Abstract
Objective
To determine the distribution of influenza vaccine coverage in the U.S. in 2008.
Design, Setting, and Participants
Cross-sectional analysis of the 2008 Behavioral Risk Factor Surveillance Survey (BRFSS). The BRFSS employs random-digit dialing to interview non-institutionalized adults in the U.S. and the territories. The sample was restricted to persons ≥50 years (N=249,723).
Measurements
Participants were asked if they had a flu shot during the past 12 months.
Results
In 2008, 42.0% of adults age 50–64 years and 69.5% of adults ≥65 years reported receiving a flu shot in the past 12 months. Vaccine coverage generally increased with advancing age (p<0.001), higher levels of education (p<0.001) and total household income (p<0.001), and greater morbidity (p<0.001). In 50–64 year olds, vaccine prevalence was lower in men than in women (39.9% vs 44.1%; p<0.001), although no significant differences were observed in older adults. Within each 5-year interval of age, non-Hispanic blacks and Hispanics had significantly lower vaccine prevalence than non-Hispanic whites (p<0.001 for all comparisons). Among participants ≥65 years, non-Hispanic blacks and Hispanics were 56% [adjusted prevalence ratio (PR): 1.56 (95% CI: 1.48, 1.64)] and 44% [adjusted PR: 1.44 (95% CI: 1.35, 1.54)], respectively, more likely to be unvaccinated compared with non-Hispanic whites, adjusting for age and sex. Racial/ethnic disparities in vaccine coverage narrowed with increasing number of diseases; however, these disparities remained significant in older adults with ≥2 diseases (p<0.05).
Conclusions
There were large disparities in influenza vaccine coverage in 2008, particularly across race/ethnicity and socioeconomic position. Accordingly, more targeted interventions are needed to improve vaccine delivery to disadvantaged segments of the U.S. population.
Keywords: Influenza, influenza vaccines, aged, health disparities, public health
INTRODUCTION
The influenza virus is a significant cause of morbidity and mortality in temperate climates globally.1,2 In the United States, influenza is responsible for approximately 36,000 deaths annually and 90% of these fatalities occur in the elderly.3 Inoculation with trivalent inactivated virus has been shown to reduce hospitalizations and all-cause mortality2 as well as deaths attributed specifically to pneumonia and influenza.1 However, recent challenges to the methodological integrity of vaccine effectiveness studies have provoked a wave of questions regarding the magnitude of benefit in the older population.4 Indeed, even accurately quantifying the influenza death toll poses a unique challenge to epidemiologists, since influenza and influenza-like illnesses are clinically indistinguishable.5
Amidst the vaccine effectiveness controversy, immunization remains the primary clinical technique for reducing the immense health and economic costs of influenza.6 Current policy recommendations direct all adults ≥50 years and persons over 18 with chronic underlying medical conditions to seek vaccination,7 as these subpopulations suffer disproportionately in terms of mortality outcomes. In addition to these high-risk groups, the Advisory Committee on Immunization Practices (ACIP) recommends that health personnel, domestic contacts with high-risk persons and women pregnant during the flu season obtain the vaccine.5
The U.S. witnessed a substantial increase in vaccine coverage among persons aged ≥65 years from 1989–2004,8 but the trend masks differential rates of uptake across subpopulations. Racial/ethnic minorities habitually receive the vaccine at lower rates than whites,7 a phenomenon that poses profound consequences, both immediate and long-term, as the nation evolves an increasingly heterogeneous demographic profile.9
Many studies acknowledge that the U.S. has yet to achieve Healthy People 2010 objectives for overall vaccination rates among the elderly (90%) and chronically ill (60%), but the role of numerous social factors, including race/ethnicity and socioeconomic status, as well as cardiovascular, metabolic and pulmonary health conditions in predicting vaccination prevalence needs to be characterized further. In light of the threat of pandemic influenza, it is critical to understand factors that affect vaccine utilization rates. We analyzed contemporary data from a nationally representative survey of the U.S. to quantify vaccine coverage by age, sex, geographic area, race/ethnicity, and social class.
METHODS
Study Population
The Behavioral Risk Factor Surveillance Survey (BRFSS) is conducted annually by state health departments in conjunction with the Centers for Disease Control and Prevention using telephone random digit dialing to obtain a representative cross-sectional sample. The survey collects information on a wide variety of health topics in all 50 states, the District of Columbia, and the organized territories. Data from the 2008 BRFSS were analyzed. Across states, the median response rate to the 2008 survey was 53.3%, but this is a conservative estimate as the sampling frame includes unresolved cases (no contact after 15 calls), many of which would be ineligible.10 The sample was limited to individuals ≥50 years (N=249,723), as we were primarily interested in vaccine uptake within the adult population targeted for immunization on the basis of ACIP age recommendations.5
Measures
Prevalence of flu vaccination was based on the following question: “During the past 12 months, have you had a flu shot?” For race/ethnicity, participants were allowed to report multiple race categories. Six racial/ethnic categories were created based on Hispanic/non-Hispanic origin and identification as white, black, Asian-American, Native American, or other (including multiracial persons). Additionally, participants reported their highest level of education and total household income from all sources.
