Abstract
Background & objectives:
Against the backdrop of insufficient public supply of primary care and reports of informal providers, the present study sought to collect descriptive evidence on 1st contact curative health care seeking choices among rural communities in two States of India - Andhra Pradesh (AP) and Orissa.
Methods:
The cross-sectional study design combined a Household Survey (1,810 households in AP; 5,342 in Orissa), 48 Focus Group Discussions (19 in AP; 29 in Orissa), and 61 Key Informant Interviews with healthcare providers (22 in AP; 39 in Orissa).
Results:
In AP, 69.5 per cent of respondents accessed non-degree allopathic practitioners (NDAPs) practicing in or near their village; in Orissa, 40.2 per cent chose first curative contact with NDAPs and 36.2 per cent with traditional healers. In AP, all NDAPs were private practitioners, in Orissa some pharmacists and nurses employed in health facilities, also practiced privately. Respondents explained their choice by proximity and providers’ readiness to make house-calls when needed. Less than a quarter of respondents chose qualified doctors as their first point of call: mostly private practitioners in AP, and public practitioners in Orissa. Amongst those who chose a qualified practitioner, the most frequent reason was doctors’ quality rather than proximity.
Interpretation & conclusions:
The results of this study show that most rural persons seek first level of curative healthcare close to home, and pay for a composite convenient service of consulting-cum-dispensing of medicines. NDAPs fill a huge demand for primary curative care which the public system does not satisfy, and are the de facto first level access in most cases.
Keywords: First healthcare contact, health seeking, informal, non-degree allopathic providers, primary curative healthcare, rural, traditional healers
Primary curative outpatient healthcare is in great demand in India. According to National Health Accounts1, 88 per cent of households’ health expenditure is spent on curative services, of which 48 per cent is towards primary curative care, also defined as “ambulatory or outpatient treatment of illness”2. Dror et al3 investigated the cost of illness among the poor in five locations in India and reported that 33 per cent of the costs were attributed to consultations and 49 per cent to payment for drugs.
National surveys suggest that the proportion of persons falling sick and seeking curative care in rural and urban India is comparable: the National Sample Survey (60th Round) reported 823/1000 ailments treated (in the 15 days preceding the survey) in rural vs. 893/1000 in urban areas4; this difference is offset by the higher proportion of rural population (more than 70%)5, so in absolute numbers, rural treatment-seekers outnumber urban ones.
Despite a larger demand for healthcare among rural persons, the quality and quantity of healthcare supply is relatively lower in rural than in urban areas6,7. For instance, a survey of all healthcare providers in the State of Madhya Pradesh (population 60.4 million) enumerated 24,807 qualified doctors, of whom, 75.6 per cent worked in the private sector, mostly (80%) in urban areas6.
Ambulatory outpatient care is supposed to be available in rural areas through the public delivery system at Primary Health Centres (PHCs). Each PHC serves on average 30,000 persons and is managed by a medical doctor. A PHC is linked to 6 sub-centres (SCs), each serving about 5,000 persons, and managed by an Auxiliary Nurse Midwife (ANM) who delivers family planning services, some maternity care and immunizations. Secondary level care is supposed to be delivered by Community Health Centres (CHCs), where four specialist doctors should offer specialized care to 120,000 persons8. A district hospital at the top provides tertiary referral care and supervision.
This basic 3-tier system has not changed since it was proposed by India's first Health Survey and Development Committee9, but the Committee's recommended ‘population norm’ of one PHC per 10,000-20,000 population has never been achieved. With a current infrastructure of 23,458 PHCs and 4,276 CHCs, and with 18.8 per cent vacancies in PHC doctors’ positions and 51.6 per cent vacancies in CHC specialists’ positions8, the system suffers from inadequate infrastructure and doctor shortages10, while India's rural population has grown to more than 700 million5. There is low utilization of primary outpatient care in public facilities because of long distances, inconvenient opening hours, lengthy waiting, staff absenteeism, poor availability of medicines, and poor quality of care11–13. One analysis showed that public facilities were utilized by people in low income States more than by people in high- and middle-income States14.
