Abstract
Context:
Blood culture is routinely taken at the time of admission to the intensive care unit (ICU) for patients suspected to have infection. We undertook this study to determine the incidence of bacteremia at the time of ICU admission and to assess its impact on the outcome.
Methods:
Retrospective cohort study from all the admissions in ICU, in whom blood cultures sent at the time of admission were analyzed. Data regarding patient demographics, probable source of infection, previous antibiotic use and ICU course was recorded. Severity of illness on admission was assessed by acute physiology and chronic health evaluation II score.
Statistical Analysis:
Qualitative data were analyzed using Chi-square or Fisher Exact test and quantitative data were analyzed using Student's t-test. Primary outcome measure was ICU mortality.
Results:
Of 567 patients, 42% patients were on antibiotics. Sixty-four percent of the patients were direct ICU admission from casualty, 10.76% were from wards and 6.17% from other ICUs, and 19.05% were transfers from other hospitals. Blood cultures were positive in 10.6% patients. Mortality was significantly higher in patients with positive blood cultures (45% vs. 13.6%; P=0.000). On univariate analysis, only previous antibiotic use was statistically associated with higher mortality (P=0.011). Bacteremic patients who were already on antibiotics had a significantly higher mortality (OR 12.9, 95% CI: 1.6–100).
Conclusions:
Blood cultures may be positive in only minority of the patients with suspected infection admitted to ICU. Nevertheless, the prognosis of those patients with positive blood culture is worse, especially if culture is positive in spite of the patient being on antibiotics.
Keywords: Blood stream infection, ICU admission bacteremia, multiorgan dysfunction, risk factors for bacteremia
INTRODUCTION
Bloodstream infection (BSI) is a severe, life-threatening condition, especially in critically ill patients. In recent years, incidence of BSI in patients admitted to intensive care units (ICU) has increased due to increased use of invasive devices and immunosuppressive therapy.[1,2] Presently, nosocomial BSI has been reported to be among the most frequently encountered nosocomial infections in the ICU.[3–5] According to an estimate, community-acquired BSI accounts for 20% of all ICU admissions and 28% of all BSI diagnosed in the ICU.[6,7] Besides increasing incidence, BSIs also have been shown to be associated with increased treatment costs, length of stay and mortality.[8] The case-fatality rate from bacteremic sepsis causing organ dysfunction ranges from 30% to 50%, and attributable mortality of up to 35% has been associated with BSI.[8,9] Delay in treatment and inappropriate antimicrobial treatment are important factors that can influence the outcome of patients admitted to the ICU with BSI. This may be especially true for those patients admitted with severe sepsis or septic shock.[7,10,11]
Numerous studies have been carried out to assess the implications and risk factors for nosocomial BSI and several factors, including age of patient, severity of illness, length of ICU stay, presence of invasive catheters and red blood cell transfusions, have been shown to independently predict mortality.[4,5,8,12,13] However, there is dearth of data regarding the implications and risk factors for BSI present at the time of ICU admission. As blood culture is routinely taken at the time of admission to ICU for all patients suspected to have infection, even though it may be positive only in a few patients, we attempted to determine the incidence of bacteremia at the time of ICU admission, to assess its impact on the outcome and to analyze the risk factors that are related to poorer outcomes.
METHODS
We conducted a retrospective cohort study in an eight-bed medical ICU of a tertiary care hospital. Data from all the ICU admissions with suspected sepsis in which blood cultures were sent at the time of admission were analyzed over a 2-year period from June 2008 to May 2010. The patients were divided into two groups depending on the positivity of their blood cultures. The patients with positive blood cultures representing clinically significant BSI were included in the positive blood culture group.[12]
The inclusion criteria were:
Clinically significant BSI was deemed to be present if a pathogenic organism was cultured from at least one set of blood cultures.
At least two positive sets of blood cultures were required to diagnose a BSI with common skin contaminants including coagulase negative staphylococci, or Bacillus, Corynebacterium or Propionibacterium species, and the patient has at least one of the signs and symptoms of sepsis (fever [>38°C], chills or rigors and hypotension) within 24 h of a positive blood culture being collected.
