Abstract
Objective
This study examined differences in treatment rates for substance use disorders (SUD) among White, Black, Hispanic, Asian, Native American/Alaskan Native, and Native Hawaiian/Pacific Islander adolescents.
Method
Eight years of cross-sectional data (2001–2008) were pooled from the National Survey on Drug Use and Health to derive a nationally representative sample of 144,197 adolescents (age 12–17); 12,634 adolescents were identified with SUD in the previous year. Weighted probit regressions were estimated with year fixed effects to examine whether racial/ethnic minorities had lower rates of treatment in: (1) any setting, (2) medical settings (i.e. hospital, rehabilitation facility, mental health clinic, and/or doctor’s office), and (3) self-help programs. Initial models controlled for demographics and health status. Additional models further adjusted for family income and health insurance status.
Results
Among adolescents with SUD, unadjusted treatment rates ranged from 8.4% among Blacks to 23.5% among Native Hawaiian/Pacific Islanders. After adjusting for demographics and health status, Blacks (RD= −3.9%, 95% CI= −6.4%,−1.3%) and Hispanics (RD= −2.3%, 95% CI= −4.1%,−0.4%) were significantly less likely to receive SUD treatment than Whites (adjusted treatment rate 10.7%). These differences were exacerbated after adjusting for family income and insurance status. Lower treatment rates for Black and Hispanic adolescents persisted when examining SUD treatment rates in medical settings and self-help programs. Treatment rates for other racial/ethnic groups did not generally differ from Whites.
Conclusion
Results highlight exceptionally low treatment rates for SUD among all adolescents, with Blacks and Hispanics experiencing the lowest treatment rates across all racial/ethnic groups.
Keywords: race, ethnicity, substance use treatment, adolescents
INTRODUCTION
Substance use disorders (SUD) are common among adolescents and associated with detrimental consequences across the life course including lower educational attainment,1,2 poorer employment outcomes,2,3 increased involvement with the criminal justice system,1 suicide attempts, and completed suicides.4 Among those between the ages of 12 and 17, approximately 5% of adolescents abused or were dependent upon alcohol and 4% abused or were dependent upon illicit drugs in 2008.5 Yet, although treatments have been shown to improve a number of behavioral and psychological outcomes for adolescents with SUD,6–8 treatment rates are exceptionally low among the adolescent population.9 Only 7% of adolescents in need of SUD treatment received specialty treatment in 2008, which is lower than the percentage of adults in need of SUD services who received specialty treatment (11%).5,10 Consequently, it is important to identify key factors that impede adolescent treatment for SUD. A recent review of the literature explicitly called for nationally representative studies to examine the role of race/ethnicity in SUD treatment among youth.9
When examining mental health (MH) service use among adolescents, research has revealed that race/ethnicity is one of the most important factors associated with the receipt of treatment. Studies have documented substantially lower rates of MH service use among Black, Hispanic, and Asian adolescents compared to their White counterparts.11–13 Less is known, however, about the role of race/ethnicity in the receipt of treatment for SUD among adolescents. Although bivariate analyses have found that Black adolescents with SUD are significantly less likely to receive specialty treatment than Whites,9 and multivariate studies have reported that non-Whites are less likely to receive treatment for drug and alcohol problems relative to Whites,14,15 no known study has assessed differences in SUD treatment among adolescents across multiple racial/ethnic groups using a multivariate approach to account for differences in sociodemographic characteristics and health status.
To address this gap in the literature, we pooled eight years of a large nationally representative dataset to conduct the first comprehensive study of racial/ethnic differences in SUD treatment among White, Black, Hispanic, Asian, Native American/Alaskan Natives, Native Hawaiian/Pacific Islanders, and multiracial adolescents. We identify a sample of adolescents who were dependent upon or abused alcohol and/or illicit drugs within the past 12 months. Using probit regressions, we examine racial/ethnic differences in the receipt of any SUD treatment, the receipt of treatment in medical settings, and the receipt of self-help treatment.
METHOD
Data
Eight years of data (2001–2008) were pooled from the National Survey of Drug Use and Health (NSDUH), which is an annual, nationally representative, cross-sectional survey that is sponsored by the Substance Abuse and Mental Health Services Administration (SAMHSA). NSDUH samples noninstitutionalized individuals in the U.S. civilian population who are at least 12 years of age from all 50 states and the District of Columbia in multiple stages. The survey was administered in English and Spanish.
Study Sample
The analytic sample was derived from a subsample of adolescents who experienced SUD in the past year. NSDUH administers a module using computer-assisted interviewing (CAI) instrumentation to measure dependence and abuse of alcohol and illicit drugs using DSM-IV criteria. For marijuana, hallucinogens, inhalants, and tranquilizers, dependence was defined as having three or more of six standard dependence criteria. For alcohol, pain relievers, cocaine, heroin, sedatives, and stimulants, a seventh withdrawal criterion was added and a respondent was defined as having dependence if he/she had three or more of the seven dependence criteria. For alcohol and each illicit drug, a respondent was classified as having abused that substance if he/she met one or more of four abuse criteria (e.g. serious problems at home, work, or school caused by the substance) and was not dependent on that particular substance.16 A study cosponsored by SAMHSA and the National Institute on Drug Abuse to evaluate the validity of self-reported data on drug use in NSDUH found that most youth (age 12 to 17) and young adults (age 18 to 25) reported their drug use accurately;17 evidence is mixed, however, about whether the accuracy of self-reported data on drug use differs across racial/ethnic groups among adolescents.18,19
Of the 144,197 adolescents who participated in the NSDUH between 2001 and 2008, 12,630 (8.8%) adolescents experienced SUD in the past year. When examining the weighted prevalence of SUD by race/ethnicity, 9.3% of Whites were dependent upon or abused substances within the past year, compared to 8.3% of Hispanics, 5.0% of Blacks, 3.7% of Asians, 17.4% of Native Americans/Alaskan Natives, 7.1% of Native Hawaiians/ Pacific Islanders, and 9.9% of multiracial adolescents. Relative to Whites, results from adjusted Wald tests indicated that the prevalence of SUD is significantly lower among Hispanics (p=0.003), Blacks (p<0.001), Asians (p<0.001), and Native Hawaiians/ Pacific Islanders (p=0.048); the prevalence is significantly greater among Native American/Alaskan Natives (p<0.001).