Evidence suggests that rural people seek outpatient primary care from private providers for many conditions, including newborn/child illnesses15,16, malaria/febrile illnesses17, TB18 and women's health19. People's choice of provider may reflect provider proximity, cost, reputation, perceived ‘recovery’, lack of faith in the public sector, and lay notions of aetiology13,20,21. The private health sector in rural India includes a heterogeneous mix of providers; some are professionally trained, but the majority are unqualified. A survey done in 2007 enumerated only about 28 per cent qualified doctors6. Almost all the 89,090 unqualified providers practiced as private rural practitioners. Different types of practitioners and systems have existed in rural India. Studies from the 1960s and 1970s reported that traditional healers or indigenous medical practitioners used both modern and traditional medicines22. Later studies refer to “rural medical practitioners”23 following mainly allopathic treatment practices. More recent studies have reported that in rural areas health-seekers approached traditional healers17,21 and also qualified practitioners of AYUSH (Ayurveda, Unani, Siddha and Homeopathy systems)6. However, only a minority (14%) utilize the pure traditional cures24.
The Indian government launched its National Rural Health Mission (NRHM) in 200525 to increase access and quality of healthcare in rural areas. The present study conducted in 2008-2009, sought to investigate the post NRHM status of curative health care seeking at first contact among rural communities. Evidence collected from health care seekers (demand side) was juxtaposed with evidence collected from providers (supply side) on first contact healthcare, including the illnesses, patients’ choices and providers’ patient load, treatments, medicines, and referrals. This study embraces a horizontal approach in investigating 1st contact curative care, regardless of the cause, and by all providers participating de-facto in the health system.
Material & Methods
This study was part of a larger baseline study to initiate rural micro health insurance programmes in two States – Andhra Pradesh (AP) and Orissa. Field work was conducted in AP during May-June 2008 and in Orissa during January-February 2009.
Quantitative methods
Household survey (HHS)
Sampling: In the two districts in AP there were 2031villages with a total population of 5,359,959 spread across 1,257,235 households5. In the three districts in Orissa (Kalahandi, Malkangiri and Khorda), there were 4436 villages, and a total population of 2,776,546 spread across 602,561households. For AP with a total of 1257,235 HHs and an assumed 10 per cent frequency of visiting qualified physicians (obtained by discussions with community leaders) the calculated sample size for an error of 2% and 99% confidence level was 1491 HHs. For Orissa, with a total of 602,561 HHs, the calculated sample size was 1489. The actual sample included 1,810 households in AP and 5,342 in Orissa.
The villages were selected purposively, where local organizations were involved in the micro health insurance project [Cooperative Development Foundation (CDF) in AP and the Madhyam Foundation in Orissa with its 11 affiliated NGOs]; 20 villages in AP (12 in Warangal and 8 in Karimnagar districts) and 80 villages in Orissa (27 in Kalahandi, 22 in Khorda, and 31 in Malkangiri districts). In every village, two cohorts were randomly sampled counting the same number of households: members of self-help groups (SHGs), and non-member households.
The SHGs were savings and borrowing societies that were already present at the two sites. The micro health insurance was intended only for existing SHG members, and we wanted to make sure that there was no difference in socio-economic status or education between the prospective insured and uninsured (to eliminate any confounding differences later on in our impact analysis).
Research tool and implementation: A structured questionnaire was developed in English, translated into Telugu and Oriya, and validated through back translation and cognitive pre-testing in 80 households each in AP and in Orissa, and modified as necessary. Project personnel trained local investigators to carry out the interviews. The questionnaire included close-ended questions on respondents’ socio-demographic characteristics, healthcare utilization, providers approached first by household members for outpatient care when ill, and reasons for approaching these providers. In the Orissa survey, the inquiry was refined to confirm whether allopathic practitioners were degree vs. non-degree [which was inferred in AP by combining HHS and focus group discussion (FGD) data].
