Abstract
Background:
Use of suxamethonium is associated with an increase in intraocular pressure (IOP) and may be harmful for patients with penetrating eye injuries. The purpose of our study was to observe the efficacy of dexmedetomidine for prevention of rise in IOP associated with the administration of suxamethonium and endotracheal intubation.
Methods:
Sixty-six American Society of Anaesthesiologists I or II patients undergoing general anaesthesia for non-ophthalmic surgery were included in this randomized, prospective, clinical study. Patients were allocated into three groups to receive 0.4 μg/kg dexmedetomidine (group D4), 0.6 μg/kg dexmedetomidine (group D6) or normal saline (group C) over a period of 10 min before induction. IOP, heart rate and mean arterial pressure were recorded before and after the premedication, after induction, after suxamethonium injection and after endotracheal intubation.
Results:
Fall in IOP was observed following administration of dexmedetomidine. IOP increased in all three groups after suxamethonium injection and endotracheal intubation, but it never crossed the baseline value in group D4 as well as in group D6. Fall in mean arterial pressure was noticed after dexmedetomidine infusion, especially in the D6 group.
Conclusion:
Dexmedetomidine (0.6 μg/kg as well as 0.4 μg/kg body weight) effectively prevents rise of IOP associated with administration of suxamethonium and endotracheal intubation. However, dexmedetomidine 0.6 μg/kg may cause significant hypotension. Thus, dexmedetomidine 0.4 μg/kg may be preferred for prevention of rise in IOP.
Keywords: Dexmedetomidine, effect on intraocular pressure, endotracheal intubation, intraocular pressure, premedication, suxamethonium
INTRODUCTION
Emergency ophthalmic surgery poses a challenge to the anaesthesiologist as patients with penetrating eye injury often present with full stomach. These patients require rapid sequence induction and intubation without increasing the intraocular pressure (IOP). Suxamethonium, the most commonly used depolarizing muscle relaxant for rapid sequence airway management, increases the IOP.[1,2] Various methods have been used to attenuate the effects of suxamethonium on IOP. They include self-taming with small dose of suxamethonium, pretreatment with non-depolarizing muscle relaxant, use of nifedipine and nitroglycerin.[3]
Dexmedetomidine is a highly selective alpha-2 adrenergic agonist that has IOP-lowering properties.[4,5] It has been approved as a short-term sedative for critically ill patients needing mechanical ventilation.[6] Some of the well-documented beneficial effects of dexmedetomidine are anxiolysis, sedation, analgesia and sympatholysis with minimal respiratory depression.[7] The elimination half-life of dexmedetomidine is 2–3 h, with a context-sensitive half-time ranging from 4 min after a 10-min infusion to 250 min after an 8-h infusion.[8] It has been observed that the rise of IOP with suxamethonium and intubation can be blunted with dexmedetomidine premedication.[9] The aim of this study is to determine the efficacy of 0.4 μg/kg and 0.6 μg/kg of intravenous (i.v.) dexmedetomidine for prevention of rise of IOP by suxamethonium and intubation.
METHODS
After obtaining the institutional ethics committee clearance and written informed consent, 66 adult patients of American Society of Anaesthesiologists (ASA) I or II undergoing elective non-ophthalmic surgeries under general anaesthesia were included in the study. Patients more than 60 years of age, having hypertension, obese (body mass index (BMI) >30), with raised IOP or any other ophthalmic disease were excluded from the study. Patients were also not included if they had any contraindication to dexmedetomidine, like haemodynamic instability, or were receiving any drug known to alter IOP.
All patients were randomly allocated into three groups of 22 patients each to receive 0.4 μg/kg dexmedetomidine (group D4), 0.6 μg/kg dexmedetomidine (group D6) or normal saline (group C) i.v. as premedication.
On arrival in the operation theatre, multichannel monitors of Philips IntelliVue MP 20 with the facility to measure pulse-oximeter, non-invasive blood pressure (NIBP), ECG, temperature and respiratory gas monitor (RGM) were attached and baseline vital parameters of the patients were recorded. Topical lignocaine 4%, two drops in each eye was applied to the cornea and IOP was measured with a Schioetz tonometer (made in Germany) by an ophthalmologist who was unaware of the nature of the study.
