Abstract
BACKGROUND:
Exclusive nutrition with breastfeeding is the health provider of the infant and mothers and its continuing would provide more advantages. Exclusive nutrition on different communities is affected by different factors. This study aimed to determine continuous exclusive breastfeeding and some of the related factors.
METHODS:
This was a descriptive-analysis prospective study. The study population included all the breastfed mothers admitted in the obstetrics wards of the selected hospitals. Selecting the hospitals also was done randomly. Data collection tools included a questionnaire completed by 291 mothers. To obtain the data about breastfeeding duration, mothers were phone called at the first and sixth postpartum months. The collected data were analyzed using descriptive and analytical statistics and software SPSS.
RESULTS:
Estimation of mean and standard deviation of exclusive breastfeeding duration at the first and sixth months after the delivery, respectively, were 3.86 (0.55) and 23.67 (6.63) weeks. One month after the delivery, 93.1%, 6.2% and 0.7% of the mothers, respectively, had exclusive breastfeeding, breastfeeding with formula milk or other ingredients and discontinuation of breastfeeding; 6 months after the delivery, these values changed to 86.3, 12 and 1.7%, respectively. The most frequent period of breastfeeding discontinuation (6.9%) was related to 1-4 weeks. The results indicated that statistically there was a significant correlation between breastfeeding duration and age and the birth hospital. While the results of the study showed no association between breastfeeding duration and number of the children, duration of marriage, educational level and mothers’ occupation.
CONCLUSIONS:
The findings of the present study represented a high continuous exclusive breastfeeding which perhaps was due to applied baby-friendly hospitals strategies. Furthermore, to prevent from discontinuation of exclusive breastfeeding, knowing the discontinuation time and its related factors, particularly the first four postpartum weeks, can increase the knowledge of the health staff about counseling and education.
KEY WORDS: Continuous exclusive breastfeeding, socio-demographic factors
Breast milk not only is an ideal nutrition for the infant1 also can protect him/her against some diseases.2 Thus, the infants fed by the breast milk are healthier and less experience diseases such as infections, diabetes, obesity and asthma.3 Breastfeeding, in addition to maintain and promote health of the infants, would provide physical and mental health of the mother and cause reduction in postpartum hemorrhages and breast and ovarian cancer. The role of breast milk in providing infant's health is in direct association with duration of breastfeeding.4 Thus, long breastfeeding can bring about more advantages for the infant and mother.5 Islam also had been considered this issue and recommended to the mothers to breast feed their children for two years. Promotion of nutrition with breast milk has been focused in recent years in line with expansion of human knowledge and researches all over the world and many organizations like World Health Organization and UNICEF emphasized breastfeeding as the superior method for the infant.6 75 percent of the women start feeding from the breast in postpartum period and 50% continue to six months and 25% continue to one year.1 In spite of Islam's recommendations and latest instructions of World Health Organization on exclusive breastfeeding until 6-month old and emphasis to continue it7 and despite numerous advantages of this method, unfortunately, a percentage of the mothers discontinue this method shortly after a while.8 Latest obtained statistics from Isfahan Province in 2006 also indicated the same finding; it indicated that only 17.4% of the infants aged 6-month old exclusively fed by breast milk.9
A number of factors can affect the ability of the mothers to breastfeed and its continuation. Among these variables, having a higher education level has been introduced as a factor for continuous exclusive breastfeed.10 Furthermore, some studies have shown that multiparous women and older mothers were more willing to continue breastfeeding for a longer time. In addition, low maternal socioeconomic status and early retuning to the workplace have been associated with early discontinuation of breastfeeding.11 Findings obtained from studies indicated that exclusive breastfeeding in different communities are affected by different factors and are resulted from social and biological factors of mother. Therefore, it is necessary to conduct such a study in different communities.12
On the other hand, despite numerous researches and implementing many efforts to encourage and support towards exclusive breastfeeding at the first six months, still not all the countries achieved to the World Health Organization recommendation about exclusive breastfeeding6 and almost failed to achieve exclusive breastfeeding.13 Therefore, to promote breastfeeding which is considered as one of the major components of the primary health care and is the important part in providing health, nutrition and other required social measures to promote optimal growth and development of infants and young children and its promotion and protection has been regularly emphasized in World Health Organization's meetings14 and considering that knowing discontinuation time of breastfeeding and its related factors is necessary to provide appropriate interventions for expanding the breastfeeding duration, the researchers of the current paper decided to carry out a study to evaluate continuous exclusive breastfeeding and some of the related factors.