The exclusion criteria were:
The patients whose medical records were incomplete in terms of previous antibiotics usage and whose blood cultures were not sent at the admission.
The blood cultures which did not fit the above-mentioned definition of clinically significant BSI.
The data regarding patient demographics, probable source of infection, previous antibiotics and ICU course (need for inotropic support, renal replacement therapy or mechanical ventilation) and microbiology report of positive blood culture were recorded. The severity of illness on admission was assessed by Acute Physiology and Chronic Health Evaluation (APACHE) II score. The primary aim of the study was to determine the incidence of bacteremia in the patients admitted into ICU and impact of clinically significant positive blood culture on patients’ survival in the ICU. The secondary measures were to determine the risk factors of admission bacteremia and effect of admission bacteremia on organ support (need of inotropes/vasopressors, renal replacement therapy and mechanical ventilation).
Statistical analysis
We used SPSS version 14.0 (SPSS Inc., Chicago, IL, USA) for the statistical analysis. Qualitative data were analyzed using Chi[2] square or Fisher Exact tests and quantitative data were analyzed using Student's t-test. Primary outcome measure was ICU mortality. Secondary outcome measures were organ support, which included requirement of inotropes, renal replacement therapy and mechanical ventilation.
RESULTS
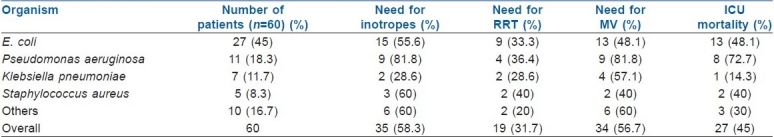
A total of 567 patients were included in the analysis. A significant proportion of these patients, 238/567 (42%), were already on antibiotics. Three hundred sixty-three (64%) patients were direct ICU admission from casualty, 61 (10.76%) were shifted from hospital wards, 35 (6.17%) from other ICUs in the hospital and 108 (19.05%) were transfers from the other hospitals. Blood cultures were positive only in 60 (10.6%) patients, which was consistent with significant BSI. The ICU mortality was significantly higher in patients with positive blood cultures (27/60, 45% vs. 69/507, 13.6%; P=0.000). Univariate analysis for assessing the risk factors for ICU mortality among bacteremic patients was done, in which age (P=0.061), sex (P=0.253), type of admission (P=0.203), type of organism, severity of illness (P=0.234) and site of infection (P=0.250), were analyzed, but only previous antibiotic use was statistically associated with higher mortality (P=0.011) [Table 1]. Bacteremic patients who were already on antibiotics had a significantly higher mortality (54.2% vs. 8.3%), (OR 12.9, 95% CI: 1.6–100). Mortality was higher in patients with pseudomonas bacteremia (72.7%), although it was not statistically significant (P=0.08) [Table 2].
Table 1.
Comparison of patient characteristics and their ICU course according to blood culture positivity
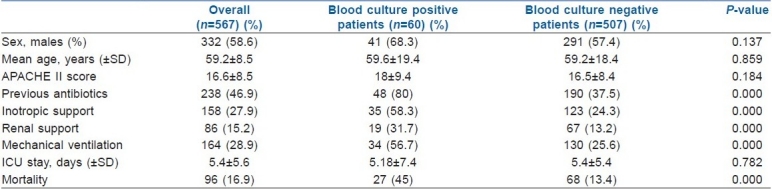
Table 2.
Organ support and ICU mortality according to the organism isolated in patients with positive blood cultures
DISCUSSION
Blood cultures are routinely taken from the patients who are admitted to ICU with suspected infection. The blood cultures may be positive not only in patients with primary BSI but also in patients with bacteremia with primary infection at some other site. However, the reported incidence of positive blood culture consistent with BSI in patients admitted to ICUs is low, and varies from 3.2% to 4.3%.[14] In our study, we found the incidence of positive blood cultures taken at the time of admission to the ICU to be 10.6%. Bacteremic sepsis remains associated with high morbidity and mortality in the critical care setting. We found that the ICU mortality was significantly higher in patients with BSI as compared with patients with negative blood cultures (45% vs. 13.6%). In addition, there was increased incidence of organ failure in bacteremic patients as evidenced by increased need for organ support.