The method as adopted by the Indian National Sample Survey Organization (NSSO) was followed to obtain a proxy for income through questions on many items of household expenditures. Similar to NSSO, the monthly per capita expenditure (MPCE) served as proxy for income.
Qualitative methods
Focus group discussions (FGDs)
Sampling: A total of 19 FGDs (9 men's, 10 women's) in AP, and 29 FGDs (13 men's and 16 women's) were conducted in Orissa; 214 persons participated in FGDs in AP (96 men and 118 women), and 314 in Orissa (121 men, 193 women). Villages for FGDs were selected (5 in AP and 15 in Orissa) by location within districts, distance from towns and from medical facility (near, medium or far). Participants in FGDs were men and women aged 25 to 45 yr. Groups were gender- and income homogenous (proxy for income was land ownership). As far as possible, the same number of FGDs were conducted with males and females in each village.
Research tool and implementation: An FGD guide (pre-tested with 2 male and 2 female focus groups in each State) was developed and local persons (2 in AP, 4 in Orissa) were trained to facilitate discussions on morbidity and incidence, health seeking decisions, first providers approached, perceptions of how providers treated and what they charged. The facilitators were debriefed after every session. All FGDs were held in settings ensuring privacy and confidentiality to participants.
Key informant interviews (KII)
Sampling: KIIs were conducted with 9 village-based providers in AP and 20 in Orissa, plus solo general practitioners (GPs) and specialists in nearby towns, and hospital-based providers (13 in AP and 19 in Orissa). First popular providers were located and interviewed and then other providers were identified with their help.
Research tools and implementation: Semi-structured interview tools were developed per provider category (pre-tested with 4-6 providers in each State) to collect information on education and training of village providers, practice characteristics, services rendered, and types of patients. Interviews in health facilities or with GPs focused on listing services, staff, and basic information on patients.
Ethical compliance
This research project met all the requirements of the funding agency (NWO-WOTRO) on ethical issues arising in social science research. The research document for all the interventions (e.g. FGDs, HHS interviews, and KIIs) included an introductory section tantamount to a protocol of informed choice in which the researchers explained the purpose of the study, what would be done with the data, and sought and obtained verbal consent of participants to participate in the interviews and discussions, and to record the FGD meetings. Participants’ names were kept confidential in data recording and analysis. All interviews were organized so as to ensure interviewees that confidentiality would be kept.
Statistical analysis: SPSS v.17 (Source: www.ibm.com/software/analytics/spss) was used to analyse HHS data. We organised the taped, transcribed and translated FGD data into matrices and explored similarities, differences, recurrent themes and categorizations within data driven sub themes, broadly covering perceptions of common diseases, hierarchy of care seeking, characteristics of and perceptions related to providers of first contact. KII data were entered in Excel, and simple frequencies for close-ended questions were calculated. Open-ended questions were entered verbatim and analyzed qualitatively to determine common characteristics, relationship with communities, and treatment patterns.
