Abstract
Background:
The growing increase in the rates of antibiotic resistance is a major cause for concern in both non-fermenting bacilli and isolates of the Enterobacteriaceae family. β-lactams have been the mainstay of treatment for serious infections, and the most active of these are the carbapenems. Acquired metallo-β-lactamases (MBL) have recently emerged as one of the most worrisome resistance mechanisms owing to their capacity to hydrolyze all β-lactams, including carbapenems. We have undertaken this investigation to ascertain the prevalence of MBL-producing non-fermenting bacilli and Enterobacteriaceae.
Materials and Methods:
The study was conducted over a period of 4 months in a 1200-bedded teaching hospital. Isolates included in the study were screened for imipenem resistance both by conventional methods and mini analytical profile index (miniAPI). The isolates that showed imipenem resistance were tested for MBL production by imipenem (IMP)-ethylenediaminetetraacetic acid combined disc test. Imipenem-resistant non-MBL isolates also tested for Modified Hodge test and AmpC β-lactamases production to detect other mechanisms of carbapenem resistance.
Results:
Of 638 gram negative bacilli isolates and 3.39% showed imipenem resistance, 2.9% showed MBL production, of which 1.7% were non-fermenters and 1.25% were Enterobacteriaceae, 0.3% showing non-MBL KPC carbapenemas. Most isolates were from the intensive care unit and from post-operative patients. Our findings show that there are significant numbers of isolates having MBL production along with multidrug resistance. There is a need for active surveillance to detect MBL producers.
Keywords: Enterobacteriaceae, imipenem, metallo-β-lactamases, non-fermenting bacilli
INTRODUCTION
The increase in the rates of antibiotic resistance is a major cause for concern in both non-fermenting bacilli and isolates of the Enterobacteriaceae family. β-lactams have been the mainstay of treatment for serious infections. Most active of these are the carbapenems, which are advocated for use for the treatment of infections caused by extended-spectrum-β-lactamase (ESBL)-producing Enterobacteriaceae, particularly Escherichia coli and Klebsiella pneumonia,[1] and non-fermenters, particularly Pseudomonas spp. and Acinetobacter spp.
Acquired metallo-β-lactamases (MBL) have recently emerged as one of the most worrisome resistance mechanisms owing to their capacity to hydrolyze all β-lactams, including carbapenems. Such strains are not susceptible to therapeutic serine β-lacatamase inhibitors (such as clavulanate and sulfones). Moreover, their genes are carried on highly mobile elements, allowing easy dissemination.[2] Invasive infections with MBL-producing isolates are also associated with a higher morbidity and mortality.[3] The occurrence of an MBL-positive isolate in a hospital environment poses not only a therapeutic problem but is also a serious concern for infection control management. As a result of being difficult to detect, such organisms pose significant risks, particularly due to their role in unnoticed spread within institutions and their ability to participate in horizontal MBL gene transfer with other pathogens in the hospital. In recent years, MBL genes have spread from P. aeruginosa to members of the Enterobacteriaceae.[4,5]
Five different types of MBLs whose prevalence are increasing rapidly are IMP, VIM, SPM, GIM and SIM.[6] Among these, IMP and VIM are the most predominant.[7] With the global increase in the occurrence and types of MBLs, early detection is crucial, the benefits of which include timely implementation of strict infection control practices and treatment with alternative antimicrobials.[5] Molecular techniques are available to detect MBL producers. But, these are not available at smaller centers. Among the simple and cheaper methods available for testing MBL production, the imipenem (IMP)-EDTA combined disc test is sensitive and specific. According to Yong et al.,[8] the 0imipenem(IMP) 10 μg-EDTA 750 μg combined disc test has 95.7% sensitivity and 91.0% specificity for detection of metallo-betalactames in MBL-producing Pseudomonas spp and Acinetobacter spp.
Galan et al.[9] have reported the utility of the same combination for Enterobacteriaceae, with 80% sensitivity and 100% specificity for the detection of MBL.