The 50 states and the District of Columbia were aggregated into 9 geographic divisions according to the standard U.S. Census Bureau classification: New England–CT, ME, MA, NH, RI, VT; Middle Atlantic–NJ, NY, PA; East North Central–WI, MI, OH, IN, IL; West North Central–ND, SD, NE, KS, MO, IA, MN; South Atlantic–DC, DE, MD, WV, VA, NC, SC, GA, FL; East South Central–KY, TN, MS, AL; West South Central–OK, AR, LA, TX; Mountain–MT, ID, WY, NV, UT, CO, NM, AZ; and Pacific–CA, OR, WA, HI, AK. The organized territories (Guam, Puerto Rico and the Virgin Islands) were designated as a tenth division.
Participant self-report was used to identify persons with chronic cardiovascular, metabolic and pulmonary conditions known to increase susceptibility to influenza complications. Respondents were asked if they had ever been diagnosed with asthma, diabetes mellitus, myocardial infarction, angina/coronary heart disease (CHD) or stroke. Those who had been told they had asthma in the past but were not asthmatic at the time of the interview were grouped with persons who had never received an asthma diagnosis. A new variable was generated for CHD to identify individuals who reported either angina/CHD or myocardial infarction.
Statistical Analysis
All analyses were performed separately for persons 50–64 (n=129,769) and those 65 and older (n=119,954). Prevalence of vaccination was determined overall and for various subgroups shown in Table 1 and Figure 2. Poisson regression was used to model the probability of not receiving the flu shot.11 Multivariable adjusted prevalence ratios from those models are shown in Table 2. Data analysis was performed using Stata/SE 10.0. All analyses were weighted and accounted for the complex sampling design of the BRFSS, including bias resulting from non-response and non-coverage.
Table 1.
Participant characteristics and vaccination prevalence in demographic, geographic and disease subgroups.
| 50–64 years (n=129,769) | ≥ 65 years (n= 119,954) | |||
|---|---|---|---|---|
| No. (%) | Percent Vaccinated (95% CI) | No. (%) | Percent Vaccinated (95% CI) | |
| Sex | ||||
| Men | 50,667 (49.0) | 39.9 (39.1, 40.7) | 41,862 (42.2) | 69.9 (69.1, 70.7) |
| Women | 79,102 (51.0) | 44.1 (43.4, 44.7) | 78,092 (57.8) | 69.3 (68.7, 69.9) |
| Race/Ethnicity | ||||
| Non-Hispanic white | 106,215 (74.0) | 44.2 (43.7, 44.7) | 102,988 (79.8) | 72.1 (71.7, 72.6) |
| Non-Hispanic black | 10,295 (9.7) | 36.2 (34.3, 38.0) | 7,166 (7.7) | 55.5 (53.3, 57.7) |
| Hispanic | 6,848 (10.3) | 32.2 (30.0, 34.4) | 5,204 (7.8) | 58.7 (56.0, 61.4) |
| Asian American | 1,625 (2.5) | 41.4 (36.5, 46.5) | 1,257 (1.8) | 74.2 (68.5, 79.3) |
| Native American | 1,748 (1.1) | 44.8 (39.8, 49.8) | 1,047 (0.9) | 61.8 (55.4, 67.8) |
| Other | 3,038 (2.4) | 39.1 (35.5, 42.7) | 2,292 (2.1) | 62.5 (58.0, 66.7) |
| Education | ||||
| Less than high school graduate | 9,583 (8.9) | 33.7 (31.8, 35.7) | 17,552 (15.1) | 62.2 (60.7, 63.6) |
| High school graduate | 37,106 (27.4) | 37.9 (37.0, 38.8) | 43,123 (34.1) | 68.5 (67.7, 69.3) |
| Attended college or technical school | 35,770 (26.8) | 41.3 (40.4, 42.3) | 28,676 (23.4) | 71.6 (70.7, 72.5) |
| College or technical school graduate | 47,173 (37.0) | 47.5 (46.7, 48.3) | 30,300 (27.3) | 73.3 (72.4, 74.2) |
| Total Household Income | ||||
| <$10,000 | 6,148 (4.6) | 37.3 (34.7, 39.9) | 6,103 (6.0) | 56.6 (53.7, 59.4) |
| $10,000–14,999 | 5,560 (4.2) | 37.0 (34.4, 39.8) | 9,636 (8.3) | 65.0 (63.2, 66.7) |
| $15,000–19,999 | 6,775 (5.5) | 36.4 (34.0, 38.9) | 11,689 (11.0) | 65.9 (64.2, 67.6) |
| $20,000–24,999 | 8,991 (6.8) | 37.0 (35.0, 39.0) | 14,163 (13.4) | 67.6 (66.1, 69.0) |