Intravenous (i.v) cannulation was performed and 0.1 ml/kg of study solution was administered by a syringe pump over a period of 10 min. The following solutions were prepared by an anaesthesiologist who was not involved in data recording:
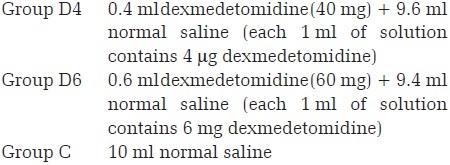
After pre-oxygenation for 3 min, patients were induced with a sleep dose of thiopentone sodium. Suxamethonium was administered at a dose of 1.5 mg/kg to achieve muscular relaxation for intubation. After cessation of fasciculation, the trachea was intubated under direct vision laryngoscopy. The patient was excluded from the study if the trachea could not be intubated at the first attempt. After securing the airway, anaesthesia was maintained in all three groups with oxygen (33%), nitrous oxide (66%), isoflurane (1%), fentanyl citrate (1 μg/kg) and incremental doses of vecuronium bromide. The lung was ventilated to maintain the end tidal carbon dioxide partial pressure between 4.3 and 4.6 kPa. Decrease in systolic blood pressure (more than 30% below baseline) was recorded as hypotension and treated with crystalloids and phenylephrine. Bradycardia [heart rate (HR) <50 beats/min] was treated by i.v. atropine. These cases were also excluded from the study.
Mean arterial pressure (MAP), HR and IOP was recorded at the following time points:
T1: Before premedication
T2: Five minutes after premedication
T3: Thirty seconds after thiopentone sodium
T4: Thirty seconds after suxamethonium
T5: One minute after intubation
T6: Two minutes after intubation
T7: Four minutes after intubation
T8: Six minutes after intubation
Sample size estimation was performed using power and sample size calculation software version 3.0 to detect a mean IOP difference of 30% between the study groups with alpha error 0.05 and beta error of 0.20. Minimum adequate sample size was 20 in each group. Power (0.9) analysis was based on the observation of previous studies,[9] which showed an average increase in IOP of 6 mmHg after suxamethonium and intubation.
Data were presented in mean±SD. One-way ANOVA was used for analysis of differences in age, weight, duration of laryngoscopy, haemodynamic variables and IOP. A P-value <0.05 was considered statistically significant.
RESULT
Two patients in the D6 group developed hypotension after administration of dexmedetomidine and were therefore excluded from study. One patient of the D4 group and two patients of the control group were also excluded, as intubation could not be done on first attempt. Final tabulation was done on 61 patients.
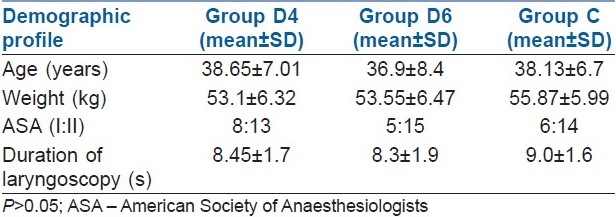
There were no significant differences among the groups regarding age, weight, ASA physical status of the patients and duration of laryngoscopy [Table 1]. Baseline HR, MAP and IOP of the different groups were also comparable.
Table 1.
