Abstract
Background:
Bispectral index monitoring system (BIS) is one of the several systems used to measure the effects of anaesthetic and sedative drugs on the brain and to track changes in the patient's level of sedation and hypnosis. BIS monitoring provides information clinically relevant to the adjustment of dosages of sedating medication. It can help the nursing personnel in preventing under- and over sedation among intensive care unit (ICU) patients.
Objective:
The present study was conducted to assess the knowledge of nursing personnel working in the ICU regarding BIS.
Methods:
Fifty-four subjects participated in the study. A structured questionnaire was developed to assess the knowledge of the nursing personnel regarding BIS. Focus group discussions were held among the nursing personnel to know their views regarding BIS.
Results:
Mean age (years) of the subjects was 30.7±7.19 (21–47) years, with a female preponderance. Although the use of BIS in ICU is not common, majority (94.44%) were aware of BIS and its purpose. 79.62% of the subjects knew about its implication in patient care. The mean knowledge score of the subjects was 11.87±2.43 (maximum score being 15).
Conclusion:
There exists an awareness among the critical care nursing staff in our institution regarding BIS and its clinical implications. Its use in the critical care setting may benefit the patients in terms of providing optimal sedation.
Keywords: Awareness, bispectral index monitoring system, nursing personnel
INTRODUCTION
Nursing forms the backbone of patient care management in an intensive care setting. The overall care, including patient comfort and sedation, is provided by the nursing personnel. Because of lack of scientific sedation practices in the intensive care unit (ICU), patients usually face over- or undersedation.[1] The results of oversedation in the mechanically ventilated patients are an increased time of ventilation, an increased stay in the ICU and an increased cost of care.[2] The untoward effects of undersedation include an increased production of endogenous catecholamines that result in an increase in blood pressure, heart rate and myocardial oxygen consumption.[3] Use of a bispectral index (BIS) monitoring in the ICU is based on three primary goals: Enhancing patient care by optimizing sedations, decreasing nurse's workload and reducing the cost of sedation. A BIS value between 60 and 80 is consistent with sedation.[4]
The use of the BIS monitoring system in many Indian ICUs is in the introductory phase. Before recommending the use of BIS in Indian intensive care settings, it is important that the critical care nursing personnel are made aware of it. Thus, this study was undertaken to assess the knowledge of BIS among the nursing personnel working in various ICUs of a tertiary care medical centre of India.
METHODS
Using the purposive sampling technique 54 nursing personnel working in various ICUs (Anaesthesia/Main, Hepatic, Respiratory, Gastroenterology and Cardiothoracic and Vascular Surgery) of the hospital were included in the study. Approval for conducting the study was sought from the ethics committee of the institute. An informed written consent was taken from each subject. Data was analyzed using descriptive statistics.
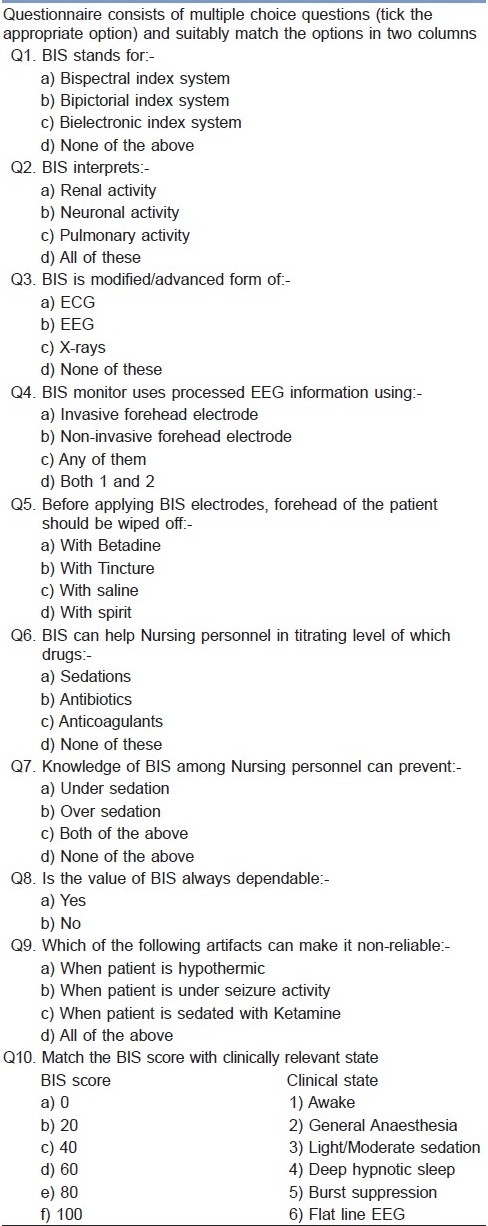
A questionnaire was developed after reviewing the relevant literature and consultation with the experts from the Department of Anaesthesia and Nursing Education. It consisted of two parts. Part-A was pertaining to demographic data of the subjects. Part-B was to assess their knowledge regarding BIS [Table 1]. It contained 10 questions, of which nine were multiple choice questions and one was to match the columns between BIS score and clinical state. Score 1 was given to each correct answer and 0 to each wrong answer. The maximum knowledge score was 15. The mean knowledge score was calculated by adding the total score of all the participants and dividing it by the total number of participants.
