Abstract
Aims:
To evaluate the accuracy of measurement of hepatic venous pressure gradient by catheter wedge as compared to balloon wedge (the gold standard).
Materials and Methods:
Forty-five patients having a clinical diagnosis of intrahepatic portal hypertension were subjected to the two different types of pressure measurements (catheter wedge and balloon wedge) during transjugular liver biopsy under fluoroscopic guidance.
Statistical Analysis:
Spearman's rank correlation coefficient, Bland–Altman plot for agreement, and single measure intraclass correlation were used for analysis of data.
Results:
There was a close correlation between the results obtained by both the techniques, with highly significant concordance (P < 0.0001). Hepatic venous pressure gradients as measured by the catheter wedge technique were either equal to or less than those obtained by the balloon wedge technique.
Conclusions:
The difference in hepatic venous pressure gradients measured by the two techniques is insignificant.
Keywords: Balloon wedge hepatic venous pressure, catheter wedge hepatic venous pressure, free hepatic venous pressure, hepatic venous pressure gradient
Introduction
Hepatic venous wedge pressure (HVWP) is a dynamic variable reflecting the hepatic sinusoidal pressure and therefore, indirectly, the portal pressure.[1] It is used to calculate the hepatic venous pressure gradient (HVPG),[2] the normal value being between 1 and 5 mmHg.[3,4] The current gold standard technique for measuring HVWP is the balloon wedge method.[3,4] The clinical importance of measuring HVPG in portal hypertension is well documented in the literature.[3,4]
Because of the technical difficulties associated with the balloon wedge technique, the potential for hepatic venous intimal injury, and the added cost of a balloon catheter, an alternative method with equivalent accuracy would be useful. We conducted the current study with the aim of determining whether a significant difference existed in the HVPG if measured using the conventional catheter wedge method.
Materials and Methods
From May 2007 to June 2008, 45 patients having a clinical diagnosis of intrahepatic portal hypertension due to etiologies that included viral (hepatitis B and C), autoimmune, metabolic (Wilson disease), cryptogenic cirrhosis, and noncirrhotic intrahepatic portal hypertension referred to our department for hepatic vein pressure measurements and transjugular liver biopsy (TJLB), were included in this study. Of the 45 patients with a mean age 41.6 ± 12.8 years, 30 were male. Cases of Budd-Chiari syndrome were excluded.
Definitions
Measurement of hepatic vein pressures
The procedure was done under local anesthesia. The right internal jugular vein was accessed under ultrasonography guidance. A 9F sheath (Cook Medical, Bloomington, USA) was placed instead of a 6F sheath (Cook Medical) if the patient had to undergo a TJLB. The right hepatic vein was selectively cannulated under fluoroscopy using a 5F multipurpose catheter and a 0.035′ guidewire (Cordis, Miami, FL, USA). An angiogram was performed to confirm the location of the catheter. Right atrial pressure and FHVP were then recorded. Subsequently, the catheter was wedged against the hepatic parenchyma and three pressures were recorded at different sites . We ensured that there was no contrast in the catheter during pressure measurement. All pressures were measured using an Agilent; monitor with a quartz pressure transducer.
The catheter was exchanged for a balloon catheter (6F/7F Swan Ganz, Edwards Lifesciences, Irvine, USA) over a 0.030’/0.035’ guidewire (Emerald, Cordis, Miami, FL, USA). The balloon was inflated using 50% iodinated contrast (iohexol, 300 mgI/mL, Omnipaque, GE Healthcare, Shanghai, China) in normal saline until the balloon flattened against the walls of the hepatic vein and the pressure through the lumen of the balloon catheter was recorded [Figure 1].
Figure 1 (A, B).
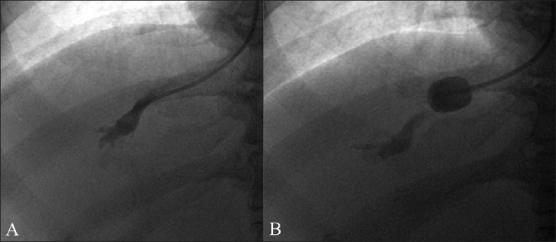
Contrast study shows hepatic venogram (A) and balloon wedging (B)
TJLB was done whenever requested. The sheath was removed and external compression was applied at the puncture site for hemostasis.