Our institute, a tertiary care center in India, has a very high prevalence of nosocomial infections due to non-fermenting bacilli and Enterobacteriaceae. We have also found a very high prevalence of multidrug-resistant (MDR) and ESBL-positive gram negative bacteria in intensive care units (ICUs) and other wards of our hospitals (Unpublished data). Carbapenems and cephalosporin/inhibitor combinations are being used as the “last resort” in these infections since the last few years. Therefore, we undertook this investigation to ascertain the prevalence of MBL-producing non-fermenting bacilli and Enterobacteriaceae in our hospital. Although a global increase in the prevalence of MBL-producing non-fermenting bacilli and Enterobacteriaceae has been reported,[3,10–15] limited data is available from our part of the world.
MATERIALS AND METHODS
The study was conducted over period of 4 months, from Jun 2009 to September 2009, in our hospital, which is a 1200-bedded teaching hospital with two ICUs, one trauma center and one neonatal intensive care unit (NICU).
Bacterial isolates
A total of 638 gram negative bacterial isolates from various clinical samples of admitted patients were included in the study. All isolates were non-duplicate. The isolates were identified by conventional methods[16] and the mini analytical profile index (miniAPI) machine. The ID32GN Automatic identification system for non-fermenting gram-negative rods and ID32E Automatic identification system for Enterobacteriaceae family were used (BioMerieux, 69280, Marey I’etoile, France).
Antimicrobial susceptibility
Antimicrobial susceptibility of all the isolates was performed by the disc diffusion method according to the CLSI guidelines.[17] The following antibiotics were tested for Enterobacteriaceae by the disk diffusion method: Ampicillin (10 ug), Cefazolin (30 μg), Cephalothin (30 μg), Gentamicin(10 μg), Cefotaxime (30 μg), Ceftriaxone (30 μg), Ceftazidime (30 μg), Ceftazidime/Clavulanic acid (30 μg/10 μg), Ciprofloxacin (5 μg) and Imipenem (10 μg).
Antibiotics tested for non-fermenters by the disk diffusion method were piperacillin (100 μg), piperacillin/tazobactam (100 μg/10 μg), ceftazidime (30 μg), cefepime (30 μg), cefoperazone (30 μg), ceftriaxone (30 μg), cefotaxime (30 μg), amikacin (30 μg), levofloxacin (5 μg), ciprofloxacin (5 μg) and imipenem (10 μg), Colistin (10 μg) from Hi-Media Laboratories Mumbai, BD Diagnostics Pvt. Ltd Gurgaon, India.
The minimum inhibitory concentration (MIC) of the isolates that show resistance to imipenem by the disk diffusion method was determined by using the mini API machine, Rapid ATB E4 Automated susceptibility testing for Enterobacteriaceae and ATB PSE5 Automated susceptibility for non-fermenters (BioMerieux, 69280). The isolates that showed imipenem MIC more than 2 μg/ml were tested for MBL screening.[18,19]
Metallo-β-lactamase screening
MBL production was detected in imipenem-resistant isolates by phenotypic tests. The Imipenem(IMP)-EDTA combined disc test was used.
The Imipenem(IMP)-EDTA combined disk test was performed as described by Yong et al.[8] Pseudomonas aeruginosa ATCC 27853 used as the control. Test organisms were inoculated on to plates of Mueller Hinton agar as recommended by the CLSI.[17] Two 10-μg imipenem disks (Hi-Media Laboratories, BD Diagnostics Pvt. Ltd.) were placed on the plate and appropriate amounts of 10 μL of EDTA solution was added to one of them to obtain the desired concentration (750 μg). The inhibition zones of the imipenem and Imipenem(IMP)-EDTA disks were compared after 16–18 h of incubation in air at 35°C. In the combined disc test, if the increase in inhibition zone with the imipenem and EDTA disc was ≥7 mm than the imipenem disc alone, it was considered as MBL positive.[8]
The isolates that are imipenem resistant and not showing MBL production were tested for Modified Hodge test[20] and AmpC β-lactamases production[21] to detect other mechanisms of carbapenem resistance.