Measures
Treatment for Substance Abuse/Dependence
After answering questions about substance use, adolescents were asked whether they received any treatment or counseling in the past 12 months for their use of alcohol or any drug, not counting cigarettes. After this initial question, adolescents were asked about the setting(s) in which they received treatment. We derived three dichotomous indicators to assess whether, in the past year, the adolescent received: (1) any treatment for SUD; (2) treatment in a medical setting for SUD other than an emergency room (i.e. treatment in a hospital, alcohol or drug rehabilitation facility, MH clinic, and/or doctor’s office); and (3) treatment in a self-help group for SUD. The last measure was derived from a question in which adolescents were asked if they received treatment for SUD “in a self-help group such as Alcoholics Anonymous or Narcotics Anonymous?” We examine self-help treatment in addition to treatment in medical settings because research has shown that the 12-step approach employed by Alcoholics Anonymous and Narcotics Anonymous is effective at reducing substance use and improving outcomes among adolescents.20
Race/Ethnicity
Race/ethnicity is assessed with seven mutually exclusive categories: White, Black, Hispanic, Native American/Alaskan Native, Asian, Native Hawaiian/Pacific Islander, and more than one race (i.e. multiracial). These categories were determined by assigning priority for any mention of Hispanic ethnicity.
Sociodemographic and Health Measures
Sociodemographics are assessed with a continuous measure of age in years (12–17), an indicator for females, an indicator for family status identifying adolescents who live with two parents versus those who do not, a categorical measure of family income (<$20K, $20K–$50K, $50K–$75K, >$75K), and a categorical measure of insurance status (any private insurance, public coverage [e.g. Medicare, Medicaid, military coverage], no insurance, and insurance unknown). General health status is measured with a dichotomous indicator of fair or poor self-reported health status versus good, very good, or excellent health. Two categorical measures assess the type of SUD. The first assesses alcohol abuse/dependence with three categories: (1) no alcohol abuse/dependence (omitted reference), (2) alcohol abuse, and (3) alcohol dependence. A second measure assesses illicit drug abuse/dependence with three categories: (1) no illicit drug abuse/dependence (reference); (2) illicit drug abuse; (3) illicit drug dependence.
Lastly, an indicator for past year MH treatment assesses the receipt of any treatment and counseling for problems with behaviors and emotions that were not caused by alcohol or drugs in the past 12 months. This measure may serve as a proxy for underlying MH problems as well as use of the behavioral health care system, which could facilitate the screening of and treatment for SUD given the high rate of comorbidity between MH problems and SUD in this population.21 No measures of specific MH problems such as depression or conduct disorder were consistently available in the years of data that were pooled for this analysis.
Data Analysis
We estimate pooled weighted probit regressions with the “svy” procedure in Stata to account for the complex survey design elements in NSDUH.22 Sampling weights adjust for differential probabilities of sampling selection, noncoverage bias, and nonresponse bias. All models include year fixed effects. Risk differences for racial/ethnic minorities are estimated at the weighted mean values of the covariates, which can be interpreted as the predicted difference in the percentage of adolescents in a racial/ethnic minority group who responded “yes” for the outcome variable (e.g. received any SUD treatment) compared to Whites holding the covariates constant at their mean. We excluded individuals with missing values on study variables (self-reported health [N=4]; receipt of past year MH treatment [N=148]) to yield an analytic sample for our regression analysis that comprises 12,478 adolescents with SUD.
The Institute of Medicine’s (IOM) report Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare defines a health care disparity as comprising, “differences in the quality of healthcare that are not due to access-related factors or clinical needs, preferences, and appropriateness of intervention.”23 Previous studies implementing this definition to examine MH care disparities have argued that access-related factors such as socioeconomic status (SES) and health insurance status should not be accounted for when estimating the total disparity in service use, but may be included in subsequent models to assess the degree to which they help explain the disparity.11,24 We estimate three models for each outcome measure to implement this definition in a manner consistent with prior research. First, we adjust for factors that may be associated with preferences for service use and/or differences in underlying health status – age, gender, family status, fair/poor health status, and type of SUD. Second, we adjust for the receipt of MH treatment in the past year. This measure may proxy for underlying MH problems as well as utilization of the behavioral health care system that may facilitate the treatment for SUD. The third model includes measures of health insurance status and family income to assess the extent to which these access-related variables account for the racial/ethnic differences in service use estimated in the previous model.
RESULTS
Treatment rates varied considerably across racial/ethnic groups (Table 1). When examining the receipt of any SUD treatment, treatment rates ranged from 8.4% among Blacks to 23.5% among Native Hawaiian/Pacific Islanders. Adjusted Wald tests indicated that Blacks and Hispanics were significantly less likely than Whites to receive any SUD treatment (p<0.05), treatment in a medical setting (p<0.01), and in a self-help group (p<0.05). Relative to Whites, the overall treatment rates were considerably higher among Native Hawaiian/Pacific Islanders and Native American/Alaskan Natives, but not statistically significant.
Table 1.