Statistical analysis
For statistical analysis of the results we used three different methods. In the first method, we calculated the Spearman's rank correlation coefficient, that is, Spearman's rho (ρ).[6] The second method was the Bland-Altman plot for agreement,[7,8] which can be used to compare a new measurement technique or method with a gold standard. In the final method of comparison, the correlation coefficient was calculated by single-measure intraclass correlation.[9]
Results
The measured values of both catheter wedge and balloon wedge HVPGs are plotted in Figure 2, along with the line of equality. Statistical analysis was done using the 3 different methods as explained:
Figure 2.
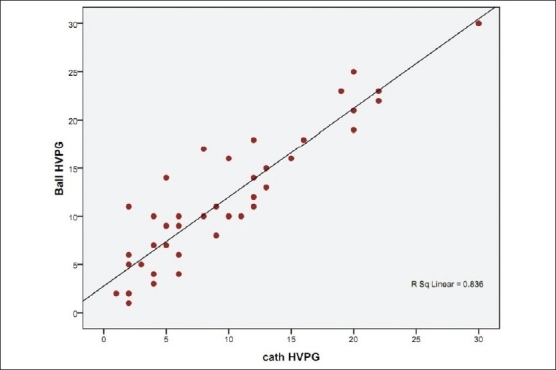
Hepatic venous pressure gradient measured using catheter wedge method and balloon wedge method with the line of equality
Spearman's correlation coefficient (ρ) was found to be 0.876, with P < 0.01, showing that there is a significant correlation.
The Bland–Altman plot for agreement between catheter wedge and balloon wedge pressure gradients [Figure 3] showed good correlation.
The intraclass correlation coefficient was 0.8895, with P < 0.001, showing that the correlation is significant.
Figure 3.
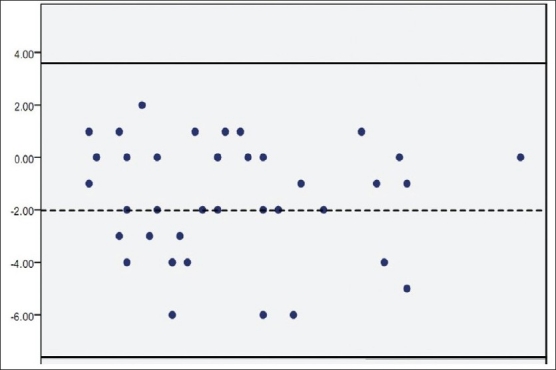
Bland–Altman plot for agreement of catheter wedge and balloon wedge techniques
Subgroup analysis (1–12, 13–20, and >20 mmHg) was not possible because there weren’t enough cases in the 2nd and 3rd subgroups to allow any significant statistical correlation.
All the patients tolerated the procedure well and there were no postprocedural complications.
Discussion
HVWP measurement plays an integral role in the evaluation of patients with portal hypertension. A few important applications include the assessment of portal pressure in cirrhosis to predict risk of formation of varices (HVPG > 12 mmHg) or the risk of rebleeding from varices (HVPG > 20 mmHg), to assess the response to pharmacologic agents during treatment of portal hypertension (>20% fall in HVPG from baseline), and to help differentiate between presinusoidal (as in the case of noncirrhotic portal hypertension) and sinusoidal causes of portal hypertension.[2,10,11] Hence HVPG monitoring provides important information for patients undergoing treatment for the prevention of variceal bleeding or rebleeding, allowing identification of patients who will be effectively protected against the risk of bleeding and those who, by not achieving an HVPG reduction by 20% of baseline or to ≤2 mmHg, remain at a very high risk of bleeding.[12]
There is only one similar study in the literature; that study, done by Barth and Udoffin 1980, compared the HVPGs in a smaller number (11) of patients with alcoholic cirrhosis as measured by balloon wedge and catheter wedge techniques. Variations in results between the 2 methods ranged up to 3 mmHg, with all patients having elevated hepatic wedge pressures of 15-25 mgHg. They found that the difference was insignificant.[1] Our study includes patients of varied etiology and a wide range of HVPGs of 1–30 mmHg.
