Abstract
Context:
Critical care units provide a favourable environment for the antimicrobial resistant organisms to disseminate. There is recent increase in number of extended spectrum beta lactamase (ESBL) producers because of the emergence of CTX M Beta lactamases produced by Enterobacteriaceae. They colonize the intestinal flora and spread with greater intensity in the community and hospital. Usage of Carbapenems becomes mandatory as the ESBL inhibitor combination antibiotics (Amoxicillin/Clavulanate) are not effective especially against CTX M ESBLs.
Aim:
The aim of this study is to detect ESBL producing bla CTX M gene in Enterobacteriaceae from infections in Critical care patients and to stress on the intensity of the problem and to make interventions to curb the emergence and dissemination of CTX M ESBLs.
Materials and Methods:
A total of 118 Enterobacteriaceae isolates from Critical care unit patients were recovered from a variety of clinical specimens. Antimicrobial susceptibility test was done and isolates with resistance or with reduced susceptibility to any of the third generation Cephalosporins were selected for the study. Phenotypic confirmation of ESBL production was done by Double Disc Synergy Test and confirmed by minimum inhibitory concentration. Multiplex polymerase chain reaction was performed to screen the four groups of CTX-M ESBLs.
Results:
Among the 118 isolates of Enterobacteriaceae 54 isolates were positive for CTX-M group I ESBL which constitutes 45.7 %.
Conclusions:
Early detection of CTX M producing Enterobacteriaceae by continuous surveillance and thereby reducing their spread and restricted use of third generation Cephalosporins (3GC) antibiotics could be the possible routes to prevent the emergence and spread of CTX M ESBL producing organisms.
Keywords: CTX M, Critical care, Enterobacteriaceae, Extended spectrum beta lactamase
INTRODUCTION
Antimicrobial resistance is an emerging problem in treating the critically ill patients. The production of extended-spectrum beta-lactamase (ESBL) is one of the most important mechanisms of antimicrobial resistance. Recent increase in number of ESBLs attributes to the emergence of beta-lactamase producing blaCTX M gene in Enterobacteriaceae.[1] This study focuses on detecting blaCTX M ESBL producing Enterobacteriaceae from infections in critical care patients and to bring awareness to the clinicians about the intensity of the problem and to make interventions to curb the emergence and dissemination of CTX M ESBLs.
MATERIALS AND METHODS
A total of 118 Enterobacteriaceae from critical care units patients were recovered over a period of eight months (January 2010 to August 2010) from a variety of clinical specimens, i.e. urine, pus, sputum, blood, catheter tips, tracheal secretions, endotracheal tube etc. Identification of these isolates was done based on colony morphology on blood agar, MacConkey agar and by standard biochemical reactions.[2] Antibiotic susceptibility testing was done on Muller-Hinton agar after standardizing the suspension to 0.5 McFarland's standards. The sensitivity of the isolates to 3 GC (Ceftriaxone, Ceftazidime and Cefotaxime) and to the other antibiotics such as Cotrimoxazole, Amikacin, Ciprofloxacin, Cefepime (Fourth generation cephalosporins), Augumentin and Imepenem was determined by Disc Diffusion Method. The results were interpreted as per Clinical and Laboratory Standards Institute (CLSI) recommendations.[3] Escherichia coli ATCC 25922 strain was used for quality control. Isolates with resistance or with reduced Susceptibility to Ceftriaxone (‹ 21 mm), Ceftazidime (‹ 18 mm) and Cefotaxime (‹ 20 mm) were selected for the study.
Extended spectrum beta lactamase detection by double disc synergy test
In the DDST, synergy was determined between a disc consisting 20 mcg of Amoxicillin and 10 mcg of Clavulanic Acid (Augmentin) and 30 mcg disc of each of the 3 GC antibiotics placed at a distance of 30 mm apart on a lawn culture of the resistant isolate under test on Muller-Hinton Agar (MHA) (Hi Media, India).[4] The test organism was considered to produce ESBL if the zone size around the test antibiotic increased towards the Augmentin disc. Escherichia coli ATCC 25922 and Klebsiella pneumoniae ATCC 700603 were used as negative and positive controls, respectively, for ESBL production.