Methods
This was a correlation, prospective descriptive-analytical study. The study population included all the breastfed mothers admitted to the obstetric wards of private and public hospitals of Isfahan. In this study, the hospitals selected randomly and the study subjects selected by simple sampling method. The researchers and interviewers referred to three public and private hospitals after receiving the introduction letter. The mothers who recently had delivery and were admitted to obstetric ward and also had the inclusion criteria entered the study by simple sampling and also receiving the consent from. Sampling was done in 2009-2010. In this study, inclusion criteria included age up to 16 years old, term delivery (37th to 42nd week), started breastfeeding, no history of high-risk pregnancy and feeding the infant with breast milk in the past 24 hours. If the breastfed mother or her infant required intensive care after the delivery or a mother did not want to participate in the study, they excluded from the study. Data collection tools included a questionnaire which was completed in interviewing method. In this study, in order to obtain validity of the data collection tools, content validity method was used and in order to identify reliability, Cronbach's alpha correlation coefficient and split-half method were applied. After explanation about study objectives, the information about individual and productivity of 300 mothers were collected; however, due to lack of accessibility to all the subjects to answer to the questions, phone interviewing was done with 291 mothers. In order to obtain the data related to breastfeeding duration, these mothers were phone called at the first and sixth postpartum months. In phone calls, the mothers were asked about continuation or discontinuation of the breast milk or using formula milk or other ingredients. If a mother had stopped breast milk, she was asked about the discontinuation time and then, her exclusive breastfeeding duration was calculated per week and was recorded in the questionnaire. And if a mother, in addition to her breast milk, had used other ingredients or formula, it was recorded in the questionnaire. Finally, the data collected from 291 left mothers were analyzed using descriptive and analytical statistics and Software SPSS.
Results
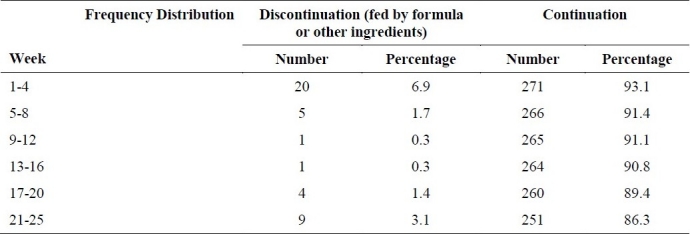
The results of exclusive breastfeeding duration showed that in one month and six months after the delivery, mean and standard deviation of breastfeeding duration, respectively, were 3.86 (0.55) and 23.67 (6.63) weeks. According to Table 1, out of the total samples (291 subjects) the most frequent period of exclusive breastfeeding discontinuation (6.9%) was related to the 1st to 4th week. But, 83.6% of the mothers still had exclusive breastfeeding at the 21st to 25th week.
Table 1.
Frequency distribution of exclusive breastfeeding continuation and discontinuation per week after six months
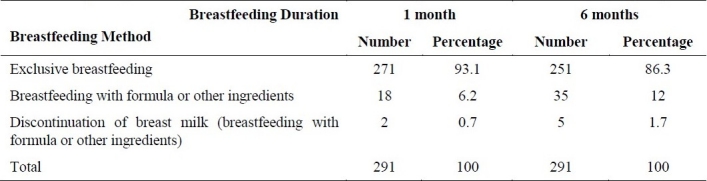
As indicated in Table 2, one month after delivery, respectively, 93.1, 6.2 and 0.7 percent of the mothers had exclusive breastfeeding, breastfeeding with formula or with other ingredients; breastfeeding discontinuation included 86.3, 12 and 1.7 percent of mothers six months after the delivery, respectively. Thus, one and six months postpartum, among all the mothers who started breast milk, respectively, 2 and 5 mothers completely stopped breastfeeding.
Table 2.
Frequency distribution of method of breastfeeding after one and six months in postpartum
Study findings showed that the majority of the mothers (62.2%) only had one child and 49.1% of them were 26-35 years old. The most frequent (66.3%) educational level of the mothers included intermediate and high school graduates.
The results of Pearson test showed that statistically there was a significant correlation between age and duration of breastfeeding (p < 0.001). But, Pearson test showed no significant correlation between duration of breastfeeding and the variables of number of children and duration of marriage (p > 0.05). This test also showed no significant correlation between exclusive breastfeeding duration and educational level (p > 0.05).
The findings of one way ANOVA to evaluate the association between the type of hospital and duration of breastfeeding indicated that after 6 months of breastfeeding duration, statistically there was no significant correlation between these two variables in any hospital (p < 0.05). Furthermore, t test showed no significant correlation between the occupation of the mothers at the 6 months postpartum and the duration of breastfeeding (p > 0.05).