Results
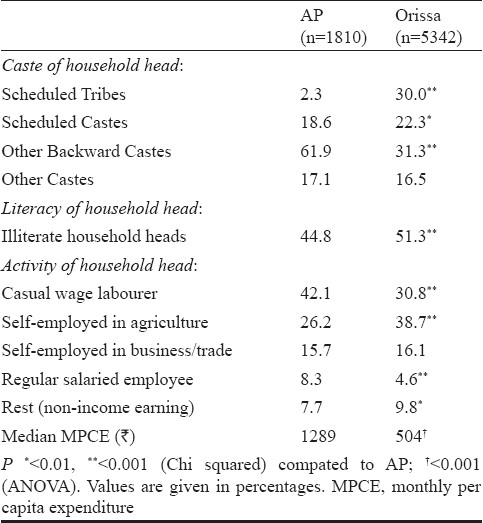
The study populations in the two States reported significantly different household incomes. Median MPCE in AP was INR 1,289, more than twice that of Orissa (INR 504). The proportion of Scheduled Tribes (STs) was significantly (P<0.001) higher in Orissa than in AP, while the proportion of OBCs was higher (P<0.001) in AP. Illiteracy was higher (P<0.001) in Orissa (Table I). There were also differences in economic activity of household heads: in Orissa the largest group was that of self employed small farmers, while the largest group in AP was composed of casual wage labourers. No significant differences were found between SHG members and non-members. Women formed the majority of HHS respondents in both States: 72.3 per cent in AP and 67.7 per cent in Orissa. Other available household members if present, also contributed.
Table I.
Profile of the study communities in Andhra Pradesh (AP) and Orissa
In AP as village sizes were bigger than in Orissa and there was sufficient representation of men and women from different socio-economic groups, four different FGDs were organized per village (2 men's and 2 women′s) representing poor and better off households in each village. In most of the poorer groups, half or more of the participants were illiterate and a few only had completed 10 years of schooling. However, literacy differences were less pronounced in the women's groups where even the better off groups had more illiterate than literate members. Participants in the poorer groups were either landless and worked as “coolies”( daily wage farm labourers), or as other types of daily wage labourers (e.g. loaders), or had small farms less than 3 acres in size but also sometimes worked as "coolies" or ran small businesses (such as a small shop) to supplement their farm income. Participants in the better off groups usually owned medium sized (3-6 acres) farms and a few owned bigger ones (10-20 acres). These groups also had participants with less land but with bigger businesses (e.g. tailor) and some had salaried jobs (e.g. teacher, driver).
In Orissa, villages were smaller and communities more homogenous with respect to occupations and land ownership. Thus only two FGDs could be organized per village, one male and one female. In general, there were more illiterate participants here than in AP. While in each district 1-2 FGDs comprised landless daily wage labourers (e.g. farm labour/constructions workers/ small vendors), the majority were small farmers with 1-5 acres of land. As in AP the latter supplemented their income through daily wage activities, or through small businesses such as selling fruits, vegetables and also fish, and in those villages that were close to the capital city of Bhubaneswar, through salaried jobs (e.g. clerks and peons).
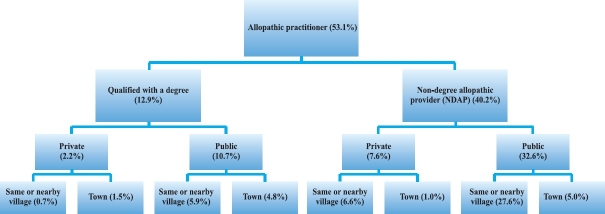
Providers of first health-seeking contact: In both States, FGD narratives suggested that the first response to an illness could be self medication, with men more likely to buy an over-the-counter paracetamol or other medicine and the women more likely to rely on home remedies. When these were not effective, they sought care from available providers. In AP, 94.8 per cent HHS respondents usually approached an allopathic practitioner first (Fig. 1); most (69.5%) approached private allopathic practitioners in the same village or nearby village and 22.1 per cent approached private practitioners in town. FGDs revealed that in villages, private ‘allopathic’ practitioners were informally trained and unlicensed, often called Registered Medical Practitioner (RMPs), a designation used in some States until the 1970s, and still included in some State Medical Councils26, but currently synonymous with unregistered practitioners without formal qualifications in medicine. We refer to these as non-degree allopathic providers (NDAPs).
Fig. 1.
First care seeking contact in Andhra Pradesh.