| $25,000–34,999 | 12,580 (9.6) | 38.2 (36.5,39.9) | 16,494 (16.5) | 72.1 (70.9, 73.4) |
| $35,000–49,999 | 18,471 (14.4) | 40.6 (39.2, 42.0) | 15,577 (16.3) | 72.4 (71.2, 73.6) |
| $50,000–74,999 | 22,196 (18.5) | 42.4 (41.2, 43.5) | 11,329 (13.1) | 72.4 (71.0, 73.8) |
| ≥$75,000 | 36,424 (36.5) | 46.2 (45.3, 47.1) | 12,067 (15.4) | 73.4 (72.0, 74.7) |
| Geographic Division | ||||
| New England | 16,240 (4.9) | 46.8 (45.7, 47.9) | 14,427 (5.0) | 73.8 (72.7, 74.8) |
| Middle Atlantic | 9,938 (13.7) | 42.8 (41.3, 44.3) | 9,516 (14.5) | 70.3 (68.9, 71.7) |
| East North Central | 12,537 (15.4) | 41.1 (39.9, 42.3) | 11,589 (15.4) | 68.6 (67.4, 69.7) |
| West North Central | 16,206 (6.7) | 47.7 (46.3, 49.0) | 16,261 (7.0) | 74.1 (73.0, 75.3) |
| South Atlantic | 21,824 (19.4) | 40.8 (39.6, 42.0) | 20,700 (20.2) | 67.6 (66.4, 68.8) |
| East South Central | 9,002 (6.1) | 42.1(40.6, 43.5) | 8,285 (6.1) | 70.4 (69.1, 71.8) |
| West South Central | 9,161 (10.6) | 43.6 (41.8, 45.3) | 9,252 (10.1) | 71.0 (69.4, 72.4) |
| Mountain | 16,977 (6.6) | 41.8 (40.2, 43.3) | 14,859 (6.4) | 70.6 (69.2, 71.9) |
| Pacific | 15,560 (15.3) | 40.8 (39.2, 42.4) | 13,058 (14.2) | 70.4 (68.8, 71.9) |
| Unincorporated Organized Territories | 2,324 (1.3) | 16.0 (14.0, 18.3) | 2,007 (1.3) | 31.5 (29.0, 34.0) |
| Diseases | ||||
| Asthma | 12,393 (8.8) | 55.1 (53.5, 56.8) | 9,817 (8.0) | 77.2 (75.6, 78.6) |
| Coronary heart disease | 10,916 (8.5) | 54.6 (52.8, 56.4) | 23,081 (20.4) | 75.7 (74.7, 76.7) |
| Diabetes | 17,046 (13.7) | 56.5 (55.0, 58.0) | 22,459 (19.8) | 75.0 (73.9, 76.0) |
| Stroke | 4,405 (3.2) | 51.1 (48.3, 53.9) | 9,864 (8.4) | 73.3 (71.7, 74.8) |
| Number of Diseases | ||||
| 0 | 94,814 (73.2) | 37.8 (37.3, 38.4) | 71,600 (58.4) | 65.8 (65.2, 66.4) |
| 1 | 26,957 (20.7) | 51.1 (50.0, 52.3) | 34,325 (29.3) | 73.9 (73.0, 74.7) |
| ≥ 2 | 7,998 (6.0) | 61.1 (59.0, 63.1) | 14,029 (12.3) | 77.0 (75.7, 78.2) |
Table 2.
Multivariate adjusted prevalence ratios for not reporting influenza vaccination.
| 50–64 years (n=129,769) | ≥ 65 years (n= 119,954) | |||
|---|---|---|---|---|
| Model 1 PR (95% CI) |
Model 2 PR (95% CI) |
Model 1 PR (95% CI) |
Model 2 PR (95% CI) |
|
| Age group | ||||
| 50–54 | 1.32 (1.29, 1.35) | 1.29 (1.26, 1.32) | -- | -- |
| 55–59 | 1.17 (1.14, 1.19) | 1.16 (1.13, 1.19) | -- | -- |
| 60–64 | 1.00 | 1.00 | -- | -- |
| 65–69 | -- | -- | 1.58 (1.50, 1.66) | 1.68 (1.59, 1.79) |
| 70–74 | -- | -- | 1.28 (1.21, 1.36) | 1.37 (1.29, 1.46) |
| 75–80 | -- | -- | 1.10 (1.04, 1.16) | 1.15 (1.08, 1.23) |
| 80–84 | -- | -- | 1.00 | 1.00 |
| 85+ | -- | -- | 1.10 (1.02, 1.18) | 1.09 (1.00, 1.19) |
| Sex | ||||
| Men | 1.07 (1.06, 1.09) | 1.10 (1.08, 1.12) | 0.96 (0.93, 0.99) | 1.06 (1.02, 1.09) |
| Women | 1.00 | 1.00 | 1.00 | 1.00 |
| Race/Ethnicity | ||||
| Non-Hispanic white | 1.00 | 1.00 | 1.00 | 1.00 |
| Non-Hispanic black | 1.14 (1.11, 1.18) | 1.12 (1.08, 1.16) | 1.56 (1.48, 1.64) | 1.44 (1.36, 1.53) |
| Hispanic | 1.20 (1.16, 1.24) | 1.06 (1.02, 1.11) | 1.44 (1.35, 1.54) | 1.11 (1.01, 1.22) |
| Asian-American | 1.04 (0.95, 1.13) | 1.02 (0.94, 1.12) | 0.91 (0.74, 1.11) | 0.78 (0.63, 0.97) |
| Native American | 0.99 (0.90, 1.08) | 1.00 (0.91, 1.10) | 1.34 (1.13, 1.58) | 1.31 (1.10, 1.57) |
| Other | 1.09 (1.03, 1.16) | 1.09 (1.02, 1.16) | 1.33 (1.19, 1.49) | 1.27 (1.13, 1.43) |
| Education | ||||
| Less than high school graduate | 1.18 (1.13, 1.22) | 1.16 (1.09, 1.24) | ||
| High school graduate | 1.15 (1.12, 1.17) | 1.09 (1.04, 1.15) | ||
| Attended college or technical school | 1.10 (1.08, 1.13) | 1.04 (0.98, 1.09) | ||
| College or technical school graduate | 1.00 | 1.00 | ||
| Total Household Income | ||||