Discussion
The findings of the study indicated that after one and six months after the delivery, 93.1% and 86.3% of the infants were fed exclusively from the breast milk, respectively, while in Romania, study results showed that only 68 percent of the mothers who started breast milk still continued exclusive breastfeeding one month after delivery and this rate reduced to 6 and 8 months after that period.6 The results of a study in the United States also showed that among 73% of the mother who started breastfeeding, only 23% continued it until 6 months.1 Moreover, findings of a study in Netherland indicated that in 1 and 6 months in postpartum, 51 and 25% of the mothers, respectively, continued exclusive breastfeeding.15 Thus, our study results showing the continuous exclusive breastfeeding in three selected hospitals in Isfahan compared to other countries and especially compared to the World Health Organization recommendations had a high standard values; this probably might be due to implementation of the measures including strategies of baby-friendly hospitals carried out in the past 12 years.19 It should be noted that to promote exclusive breastfeeding in the baby-friendly hospitals, the hospital staff have conducted some measures and provided the necessary recommendations to the lactating mothers. Findings of Lewallen in 2005 showed that most of the lactating mothers obtained the information and assistive breastfeeding in hospitals.17 Baby-friendly hospital's policy had an obvious influence on breastfeeding behaviors.18 In addition, the findings of some of the studied have shown that cultural values and beliefs of each society also can influence nutrition with breast milk.19 Therefore, a high percentage of breastfeeding to 6 months after the delivery in this study can be associated with religious beliefs of the mothers about breastfeeding until 2 years and the recommendation of Islam religion.
Furthermore, findings have shown that a large number of the mothers had exclusive breastfeeding for nearly 6 months. On the other hand, the highest frequency of breastfeeding discontinuation occurred at the 1-4 weeks; in other words, its discontinuation mostly was observed at the early breastfeeding period. In this regard, Taveras also stated that the most exclusive breastfeeding discontinuation occurred at the early time of using this method.8 On the other hand, it seems that the differences in duration of exclusive breastfeeding in different hospitals were associated with study environments. Since mean exclusive breastfeeding duration in the studied educational hospitals was higher than two other hospitals, encouragement and persuasion for breastfeeding and its related trainings by the educational staff might influence the increase in continuation of breastfeeding.
The findings of Lanting about continuation of breastfeeding in 2005 showed that mothers with higher educational level continued breastfeeding for a longer time.15 However, findings of other researchers indicated that continuation of breastfeeding in mother who had academic education was higher than those who did not have academic education.20 Therefore, it seems that lack of an association between education and duration of breastfeeding in this study was related to low number of the samples with high educational level. In terms of association between age of the mothers with continuation of exclusive breastfeeding, results of Nichols and Rebhan confirmed the association of a significant correlation between these two variables.21,22 The findings of some of the studies showed that working mothers were more likely to stop breastfeeding18,23 which was not in accordance with the present study. In this regard, Murtagh (2011) announced that modern mothers gained more awareness and knowledge about breastfeeding and its supportive laws in the workplace.24 Thus, perhaps lack of an association between job and duration of breastfeeding in this study was related to the use of 6-month sick leave by the breastfeeding mothers that provided the possibility of exclusive breastfeeding continuation for these mothers as well as non-working mothers.
Conclusion
It should be noted that interventions of the caregivers in hospitals and dedication of some places to conduct follow-ups and consultation to the mothers during the breastfeeding period can help exclusive breastfeeding continuation.19 Therefore, to prevent exclusive breastfeeding discontinuation particularly at the first 4 weeks, appropriate follow-ups and care should be implemented. On the other hand, considering the related factors of exclusive breastfeeding continuation such as age of the mother and birth hospital in the community can increase the knowledge of the health staff about their important task which certainly is the appropriate counseling and training.
The authors declare no conflict of interest in this study.