Weighted descriptive statistics for pooled sample of U.S. adolescents with past year substance abuse/dependence (2001–2008)
| Total (N=12,634) | Whites (N=8,506) | Blacks (N=1,051) | Hispanics (N=2,004) | Nat Amer./ Alas Native (N=325) | Asians (N=181) | Nat Haw. / Pac. Islander (N=68) | Multiracial (N=499) | |
|---|---|---|---|---|---|---|---|---|
| %/Mean (SE) | %/Mean (SE) | %/Mean (SE) | %/Mean (SE) | %/Mean (SE) | %/Mean (SE) | %/Mean (SE) | %/Mean (SE) | |
| Treatment for Substance Use Disorders | ||||||||
| Any treatment | 11.4 | 11.9 | 8.4 *** | 9.8 * | 18.2 | 11.0 | 23.5 | 15.6 |
| Treatment in a Medical Setting | 6.7 | 7.5 | 4.4 ** | 4.2 *** | 11.6 | 5.6 | 18.9 | 6.9 |
| Specialty Treatment | 6.0 | 6.6 | 4.0 * | 3.8 *** | 11.5 | 5.6 | 15.5 | 6.1 |
| Treatment in a Doctor’s Office | 1.7 | 2.0 | 0.9 ** | 0.8 *** | 0.2 *** | 1.9 | 13.3 | 1.2 |
| Self-help Treatment | 4.7 | 5.0 | 2.9 ** | 3.5 * | 10.3 | 4.8 | 14.8 | 6.8 |
| Explanatory Variables | ||||||||
| Demographics | ||||||||
| Age | 15.65 (0.01) | 15.69 (0.02) | 15.52 (0.05) *** | 15.57 (0.05) ** | 15.43 (0.12) ** | 15.77 (0.13) | 15.30 (0.23) | 15.65 (0.08) |
| Female | 50.1 | 51.9 | 45.0 ** | 45.8 *** | 48.9 | 45.8 | 51.9 | 52.7 |
| Lives with Two Parents | 63.5 | 68.4 | 32.4 *** | 60.1 *** | 48.3 *** | 81.0 *** | 54.6 | 60.6 * |
| Type of Substance Use Disorders | ||||||||
| Alcohol dependence (0/1) | 24.8 | 24.6 | 20.6 * | 26.9 | 35.6 ** | 21.1 | 23.8 | 27.9 |
| Alcohol abuse (0/1) | 42.2 | 44.9 | 26.2 *** | 40.6 * | 34.2 * | 37.2 | 40.0 | 42.5 |
| Illicit drug dependence (0/1) | 32.4 | 31.7 | 36.3 * | 31.6 | 30.8 | 37.4 | 39.7 | 43.4 ** |
| Illicit drug abuse (0/1) | 26.6 | 24.8 | 36.4 *** | 28.3 * | 32.3 | 18.3 | 24.4 | 30.3 |
| General and Mental Health Status | ||||||||
| Self-Rated Health Fair/Poor a | 6.4 | 5.6 | 8.4 ** | 7.9 ** | 8.2 | 9.0 | 10.8 | 8.7 |
| Received Any Mental Health Treatment b | 35.9 | 35.8 | 39.7 * | 34.4 | 37.4 | 29.6 | 30.7 | 42.3 |
| Family Income | ||||||||
| Income <20K | 17.2 | 11.0 | 39.8 *** | 27.7 *** | 44.5 *** | 16.9 | 21.2 | 22.3 ** |
| Income 20–50K | 34.6 | 31.9 | 40.6 *** | 42.2 *** | 38.6 | 34.6 | 36.1 | 28.7 |
| Income 50–75K | 18.7 | 21.1 | 12.4 *** | 13.1 *** | 7.7 *** | 20.9 | 22.9 | 18.4 |
| Income >75K | 29.5 | 36.0 | 7.2 *** | 17.0 *** | 9.2 *** | 27.6 | 19.8 ** | 30.6 |
| Insurance Coverage | ||||||||
| Uninsured | 8.2 | 6.1 | 7.3 | 16.8 *** | 9.2 | 14.4 | 14.7 | 5.2 |
| Private Insurance | 63.6 | 72.9 | 37.0 *** | 45.2 *** | 23.6 *** | 59.9 * | 51.9 * | 53.4 *** |
| Public Insurance | 26.5 | 19.6 | 53.9 *** | 36.7 *** | 55.3 *** | 25.1 | 33.3 | 37.5 *** |
| Other Insurance | 1.6 | 1.5 | 1.8 | 1.4 | 11.9 *** | 0.6 | 0.1 *** | 3.8 |
Notes: Results from adjusted Wald Tests compare measures between each racial/ethnic minority group and Whites.
N=12,630
N=12,482
p<0.05,
p<0.01,
p<0.001;
Blacks, Hispanics, Native American/Alaskan Natives, Native Hawaiian/Pacific Islanders, and multiracial adolescents were less likely to live with two parents (p<0.05), had significantly lower family incomes (p<0.05), and were less likely to have private health insurance (p<0.05) than whites. Although Asians did not differ from Whites in their levels of family income, they were less likely to have private health insurance (p<0.001).