| <$10,000 | 1.16 (1.10, 1.21) | 1.55 (1.41, 1.71) | ||
| $10,000–14,999 | 1.18 (1.13, 1.24) | 1.38 (1.28, 1.50) | ||
| $15,000–19,999 | 1.17 (1.12, 1.22) | 1.35 (1.25, 1.46) | ||
| $20,000–24,999 | 1.16 (1.12, 1.20) | 1.30 (1.20, 1.39) | ||
| $25,000–34,999 | 1.13 (1.09, 1.17) | 1.11 (1.04, 1.19) | ||
| $35,000–49,999 | 1.09 (1.06, 1.12) | 1.09 (1.01, 1.16) | ||
| $50,000–74,999 | 1.06 (1.04, 1.09) | 1.06 (0.99, 1.14) | ||
| ≥$75,000 | 1.00 | 1.00 | ||
| Geographic Division | ||||
| New England | 1.00 | 1.00 | ||
| Middle Atlantic | 1.05 (1.01, 1.08) | 1.07 (1.01, 1.14) | ||
| East North Central | 1.08 (1.05, 1.11) | 1.15 (1.08, 1.22) | ||
| West North Central | 0.97 (0.94, 1.00) | 0.97 (0.91, 1.03) | ||
| South Atlantic | 1.08 (1.05, 1.12) | 1.15 (1.09, 1.22) | ||
| East South Central | 1.04 (1.01, 1.08) | 1.02 (0.96, 1.09) | ||
| West South Central | 1.01 (0.97, 1.05) | 1.01 (0.94, 1.08) | ||
| Mountain | 1.08 (1.04, 1.11) | 1.08 (1.01, 1.15) | ||
| Pacific | 1.08 (1.05, 1.12) | 1.10 (1.03, 1.18) | ||
| Unincorporated Organized Territories | 1.40 (1.30, 1.47) | 1.90 (1.71, 2.12) | ||
| Number of Diseases | ||||
| 0 | 1.70 (1.60, 1.79) | 1.64 (1.54, 1.74) | ||
| 1 | 1.30 (1.23, 1.38) | 1.22 (1.13, 1.30) | ||
| ≥2 | 1.00 | 1.00 | ||
Model 1 includes age, sex and race/ethnicity.
Model 2 includes age, sex, race/ethnicity, education, total household income, geographic area and number of diseases.
PR = Prevalence ratio; CI = Confidence interval
RESULTS
The overall prevalence of influenza vaccination in 2008 was 53.3% among adults 50 years and older. There were large age-related differences in vaccine coverage. Persons 65 and older achieved a vaccine prevalence of 69.5% in 2008, while less than half (42.0%) of 50–64 year olds were vaccinated. Table 1 shows that in the younger group, immunization was lower among men (39.9%) than in women (44.1%), but there were no sex differences in vaccine coverage among older adults.
Marked racial/ethnic differences in vaccination were evident. Asian Americans, Native Americans, and Non-Hispanic whites had the highest vaccine coverage among 50–64 year olds; whereas in those 65 and older, vaccine prevalence was higher in Asian-Americans and non-Hispanic whites than in the other groups. Non-Hispanic blacks and Hispanics had particularly low coverage in both age groups. Lower vaccine coverage was also observed in older Native-Americans. The supplemental figure that is available online illustrates the persistence of racial/ethnic disparities across age groups. In fact, disparities between non-Hispanic whites and blacks grew from age 50 to age 80 and remained large thereafter (Figure online). Although age is associated with increased vaccine uptake, rates declined after age 85 among non-Hispanic whites and, more severely, Hispanics. This steep decrease in Hispanic immunization translates to an absolute disparity of more than 20% between non-Hispanic whites and Hispanics age 85 and older (Figure online).
Vaccination in both age groups followed a clear social gradient (Table 1). Each stepwise increase in education level or total household income corresponded to an incremental rise in flu shot prevalence. Some geographic variation in vaccine uptake was observed but coverage among 50–64 year olds never exceeded 50% in any of the geographic areas. Excluding the territories, the lowest vaccination rates were reported by the South Atlantic and Pacific states in 50–64 year olds and by the South Atlantic states in persons 65 and older. Vaccine prevalence was very low in the territories, where only 31.5% of seniors and 16.0% of 50–64 year olds were immunized (Table 1).