RESULTS
Of the total 638 gram negative isolates, 21 (3.29%) showed imipenem resistance in a period of 4 months both by the disk diffusion method and by testing the MIC using mini API. Of these, 12 (1.88%) were non-fermenters and nine (1.41%) were Enterobacteriaceae. A total of 19 (2.97%) isolates showed MBL production by the imipenem(IMP)-EDTA combined disc test, 11 (1.7%) were non-fermenters and eight (1.25%) were Enterobacteriaceae.
Of the 19 MBL producers, seven (36.8%) were Pseudomonas aeruginosa, four (21%) Acinetobacter baumannii, six (31.6%) Klebsiella pneumoniae and two (10.5%) Proteus species.
Location-wise distribution shows that 11 (57.9%) isolates were from the ICU, six (31.6%) isolates were from the post-operative patient, two isolates of Klebsiella pneumonia were from the urine of patients who were catheterized for 10 days in the ICU and transferred to the ward. After 2 days, they developed urinary tract infection symptoms. This indicates that these isolates could be from the ICU.
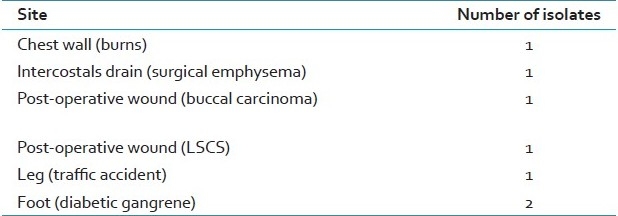
Of 19 isolates showing MBL production, seven (36.8%) were from the pus. The sites from where the pus was collected are shown in Table 1. Of the remaining 12, five (26.3%) isolates were from tracheal secretions, three (15.9%) from urine, two (10.6%) from blood and two (10.6%) from ascetic fluid.
Table 1.
Sites of pus collection having metallo-β-lactamases producers
Two isolates (0.3%), one Pseudomonas aeruginosa from the pus of infected post-operative wound and the other, Klebsiella pneumoniae from the urine, were imipenem resistant, but did not show MBL production. Both these isolate do not show AmpC β-lactames production, but Klebsiella pneumoniae indicated a positive reaction for Carbapenemas production by the Modified Hodge test and, therefore, these could be the KPC (Klebsiella pneumoniae Carbapenemas) strain.
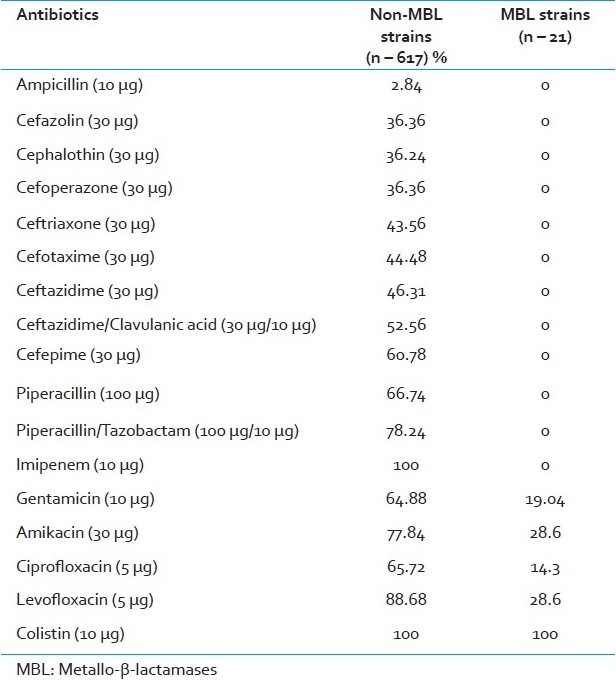
Of the 21 imipenem-resistant gram negative organisms, four (19.04%) isolates were sensitive to gentamicin, six (28.6%) to amikacin and levofloxacin and three (14.3%) to ciprofloxacin. All (100%) isolates were sensitive to colistin. All isolates were resistant to Ampicillin, Piperacillin, Piperacillin/Tazobactam, Cefazolin, Cephalothin, Cefoperazone, Cefotaxime, Ceftriaxone, Ceftazidime, Ceftazidime/Clavulanic acid and cefepime. The sensitivity pattern of MBL producers and non-producers to other antibiotics is shown in Table 2.