Comparison of techniques
The catheter wedge technique is relatively easy to perform but requires multiple measurements of HVWP. Sometimes it needs injection of contrast media to confirm the wedge position. There are certain risks associated with this technique, such as perforation of the vessel by the guide wire or catheter or hepatic parenchymal damage by forceful contrast injection. On the other hand, the balloon wedge technique results are more representative of average parenchymal pressure than the standard wedged catheter measurements. It requires a balloon and an exchange wire, is more time consuming, and exposes patients to slightly higher levels of radiation. Enlargement of the puncture site with severe bleeding may occur with dislodgement of the incompletely deflated balloon. So prior to withdrawal of the catheter through the puncture site, complete balloon deflation is necessary.[1] Potential intimal injury is a rare but important complication with the balloon wedge technique.
The total cost of HVPG measurement at our center using the catheter wedge technique is INR 8000. The use of the balloon catheter would result in an additional cost of INR 2000.
Acknowledgments
We acknowledge our sincere thanks to our statistician Mrs. Visalakshi Jeyaseelan, MSc, Department of Biostatistics, Christian Medical College, Vellore, for her guidance and help.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
References
- 1.Barth KH, Udoff EJ. Transfemoral balloon catheterization for hepatic wedge pressure measurements. Radiology. 1980;135:779–80. doi: 10.1148/radiology.135.3.7384475. [DOI] [PubMed] [Google Scholar]
- 2.Jaime Bosch, Gennaro D’Amico. Schiff's disease of liver. 10th ed. Vol. 1. Philadelphia, USA: Lippincott Williams & Wilkins; 2007. Portal Hypertension and non surgical management; pp. 436–9. [Google Scholar]
- 3.Groszmann r. Measurement of portal pressure: When, How and Why to Do It? Clin Liver Dis. 2006;10:499–512. doi: 10.1016/j.cld.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 4.Groszmann RJ, Wongcharatrawee S. The hepatic venous pressure gradient: Anything worth doing should be done right. Hepatology. 2004;39:280–2. doi: 10.1002/hep.20062. [DOI] [PubMed] [Google Scholar]
- 5.Boyer TD. WHVP: Ready for prime Time. Hepatology. 2006;43:405–6. doi: 10.1002/hep.21118. [DOI] [PubMed] [Google Scholar]
- 6.Spearman C. The proof and measurement of association between two things. Am J Psychol. 1987;100:441–71. [PubMed] [Google Scholar]
- 7.Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8:135–60. doi: 10.1177/096228029900800204. [DOI] [PubMed] [Google Scholar]
- 8.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10. [PubMed] [Google Scholar]
- 9.Fisher RA. 12th ed. New York: Hafner publishing company; 1954. Statistical methods for research workers; pp. 211–47. [Google Scholar]
- 10.Thomas D, Boyer J, Michael Henderson . 4th ed. Philadelphia, USA: Saunders; 2003. Portal Hypertension and bleeding esophageal varices, Hepatology; pp. 581–630. [Google Scholar]
- 11.Madhu K, Avinash B, Ramakrishna B, Eapen CE, Shyamkumar NK, Zachariah U, et al. Idiopathic non-cirrhotic intrahepatic portal hypertension: Common cause of cryptogenic intrahepatic portal hypertension in a Southern Indian tertiary hospital. Indian J Gastroenterol. 2009;28:83–7. doi: 10.1007/s12664-009-0030-3. [DOI] [PubMed] [Google Scholar]
- 12.D’Amico G, Garcia-Pagan JC, Luca A, Bosch J. Hepatic vein pressure gradient reduction and prevention of variceal bleeding in cirrhosis: A systematic review. Gastroenterology. 2006;131:1611–24. doi: 10.1053/j.gastro.2006.09.013. [DOI] [PubMed] [Google Scholar]