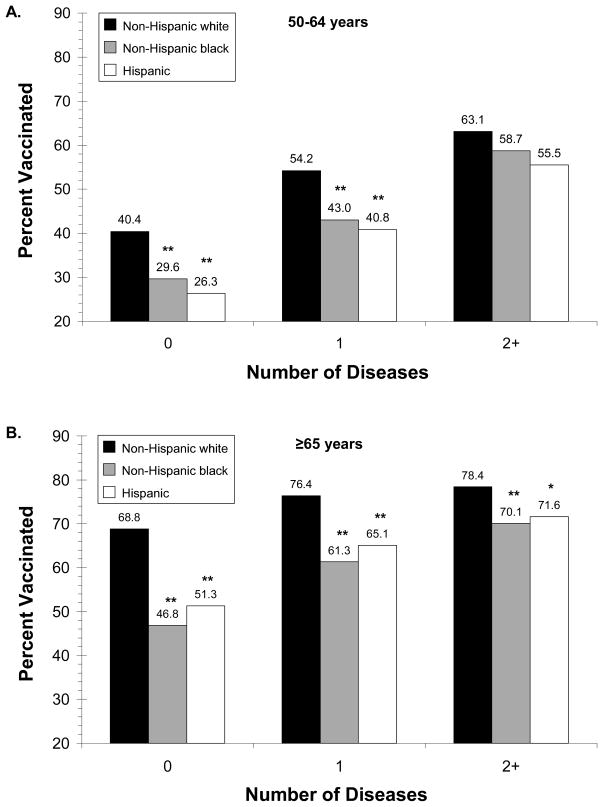
Table 1 also shows that prevalence of vaccination was higher in adults with asthma, CHD, diabetes or stroke than compared with the general population. Additionally, there was a gradient in vaccine coverage related to the number of reported conditions. Adults with 2 or more conditions were immunized at higher rates than persons with 0 or 1 disease (Table 1). This pattern was observed in all 3 racial/ethnic groups shown in Figure 1, although disparities between groups persisted in those with and without disease. Importantly, disparities were largest in those without disease. For instance, the absolute disparity in vaccination between non-Hispanic whites and blacks age ≥65 was wider in seniors without a disease (22%) than in seniors with 2 or more diseases (8.3%) (Figure 1b).
Figure 1. Vaccine coverage by race/ethnicity and number of diseases in adults ages 50–64 years (A) and ≥65 years (B).
Note: Diseases included asthma, coronary heart disease, diabetes, and stroke
* p<0.05 for comparison with non-Hispanic whites
** p<0.001 for comparison with non-Hispanic whites
After adjusting for age and sex, the probability of being unvaccinated in persons age ≥65 was 56% greater for non-Hispanic blacks and 44% greater for Hispanics than for non-Hispanic whites (Model 1, Table 2). Further adjustments for socioeconomic position, geographic area and number of diseases in Model 2 reduced the Hispanic to non-Hispanic white prevalence ratios considerably but did not substantially attenuate the non-Hispanic black-white disparity. Notably, in Model 2, the socioeconomic gradient in vaccination persisted and adults without a known disease were 60 to 70% (ages ≥50 years) more likely (p<0.001) not to be vaccinated than their peers with 2 or more diseases.
DISCUSSION
In this national survey of the United States in 2008, there was significant variation in influenza vaccination according to age, race/ethnicity, and socioeconomic position. Vaccination coverage was substantially below the Federal government’s Healthy People 2010 targets in subpopulations recommended to receive vaccination. Despite the ACIP revising its flu vaccine guidelines in 2004 to include adults ages 50 and older, most adults ages 50–64 years in 2008 reported that they had not been vaccinated in the past 12 months. Additionally, there was a clear social gradient in vaccine coverage. With the exception of Asian Americans, all other racial/ethnic minorities were significantly less likely to be vaccinated relative to non-Hispanic whites. Racial/ethnic disparities were even apparent among those with diseases known to increase risk for influenza-related complications and mortality. Persons with lower levels of education and total household income were also less likely to be vaccinated than more socioeconomically advantaged persons. In view of the H1N1 influenza pandemic as well as other potentially emerging vaccine-preventable communicable diseases, it is imperative that we identify and overcome barriers to vaccine delivery in major segments of the U.S. population.
Vaccine prevalence increased with advancing age, suggesting that older individuals were engaged in the healthcare system and better equipped with the information, resources and motivation to be vaccinated. A positive association between disease number and quality of care resulting primarily from greater use of health care services.12 Multimorbidity may constitute a driving force in the greater vaccine coverage observed with advancing age. Beyond improving overall vaccine coverage, having multiple chronic diseases was associated with reduced disparities between racial/ethnic groups. Previous studies involving patients with type 2 diabetes13 or cardiovascular disease14 detected no racial/ethnic differences in the frequency of annual physician visits. To some extent, these earlier findings may explain the narrowing of racial/ethnic disparities visible in Figures 1a–b; however, these figures also highlight the challenge of vaccinating racial/ethnic minorities not engaged in the health care system.13, 14 In addition, gender differences in vaccination prevalence among 50–64 year olds (Table 1) may reflect lower health care utilization in men compared with women.