Demographic profile
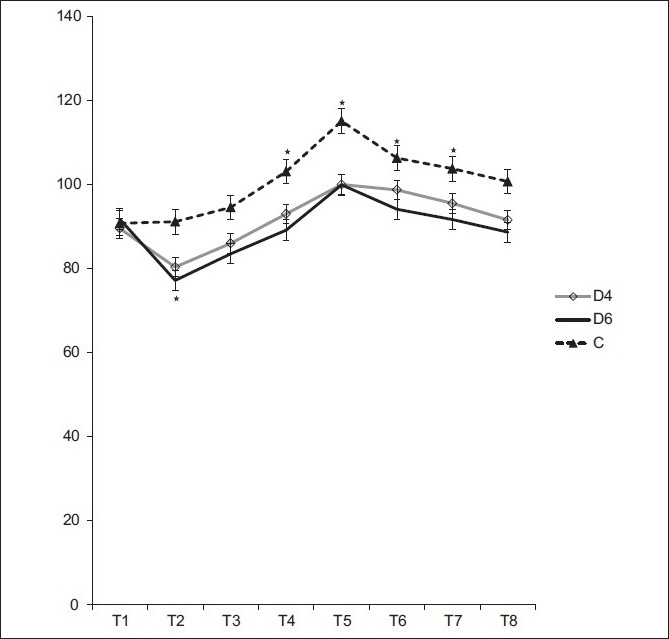
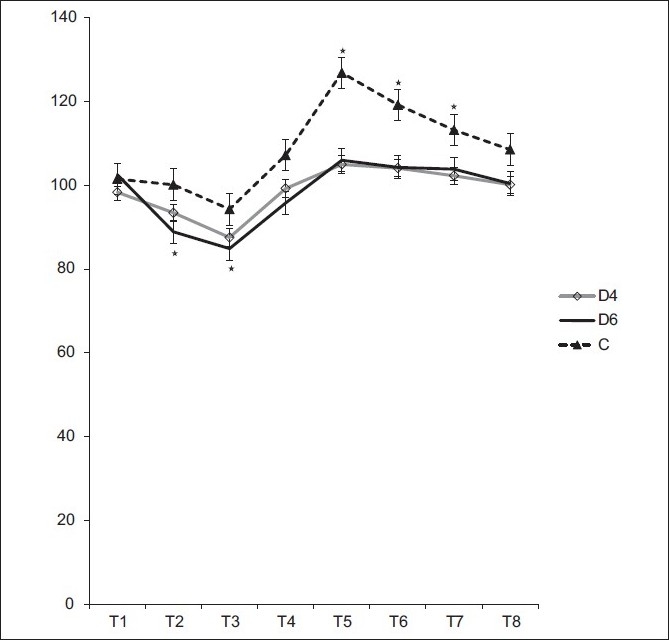
Decrease in IOP was observed in group D4 and group D6 following dexmedetomidine injection (P<0.001). Following suxamethonium injection and endotracheal intubation, IOP increased in all the groups, but it dropped below baseline in the D4 and D6 groups. IOP was more than the baseline in the control group even after 6 min following intubation [Figure 1, Table 2]. After premedication with dexmedetomidine, decrease in HR was observed in both groups (P<0.01 and <0.001), while significant increase in HR was recorded following intubation in the control group [Figure 2] (P<0.001). Similarly, a fall in MAP following dexmedetomidine injection in the D4 and D6 groups and increase in MAP above the baseline following intubation in the control group was recorded [Figure 3].
Figure 1.
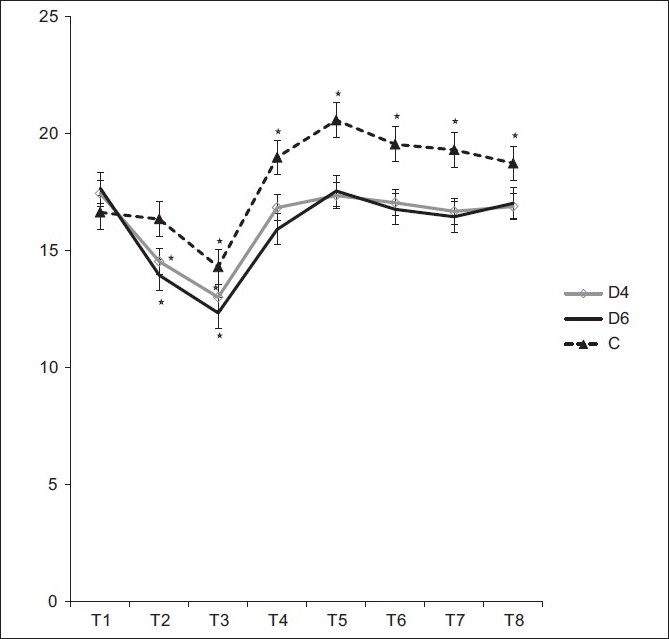
Changes in intraocular pressure in group D4, group D6 and group C. Measurements were recorded before premedication (T1), 5 mins after premedication (T2), 30 s after thiopental (T3), 30 s after suxamethonium (T4) and 1, 2, 4 and 6 mins after intubation (T5, T6, T7, T8). *P<0.001
Table 2.