Our study has shown a mortality rate of 45% in patients with BSI, which is well within the range of the reported crude mortality rate of 31.5–82.4% in such patients.[8,15–18] There are various factors that influence the outcome in patients with BSIs, like the type/source of bacteremia (primary vs. secondary) and place of acquisition (community versus nosocomial).[15,18,19] Higher mortality rates have been shown to be associated with secondary bacteremia (e.g., from an abdominal or pulmonary source) than with primary bacteremia.[15,18] Similarly, studies have reported significantly higher mortality rates in hospital-acquired BSI and health care-associated BSI as compared with community-acquired BSI.[19–21] A large multicentre American study reported a significantly higher mortality in patients with health care-associated (29%) or hospital-acquired BSI (37%) as compared with community-acquired BSI (16%).[19]
In our study, even though we observed a three-fold increase in mortality in bacteremic patients, there was no statistically significant difference in the APACHE II scores at admission between the bacteremic and non-bacteremic groups. Similarly, other researchers have also reported a higher mortality in bacteremic patients irrespective of their severity of illness at the time of ICU admission, as assessed by the APACHE II score.[22] This increased mortality seen with bacteremic sepsis may be due to the development of multiple organ dysfunctions, which is more often present in bacteremic patients. We found that there was a significantly increased need for organ support, as evidenced by increased requirement of vasopressors, mechanical ventilation and renal replacement therapy, in patients with positive blood cultures, which can be taken as a surrogate marker of organ dysfunction. There are several other studies that have shown that the risk of death after sepsis correlates with the number of organ dysfunctions.[23,24]
Even though the western literature have reported a higher incidence of gram positive bacteremia, our study showed a higher incidence of gram negative bacteremia, which is in accordance with the previously published Indian subcontinent data.[25] We found that Escherichia coli (45%) was the most common organism isolated, followed by Pseudomonas (18.3%) and Klebsiella (11.7%). In addition, we observed increased mortality in patients infected with Pseudomonas, which is in accordance with the other studies.[26,27] However, this increased mortality with Pseudomonas did not reach statistical significance in our patient cohort, which could be partially attributable to a small sample size.
On subgroup analysis, we found that those patients whose blood cultures were positive in spite of them being on antibiotics had a significantly higher mortality (54.2% vs. 8.3%). This could be partially explained by the use of inappropriate or under-dosing of antibiotics or infection with multidrug-resistant organisms. Several studies have shown that the early use of appropriate empirical antibiotic therapy is crucial for a better patient outcome.[7,28]
There are a few limitations of our study that need consideration. Firstly, besides the study's retrospective nature, our study was from a single centre. Therefore, our findings cannot be generalized and may not reflect widespread trends in the epidemiology of BSIs. Secondly, the study was performed in a medical ICU and, hence, may not be applicable to other types of critical care units. Finally, we did not classify the BSI into health care-associated BSI and community-acquired BSI as such information is mainly based on clinical history at presentation, which may not be completely authentic in a retrospective data.
Even though bacteremia may be present in a minority of patients at the time of ICU admission, surveillance of bacteremia is important as it may help in identifying patients at higher risk of morbidity or mortality during their ICU stay, recognizing the resistance patterns in the prevailing organisms, detecting changes in epidemiology and are essential to design future studies.