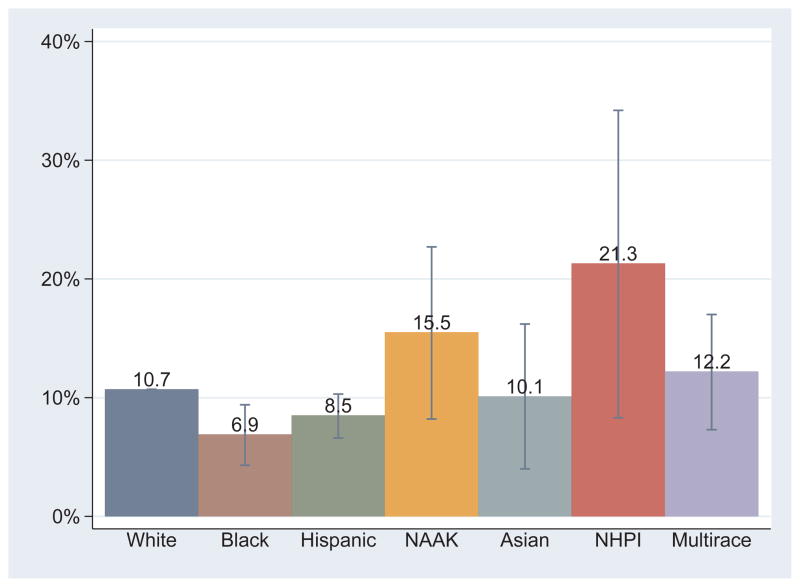
Multivariate results adjusting for demographics and health status (Table 2, Model 1) indicated that Blacks (RD=−3.9%, 95% CI −6.4%,−1.3%) and Hispanics (RD=−2.3%, 95% CI=−4.1%,−0.4%) were significantly less likely to receive any treatment for SUD relative to Whites. In other words, the adjusted percentages of those who received any SUD treatment were 6.9% for Blacks and 8.5% for Hispanics, compared to 10.7% for Whites (model-based prediction not shown). Other racial/ethnic groups, however, did not significantly differ from Whites in their likelihood of receiving any SUD treatment.
Table 2.
Racial/Ethnic Differences in the Receipt of Any Treatment for Substance Use Disorders among U.S. Adolescents
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| RD(%) | 95% CI | RD(%) | 95% CI | RD(%) | 95% CI | ||||
| Race/Ethnicitya | |||||||||
| Black | −3.9 | −6.4 | −1.3 | −3.8 | −6.3 | −1.2 | −4.2 | −6.8 | −1.6 |
| Hispanic | −2.3 | −4.1 | −0.4 | −2.1 | −3.9 | −0.2 | −2.7 | −4.5 | −0.8 |
| Native American/Alaskan Native | 4.7 | −2.6 | 12.0 | 4.8 | −2.3 | 11.8 | 3.9 | −2.9 | 10.6 |
| Asian | −0.6 | −6.7 | 5.5 | −0.3 | −6.4 | 5.7 | −0.7 | −6.7 | 5.3 |
| Native Hawaiian/Pacific Islander | 10.5 | −2.4 | 23.5 | 11.2 | −2.6 | 25.1 | 10.6 | −3.0 | 24.1 |
| Non-Hispanic >1 Race | 1.5 | −3.4 | 6.3 | 1.4 | −3.6 | 6.4 | 1.2 | −4.0 | 6.3 |
| Any Mental Health Treatment (1=yes) | 6.7 | 5.0 | 8.3 | 6.7 | 5.0 | 8.3 | |||
| Family Incomeb | |||||||||
| Income 20–50K | 1.5 | −0.9 | 3.9 | ||||||
| Income 50–75K | 0.7 | −2.4 | 3.8 | ||||||
| Income >75K | 1.3 | −1.6 | 4.1 | ||||||
| Insurance Coveragec | |||||||||
| Private Insurance | −3.3 | −6.6 | 0.0 | ||||||
| Public Insurance | 0.2 | −2.9 | 3.3 | ||||||
| Insurance Unknown | −3.9 | −8.6 | 0.8 | ||||||
Note: N=12,478. All models adjust for age, gender, family status, type of SUD, and self-rated health. Risk differences (RD) for race/ethnicity estimated at the mean values of the other model covariates.
Whites omitted
Family income <20K omitted
Uninsured omitted
After further adjusting for the receipt of any past year MH treatment, the risk differences for Blacks and Hispanics were slightly attenuated (Table 2, Model 2). Additionally, those who received MH treatment in the past year were significantly more likely to receive SUD treatment than those who had not received any MH treatment (RD= 6.7%, 95% CI=5.0%, 8.3%). Lastly, the inclusion of family income and health insurance status (Table 2, Model 3) resulted in an unexpected exacerbation of the risk differences for Blacks and Hispanics.
The model-based adjusted treatment rates for each racial/ethnic group are presented in Figure 1. Note that the difference between the height of the bar for each minority racial/ethnic group relative to Whites corresponds to the risk differences estimated in Model 1. Additionally, the 95% confidence interval for each risk difference is presented using lines and whiskers.
Figure 1.
Receipt of Treatment for Substance Use Disorder (SUD) by Race/Ethnicity among U.S. Adolescents. Note: N=12,478 adolescents with SUD. Results for figure derived from model-based prediction for Whites and risk differences for minority racial/ethnic groups estimated with probit model adjusting for demographics, type of SUD, and self-rated health. Lines and whiskers correspond to 95% Confidence Intervals for risk differences. NAAK = Native American/Alaskan Native; NHPI = Native Hawaiian/Pacific Islander
When examining racial/ethnic differences in the receipt of SUD treatment across settings, results from multivariate probit models yielded a similar pattern (Table 3). Turning first to medical settings, findings from Model 1 indicated that 6.4% of Whites received treatment for SUD in these settings during the year (model based prediction not shown), compared to 3.3% of Blacks (RD=−3.0%, 95% CI=−5.0%,−1.1%), and 3.2% of Hispanics (RD=−3.2%, 95% CI=−4.4%,−2.0%). Furthermore, these lower rates of treatment among Blacks and Hispanics were slightly attenuated after adjusting for past year MH treatment (Model 2), but slightly exacerbated after adjusting for family income and health insurance status (Model 3). Lastly, multiracial adolescents were significantly less likely to receive SUD treatment in medical settings relative to Whites in the fully adjusted model (RD=−2.2%, 95% CI=−4.0%,−0.3%).
Table 3.