Extended spectrum beta lactamase confirmation by minimum inhibitory concentration
MIC assay was performed on all strains that showed zone reduction for one or more of the 3GC antibiotics used in ESBL screening test. MIC was determined by agar dilution method against Ceftriaxone, Ceftazidime and Cefotaxime as described by National Committee for Clinical Laboratory Standards (NCCLS).[5]
Polymerase chain reaction screening
Multiplex PCR was performed on 68 Enterobacteriaceae isolates which were positive for ESBL by phenotypic detection, to screen the four-groups of CTX-M type ESBLs as described by Pitout JDD et al., 2004.[6] A loopful of bacteria grown in an agar plate were suspended in 50 μl of sterile water. Bacterial deoxyribonucleic acid (DNA) extraction was performed using the QIAMP DNA MINI kit (QIAGEN, Dueseeeldorf, Germany). 1 μL of the DNA template was added to 20 μL of the PCR reaction mixture. The cycling conditions were: initial DNA release and denaturation at 94°C for 3 minutes, followed by 25 cycles of 94°C for 30 seconds, 57°C for 30 seconds and 72°C for 30 seconds, followed by final elongation step at 72°C for 5minutes. The PCR products were analyzed by gel electrophoresis with 2 % agarose in Tris/Borate/ Ethylenediaminetetraacetic acid (TBE) with ethidium bromide (5 μg/ml) and visualized by ultraviolet (UV)-transillumination. A 100-bp DNA ladder (Invitrogen) was used as a marker.
RESULTS
A total of 118 Enterobacteriaceae isolates were obtained during the study period, of which 68 isolates showed enhanced zone size towards the Augmentin disc and were considered positive for ESBL by DDST. Of the 68 isolates, the zone around Cefatoxime was enhanced towards Augmentin in 51 isolates. Multiplex PCR yielded the products with predicted size for group 1 CTX-M (499 bp) enzyme in 54 isolates. The distribution of organisms in Enterobacteriaceae, results of their phenotypic confirmation for ESBL and PCR for CTX M were given in Table 1. MIC of 3GC antibiotics for ESBL producing Enterobacteriaceae is shown in Table 2. In our study among the 118 isolates of Enterobacteriaceae, 54 isolates were positive for CTX-M extended spectrum beta lactamase which constitutes 45.7% [Table 3] None of the isolates were Positive for CTX-M group II, CTX-M group III and CTX-M group IV ESBL's.
Table 1.
Results of phenotypic confirmation of extended spectrum beta lactamase and CTX M polymerase chain reaction
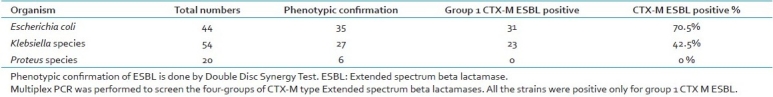
Table 2.
Minimum inhibitory concentration of 3gc antibiotics for Escherichia coli and Klebsiella
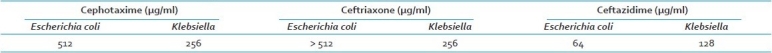
Table 3.
Enterobacteriaceae positive for CTX M

DISCUSSION
Many patients have to be hospitalized for a long duration and treated with heavy dose of antibiotics in the Critical Care units which facilitate them to acquire infection with multi drug resistant organisms.[7–9] Furthermore, there is a remarkable rise in morbidity and mortality as well as the expenses for the patients in the critical care units.[10,11] The commonest way of acquiring antibiotic resistance is by inactivating the antibiotic by the production of enzymes like beta-lactamases. The production of ESBLs is one of the most important mechanisms of antimicrobial resistance. Recent increase in number of ESBLs attributes to the emergence of CTX-M beta-lactamase producing Enterobacteriaceae.[1] Many studies have been conducted in the Critical Care units regarding antimicrobial resistant organisms.[11–14] But very few studies have been conducted about CTX M beta lactamases as blaCTXM is newly emerged gene of ESBL having preference for Enterobacteriaceae.[15,16] In our study, 68 isolates were found to be ESBL producers by phenotypic confirmation. Among them 35 isolates were Escherichia coli, 27 isolates were Klebsiella species. and 6 isolates were Proteus species. Among the 68 ESBL producers, 54 isolates were positive for CTX-M group I ESBL and all the isolates were negative for other CTX M Groups (Group II, III and IV) confirmed by PCR. These data could indicate that the ESBL phenotype is due to production of ESBLs other than CTX-Ms. This also shows that CTX-M group I is the predominant form in Enterobacteriaceae.[17] Our study is in accordance with James. S, et al. in which the most common CTX-M-type ESBL was CTX-M-15 in the critically ill patients recovered from blood and other sterile fluids.