One age subgroup departed from the pattern of age-dependence in vaccine coverage. The oldest respondents (ages 85 and older) reported lower rates of vaccine uptake than 80–84 year olds (see the supplemental figure online). The decline after age 85 was particularly striking among Hispanics, and possibly reflects lower levels of acculturation. Indeed, one component of acculturation –the patient’s spoken/written language– is related to the Hispanic experience of health care in the United States.15 Persons who prefer to speak Spanish and those with low English proficiency make fewer doctor visits,16 possess lower health care comprehension,17 and use fewer physician services.16,18 It is possible that Hispanics over age 85 in our study encountered greater linguistic barriers in the clinical environment, compared with younger Hispanics, and consequently did not receive sufficient information about the vaccine. To overcome this barrier, greater use of medical interpreters may be warranted. One study showed that Spanish speakers equipped with medical interpreters were more likely than English proficient adults to utilize primary care.19 In addition, the relatively low prevalence of vaccination among Hispanics at all ages (see online Figure) might reflect, in part, a fatalistic view that illnesses cannot be controlled or prevented, which has been suggested to play a role in lower utilization of preventive services in several minority populations, including Hispanics. Accordingly, culturally specific education campaigns for targeted minority populations as well as cross-cultural communication training programs for health care providers might lead to improved patient knowledge and decision-making.20
The results of the current study demonstrate a continuation of the racial/ethnic differences in vaccine coverage documented in previous influenza seasons.21–24 Significantly lower rates of immunization were reported by non-Hispanic blacks, Hispanics and other racial/ethnic minorities. Compared to 2000–2001 vaccine prevalence, raw uptake rates by all racial/ethnic subgroups have increased but disparities have persisted.22 In the current study using 2008 data, non-Hispanic blacks were least likely to be immunized and the black-white disparity remained even after controlling for social class, demographic risk factors and self-reported diseases. The social class gradient we observed may exacerbate suboptimal vaccine coverage among minorities plagued by concentrated poverty, but it does not fully explain racial/ethnic differences.
Explanations of racial disparities include barriers to preventive care,23 false impressions of influenza severity,23 and minority patient mistrust.9,21,23 Studies have cited minority fears of contracting flu from the vaccine or experiencing side effects24 from interactions with other medications. Lower motivation to get vaccinated may reflect entrenched mistrust of the health care system9 or a deficiency of knowledge22, 24 resulting from low exposure to preventive care services.8 Generalizations about “minority” health behaviors may be deceptive, however, since different racial/ethnic groups face distinct obstacles to vaccination. Unvaccinated Hispanics enumerate structural barriers to preventive care including costs, transportation, language and lack of insurance.21 In contrast, unvaccinated non-Hispanic blacks frequently mention fears of contracting the influenza virus or experiencing negative side effects.21 Such fears are consistent with an ingrained black consciousness of discriminatory medical practices, including the infamous Tuskegee syphilis study.9
Variability in motivation may be a primary cause of differential vaccine uptake. It is believed that by increasing motivation, a substantial portion of “missed opportunities”22 across three major racial/ethnic categories could be eliminated. The projected effect would be most dramatic for non-Hispanic blacks and Hispanics, who are less likely than non-Hispanic whites to initiate trips to healthcare providers for the express purpose of obtaining an influenza vaccine.22 Another strategy proposed by Bouye et al. would utilize WIC sites as vaccination clinics.20 This concept is consistent with previous findings in support of alternative settings for vaccine dissemination, including pharmacies, groceries and other community locales, reducing time and transportation barriers as well as the need to coordinate with a health care provider.
Psychosocial barriers to the flu shot are not inevitable. Interventions within underserved populations can generate vaccine interest, particularly if they involve community-based participatory research.23.25 One multilevel intervention in East Harlem and the Bronx entitled Project VIVA employed door-to-door and street-based inoculation to create a local environment amenable to the vaccine while developing a generalizable method of rapid urban vaccine dissemination.25 Another means of increasing coverage is the use of a non-traditional setting as a proxy for the physician’s office. For example, in a study of different flu shot venues, Singleton et al. found that one third of adults sampled (aged ≥65) received the vaccine in a pharmacy, supermarket, workplace, or other non-clinical locale.26 Allocating additional resources to non-traditional settings might alleviate racial/ethnic disparities by increasing immunization among the “hard-to-reach,”25 the uninsured and individuals whose work commitments make vaccination difficult. Alternate vaccine venues may lower transportation and cost barriers, and thereby confer benefits to socioeconomically disadvantaged populations. Although low uptake by non-Hispanic blacks was not explained by SES or other demographic factors (Table 2), non-traditional settings could offer alternative vaccine opportunities to persons in less frequent contact with the health care system.
The present study describes influenza vaccination in the U.S. during the 2007–2008 flu season. A large, nationally representative sample allowed for detailed analyses of social disparities in vaccination. However, several limitations in this study warrant acknowledgment. Data were derived from self-report, which may be subject to respondent bias. Flu shot self-response has high sensitivity (98%) but low specificity (38%),7 suggesting that real vaccination rates may be lower than those reported here. It is also probable that many respondents were not aware of underlying medical conditions. This is particularly true among minorities, who receive lower levels of preventive care services and are more likely to be underinsured or lack any form of insurance. The 2008 BRFSS excluded households that rely exclusively on wireless phones. These households constitute a growing segment of the population (14% in 2004).27 Finally, we analyzed all interviews conducted during 2008, so some participants may have reported vaccination for different influenza seasons; however, when the sample was restricted to the first quarter of 2008 to avoid respondents referencing different influenza seasons, the overall prevalence and disparities were essentially the same. As expected, the prevalence generally increased for all racial/ethnic groups when interviews were restricted to the first quarter.