Racial/Ethnic Differences in the Receipt of Medical Treatment for Substance Use Disorders among U.S. Adolescents
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| RD(%) | 95% CI | RD(%) | 95% CI | RD(%) | 95% CI | ||||
| Race/Ethnicitya | |||||||||
| Black | −3.0 | −5.0 | −1.1 | −2.8 | −4.7 | −0.9 | −3.3 | −5.1 | −1.6 |
| Hispanic | −3.2 | −4.4 | −2.0 | −2.9 | −4.1 | −1.8 | −3.3 | −4.4 | −2.1 |
| Native American/Alaskan Native | 2.8 | −3.9 | 9.6 | 2.8 | −3.6 | 9.2 | 1.7 | −3.9 | 7.3 |
| Asian | −1.6 | −5.7 | 2.6 | −1.3 | −5.3 | 2.6 | −1.5 | −5.4 | 2.3 |
| Native Hawaiian/Pacific Islander | 10.1 | −2.8 | 23.0 | 10.5 | −3.3 | 24.4 | 10.3 | −4.0 | 24.6 |
| Non-Hispanic >1 Race | −1.7 | −3.8 | 0.3 | −1.8 | −3.8 | 0.1 | −2.2 | −4.0 | −0.3 |
| Any Mental Health Treatment (1=yes) | 4.7 | 3.6 | 5.9 | 4.7 | 3.6 | 5.9 | |||
| Family Incomeb | |||||||||
| Income 20–50K | 1.9 | −0.1 | 3.9 | ||||||
| Income 50–75K | 0.5 | −1.7 | 2.8 | ||||||
| Income >75K | 1.0 | −1.3 | 3.2 | ||||||
| Insurance Coveragec | |||||||||
| Private Insurance | −0.8 | −3.2 | 1.7 | ||||||
| Public Insurance | 3.0 | 0.4 | 5.6 | ||||||
| Insurance Unknown | −2.3 | −5.4 | 0.8 | ||||||
Note: N=12,478. All models adjust for age, gender, family status, type of SUD, and self-rated health. Risk differences (RD) for race/ethnicity estimated at the mean values of the other model covariates.
Whites omitted
Family income <20K omitted
Uninsured omitted
Relative to Whites, Blacks and Hispanics were also less likely to receive SUD treatment in a self-help program (Table 4). The adjusted percentage of Whites who received SUD treatment in a self-help program is 4.1% (model-based prediction not show), compared to 2.0% of Blacks (RD=−2.1%, 95% CI=−3.1%,−1.0%) and 2.6% of Hispanics (RD=−1.5%; 95% CI=−2.4%,−0.5%). As in previous models, these differences were attenuated after adjusting for the receipt of past year MH treatment and exacerbated after adjusting for family income and health insurance status.
Table 4.
Racial/Ethnic Differences in the Receipt of Self-Help Treatment for Substance Use Disorders among U.S. Adolescents
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| RD(%) | 95% CI | RD(%) | 95% CI | RD(%) | 95% CI | ||||
| Race/Ethnicitya | |||||||||
| Black | −2.1 | −3.1 | −1.0 | −2.0 | −3.1 | −1.0 | −2.2 | −3.3 | −1.2 |
| Hispanic | −1.5 | −2.4 | −0.5 | −1.4 | −2.3 | −0.5 | −1.6 | −2.5 | −0.7 |
| Native American/Alaskan Native | 3.4 | −2.2 | 9.0 | 3.3 | −2.1 | 8.7 | 2.4 | −2.5 | 7.2 |
| Asian | 0.4 | −4.0 | 4.7 | 0.4 | −3.9 | 4.8 | 0.3 | −4.1 | 4.8 |
| Native Hawaiian/Pacific Islander | 7.7 | −4.3 | 19.7 | 8.1 | −4.5 | 20.7 | 7.7 | −4.7 | 20.1 |
| Non-Hispanic >1 Race | 0.6 | −2.4 | 3.5 | 0.5 | −2.5 | 3.5 | 0.4 | −2.6 | 3.4 |
| Any Mental Health Treatment (1=yes) | 1.7 | 0.8 | 2.7 | 1.7 | 0.8 | 2.7 | |||
| Family Incomeb | |||||||||
| Income 20–50K | 1.0 | −0.5 | 2.5 | ||||||
| Income 50–75K | 0.6 | −1.2 | 2.3 | ||||||
| Income >75K | 0.8 | −0.8 | 2.5 | ||||||
| Insurance Coveragec | |||||||||
| Private Insurance | −1.4 | −3.5 | 0.7 | ||||||
| Public Insurance | 0.6 | −1.4 | 2.6 | ||||||
| Insurance Unknown | −0.2 | −4.0 | 3.6 | ||||||
Notes: N=12,478. All models adjust for age, gender, family status, type of SUD, and self-rated health. Risk differences (RD) for race/ethnicity estimated at the mean values of the other model covariates.
Whites omitted
Family income <20K omitted
Uninsured omitted
To assess whether findings for Blacks and Hispanics were similar among those with more severe cases of SUD, we conducted sensitivity analyses by limiting the analytic sample to those with alcohol and/or illicit drug dependence. Dependence is more severe than abuse because it involves the psychological and physiological effects of tolerance and withdrawal. The lower rates of SUD treatment were even more pronounced for Blacks compared to Whites across all outcome measures when focusing on this subsample. Findings for Hispanics were similar for two of the outcome measures – the receipt of any treatment (p<0.10) and the receipt of treatment in medical settings (p<0.05). However, Hispanics did not differ from Whites in their likelihood of receiving treatment in self-help programs among those with substance dependence. Additional sensitivity analyses also revealed that findings for race/ethnicity were virtually unchanged when models adjusted for language of interview and population density.