Table 2.
Sensitivity pattern of metallo-β-lactamases- and non-MBL-producing gram negative isolates to other antibiotics in vitro
DISCUSSION
In our study, the imipenem-resistant isolates also show resistance to other groups of antibiotics, which is a unique problem with MBLs that show a broad-spectrum resistance profile. The genes encoding MBLs are often procured by class 1 (sometimes class 3) integrons. Other gene cassettes within the integrons confer resistance to other antibiotics such as fluoroquinolones, aminoglycosides and co-trimoxazole. Integrons are, in turn, embedded in transposons, resulting in a highly transmissible genetic apparatus that can be transferred between bacteria.[3] Although our MBL producers showed resistance to many antibiotics, all MBL isolates were susceptible to Colistin.
The majority of these MBL isolates were from patients of the ICU and post-operative wards; areas where the majority of critically ill patients are concentrated. Use of indwelling medical devices is common in these areas, which can play an important role in the spread of infective agents. The majority of the organisms were from pus and tracheal secretion samples. Pseudomonas aeruginosa and Klebsiella pneumoniae were the predominant MBL producers.
We report that 2.9% were MBL-producing gram negative bacilli, of which 1.7% were non-fermenters and 1.25% Enterobacteriaceae. MBL production has been previously reported from India. Most studies have used the Imipenem(IMP)-EDTA combined disc, double disc synergy test using the Imipenem(IMP)-EDTA and modified Hodge tests. According to those studies, MBL production ranged from 7 to 65%.[22–26]
Most of these studies reported MBL production in non-fermenters like Pseudomonas aeruginosa and Acinetobacter baumannii. There are very few studies that report MBL production in Enterobacteriaceae.
The number of MBL producers in our institute is much less than that reported from other centers. But, the fact remains that even in a teaching hospital with fewer ICUs and critical care units, MBL producers have made their presence felt.
Of the 21 imipenem-resistant strains, two did not show MBL production. One of the strains was Klebsiella pneumoniae, which showed cabapenemas production, and, therefore, this could be the KPC strain. KPC carbapenemas is a Class A β-lactamases that is a very important mechanism of carbapenems resistance in Enterobacteriaceae.[27] The other strain was Pseudomonas aeruginosa, which was negative for both AmpC and cabapenemas production and, therefore, it may have had other mechanisms of carbepenem resistance, like drug efflux pumps, low degree of outer membrane permeability and loss of OprD.[28]
As our institute does not have a molecular set-up, we were not able to confirm these findings by the genotypic method, which is limitation in our study.
Also, in India, we do not have any referral center for the detection of antibiotic resistance mechanisms, which is eagerly needed.
Reports from various parts of the world showing emergence of MBL enzymes in gram negative bacilli is alarming, and reflects the excessive use of carbapenems. Therefore, early detection and prompt instillation of infection control measures is important to prevent further spread of MBLs to other gram negative rods. Additionally, it is also important to follow antibiotic restriction policies to avoid excessive use of carbapenems and other broad-spectrum antibiotics. Finally, to understand the epidemiology, there is a need for active surveillance to detect MBL producers.