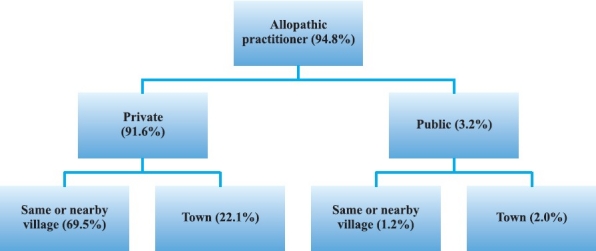
In Orissa 53.1 per cent of respondents had their first health-seeking contact was with an allopathic practitioner; of these 40.2 per cent approached NDAPs and 12.9 per cent consulted qualified physicians (Fig. 2). In the FGDs, people referred to the NDAP as “choto doctor” (small doctor). Triangulation of the HHS, FGDs and KIIs showed that in Orissa, some NDAPs (e.g. pharmacists, nurses and compounders) were employed in government health centres, and treated patients in villages for-a-fee. In Orissa, 32.6 per cent of HHS respondents usually approached such “public sector NDAPs” first, mostly in the same or nearby village (27.6%) (Fig. 2).
Fig. 2.
First care seeking contact in Orissa (allopathic practitioner details).
Around a quarter or less of respondents in both States approached qualified doctors in the first instance. In AP, these were doctors in private practice in nearby towns (22.1% - Fig. 1), whereas public practitioners were mentioned by only 3.2 per cent. In Orissa a smaller proportion of respondents (12.9%) approached qualified doctors first, and the majority of those (10.7%) went to public sector doctors (Fig. 2).
A substantial proportion of respondents in Orissa (36.2%) also approached other non-allopathic practitioners first: traditional healers. Fewer households approached other types of practitioners: only 0.2 per cent respondents in AP and 4.2 per cent in Orissa approached AYUSH practitioners, and 5 per cent in AP and 6.4 per cent in Orissa approached government health workers like ANMs, ASHAs (Accredited Social Health Activist) and AWWs (Aanganwadi Worker).
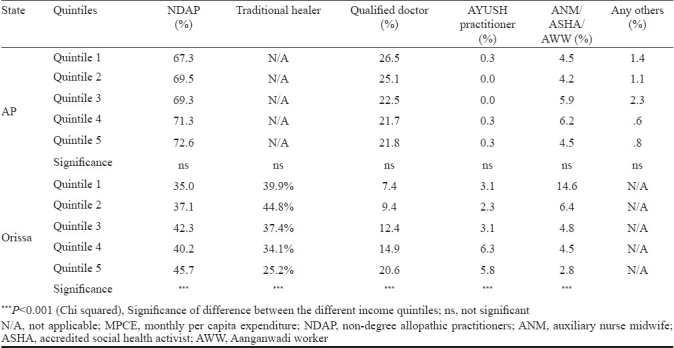
Association between income and choice of provider: In view of the diversity of first contact providers, association between income of the population (MPCE quintiles) and choice of first contact provider was examined, a significant association was seen in Orissa but not in AP (Table II). In Orissa, a significant decrease was observed in the frequency of accessing traditional healers with income, which was mainly due to a lower frequency in the fifth income quintile. A positive association was found between income quintiles and frequency of seeking care with qualified doctors. The lowest quintile reported 7.4 per cent and the highest 20.6 per cent. There was a small but significant increase in the frequency of choosing NDAPs with increasing income.
Table II.
Type of provider first approached by different MPCE quintiles in Andhra Pradesh (AP) and Orissa
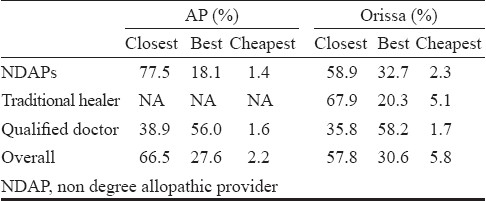
Reasons for choice of first contact provider: Respondents named proximity as the most important reason for their choice of first contact provider. It was the main reason for a majority of respondents that approached NDAPs and traditional healers (77.5% in AP and 58.9% in Orissa for NDAPs; 67.9% for traditional healers in Orissa; Table III). Fewer respondents named their reason as provider being ‘best’ (18.1% in AP and 32.7% in Orissa for NDAPs; 20.3% for traditional healers in Orissa). However, among those who approached a qualified doctor first, a majority said it was because that provider was ‘best’ (56.0% AP; 58.2% Orissa) followed by ‘closest’ (38.9% AP; 35.8% Orissa).