Changes in intraocular pressure (mmHg)
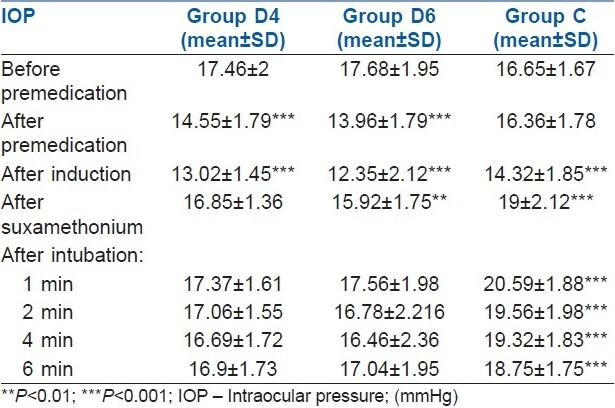
Figure 2.
Changes in heart rate in group D4, group D6 and group C. Measurements were recorded before premedication (T1), 5 mins after premedication (T2), 30 s after thiopental (T3), 30 s after suxamethonium (T4) and 1, 2, 4 and 6 mins after intubation (T5, T6, T7, T8). *P<0.001
Figure 3.
Changes in mean arterial pressure in group D4, group D6 and group C. Measurements were recorded before premedication (T1), 5 mins after premedication (T2), 30 s after thiopental (T3), 30 s after suxamethonium (T4) and 1, 2, 4 and 6 mins after intubation (T5, T6, T7, T8). *P<0.001
DISCUSSION
Patients with penetrating eye injury may present with full stomach. Goal of anaesthesia in this scenario is to secure the airway by the rapid sequence technique without increasing the IOP. Although rocuronium, an intermediate acting non-depolarising muscle relaxant, provides good intubating condition after 60–90 s, it is not preferred in patients with anticipated difficult airway.[10,11] Suxamethonium, the most commonly used muscle relaxant for rapid sequence airway management, increases the IOP. Different methods have been used to attenuate the effects of suxamethonium on IOP with variable success rates.[12] The alpha-2 agonist, clonidine, has proved its efficacy in preventing rise of IOP by suxamethonium.[13,14]
Dexmedetomidine, a highly selective alpha-2 adrenergic agonist, was approved by the Food and Drug Administration and introduced into clinical practice as an intensive care unit sedative and anaesthesia adjuvant in 1999.[15] Later on, it has been established that dexmedetomidine infusion produces ocular hypotension in rabbits with normal and elevated IOP.[16] Based on this observation, the present study was designed to attenuate suxamethonium-induced rise of IOP by dexmedetomidine premedication.
The effect of dexmedetomidine on the IOP may be due to its direct vasoconstrictor effect on the afferent blood vessels of the ciliary body leading to reduction of aqueous humour production.[17] It may also facilitate the drainage of aqueous humour by reducing sympathetically mediated vasomotor tone of the ocular drainage system.[16] Finally, the haemodynamic effect of dexmedetomidine can be responsible for reduction of IOP.[18]
The dosage of dexmedetomidine (0.4 μg/kg and 0.6 μg/kg) premedication used in the present study was based on a previous trial.[9] They used 0.6 μg/kg of dexmedetomidine and observed significant fall of IOP. Higher doses of dexmedetomidine were associated with episodes of hypotension and bradycardia without further decrease in IOP.[19,20]
Reduction in IOP was noticed in this series following administration of dexmedetomidine in both groups (Gr D4 and Gr D6), which was again increased after administration of suxamethonium and intubation. However, it still remained less than the baseline value. Similar observations were recorded in a previous trial using 0.6 μg/kg of dexmedetomidine.[9] None of the previous workers used 0.4 μg/kg of dexmedetomidine in their series and hence related data is not available. Fall in IOP by 0.4 μg/kg and 0.6 μg/kg of dexmedetomidine was comparable in this series. Hence, both the doses are equally effective in attenuating the rise of IOP by suxamethonium and intubation.