CONCLUSION
Blood cultures may be positive in only minority of the patients with suspected infection admitted to the ICU. Nevertheless, the prognosis of those patients with positive blood culture is worse, especially if the culture is positive in spite of the patient being on antibiotics.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Mnatzaganian G, Galai N, Sprung CL, Zitser-Gurevich Y, Mandel M, Ben-Hur D, et al. Increased risk of bloodstream and urinary infections in intensive care unit (ICU) patients compared with patients fitting ICU admission criteria treated in regular wards. J Hosp Infect. 2005;59:331–42. doi: 10.1016/j.jhin.2004.07.028. [DOI] [PubMed] [Google Scholar]
- 2.van der Kooi TI, de Boer AS, Mannien J, Wille JC, Beaumont MT, Mooi BW, et al. Incidence and risk factors of device-associated infections and associated mortality at the intensive care in the Dutch surveillance system. Intensive Care Med. 2007;33:271–8. doi: 10.1007/s00134-006-0464-3. [DOI] [PubMed] [Google Scholar]
- 3.Vincent JL, Bihari DJ, Suter PM, Bruining HA, White J, Nicolas-Chanoin MH, et al. The prevalence of nosocomial infection in intensive care units in Europe.Results of the European Prevalence of Infection in Intensive Care (EPIC) Study. EPIC International Advisory Committee. JAMA. 1995;274:639–44. [PubMed] [Google Scholar]
- 4.Garrouste-Orgeas M, Timsit JF, Tafflet M, Misset B, Zahar JR, Soufir L, et al. Excess risk of death from intensive care unit-acquired nosocomial bloodstream infections infections: A reappraisal. Clin Infect Dis. 2006;42:1118–26. doi: 10.1086/500318. [DOI] [PubMed] [Google Scholar]
- 5.Blot SI, Depuydt P, Annemans L, Benoit D, Hoste E, De Waele JJ, et al. Clinical and economic outcomes in critically ill patients with nosocomial catheter-related bloodstream infections. Clin Infect Dis. 2005;41:1591–8. doi: 10.1086/497833. [DOI] [PubMed] [Google Scholar]
- 6.Bourneton O, Mutel T, Heranney D, Hernandez C, Lavigne T, Waller J, et al. Incidence of hospital-acquired and community-acquired bloodstream infections in the University of Strasbourg Hospitals, France, between 2005 and 2007. Pathol Biol (Paris) 2010;58:29–34. doi: 10.1016/j.patbio.2009.07.028. [DOI] [PubMed] [Google Scholar]
- 7.Vallés J, Rello J, Ochagavía A, Garnacho J, Alcalá MA. Community-acquired bloodstream infection in critically ill adult patients: Impact of shock and inappropriate antibiotic therapy on survival. Chest. 2003;123:1615–24. doi: 10.1378/chest.123.5.1615. [DOI] [PubMed] [Google Scholar]
- 8.Pittet D, Tarara D, Wenzel RP. Nosocomial bloodstream infection in critically ill patients.Excess length of stay, extra costs, and attributable mortality. JAMA. 1994;271:1598–601. doi: 10.1001/jama.271.20.1598. [DOI] [PubMed] [Google Scholar]
- 9.Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: Analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–10. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Zaragoza R, Artero A, Camarena JJ, Sancho S, González R, Nogueira JM. The influence of inadequate empirical antimicrobial treatment on patients with bloodstream infections in an intensive care unit. Clin Microbiol Infect. 2003;9:412–418. doi: 10.1046/j.1469-0691.2003.00656.x. [DOI] [PubMed] [Google Scholar]
- 11.Artero A, Zaragoza R, Camarena JJ, Sancho S, González R, Nogueira JM. Prognostic factors of mortality in patients with community-acquired bloodstream infection with severe sepsis and septic shock. J Crit Care. 2010;25:276–81. doi: 10.1016/j.jcrc.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 12.Laupland KB, Zygun DA, Davies HD, Church DL, Louie TJ, Doig CJ. Population-based assessment of intensive care unit-acquired bloodstream infections in adults: Incidence, risk factors, and associated mortality rate. Crit Care Med. 2002;30:2462–7. doi: 10.1097/00003246-200211000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Elward AM, Fraser VJ. Risk factors for nosocomial primary bloodstream infection in pediatric intensive care unit patients: A 2-year prospective cohort study. Infect Control Hosp Epidemiol. 2006;27:553–60. doi: 10.1086/505096. [DOI] [PubMed] [Google Scholar]