Table III.
Reasons why HHS respondents chose 1st contact health provider
Provider profiles and people's perceptions
Traditional healers: Traditional healers provided a substantial proportion of health care at first contact in Orissa but not in AP. In Orissa, over one-third of the HHS respondents usually sought first consultation with traditional healers (Fig. 2) as they were their closest providers (Table III).
These practices could not be generalized across all study communities, since care seeking from traditional healers was expressed more by groups that were more remotely located and had fewer allopathic options in or around their villages, or among groups with greater economic impoverishment. These findings were in agreement with the HH survey results that showed an inverse relationship between income and care seeking from traditional healers. However, tribal populations (STs) chose traditional healers less frequently than SCs and OBCs (28.3 vs. 43.3% and 40.2% respectively, P<0.001). There was no significant association between frequency of choice of traditional healer and literacy.
Non-degree allopathic providers (NDAPs): NDAPs were sought by almost 70 per cent HHS respondents in AP and 40 per cent in Orissa. NDAPs in AP were private practitioners but in Orissa people also sought care from public sector NDAPs. Some employees in government health centres, especially the primary health centres (PHCs) including pharmacists, nurses, and even health attendants, acted as NDAPs in Orissa in three situations: firstly, when the health facility had no doctor and was managed entirely by non-doctor staff. Doctor shortages in Malkangiri (with large tracts of inaccessible areas) were particularly acute. Secondly, when a doctor was assigned, but absent from duty for any reason, some of the doctor's tasks were routinely performed by other health workers. Thirdly, when the doctor was present but patient load at the facility was high, other health workers (e.g. pharmacists, nurses, female/male health workers, health attendants) performed some of the doctor's tasks.
From the FGDs with men and women, and KIIs with 9 NDAPs, some common characteristics as well as differences were identified between private NDAPs in the two States. All were male. Their average age was 36 yr in AP (range of 24 to 50 yr) and 43 yr in Orissa (range of 28 to 60 yr). All had well-established independent practices with an average professional experience of 13.3 yr in AP and 20.5 yr in Orissa. The majority had completed 10 or more years of schooling. Most NDAPs acquired skills through informal apprenticeships, usually with other doctors both private and public. NDAPs in AP delivered mainly mobile services. All 9 possessed mobile phones and responded to emergency calls plus provided services within a radius of 0-5 km (1-5 villages) of where they lived; two who owned a scooter/motorcycle extended their catchment area to 20-25 km. Five NDAPs also had rudimentary clinics. Most, however, spent between 6 and 12 h daily circulating in villages and providing doorstep services. In Orissa, only half the NDAPs provided mobile healthcare in a larger radius of 5-20 km from their village; those who had a motorcycle travelled longer distances. The other half combined static and mobile services, during 1-4 h daily for rounds or to respond to calls, within a smaller radius of 2-5 km.
Most NDAPs in AP saw 20 or more patients daily (range from 10 to 70 patients); mobile providers had most patients. In Orissa, NDAPs saw a smaller average of 12 patients daily (range from 2 to 40 patients) and older practitioners had higher patient-loads. The providers were asked to estimate their catchment population (households they usually served). In AP, it ranged from 50 to 300 households, with an average of 100 households. In Orissa, it ranged from 40 to 1200 households with an average of 300 households.