Dexmedetomidine premedication also produced significant fall in arterial pressure and HR. Fall in MAP was more in the D6 group as compared with the D4 group. Two patients in Group D6 developed hypotension, treated by phenylephrine, and were excluded from the study. Hence, patients who received 0.4 μg/kg dexmedetomidine were haemodynamically more stable.
The present series also observed significant attenuation of pressure response related to laryngoscopy and intubation, which supports the statements made by previous workers.[21,22]
Thus, dexmedetomidine prevents the rise of IOP due to suxamethonium injection and intubation. However, haemodynamic stability is better maintained with a lower dose (0.4 μg/kg) of dexmedetomidine. Hence, use of dexmedetomidine premedication 0.4 μg/kg is desirable for prevention of rise in IOP.
CONCLUSION
Dexmedetomidine prevents the rise in IOP associated with suxamethonium and intubation. Therefore, it should be used as a premedication before suxamethonium injection, where raised IOP is detrimental for patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Durant NN, Katz RL. Suxamethonium. Br J Anaesth. 1982;54:195–208. doi: 10.1093/bja/54.2.195. [DOI] [PubMed] [Google Scholar]
- 2.Edmondson L. Intraocular pressure and suxamethonium. Br J Anaesth. 1997;79:146. doi: 10.1093/bja/79.1.146. [DOI] [PubMed] [Google Scholar]
- 3.Chidiac EJ, Raiskin AO. Succinylcholine and the open eye. Ophthalmol Clin North Am. 2006;19:279–85. doi: 10.1016/j.ohc.2006.02.015. [DOI] [PubMed] [Google Scholar]
- 4.Abdalla MI, AI Mansouri F, Bener A. Dexmedetomidine during local anesthesia. J Anesth. 2006;20:54–6. doi: 10.1007/s00540-005-0351-z. [DOI] [PubMed] [Google Scholar]
- 5.Lee YY, Wong SM, Hung CT. Dexmedetomidine infusion as a suplement to isoflurane anaesthesia for vitreoretinal surgery. Br J Anaesth. 2007;98:477–83. doi: 10.1093/bja/aem040. [DOI] [PubMed] [Google Scholar]
- 6.Wunsch H, Kahn JM, Kramer AA, Wagener G, Li G, Sladen RN, et al. Dexmedetomidine in the care of critically ill patients from 2001 to 2007: An observational cohort study. Anesthesiology. 2010;113:386–94. doi: 10.1097/ALN.0b013e3181e74116. [DOI] [PubMed] [Google Scholar]
- 7.Chen BS, Peng H, Wu SN. Dexmedetomidine, an α2 adrenergic agonist, inhibits neuronal delayed-rectifier potassium current and sodium current. Br J Anaesth. 2009;103:244–54. doi: 10.1093/bja/aep107. [DOI] [PubMed] [Google Scholar]
- 8.Reves JG, Peter SA, Lubarsky DA, Mcevoy MD, Ruiz RM. Intravenous Anesthetics. In: Miller RD, editor. Miller's Anesthesia. 7th Ed. Vol. 1. Philadelphia: Churchill Livingstone Elsevier; 2010. pp. 751–7. [Google Scholar]
- 9.Mowafi HA, Aldossary N, Ismail SA, Alquahtani J. Effect of dexmedetomidine premedication on the intraocular pressure changes after succinylcholine and intubation. Br J Anaesth. 2008;100:485–9. doi: 10.1093/bja/aen020. [DOI] [PubMed] [Google Scholar]
- 10.Abou-Arab MH, Heier T, Caldwell JE. Dose of alfentanil needed to obtain optimal intubation conditions during rapid-sequence induction of anaesthesia with thiopentone and rocuronium. Br J Anaesth. 2007;98:604–10. doi: 10.1093/bja/aem064. [DOI] [PubMed] [Google Scholar]