[18] Macrorestriction polymorphism of genomic is DNA determined by Pulse Field Gel Electrophoresis would indicate whether CTX M – 15 producing Enterobacteriaceae strains belong to a single clone.[19] The major clones of Escherichia coli isolates with CTX M – 15 Beta lactamase had 78% similarity by PFGE and may share a common ancestor as stated by D.M. Livermore, P.M.Howkey, et al. CTX-M group I includes CTX- M-1, M-3, M-10 to M-12, M-15, M-22, M-23, M-28, M-29 and M-30.[6] Among the 54 CTX-M group I ESBL producing Enterobacteriaceae, 31 isolates were Escherichia coli, 23 were Klebsiella species and none of the Proteus species produced CTX M ESBL's. Escherichia coli is the predominant CTX M group I ESBL producing Enterobacteriaceae in our study. Cefatoxime was considered to be the best 3GC antibiotic for phenotypic ESBL detection, as most of the isolates (75%) were positive in DDST for cefotaxime. CTX M beta lactamases has raised many concerns that, among the first 105 patients infected with CTX-M-15-producing Escherichia coli in Shropshire, there had been 28 deaths in 2002 as stated by D.M. Livermore P.M.Howkey, et al.[1] The data of D.M.Livermore, Yuan M et al. is supportive of our study in which among the isolates with confirmed cephalosporin resistance, 51% were Escherichia coli, and a large number of Escherichia coli were with CTX-M enzymes.[14]
The same study shows that CTX M lactamases are increasingly prevalent in Enterobacteriaceae .[1] Endogenous intestinal flora formed by Enterobacteriaceae is the reservoir for CTX M beta lactamase infections and they colonize in the gut without harming the host. Munday CJ, et al., and Valverde A et al., have proved that CTX M ESBLs are carried by Enterobacteriaceae in the community fecal flora[15,16] and they are predominantly responsible for urinary tract infections.[20,21] This situation increases the potential of CTX M lactamases to disseminate rapidly in the community and produce serious infections which may not respond to the antibiotics that are used normally. D.M. Livermore, Yuan M, et al. has further mentioned that Enterobacteriaceae with CTX-M-15 (Group I) enzyme are resistant to inhibitor combinations (such as Piperacillin/Tazobactam and Amoxicillin/Clavulanate) by producing inhibitor-resistant penicillinases.[14] Reconsideration of antibiotics becomes mandatory and higher level antibiotics like Carbapenems may have to be used which in turn escalates the cost and duration of hospital stay for the patients.
This condition is even worse in Critical care units because of factors such as severity of illness in these patients, closeness with other patients, many invasive procedures (catheter, endotracheal tube, IV lines etc) and failure to follow aseptic conditions (hand washing etc). All these create a fertile environment for the antimicrobial resistant bacteria to disseminate in the Critical Care units which insists special care to be exercised in the management of Critical Care patients. Early detection of CTX M producing Enterobacteriaceae by repeated surveillance and usage of 3GC antibiotics under proper guidance could be the possible routes to prevent the emergence and spread of CTX M ESBL producing organisms.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Livermore DM, Hawkey PM. CTX M Changing The Face Of ESBLs in UK. J Antimicrob Chemother. 2005;56:451–4. doi: 10.1093/jac/dki239. [DOI] [PubMed] [Google Scholar]
- 2.Mackie, McCartney . Practical Medical Microbiology. 14th ed. New Delhi: Elsevier; 2007. Chapter 20 Enterobacteriaceae. J.Gerald Collee; pp. 362–3. [Google Scholar]
- 3.Clinical and Laboratory Standards Institute (CLSI). Performance standards for antimicrobial susceptibility testing. 20th informational supplement: M100-S20U Journal Of Clinical Microbiology. 2010;30:1–16. [Google Scholar]
- 4.Vercauteren E, Descheemaeker P, Ieven M, Sanders CG, Goossens H. Comparison of Screening methods for detection of extended spectrum lactamases and their prevalence among blood isolates of Escherichia coli and Klebsiella speciesin a Belgian Teaching Hospital. J Clin Microbiol. 1997;35:2191–7. doi: 10.1128/jcm.35.9.2191-2197.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.5th ed. Wayne, PA, USA: NCCLS, Approved Standard; 2000. National Committee for Clinical Laboratory Standards. Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically; pp. M7–A5. [Google Scholar]