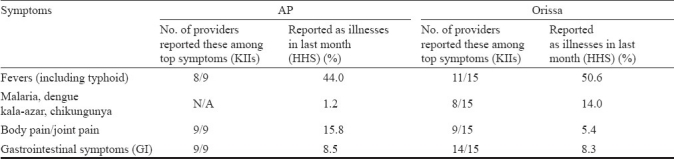
NDAPs in both States treated the most commonly reported morbidities. We compared five most frequently treated conditions named by NDAPs with replies to the HHS question: “Did a person in the HH have an illness episode last month? What kind of illness was it?” The information from both sources tallied closely (Table IV). ‘Fever’ topped the list, followed by body pains and GI symptoms in AP, and malaria in Orissa.
Table IV.
Most common symptoms/illnesses reported by HHS respondents and private NDAPs in AP and Orissa
NDAPs in both States used allopathic medicines to provide symptomatic relief. Typically, they dispensed medicines for 2-3 days (rarely up to a week), and if there was no improvement, they referred patients. NDAPs also referred in emergencies, sometimes providing first aid or accompanying patients to a qualified physician or hospital. In Orissa, NDAPs sometimes performed simple diagnostic tests (e.g. blood test for malaria).
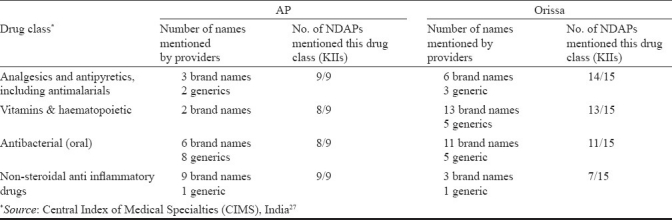
Some NDAPs also prescribed drugs additional to those they dispensed. We listed 37 brand names of drugs named by NDAPs in AP and 49 in Orissa (Table V). The various drug types mentioned were classified by mode of action (following CIMS India Reference System)27. CIMS information revealed that 44 manufacturers produced the 37 AP brands and 48 produced the 49 Orissa brands. This suggests that NDAPs were familiar with multiple branded drugs with different names (different manufacturers) and that these brands were available over the counter in the retail market, from where NDAPs said they restocked their supplies weekly or fortnightly. NDAPs used mostly four classes of drugs: analgesics/antipyretics/antimalarial, vitamin and iron supplements, antibacterial and non steroidal anti inflammatory drugs (NSAIDs) (Table V). In Orissa, three providers also dispensed ayurvedic remedies. AP providers mentioned no indigenous medicines. Some NDAPs also gave nutritional advice on consumption of foods rich in vitamins and minerals such as leafy vegetables, eggs, milk and fruits.
Table V.
Drugs named by private NDAPs in AP and Orissa
NDAPs were asked to name five common conditions for which they referred patients, and where they referred to. Most NDAPs referred for gynaecological problems (e.g. pregnancy and institutional delivery), pains, chronic non-communicable conditions (e.g. heart problems, hypertension, diabetes, kidney related problems), acute fevers and gastrointestinal conditions, and in Orissa also for accidents and injuries including snakebites.
NDAPs usually referred to private doctors in AP, and to public facilities in Orissa. In Orissa, the public sector doctors (especially in peripheral facilities) confirmed that NDAPs referred cases for pregnancy, delivery and for serious conditions (e.g. malaria and pneumonia).
Yet we could not find any incentive for NDAPs to refer cases, either through training to improve recognition of referral conditions, or through financial incentives similar to those that government workers like ASHAs receive for each delivery they refer. In AP, NDAPs who referred to private doctors, received occasional gifts (like table calendars) but no financial incentives.
Qualified doctors: Around a quarter of HHS respondents in AP and roughly half that proportion in Orissa approached qualified allopathic doctors at first contact (Figs 1 & 2). The major difference was that doctors approached in AP were primarily town based private practitioners while in Orissa they were public servants employed at government PHCs and CHCs.