- 11.Molina AL, de Boer HD, Klimek M, Heeringa M, Klein J. Reversal of rocuronium induced (1.2 mg kg–1) profound neuromuscular block by accidental high dose of sugammadex (40 mg kg–1) Br J Anaesth. 2007;98:624–7. doi: 10.1093/bja/aem057. [DOI] [PubMed] [Google Scholar]
- 12.Ghignone M, Noe C, Calvillo O, Quintin L. Anesthesia for ophthalmic surgery in elderly; the effects of clonidine on intraocular pressure, perioperative hemodynamics and anesthetic requirements. Anesthesiology. 1988;68:707–16. [PubMed] [Google Scholar]
- 13.Polarz H, Bohrer H, Martin E, Wolfrum J, Volcker HE. Oral clonidine premedication prevents the rise in intraocular pressure following succinylcholine administration. Ger J Ophthalmol. 1993;2:97–9. [PubMed] [Google Scholar]
- 14.Kumar A, Bose S, Bhattacharya A, Tandon OP, Kundra P. Oral clonidine premedication for elderly patients undergoing intraocular surgery. Acta Anaesthesiol Scand. 1992;36:159–64. doi: 10.1111/j.1399-6576.1992.tb03444.x. [DOI] [PubMed] [Google Scholar]
- 15.Gertler R, Brown C, Mitchell DH, Silvius EN. Dexmedetomidine: A novel sedative analgesic agent. Baylor University Medical Center Proceedings. 2001;14:13–21. doi: 10.1080/08998280.2001.11927725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vartianinen J, MacDonald E, Urtti A, Ronhiainen H, Virtanen R. Dexmedetomidine induced ocular hypotension in rabbits with normal or elevated intraocular pressure. Invest Ophthalmol Vis Sci. 1992;33:2019–23. [PubMed] [Google Scholar]
- 17.Macri FJ, Cervario SJ. Clonidine. Arch Ophthalmol. 1978;96:2111–3. doi: 10.1001/archopht.1978.03910060491022. [DOI] [PubMed] [Google Scholar]
- 18.Georgiou M, Parlapani A, Argiriadou H, Papagiannopoulou P, Katsikis G, Kaprini E. Sufentanil or clonidine for blunting the increase in intraocular pressure during rapid sequence induction. Eur J Anaesthesiol. 2002;13:519–22. doi: 10.1017/s0265021502001321. [DOI] [PubMed] [Google Scholar]
- 19.Virkkila M, Ali-Melkkila T, Konto J, Turuner J, Scheinin H. Dexmedetomidine as intramuscular premedication for day case cataract surgery.A comparative study of dexmedetomidine, midazolam and placebo. Anaesthesia. 1994;49:853–8. doi: 10.1111/j.1365-2044.1994.tb04257.x. [DOI] [PubMed] [Google Scholar]
- 20.Virkkila M, Ali-Melkkila T, Konto J, Turuner J, Scheinin H. Dexmedetomidine as intramuscular premedication in outpatient cataract surgery: A placebo-controlled dose ranging study. Anaesthesia. 1993;4:482–7. doi: 10.1111/j.1365-2044.1993.tb07066.x. [DOI] [PubMed] [Google Scholar]
- 21.Ozkose Z, Demir FS, Pampal K, Yardim S. Hemodynamic and anesthetic advantages of dexmedetomidine, an alpha-2 agonist for surgery in prone position. Tohoku J Exp Med. 2006;210:153–60. doi: 10.1620/tjem.210.153. [DOI] [PubMed] [Google Scholar]
- 22.Yildiz M, Tavlan A, Tuncer S, Reisli R, Yosunkaya A, Otelcioglu S. Effect of dexmedetomidine on haemodynamic responses to laryngoscopy and intubation, perioperative haemodynamics and anaesthetic requirements. Drugs R D. 2006;7:43–52. doi: 10.2165/00126839-200607010-00004. [DOI] [PubMed] [Google Scholar]