CONCLUSION
Our findings show that there are significant numbers of isolates showing MBL production along with MDR. There is a need for active surveillance to detect MBL producers. The Imipenem(IMP)-EDTA combined disc test is a simple test that can be used in district health laboratories or where molecular diagnostic techniques are not available to detect these types of resistance. There should be judicious use of carbapenems to prevent their spread and use of effective antibiotics as per the antibiotic-sensitivity report. We could have at least some referral lab to confirm these findings.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Yong D, Toleman MA, Giske CG, Cho HS, Sundman K, Lee K, et al. Characterization of a new metallo-βlactamase gene, blaNDM-1, and a novel erythromycin esterase gene carried on a unique genetic structure in Klebsiella pneumoniae Sequence Type 14 from India. Antimicrob Agents Chemother. 2009;53:5046–54. doi: 10.1128/AAC.00774-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Behera B, Mathur P, Das A, Kapil A, Sharma V. An evaluation of four different phenotypic techniques for detection of metallo-â-lactamase producing Pseudomonas aeruginosa. Indian J Med Microbiol. 2008;26:233–7. doi: 10.4103/0255-0857.39587. [DOI] [PubMed] [Google Scholar]
- 3.Walsh TR, Toleman MA, Poirel L, Nordmann P. Metallo-ß-lactamases: the quiet before the storm? Clin Microbiol Rev. 2005;18:306–25. doi: 10.1128/CMR.18.2.306-325.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peleg AY, Franklin C, Bell JM, Spelmann DW. Dissemination of the metallo-β lactamase gene bla IMP4 among gram-negative pathogens in a clinical setting in Australia. Clin Infect Dis. 2005;41:1549–56. doi: 10.1086/497831. [DOI] [PubMed] [Google Scholar]
- 5.Nordmann P, Poirel L. Emerging carbapenemases in gram-negative aerobes. Clin Microbial Infect. 2002;8:321–31. doi: 10.1046/j.1469-0691.2002.00401.x. [DOI] [PubMed] [Google Scholar]
- 6.Luzzaro F, Endimiani A, Docquier JD, Mugnaioli C, Bonsignori M, Amicosante G, et al. Prevalence and characterization of metallo-beta-lactamases in clinical isolates of Pseudomonas aeruginosa. Diagn Microbiol Infect Dis. 2004;48:131–5. doi: 10.1016/j.diagmicrobio.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 7.Senda K, Arakawa Y, Nakashima K, Ito H, Ichiyama S, Shimokata K, et al. Multifocal outbreaks of metallo-beta-lactamase producing Pseudomonas aeruginosa resistant to broad-spectrum beta lactams, including carbapenems. Antimicrob Agents Chemother. 1996;40:349–53. doi: 10.1128/aac.40.2.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yong D, Lee K, Yum JH, Shin HB, Rossolini GM, Chong Y. Imipenem-EDTA disk method for differentiation of metallo-β-lactamases producing clinical isolates of Pseudomonas spp and Acinetobacter spp. J Clin Microbiol. 2002;40:3798–801. doi: 10.1128/JCM.40.10.3798-3801.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Galan I I, Rekatsina PD, Hatzaki D, Plachouras D, Souli M, Giamarellou H. Evaluation of different laboratory tests for the detection of metallo-b-lactamase production in Enterobacteriaceae. J Antimicrob Chemother. 2008;61:548–53. doi: 10.1093/jac/dkm535. [DOI] [PubMed] [Google Scholar]
- 10.Garza-Ramos U, Morfin-Otero R, Sader HS, Jones RN, Hernández E, Rodriguez-Noriega E, et al. Metallo-β lactamase gene blaIMP-15 in a class 1 integron, In95, from Pseudomonas aeruginosa clinical isolates from a hospital in Mexico. Antimicrob Agents Chemother. 2008;52:2943–6. doi: 10.1128/AAC.00679-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Toleman MA, Simm AM, Murphy TA, Gales AC, Biedenbach DJ, Jones RN, et al. Molecular characterization of SPM-1, a novel metallo-β-lactamaseisolated in Latin America: report from the SENTRY antimicrobial surveillance programme. J Antimicrob Chemother. 2002;50:673–9. doi: 10.1093/jac/dkf210. [DOI] [PubMed] [Google Scholar]