- 14.Hugonnet S, Harbarth S, Ferrière K, Ricou B, Suter P, Pittet D. Bacteremic sepsis in intensive care: Temporal trends in incidence, organ dysfunction, and prognosis. Crit Care Med. 2003;31:390–4. doi: 10.1097/01.CCM.0000045026.81584.6F. [DOI] [PubMed] [Google Scholar]
- 15.Rello J, Ricart M, Mirelis B, Quintana E, Gurgui M, Net A, et al. Nosocomial bacteremia in a medical-surgical intensive care unit: Epidemiologic characteristics and factors influencing mortality in 111 episodes. Intensive Care Med. 1994;20:94–8. doi: 10.1007/BF01707661. [DOI] [PubMed] [Google Scholar]
- 16.Smith RL, Meixler SM, Simberkoff MS. Excess mortality in critically ill patients with nosocomial bloodstream infections. Chest. 1991;100:164–7. doi: 10.1378/chest.100.1.164. [DOI] [PubMed] [Google Scholar]
- 17.Forgacs IC, Eykyn SJ, Bradley RD. Serious infection in the intensive therapy unit: A 15-year study of bacteraemia. Q J Med. 1986;60:773–9. [PubMed] [Google Scholar]
- 18.Brun-Buisson C, Doyon F, Carlet J. Bacteremia and severe sepsis in adults: A multicenter prospective survey in ICUs and wards of 24 hospitals.French Bacteremia-Sepsis Study Group. Am J Respir Crit Care Med. 1996;154:617–24. doi: 10.1164/ajrccm.154.3.8810595. [DOI] [PubMed] [Google Scholar]
- 19.Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, et al. Health care-associated bloodstream infections in adults: A reason to change the accepted definition of community acquired infections. Ann Intern Med. 2002;137:791–7. doi: 10.7326/0003-4819-137-10-200211190-00007. [DOI] [PubMed] [Google Scholar]
- 20.Shorr AF, Tabak YP, Killian AD, Gupta V, Liu LZ, Kollef MH. Healthcare.associated bloodstream infection: A distinct entity? Insights from a large U.S. database. Crit Care Med. 2006;34:2588–95. doi: 10.1097/01.CCM.0000239121.09533.09. [DOI] [PubMed] [Google Scholar]
- 21.Vallés J, Calbo E, Anoro E, Fontanals D, Xercavins M, Espejo E, et al. Bloodstream infections in adults: Importance of healthcare-associated infections. J Infect. 2008;56:27–34. doi: 10.1016/j.jinf.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 22.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: A severity of disease classification. Crit Care Med. 1985;13:818–29. [PubMed] [Google Scholar]
- 23.Hebert PC, Drummond AJ, Singer J, Bernard GR, Russell JA. A simple multiple system organ failure scoring system predicts mortality of patients who have sepsis syndrome. Chest. 1993;104:230–5. doi: 10.1378/chest.104.1.230. [DOI] [PubMed] [Google Scholar]
- 24.Fagon JY, Chastre J, Novara A, Medioni P, Gibert C. Characterization of intensive care unit patients using a model based on the presence or absence of organ dysfunctions and/or infection: The ODIN model. Intensive Care Med. 1993;19:137–44. doi: 10.1007/BF01720528. [DOI] [PubMed] [Google Scholar]
- 25.Singhi S, Ray P, Mathew JL, Jayashree M, Dhanalakshmi Nosocomial bloodstream infection in a pediatric intensive care unit. Indian J Pediatr. 2008;75:25–30. doi: 10.1007/s12098-008-0002-0. [DOI] [PubMed] [Google Scholar]
- 26.Bhat S, Fujitani S, Potoski BA, Capitano B, Linden PK, Shutt K, et al. Pseudomonas aeruginosa infections in the Intensive Care Unit: Can the adequacy of empirical beta-lactam antibiotic therapy be improved? Int J Antimicrob Agents. 2007;30:458–62. doi: 10.1016/j.ijantimicag.2007.05.022. [DOI] [PubMed] [Google Scholar]
- 27.Tam VH, Rogers CA, Chang KT, Weston JS, Caeiro JP, Garey KW. Impact of multidrug-resistant Pseudomonas aeruginosa bacteremia on patient outcomes. Antimicrob Agents Chemother. 2010;54:3717–22. doi: 10.1128/AAC.00207-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ibrahim EH, Sherman G, Ward S, Fraser VJ, Kollef MH. The influence of inadequate antimicrobial treatment of bloodstream infections on patient outcomes in the ICU setting. Chest. 2000;118:146–55. doi: 10.1378/chest.118.1.146. [DOI] [PubMed] [Google Scholar]