Table 1.
Knowledge Assessment Questionnaire
Focused group discussions were also conducted in a group of four to six nursing personnel. It helped the interviewer to collect data regarding the viewpoint of nursing personnel about BIS.
RESULTS
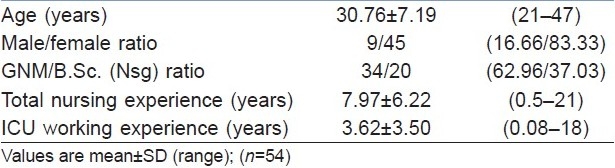
The mean age (years) of the subjects was 30.7±7.19 years, with the range of 21–47 years. Majority (83.3%) were females, of which 34 (62.96%) were diploma holders and 20 (37.03%) were graduates. The mean working experience was 7.97±6.22 years. The mean experience of working in ICU was 3.62±3.50 years [Table 2].
Table 2.
Demographic data of the subjects
Awareness of subjects regarding bispectral index monitoring system
All the study subjects were aware of the fact that BIS stands for “bispectral index monitoring system”. Majority (94.44%) had the knowledge that BIS interprets neuronal activity and is a modified form of electroencephalogram (EEG), which is interpreted by using noninvasive forehead electrodes. In actual practice, BIS monitoring was incorporated only in the main ICU; hence, nursing personnel working in the main ICU were comparatively more aware of the fact.
Regarding cleansing of the patient's forehead before applying the BIS electrode, 40 (74.07%) subjects considered spirit to be used for cleaning, whereas 10 (18.15%) considered tincture, three (5.55%) considered saline and one (1.85%) considered betadine for the same purpose.
Majority (94.44%) of the subjects were of the clear-cut view point that BIS will help the nursing personnel in titrating the sedative drugs in patients. Forty-three (79.62%) nursing personnel knew that knowledge of BIS can prevent both under- and oversedation. Forty-one (75.92%) subjects responded that BIS is not always reliable in assessing the neuronal activity of the patient, 11 (20.37%) subjects had no comments on its reliability, whereas two (3.70%) subjects thought that BIS is always reliable. Forty-four (81.48%) subjects were aware of the artifacts that makes BIS nonreliable sometimes.
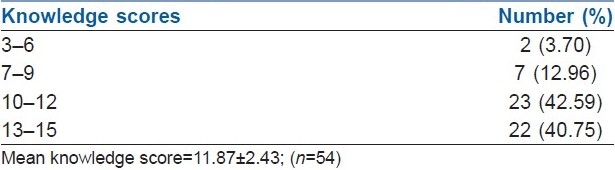
The maximum knowledge score was 15. The mean knowledge score of the subjects was 11.87±2.43, with a range of 6–15. Majority (83.34%) scored between 10 and 15 marks [Table 3].
Table 3.
Mean knowledge score of the subjects regarding bispectral index monitoring system
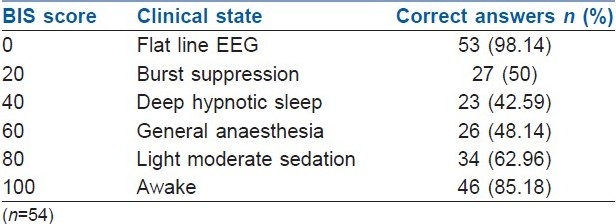
Majority of the subjects knew that 0 BIS score represents clinical state of flat line of EEG (98.14%) and 100 BIS score represents state of awake (85.18%). Around 50% of the subjects were aware of the clinical state of the patient as per the 20, 40, 60 and 80 BIS score [Table 4].
Table 4.