- 12.Giakkoupi P, Xanthaki A, Kanelopoulou M, Vlahaki A, Miriagou V, Kontou S, et al. VIM-1 metallo-_lactamase-producing Klebsiella pneumonia strains in Greek hospitals. J Clin Microbiol. 2003;41:3893–6. doi: 10.1128/JCM.41.8.3893-3896.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dong F, Xu XW, Song WQ, Lü P, Yu SJ, Yang YH, et al. Characterization of multidrug-resistant and metallo-betalactamase- producing Pseudomonas aeruginosa isolates from a paediatric clinic in China. Chinese Med J (Engl) 2008;121:1611–6. [PubMed] [Google Scholar]
- 14.Yan JJ, Ko WC, Chuang CL, Wu JJ. Metall-βlactamase-producing Enterobacteriaceae isolates in a university hospital in Taiwan: prevalence of IMP-8 in Enterobacter cloacae and first identification of VIM-2 in Citrobacter freundii. J Antimicrob Chemother. 2002;50:503–11. doi: 10.1093/jac/dkf170. [DOI] [PubMed] [Google Scholar]
- 15.Fiett J, Baraniak A, Mrówka A, Fleischer M, Drulis-Kawa Z, Naumiuk Ł, et al. Molecular epidemiology of acquired-metallo-_lactamase-producing bacteria in Poland. Antimicrob Agents Chemother. 2006;50:880–6. doi: 10.1128/AAC.50.3.880-886.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Collee JG, Diguid JP, Fraser AG. 14th ed. Edinburgh: Churchill Livingstone; 1996. Mackie and McCartney practical Medical Microbiology. [Google Scholar]
- 17.Wayne PA: CLSI Document M2-A9; 2006. Clinical and Laboratory standards institute (CLSI). Performance standards for antimicrobial susceptibility testing, 16th informational supplements. [Google Scholar]
- 18.Clinical and Laboratory standards institute (CLSI). Performance standards for antimicrobial susceptibility testing CLSI document M100-S18: Interpretation Standards for Enterobacteriaceae Table 2A, Interpretation Standards for Pseudomonas aeruginosa Table 2B1. 2008;28(No.1):32–39. [Google Scholar]
- 19.Qu TT, Zhang JL, Wang J, Tao J, Yu YS, Chen YG, et al. valuation of phenotypic tests for detection of metallo-_lactamase-Producing Pseudomonas aeruginosa Strains in China. J Clin Microbiol. 2009;47:1136–42. doi: 10.1128/JCM.01592-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee K, Chong Y, Shin HB, Kim YA, Yong D, Yum JH. Modified Hodge and EDTA-disk synergy tests to screen metallo-_-lactamase-producing strains of Pseudomonas and Acinetobacter species. Clin Microbiol Infect. 2001;7:88–91. doi: 10.1046/j.1469-0691.2001.00204.x. [DOI] [PubMed] [Google Scholar]
- 21.George AJ. AmpC β lactamases clinical microbiology reviews. Am Soc Microbiol. 2009;22:161–82. doi: 10.1128/CMR.00036-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Navneeth BV, Sridaran D, Sahay D, Belwadi M. A preliminary study of metallo-β-lactamase producing Pseudomonas aeruginosa in hospitalized patients. Indian J Med Res. 2002;116:264–8. [PubMed] [Google Scholar]
- 23.Gupta V, Datta P, Chander J. Prevalence of metallo-β-lactamase (MBL) producing Pseudomonas spp and Acinetobacter spp in a tertiary care hospital in India. J Infect. 2006;52:311–4. doi: 10.1016/j.jinf.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 24.Jesudason MV, Kandathil AJ, Balaji V. Comparison of two methods to detect carbapenemase and metallo-β-lactamase production in clinical isolates. Indian J Med Res. 2005;121:780–3. [PubMed] [Google Scholar]
- 25.Agarwal VA, Dongre SA, Powar RM. Antimicrobial resistance profile of metallo-β-lactamase Pseudomonas aeruginosa producing metallo-β-lactamases. Indian J Med Res. 2006;124:588–90. [PubMed] [Google Scholar]
- 26.Chakraborty D, Basu S, Das S. A study on infections caused by metallo beta lactamase producing gram negative bacteria in intensive care unit patients. Am J Infect Dis. 2010;6:34–9. [Google Scholar]
- 27.Livermore DM, Woodford N. The β-lactamase threat in Enterobacteriaceae, Pseudomonas and Acinetobacter. Trends Microbiol. 2006;14:413–20. doi: 10.1016/j.tim.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 28.Pai H, Kim J, Kim J, Lee JH, Choe KW, Gotoh N. Carbapenem resistance mechanisms in Pseudomonasaeruginosa clinical isolates. Antimicrob Agents Chemother. 2001;45:480–4. doi: 10.1128/AAC.45.2.480-484.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]