References
- 1.Gill SL, Reifsnider E, Lucke JF, Mann AR. Predicting breast-feeding attrition: adapting the breast-feeding attrition prediction tool. J Perinat Neonatal Nurs. 2007;21(3):216–24. doi: 10.1097/01.JPN.0000285811.21151.37. [DOI] [PubMed] [Google Scholar]
- 2.Rice S, Coombs D, Fish L, Leeper J. Breast-feeding and contraception in Peru. J Health Popul Nutr. 2002;20(1):51–58. [PubMed] [Google Scholar]
- 3.McCarter-Spaulding D, Gore R. Breastfeeding self-efficacy in women of African descent. J Obstet Gynecol Neonatal Nurs. 2009;38(2):230–43. doi: 10.1111/j.1552-6909.2009.01011.x. [DOI] [PubMed] [Google Scholar]
- 4.Askenler RJ. Breastfeeding. In: Nik Nafs P, translator. Tehran: Publishing Information; 2002. p. 165. [Google Scholar]
- 5.Tarrant M, Dodgson JE, Choi VW. Becoming a role model: the breastfeeding trajectory of Hong Kong women breastfeeding longer than 6 months. Int J Nurs Stud. 2004;41(5):535–46. doi: 10.1016/j.ijnurstu.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 6.Wutke K, Dennis CL. The reliability and validity of the Polish version of the Breastfeeding Self-Efficacy Scale-Short Form: translation and psychometric assessment. Int J Nurs Stud. 2007;44(8):1439–46. doi: 10.1016/j.ijnurstu.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 7.Ravi M. Said and unsaid about the artificial milk, and to warn doctors and parents. Quarterly of Shiremadar. 2003;4(15):6–11. [Google Scholar]
- 8.Taveras EM, Capra AM, Braveman PA, Jensvold NG, Escobar GJ, Lieu TA. Clinician support and psychosocial risk factors associated with breastfeeding discontinuation. Pediatrics. 2003;112(1 Pt 1):108–15. doi: 10.1542/peds.112.1.108. [DOI] [PubMed] [Google Scholar]
- 9.Aghdak P. Child health indicators based on the results of IMES, executive programs operating single children health [Online] 2006. Available from: URL: www.http.phc-isf.ir/Files/
- 10.Li L, Li S, Ali M, Ushijima H. Feeding practice of infants and their correlates in urban areas of Beijing, China. Pediatr Int. 2003;45(4):400–6. doi: 10.1046/j.1442-200x.2003.01754.x. [DOI] [PubMed] [Google Scholar]
- 11.Ystrom E, Niegel S, Klepp KI, Vollrath ME. The impact of maternal negative affectivity and general self-efficacy on breastfeeding: the Norwegian Mother and Child Cohort Study. J Pediatr. 2008;152(1):68–72. doi: 10.1016/j.jpeds.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 12.Imani M, Mohammadi M, Rakhsha F, Shafiee S. The prevalence of exclusive breast feeding and related factors in infants in Zahedan, 2000-2001. Feyz. 2003;7(2):26–33. [Google Scholar]
- 13.Alus TM, Okumus H, Dennis CL. Translation and psychometric assessment of the Breast-feeding Self-Efficacy Scale-Short Form among pregnant and postnatal women in Turkey. Midwifery. 2010;26(1):101–8. doi: 10.1016/j.midw.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 14.Sadondiyan S, Taheri M. Mashhad: Sokhan Gostar Publication; 2008. Help support breast feeding. [Google Scholar]
- 15.Lanting CI, Van Wouwe JP, Reijneveld SA. Infant milk feeding practices in the Netherlands and associated factors. Acta Paediatr. 2005;94(7):935–42. doi: 10.1111/j.1651-2227.2005.tb02014.x. [DOI] [PubMed] [Google Scholar]
- 16.Guidelines to promote breastfeeding in hospitals, child-friendly [Online] Available from: URL: www.darman.umsu.ac.ir/
- 17.Lewallen LP. A review of instruments used to predict early breastfeeding attrition. J Perinat Educ. 2006;15(1):26–41. doi: 10.1624/105812406X92967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen YC, Wu YC, Chie WC. Effects of work-related factors on the breastfeeding behavior of working mothers in a Taiwanese semiconductor manufacturer: a cross-sectional survey. BMC Public Health. 2006;6:160. doi: 10.1186/1471-2458-6-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ergenekon-Ozelci P, Elmaci N, Ertem M, Saka G. Breastfeeding beliefs and practices among migrant mothers in slums of Diyarbakir, Turkey, 2001. Eur J Public Health. 2006;16(2):143–8. doi: 10.1093/eurpub/cki170. [DOI] [PubMed] [Google Scholar]
- 20.Hendricks K, Briefel R, Novak T, Ziegler P. Maternal and child characteristics associated with infant and toddler feeding practices. J Am Diet Assoc. 2006;106(1 Suppl 1):S135–S148. doi: 10.1016/j.jada.2005.09.035. [DOI] [PubMed] [Google Scholar]
- 21.Nichols S, Dillon-Remy M, Thomas-Murray T, Baker N. Socio-demographic and health system factors in relation to exclusive breast-feeding in Tobago. West Indian Med J. 2002;51(2):89–92. [PubMed] [Google Scholar]
- 22.Rebhan B, Kohlhuber M, Schwegler U, Koletzko BV, Fromme H. Infant feeding practices and associated factors through the first 9 months of life in Bavaria, Germany. J Pediatr Gastroenterol Nutr. 2009;49(4):467–73. doi: 10.1097/MPG.0b013e31819a4e1a. [DOI] [PubMed] [Google Scholar]
- 23.Ong G, Yap M, Li FL, Choo TB. Impact of working status on breastfeeding in Singapore: evidence from the National Breastfeeding Survey 2001. Eur J Public Health. 2005;15(4):424–30. doi: 10.1093/eurpub/cki030. [DOI] [PubMed] [Google Scholar]
- 24.Murtagh L, Moulton AD. Working mothers, breastfeeding, and the law. Am J Public Health. 2011;101(2):217–23. doi: 10.2105/AJPH.2009.185280. [DOI] [PMC free article] [PubMed] [Google Scholar]