Awareness of the subjects regarding their knowledge about correlation of bispectral index monitoring system with its clinical state
Focused group discussion
Most of the nursing personnel were in favour of the use of BIS in ICUs to titrate the sedation levels within the recommended dosage levels. The use of BIS will prevent both the under- and oversedation among mechanically ventilated patients.
Nursing personnel considered BIS a relevant tool to assess the neuronal state of the patient as compared with the glasgow coma scale (GCS), which becomes irrelevant when patients are on paralytic sedations or muscle relaxants. One factor that they considered as a drawback was the cost of the BIS sensor, which is around 1000 in Indian rupees. The patients in our hospital belong to the low-socioeconomic income group and they find this expensive to purchase.
All the nursing personnel appreciated the BIS monitoring system, but they wanted to have more elaborated and detailed teaching programmes regarding the BIS monitoring system.
DISCUSSION
The use of BIS is not very popular in a greater part of the intensive care settings in India. Although majority of the nurses working in our ICUs were aware of BIS and its purpose, this finding may not be true about other ICUs in India. The awareness of BIS in other ICUs needs to be studied. It is imperative that knowledge should be succeeded by its practical application. Use of a BIS monitoring may help standardize clinical practice and improve patient care.[5] BIS-guided sedation needs to be introduced in the critical care settings in an Indian scenario.
Focused group discussion revealed that BIS is a relevant tool to assess the neuronal state of the patient as compared with GCS, which becomes irrelevant at various clinical situations. Similarly, the study by Olson et al. showed that indirect monitoring of sedation by using vital signs and subjective sedation scales have shortfalls, because heart rate and blood pressure are not consistently sensitive to changing levels of consciousness.[6] Monitoring of sedation in an intensive care setting can be challenging for the nursing staff because the effects of sedative medications vary from patient to patient. As per Kaplan, 69% of the ICU patients were inappropriately sedated, 54% were oversedated and 15% were undersedated.[7] With BIS monitoring, fewer patients experience adverse physiological effects related to inadequate sedation.[8] According to the study held in a neurocritical care unit, nurses found that sedation could be optimized by incorporating BIS monitoring into the care of patients in the ICU.[6]
CONCLUSION
The survey reveals that greater part of the critical care nursing personnel in our institution were aware of the importance of BIS monitoring. However, this may not be true for majority of the ICUs throughout our country, and needs to be studied in the national perspective. It is high time that we introduce BIS monitoring in the critical care settings in the Indian scenario to optimize sedation. Before that, we need to generate awareness among the critical care personnel as a strategy to successfully implement its use in the Indian context.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Smith SE. What is an ICU? [Last Accessed on 2010 Mar 15]. Available from: www.Pubmed.com/what is an icu.htm .
- 2.Donaldson M, Goodchild JH. Use of bispectral index system (BIS) to monitor enteral conscious (Moderate) sedation during general dental procedures. J Can Dent Assoc. 2009;75:709. [PubMed] [Google Scholar]
- 3.Ostermann ME, Keenan SP, Seiferling RA, Sibbald WJ. Sedation in the intensive care unit. JAMA. 2000;283:1451–9. doi: 10.1001/jama.283.11.1451. [DOI] [PubMed] [Google Scholar]
- 4.Olson DM, Chioffi SM, Macy GE, Meek LG, Cook HA. Potential benefits of bispectral index monitoring in critical care.A case study. Crit Care Nurse. 2003;23:45–52. [PubMed] [Google Scholar]
- 5.Struys M, Versichelen L, Byttebier G, Mortier E, Moerman A, Rolly G. Clinical usefulness of the bispectral index for titrating propofol target effect-site concentration. Anaesthesia. 1998;53:4–12. doi: 10.1111/j.1365-2044.1998.00279.x. [DOI] [PubMed] [Google Scholar]
- 6.Olson DM, Chioffi SM, Macy GE, Meek LA, Cook HA. Role of the bispectral index in sedation monitoring in the ICU. Crit Care Nurs. 2003;23:45–52. [PubMed] [Google Scholar]
- 7.Kaplan LJ, Bailey H. Bispectral index (BIS) monitoring of ICU patients on continuous infusion of sedatives and paralytics reduces sedative drug utilization and cost. Crit Care Med. 2000;4(Suppl):S110. [Google Scholar]
- 8.Coursin DR, Coursin DB. Survivors beware of posttraumatic stress disorder: What shall we tell the Men in Black? Crit Care Med. 1998;26:634–5. doi: 10.1097/00003246-199804000-00004. [DOI] [PubMed] [Google Scholar]