Racial and ethnic disparities contribute substantially to the under utilization of flu vaccine in the United States. The negative toll of inequality on minority health has been quantified and deserves reiteration. Fiscella and colleagues estimated that if disparities in vaccine coverage were eliminated across race and ethnic groups, then 33,000 minority years of life could be saved.28 Therefore, culturally relevant vaccine education programs for physicians and patients must become a public health priority. It should be noted that the goal of reporting social differentials is not to insinuate that the reference group receives the vaccine at an optimal rate. Inadequate vaccine coverage remains a problem for minorities and non-Hispanic whites, alike. However, the magnitude of disparities across groups warrants investigation. Neither the benefits arising from policies designed to minimize disparities, nor the injurious effects of inaction, are confined exclusively to vulnerable groups. For instance, failure to prepare for or respond to pandemic influenza within vulnerable populations might result in increased transmission and spread of infection in the general population.29 From this perspective, social disparities have very real implications for the health of all residents in the United States; accordingly, the nation’s collective health would benefit from an expansion of vaccine coverage in disadvantaged populations. Further, targeting underserved populations would advance infrastructure and administrative practices, as well as mass vaccination during pandemics.
The correlation between societal inequity and negative health outcomes is well-established, yet no concerted effort has been undertaken on the national scale to mitigate differential vaccine prevalence. Future studies should seek to elucidate the factors driving racial/ethnic disparities, considering both barriers to care such as language preference and socioeconomic disadvantage, as well as psychological forces including motivation, fear and trust.
Supplementary Material
Acknowledgments
Funding: This study was supported by the Intramural Research Program of the NIH, National Institute on Aging. The BRFSS was conducted by the US Centers for Disease Control and Prevention.
Sponsor’s Role: Staff at the National Institute on Aging reviewed and approved the manuscript.
Footnotes
Author Contributions: Each author participated in the study concept and design, data analysis and interpretation, and preparation of the manuscript.
Conflict of Interest: We declare no conflicts of interests in publishing this report. This study was supported by the Intramural Research Program of the NIH, National Institute on Aging.
| Elements of Financial/Personal Conflicts | Shauna T. Linn | Jack M. Guralnik | Kushang V. Patel | |||
|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | |
| Employment or Affiliation | X | X | X | |||
| Grants/Funds | X | X | X | |||
| Honoraria | X | X | X | |||
| Speaker Forum | X | X | X | |||
| Consultant | X | X | X | |||
| Stocks | X | X | X | |||
| Royalties | X | X | X | |||
| Expert Testimony | X | X | X | |||
| Board Member | X | X | X | |||
| Patents | X | X | X | |||
| Personal Relationship | X | X | X | |||
References
- 1.Antunes JLF, Waldman EA, Borrel C, et al. Effectiveness of influenza vaccination and its impact on health inequalities. Int J Epidemiol. 2007;36:1319–26. doi: 10.1093/ije/dym208. [DOI] [PubMed] [Google Scholar]
- 2.Nichol KL, Nordin JD, Nelson DB, et al. Effectiveness of influenza vaccine in the community-dwelling elderly. N Eng J Med. 2007;357:1273–81. doi: 10.1056/NEJMoa070844. [DOI] [PubMed] [Google Scholar]
- 3.Thompson WW, Shay DK, Weintraub E, et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003;289:179–86. doi: 10.1001/jama.289.2.179. [DOI] [PubMed] [Google Scholar]
- 4.Nelson JC, Jackson ML, Weiss NS, et al. New strategies are needed to improve the accuracy of influenza vaccine effectiveness estimates among seniors. J Clin Epidemiol. 2009;62:687–94. doi: 10.1016/j.jclinepi.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 5.Fiore AE, Shay DK, Broder K, et al. Centers for Disease Control and Prevention (CDC); Advisory Committee on Immunization Practices (ACIP) Prevention and control of influenza: Recommendations of the ACIP, 2008. MMWR Recomm Rep. 2008;57:1–60. [PubMed] [Google Scholar]
- 6.Gross PA, Hermogenes AW, Sacks HS, et al. The efficacy of influenza vaccine in elderly persons. A meta-analysis and review of the literature. Ann Intern Med. 1995;123:518–27. doi: 10.7326/0003-4819-123-7-199510010-00008. [DOI] [PubMed] [Google Scholar]
- 7.Ompad DC, Galea S, Vlahov D. Distribution of influenza vaccine to high-risk groups. Epidemiol Rev. 2006;28:54–70. doi: 10.1093/epirev/mxj004. [DOI] [PubMed] [Google Scholar]
- 8.Lu P, Bridges CB, Euler GL, et al. Influenza vaccination of recommended adult populations, U.S. 1989–2005. Vaccine. 2008;26:1786–93. doi: 10.1016/j.vaccine.2008.01.040. [DOI] [PubMed] [Google Scholar]
- 9.Eiser AR, Ellis G. Cultural competence and the African American experience with health care: The case for specific content in cross-cultural education. Acad Med. 2007;82:176–83. doi: 10.1097/ACM.0b013e31802d92ea. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance Survey Summary Data Quality Report. [Accessed 5 Aug. 2009];BRFSS - CDC’s Behavioral Risk Factor Surveillance System. 2008 http://www.cdc.gov/BRFSS/technical_infodata/quality.htm. Updated 2009.