- 6.Pitout JD, Hossain A, Hanson ND. Phenotypic and molecular detection of CTX-M lactamases produced by Escherichia coli and Klebsiella species. J Clin Microbiol. 2004;42:5715–21. doi: 10.1128/JCM.42.12.5715-5721.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haley RW, Bregman DA. The role of understaffing and overcrowding in recurrent outbreaks of staphylococcal infection in a neonatal special-care unit. J Infect Dis. 1982;145:875–85. doi: 10.1093/infdis/145.6.875. [DOI] [PubMed] [Google Scholar]
- 8.McGowan JE. Antibiotic resistance in hospital bacteria: current patterns, modes for appearance or spread, and economic impact. Rev Med Microbiol. 1991;2:161–9. [Google Scholar]
- 9.Appelgren P, Hellstrom I, Weitzberg E, Soderlund V, Bindslev L, Ransjo U. Risk factors for nosocomial intensive care infection - a long-term prospective analysis. Acta Anaesthesiol Scand. 2001;45:710–9. doi: 10.1034/j.1399-6576.2001.045006710.x. [DOI] [PubMed] [Google Scholar]
- 10.Rello J, Ollendorf DA, Oster G, Vera-Llonch M, Bellm L, Redman R, et al. Epidemiology and outcomes of ventilator-associated pneumonia in a large US database. Chest. 2002;122:2115–21. doi: 10.1378/chest.122.6.2115. [DOI] [PubMed] [Google Scholar]
- 11.Vincent JL, Bihari DJ, Suter PM, Bruining HA, White J, Nicolas-Chanoin MH, et al. The prevalence of nosocomial infection in intensive care units in Europe: results of the European Prevalence of Infection in Intensive Care (EPIC) Study.EPIC International Advisory Committee. JAMA. 1995;274:639–44. [PubMed] [Google Scholar]
- 12.Hanberger H, Garcia-Rodriguez JA, Gobernado M, Goossens H, Nilsson LE, Struelens MJ, et al. Antibiotic susceptibility among aerobic gram-negative bacilli in intensive care units in 5 European countries. JAMA. 1999;281:67–71. doi: 10.1001/jama.281.1.67. [DOI] [PubMed] [Google Scholar]
- 13.Archibald L, Phillips L, Monnet D, McGowan JE, Tenover F, Gaynes R. Antimicrobial resistance in isolates from inpatients and outpatients in the United States: increasing importance of the intensive care unit. Clin Infect Dis. 1997;24:211–5. doi: 10.1093/clinids/24.2.211. [DOI] [PubMed] [Google Scholar]
- 14.Livermore DM, Yuan M. Antibiotic resistance and production of extended-spectrum β-lactamases amongst Klebsiella spp from intensive care units in Europe. J Antimicrob Chemother. 1996;38:409–24. doi: 10.1093/jac/38.3.409. [DOI] [PubMed] [Google Scholar]
- 15.Munday CJ, Whitehead GM, Todd NJ, Campbell M, Hawkey PM. Predominance and genetic diversity of community- and hospital-acquired CTX-M extended-spectrum β-lactamases in York, UK. J Antimicrob Chemother. 2004;54:628–33. doi: 10.1093/jac/dkh397. [DOI] [PubMed] [Google Scholar]
- 16.Valverde A, Coque TM, Sánchez-Moreno MP, Rollán A, Baquero F, Cantón R. Dramatic increase in prevalence of fecal carriage of extended-spectrum β-lactamase-producing Enterobacteriaceae during nonoutbreak situations in Spain. J Clin Microbiol. 2004;42:4769–75. doi: 10.1128/JCM.42.10.4769-4775.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baby Padmini S, Appala Raju B, Mani KR. Detection of Enterobacteriaceae producing CTX-M extended-spectrum beta-lactamases from a tertiary care hospital in South India. Indian J Microbiol. 2008;26:163–6. doi: 10.4103/0255-0857.40534. [DOI] [PubMed] [Google Scholar]
- 18.Lewis JS, 2nd, Herrera M, Wickes B, Patterson JE, Jorgensen JH. First report of the emergence of CTX-M-type extended-spectrum ß-lactamases as the predominant ESBL isolated in a U.S. health care system. Antimicrob Agents Chemother. 2007;51:4015–21. doi: 10.1128/AAC.00576-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Muzaheed, Doi Y, Adams-Haduch JM, Shivannavar CT, Paterson DL, Gaddad SM. Faecal carriage of CTX-M-15-producing Klebsiella pneumoniae in patients with acute gastroenteritis. Indian J Med Res. 2009;129:599–602. [PubMed] [Google Scholar]
- 20.Bonnet R. Growing Group of Extended-Spectrum ß-Lactamases: the CTX-M Enzymes. Antimicrob Agents Chemother. 2004;48:1–14. doi: 10.1128/AAC.48.1.1-14.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Verma A, Desai N, Shannon K, Philpott-Howard J, Hill RL. Intra- and inter-generic plasmid-mediated spread of cephalosporin and aminoglycoside resistance amongst Klebsiella aerogenes K41 and other enterobacteria. Int J Antimicrob Agents. 2001;17:123–9. doi: 10.1016/s0924-8579(00)00324-1. [DOI] [PubMed] [Google Scholar]


