafted and patient is responding well to antifungal antibiotics.
DISCUSSION
There are three types of mycosis by dematiaceous fungi, namely, Phaeohyphomycosis, chromoblastomycosis and mycetoma. Phaeohyphomycosis is a rare cutaneous, subcutaneous or systemic infection that contains brown pigmented mycelial elements in tissue, which differs from the chromoblastomycosis and mycetoma by absence of sclerotic cells and grains.[3,4] These fungi are often found in soil, wood and plant as saprophytes in tropical and subtropical areas. It is more commonly found in northern and southern part of India, which provide ideal environment for their growth. In India 18 cases of subcutaneous Phaeohyphomycosis have been reported affecting various body parts.[5] Phaeohyphomycosis is caused by brown pigmented fungi having melanin in their cell walls. Melanin acts as a virulence factor because of its scavenging effects over free radicals and hypochlorite's produced by phagocytic cells, and moreover it binds to hydrolytic enzymes. This may be the explanation for infection in immunocompetent hosts.[6] Mode of transmission of infection is usually trauma in immunocompromised and immunocompetent individuals.
In this case, presumed source of infection is due to inoculation of fungus while she had avulsion injury in road traffic accident. Delayed presentation of symptoms may be due to dormant infective nidus under the grafted wound in this immunocompetent case, which overtime went on to become symptomatic. There are other cases in literature suggesting similar sequence of events.
Case report by Torstrick et al. had documented a case of a slowly enlarging olecranon bursal mass due to Phaeohyphomycosis after a thorn puncture wound sustained over 30 years before.[7] Another case report by Kaell et al. had mentioned a case where a patient had a glass injury to the knee in childhood and several years later, this nidus was likely a source of the acute fungal arthritis observed in this case (Phaeoacremonium parasiticum).[8]
Since it is a ubiquitous fungus with increasing incidence after trauma, it should also be remembered that it is often misdiagnosed as carcinomatous non healing ulcer. We have presented this case report to increase awareness about this rare fungal infection in immunocompetent individuals, with longer duration of trauma history. Here it was previously considered as a non-healing ulcer of either tuberculous or carcinomatous type, with high level of suspicion. Histopathological examination of tissue section along with special staining plays a vital role in deciding the confirmatory diagnosis of Phaeohyphomycosis, which then alleviated the anxiety of patient as well as the treating clinician.
ACKNOWLEDGMENT
We sincerely thank our technicians - Thang Chin Lian, Renu Rani and Meenakshi Sharma who helped in establishing the histopathology section for laboratory medicine. They helped in processing the tissue sample for this study.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Ajello L, Georg LK, Steigbigel RT, Wang CJ. A case of phaeohyphomycosis caused by a new species of Phialophora. Mycologia. 1974;66:490–8. [PubMed] [Google Scholar]
- 2.Kwon-Chung KJ, Bennett JE. Phaeohyphomycosis. In: Kwon Chung KJ, Bennett JE, editors. Medical mycology. Philadelphia: Lea and Febiger; 1992. pp. 620–77. [Google Scholar]
- 3.Rossmann SN, Cernoch PL, Davis JR. Dematiaceous fungi are increasing cause of human disease. Clin Infect Dis. 1996;22:73–80. doi: 10.1093/clinids/22.1.73. [DOI] [PubMed] [Google Scholar]
- 4.Fader RC, McGinnis MR. Infections caused by dematiaceous fungi: Chromoblastomycosis and phaeohyphomycosis. Infect Dis Clin North Am. 1988;2:925–38. [PubMed] [Google Scholar]
- 5.Kiran Kumar K, Kaveri Kallekeri. Phaeohyphomycosis. Indian J Pathol Microbiol. 2008;51:556–8. doi: 10.4103/0377-4929.43761. [DOI] [PubMed] [Google Scholar]
- 6.Revankar SG. Phaeohyphomycosis. Infect Dis Clin North Am. 2006;20:609–20. doi: 10.1016/j.idc.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 7.Torstrick RF, Harrison K, Heckman JD, Johnson JE. Chronic bursitis caused by Phialophora richardsiae.A case report. J Bone Joint Surg Am. 1979;61:772–4. [PubMed] [Google Scholar]
- 8.Kaell AT, Weitzman I. Acute monoarticular arthritis due to Phialophora parasitica. Am J Med. 1983;74:519–22. doi: 10.1016/0002-9343(83)91001-x. [DOI] [PubMed] [Google Scholar]