- 11.Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162:199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- 12.Higashi T, Wenger NS, Adams JL, et al. Relationship between number of medical conditions and quality of care. N Engl J Med. 2007;356:2496–2504. doi: 10.1056/NEJMsa066253. [DOI] [PubMed] [Google Scholar]
- 13.Harris MI. Racial and ethnic differences in health care access and health outcomes for adults with type 2 diabetes. Diabetes Care. 2001;24:454–9. doi: 10.2337/diacare.24.3.454. [DOI] [PubMed] [Google Scholar]
- 14.Kennedy BS. Treating patients with multiple cardiovascular conditions: An analysis of outpatient data in the United States, 2005. J Natl Med Assoc. 2008;100:1260–70. doi: 10.1016/s0027-9684(15)31504-2. [DOI] [PubMed] [Google Scholar]
- 15.Lara M, Gamboa C, Kahramanian MI, et al. Acculturation and Latino health in the United States: A review of the literature and its sociopolitical context. Annu Rev Public Health. 2005;26:367–97. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Derose KP, Escarce JJ, Lurie N. Immigrants and health care: Sources of vulnerability. Health Aff (Millwood) 2007;26:1258–68. doi: 10.1377/hlthaff.26.5.1258. [DOI] [PubMed] [Google Scholar]
- 17.Wilson E, Chen AH, Grumbach K, et al. Effects of limited English proficiency and physician language on health care comprehension. J Gen Intern Med. 2005;20:800–6. doi: 10.1111/j.1525-1497.2005.0174.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.DuBard CA, Gizlice Z. Language spoken and differences in health status, access to care, and receipt of preventive services among US Hispanics. Am J Public Health. 2008;98:2021–8. doi: 10.2105/AJPH.2007.119008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Graham EA, Jacobs TA, Kwan-Gett TS, et al. Health services utilization by low-income limited English proficient adults. J Immigr Minor Health. 2008;10:207–17. doi: 10.1007/s10903-007-9069-3. [DOI] [PubMed] [Google Scholar]
- 20.Bouye K, Truman BI, Hutchins S, et al. Pandemic Influenza Preparedness and Response Among Public-housing Residents, Single-parent Families, and Low-income Populations. Am J Public Health. 2009;99:S287–93. doi: 10.2105/AJPH.2009.165134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen JY, Fox SA, Cantrell CH, et al. Health Disparities and prevention: Racial/ethnic barriers to flu vaccination. J Community Health. 2007;32:5–20. doi: 10.1007/s10900-006-9031-7. [DOI] [PubMed] [Google Scholar]
- 22.Hebert PL, Frick KD, Kane RL, McBean AM. The causes of racial and ethnic differences in influenza vaccination rates among elderly Medicare beneficiaries. Health Serv Res. 2005;40:517–37. doi: 10.1111/j.1475-6773.2005.00370.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Logan JL. Disparities in influenza immunization among US adults. J Natl Med Assoc. 2009;101:161–6. doi: 10.1016/s0027-9684(15)30830-0. [DOI] [PubMed] [Google Scholar]
- 24.Schneider EC, Cleary PD, Zaslavsky AM, et al. Racial disparity in influenza vaccination: Does managed care narrow the gap between African Americans and whites? JAMA. 2001;286:1455–60. doi: 10.1001/jama.286.12.1455. [DOI] [PubMed] [Google Scholar]
- 25.Coady MH, Galea S, Blaney S, et al. Project VIVA: A multilevel community-based intervention to increase influenza vaccination rates among hard-to-reach populations in New York City. Am J Public Health. 2008;98:1314–21. doi: 10.2105/AJPH.2007.119586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Singleton JA, Poel AJ, Lu PJ, et al. Where adults reported receiving influenza vaccination in the United States. J Am Infect Control. 2005;33:563–70. doi: 10.1016/j.ajic.2005.03.016. [DOI] [PubMed] [Google Scholar]
- 27.Mokdad AH. The Behavioral Risk Factors Surveillance System: Past, present, and future. Annu Rev Public Health. 2009;30:43–54. doi: 10.1146/annurev.publhealth.031308.100226. [DOI] [PubMed] [Google Scholar]
- 28.Fiscella K, Dressler R, Meldrum S, et al. Impact of influenza vaccination disparities on elderly mortality in the United States. Prev Med. 2007;45:83–7. doi: 10.1016/j.ypmed.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 29.Hutchins SJ, Fiscella K, Levine RS, et al. Protection of Racial/Ethnic Minority Populations During an Influenza Pandemic. Am J Public Health. 2009;99:S261–S270. doi: 10.2105/AJPH.2009.161505. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.