DISCUSSION
The findings indicate exceptionally low rates of treatment for SUD among all adolescents, with Black and Hispanic adolescents experiencing the lowest rates of SUD treatment. The adjusted percentage of adolescents who received SUD treatment was 6.9% for Blacks and 8.5% for Hispanics, compared to 10.7% among Whites. These lower rates of SUD treatment for Black and Hispanic adolescents were evident both in the medical sector and in self-help programs.
Results also indicated that the lower SUD treatment rates for Blacks and Hispanics were slightly attenuated after adjusting for past year MH treatment, but exacerbated after adjusting for family income and insurance status. Although additional analyses (not shown) indicated that the adjusted rates of past year MH treatment did not differ among Blacks, Hispanics, and Whites in our sample, the attenuation of risk differences likely occurs because the receipt of MH treatment was more likely to correspond with the receipt of SUD treatment among Whites than among Blacks and Hispanics. The exacerbation of risk differences after adjusting for family income and insurance status was unexpected and differs from what is typically observed in the disparities literature.23 Further investigation of this finding indicated that this pattern likely occurred because Blacks and Hispanics were more likely to have public insurance than Whites, and those with public insurance were the most likely to receive SUD treatment. Thus, rather than acting as a mediator that partially explains the lower rates of treatment among Blacks and Hispanics, the exclusion of insurance status from the model suppresses the true size of the underlying difference in service use across these groups.
There are several unmeasured factors that may further explain the lower rates of treatment among Black and Hispanic adolescents. Minorities are more likely to live in socioeconomically disadvantaged communities25 that have fewer MH providers and physicians compared to higher SES communities.26–28 Furthermore, although sensitivity analyses adjusting for language of interview (English versus Spanish) did not account for any of the difference observed between Hispanics and Whites, it is possible that unmeasured differences in English proficiency of the adolescent’s parents could adversely affect the ability of Hispanic adolescents to navigate the system.29 Lastly, racial/ethnic differences in stigma, attitudes, and cultural health beliefs concerning behavioral health problems and treatment could partially explain the lower treatment rates observed for Black and Hispanic adolescents.12,30,31
Because the criminal justice system is one of the major sources of referral to treatment for adolescent substance abusers,32 it is important to assess its role in any observed racial/ethnic differences in SUD treatment. The survey design of NSDUH, however, focuses on the non-institutionalized population and therefore excludes adolescents currently in the juvenile justice system. Nevertheless, among sample respondents, NSDUH collects information about whether treatment was paid for by the court. Among the 240 adolescents in our sample for whom treatment was paid for by the court, bivariate analyses did not reveal any racial/ethnic differences in this measure. Future research should examine whether racial/ethnic differences in referral to SUD treatment by the court system -- irrespective of whether the court is the payer -- exacerbates or mitigates the lower treatment rates among Blacks and Hispanics. Future studies should also assess the extent to which lower rates of SUD treatment among Black and Hispanic adolescents contribute to their greater likelihood of being incarcerated for substance related charges in adulthood relative to Whites.
Asians, Native American/Alaskan Natives, and Native Hawaiian/Pacific Islanders did not differ significantly from Whites in their likelihood of receiving treatment for SUD. Although the adjusted SUD treatment rate was slightly lower among Asians (10.1%) relative to Whites (10.7%), it is noteworthy that the treatment rates for Native American/Alaskan Natives (15.5%) and Native Hawaiian/Pacific Islanders (21.3%) were substantially larger. The lack of statistical significance for these racial/ethnic groups may be a function of their smaller sample sizes, limiting the power to detect significant differences. Future studies that seek to understand determinants of SUD treatment among adolescents should consider oversampling these populations to elucidate this unexpected finding and inform future efforts to improve adolescent SUD treatment rates. If Native American/Alaskan Natives and Native Hawaiian/Pacific Islanders truly have the highest SUD treatment rates among adolescents, a more thorough understanding of the outreach programs, screening efforts, and treatment systems that serve these populations could shed light on effective mechanisms to improve SUD treatment among other racial/ethnic groups.
In addition to race/ethnicity, another important predictor of receiving SUD treatment is whether the adolescent received any MH treatment in the prior year. Adolescents with SUD who received any treatment for MH treatment in the prior year were approximately 60% more likely to receive SUD treatment than those who did not receive any MH treatment. This finding, which is consistent with previous research,33 highlights how the use of MH services may be a point of access and referral into substance use system, and vice versa. Yet, it is also noteworthy that 84% of the adolescents in our sample who received MH treatment in the prior year did not receive any SUD treatment, which represents a missed opportunity for improving the SUD treatment rate.
The exceptionally low rate of SUD treatment among all adolescents underscores a need for policies and interventions that improve screening and treatment efforts among this population across multiple settings. Because more than 90% of adolescents have a usual source of primary care,34 implementation of short validated screening instruments for SUD in primary care settings could help improve identification of adolescents in need of treatment.35,36 Furthermore, adolescents who currently receive MH treatment should also be targeted for improved screening efforts given that 84% of adolescents in our sample received MH treatment in the past year but did not receive any SUD treatment. Once adolescents with SUD have been identified, providers can work with their families to help decide which type of treatment setting would be most appropriate (e.g. inpatient, outpatient, self-help program).
To the extent that Black and Hispanic youth may be less likely to be seen in primary care settings or receive MH treatment,11–13,37 research has reported that school-based health centers could be a venue through which SUD can be screened and treated among low income, racial/ethnic minority adolescents.38 Additionally, educational outreach programs and interventions tailored for minority families in primary care and community settings should be explored as mechanisms to improve minority treatment rates for SUD.9
Several limitations are noted. First, we cannot establish causality in these relationships because the data are cross sectional. Second, there may be important subgroup differences in service use within the racial/ethnic groups that cannot be examined because there is no information about country/region of origin for Hispanics and Asians in the NSDUH public use data files. Third, because NSDUH was only conducted in English and Spanish, there is a selection bias against parents and youth with limited English and Spanish proficiency. To the extent that language may have been a barrier to SUD treatment for non-English and non-Spanish speaking populations, the risk differences estimated for Asians, Native Hawaiian/Pacific Islanders, and Native American/Alaskan Natives may have been biased upwards. Lastly, the NSDUH public use files do not include measures of several important mediators that could further explain these racial/ethnic differences in SUD treatment such as immigration status, health beliefs and attitudes concerning SUD treatment, and geographic access to providers.
In spite of these limitations, our study documents exceptionally low rates of SUD treatment among all adolescents, with Black and Hispanic adolescents experiencing the lowest treatment rates. Our study lays an important foundation for future research to collect the data necessary to further elucidate the barriers to treatment for each racial/ethnic group and better understand the sources of racial/ethnic differences in SUD service utilization. Future research should also examine the extent to which the lower rates of SUD treatment among Black and Hispanic adolescents translate into poorer developmental and social outcomes across the life course, such as an increased likelihood of arrests and incarcerations for substance related charges.
Acknowledgments
This work was supported by a National Institute of Mental Health grant (5K24MH075867-05).
The authors are grateful for the helpful comments and suggestions by Neetu Chawla at the National Cancer Institute and Michelle Ko at the University of California, Los Angeles School of Public Health.
Footnotes
Disclosure: Drs. Cummings and Druss, and Ms. Wen report no biomedical financial interests or potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hicks BM, Iacono WG, McGue M. Consequences of an adolescent onset and persistent course of alcohol dependence in men: adolescent risk factors and adult outcomes. Alcohol Clin Exp Res. 2010 May;34(5):819–833. doi: 10.1111/j.1530-0277.2010.01154.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Turnbull JE, George LK, Landerman R, Swartz MS, Blazer DG. Social outcomes related to age of onset among psychiatric disorders. J Consult Clin Psychol. 1990 Dec;58(6):832–839. doi: 10.1037//0022-006x.58.6.832. [DOI] [PubMed] [Google Scholar]
- 3.Kandel DB, Davies M, Karus D, Yamaguchi K. The consequences in young adulthood of adolescent drug involvement. An overview. Arch Gen Psychiatry. 1986 Aug;43(8):746–754. doi: 10.1001/archpsyc.1986.01800080032005. [DOI] [PubMed] [Google Scholar]
- 4.Brent DA. Risk factors for adolescent suicide and suicidal behavior: mental and substance abuse disorders, family environmental factors, and life stress. Suicide Life Threat Behav. 1995;25 (Suppl):52–63. [PubMed] [Google Scholar]
- 5.Substance Abuse and Mental Health Services Administration. Results from the 2008 National Survey on Drug Use and Health: National Findings. Rockville, MD: Office of Appiled Studies; 2009. [Google Scholar]
- 6.Catalano RF, Hawkins JD, Wells EA, Miller J, Brewer D. Evaluation of the effectiveness of adolescent drug abuse treatment, assessment of risks for relapse, and promising approaches for relapse prevention. Int J Addict. 1990 Aug;25(9A–10A):1085–1140. doi: 10.3109/10826089109081039. [DOI] [PubMed] [Google Scholar]
- 7.Hser YI, Grella CE, Hubbard RL, et al. An evaluation of drug treatments for adolescents in 4 US cities. Arch Gen Psychiatry. 2001 Jul;58(7):689–695. doi: 10.1001/archpsyc.58.7.689. [DOI] [PubMed] [Google Scholar]
- 8.Kaminer Y. Alcohol & drug abuse: adolescent substance abuse treatment: where do we go from here? Psychiatr Serv. 2001 Feb;52(2):147–149. doi: 10.1176/appi.ps.52.2.147. [DOI] [PubMed] [Google Scholar]
- 9.Alegria M, Carson NJ, Goncalves M, Keefe K. Disparities in treatment for substance use disorders and co-occurring disorders for ethnic/racial minority youth. J Am Acad Child Adolesc Psychiatry. 2011 Jan;50(1):22–31. doi: 10.1016/j.jaac.2010.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Substance Abuse and Mental Health Serivces Administration - Office of Applied Studies. The NSDUH Report: Treatment for Substance Use and Depression among Adults, by Race/Ethnicity. Rockville, MD: 2009. [Google Scholar]
- 11.Cummings JR, Druss BG. Racial/ethnic differences in mental health service use among adolescents with major depression. J Am Acad Child Adolesc Psychiatry. 2011 Feb;50(2):160–170. doi: 10.1016/j.jaac.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cummings JR, Ponce NA, Mays VM. Comparing racial/ethnic differences in mental health service use among high-need subpopulations across clinical and school-based settings. J Adolesc Health. 2010 Jun;46(6):603–606. doi: 10.1016/j.jadohealth.2009.11.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garland AF, Lau AS, Yeh M, McCabe KM, Hough RL, Landsverk JA. Racial and ethnic differences in utilization of mental health services among high-risk youths. Am J Psychiatry. 2005 Jul;162(7):1336–1343. doi: 10.1176/appi.ajp.162.7.1336. [DOI] [PubMed] [Google Scholar]
- 14.Wu P, Hoven CW, Fuller CJ. Factors associated with adolescents receiving drug treatment: findings from the National Household Survey on Drug Abuse. J Behav Health Serv Res. 2003 Apr–Jun;30(2):190–201. doi: 10.1007/BF02289807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu P, Hoven CW, Tiet Q, Kovalenko P, Wicks J. Factors associated with adolescent utilization of alcohol treatment services. Am J Drug Alcohol Abuse. 2002;28(2):353–369. doi: 10.1081/ada-120002978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.SAMHSA. National Survey on Drug Use and Health Codebook. United States Department of Health and Human Services. Substance Abuse and Mental Health Services Administration; 2008. [Google Scholar]
- 17.Harrison LD, Martin SS, Enev T, Harrington D. Comparing drug testing and self-report of drug use among youths and young adults in the general population. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2007. [Google Scholar]
- 18.Harris KM, Griffin BA, McCaffrey DF, Morral AR. Inconsistencies in self-reported drug use by adolescents in substance abuse treatment: Implications for outcome and performance measurements. Journal of Substance Abuse Treatment. 2008;34(3):347–355. doi: 10.1016/j.jsat.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fendrich M, Soo Kim JY. Multiwave analysis of retest artifact in the National Longitudinal Survey of Youth drug use. Drug and Alcohol Dependence. 2001;62:239–253. doi: 10.1016/s0376-8716(00)00177-0. [DOI] [PubMed] [Google Scholar]
- 20.Winters KC, Stinchfield RD, Opland E, Weller C, Latimer WW. The effectiveness of the Minnesota Model approach in the treatment of adolescent drug abusers. Addiction. 2000 Apr;95(4):601–612. doi: 10.1046/j.1360-0443.2000.95460111.x. [DOI] [PubMed] [Google Scholar]
- 21.Kandel DB, Johnson JG, Bird HR, et al. Psychiatric comorbidity among adolescents with substance use disorders: findings from the MECA Study. J Am Acad Child Adolesc Psychiatry. 1999 Jun;38(6):693–699. doi: 10.1097/00004583-199906000-00016. [DOI] [PubMed] [Google Scholar]
- 22.Stata Statistical Software: Release 10.0 [computer program] College Station, TX: Stata Corporation LP; 2007. [Google Scholar]
- 23.Smedley B, Stith A, Nelson A. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington D.C: Institute of Medicine; 2003. [PubMed] [Google Scholar]
- 24.Alegria M, Chatterji P, Wells K, et al. Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatr Serv. 2008 Nov;59(11):1264–1272. doi: 10.1176/appi.ps.59.11.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hill RP, Lubarsky DA, Phillips-Bute B, et al. Cost-effectiveness of prophylactic antiemetic therapy with ondansetron, droperidol, or placebo. Anesthesiology. 2000 Apr;92(4):958–967. doi: 10.1097/00000542-200004000-00012. [DOI] [PubMed] [Google Scholar]
- 26.Thomas CR, Holzer CE., 3rd The continuing shortage of child and adolescent psychiatrists. J Am Acad Child Adolesc Psychiatry. 2006 Sep;45(9):1023–1031. doi: 10.1097/01.chi.0000225353.16831.5d. [DOI] [PubMed] [Google Scholar]
- 27.Guzick DS, Jahiel RI. Distribution of private practice offices of physicians with specified characteristics among urban neighborhoods. Med Care. 1976 Jun;14(6):469–488. doi: 10.1097/00005650-197606000-00002. [DOI] [PubMed] [Google Scholar]
- 28.Kindig DA, Movassaghi H, Dunham NC, Zwick DI, Taylor CM. Trends in physician availability in 10 urban areas from 1963 to 1980. Inquiry. 1987 Summer;24(2):136–146. [PubMed] [Google Scholar]
- 29.Sentell T, Shumway M, Snowden L. Access to mental health treatment by English language proficiency and race/ethnicity. J Gen Intern Med. 2007 Nov;22 (Suppl 2):289–293. doi: 10.1007/s11606-007-0345-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Snowden LR. Barriers to effective mental health services for African Americans. Ment Health Serv Res. 2001 Dec;3(4):181–187. doi: 10.1023/a:1013172913880. [DOI] [PubMed] [Google Scholar]
- 31.United States Department of Health and Human Services . Mental Health: Culture, Race, and Ethnicity. A Supplement to Mental Health: A Report of the Surgeon General. Washington D.C: U.S. Government Printing Office; 2001. [PubMed] [Google Scholar]
- 32.Substance Abuse and Mental Health Services Administration - Office of Applied Studies. Adolescent Treatment Admissions by Gender. Rockville, MD: 2005. [Google Scholar]
- 33.Wu LT, Ringwalt CL. Use of alcohol treatment and mental health services among adolescents with alcohol use disorders. Psychiatr Serv. 2006 Jan;57(1):84–92. doi: 10.1176/appi.ps.57.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Klein JD, Wilson KM, McNulty M, Kapphahn C, Scott Collins K. Access to Medical Care for Adolescents: Results form the 1997 Commonwealth Fund Survey of the Health of Adolescent Girls. Journal of Adolescent Health. 1999;25 (2):120–130. doi: 10.1016/s1054-139x(98)00146-3. [DOI] [PubMed] [Google Scholar]
- 35.Clark DB, Gordon AJ, Ettaro LR, Owens JM, Moss HB. Screening and Brief Intervention for Underage Drinkers. Mayo Clinic Proceedings. 2010;85(4):380–391. doi: 10.4065/mcp.2008.0638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Knight JR, Goodman E, Pulerwitz T, DuRant RH. Reliabilities of short substance abuse screening tests among adolescent medical patients. Pediatrics. 2000;105(4 Pt 2):948–953. [PubMed] [Google Scholar]
- 37.Elster A, Jarosik J, VanGeest J, Fleming M. Racial and Ethnic Disparities in Health Care for Adolescents. Archives of Pediatrics and Adolescent Medicine. 2003;157(9):867–874. doi: 10.1001/archpedi.157.9.867. [DOI] [PubMed] [Google Scholar]
- 38.Anglin TM, Naylor KE, Kaplan DW. Comprehensive school-based health care: high school students' use of medical, mental health, and substance abuse services. Pediatrics. 1996 Mar;97(3):318–330. [PubMed] [Google Scholar]