FGDs and KIIs confirmed these two different State scenarios. In AP, FGD participants, both men and women, named a number of private doctors and facilities that they approached in nearby towns, whereas in Orissa, when participants talked about care seeking from a qualified doctor, they usually referred to a government facility identifiable by its location and referred to as a “hospital” irrespective of whether it was a PHC or a CHC or a tertiary hospital.
However, whether public or private, people usually approached these qualified doctors as the second step in their care seeking pathway, if the first level intervention in the village did not succeed, or in multiple care-seeking at the same level (e.g. going from one specialist to another in AP). FGDs suggested that seeking first contact care from qualified doctors was related to (i) economic status of the household as only better off households could afford the total higher costs (of transport, wage loss, fees, medicines, and tests) of approaching a qualified doctor, (ii) perceived severity of the health condition: if the condition was seen as beyond the scope of the village doctor (e.g. a snake bite or a heart problem), then people would bypass the village level and go straight to a doctor, and (iii) proximity to the provider/facility: those communities that lived within easy walking distance of a health facility in Orissa were likely to go straight to that facility first.
In AP, people had access to many private doctors even at block level towns and semi urban areas, but not so at the village level. In Orissa, especially in the poorer districts of Kalahandi and Malkangiri, government PHCs and CHCs were the main source of care by qualified physicians (who were government employees), and these were located even in villages beyond the block towns. Although Orissa respondents accessed public facilities more than in AP, many of these facilities were understaffed, especially in Malkangiri and Kalahandi districts. Malkangiri's Chief Medical Officer informed that only 33 out of 100 sanctioned medical doctors were available in the district public health system.
The private sector provided rural AP communities with a multiplicity of options for care seeking from qualified physicians, and both men and women, even from poorer households appeared to prefer private to public because of better perceived care and treatment. For women, it was familiarity and faith in the doctor and the doctor's kindness that was important. More than one women's group close to a certain town (Narsampet) named the same doctors repeatedly as being among the nicer ones whom they approached both for general illnesses and for women's problems as well.
In AP, men, much more than women, had a tendency to analyse the mode of operation of private qualified doctors. They complained about the high costs, doctors’ business orientation and malpractices but they still preferred to go to private doctors.
In AP, use of public primary facilities was limited to immunizations at the PHCs. Although intended for the poor and cheaper than private, public facilities were nonetheless not perceived as poor-friendly by poor consumers. In Orissa, public facilities were people's major and, in many places, only source of access to a qualified physician. Though doctor consultations were usually free of charge in PHCs and CHCs and even the sub-divisional hospitals, people said that doctors usually prescribed medicines and tests from outside private sources. In FGDs, people repeatedly complained about two problems: (i) the money they had to spend on transport to reach public facilities - an amount that could exceed the cost of medicines; and (ii) the money they had to spend out of pocket for medicines and tests, and at one district hospital (which allowed private practice by public doctors) also for the doctors’ consultation fee.
Discussion
Through multifarious strategies and enhanced funding, the Government of India provides accessible, affordable and quality healthcare to rural persons. The National Rural Health Mission (NRHM) launched in 2005 for implementation up to 201225 is the most recent large-scale programme to strengthen the existing 3-tier public health delivery system. Our study demonstrated that the huge need for primary level curative healthcare was different from what the 3-tier system has been able to provide, and that this need was satisfied mainly outside the public system. For one, the data showed that the overwhelming reason given for the choice of first contact curative provider was proximity. From the FGDs it was known that the proximate providers were also available at all hours of the day and night, and responded to telephone calls.
The doctors at public, and even more at private health facilities, often required that patients undergo diagnostic tests and buy prescribed medicines, the combined cost of which was high, plus there were indirect costs of transportation and wage-loss. NDAPs were much closer to care-seekers in villages, made house calls when requested, charged lower fees and provided the all-in-one “quick-fix” service. Thus, more than 75 per cent of the population preferred to go to NDAPs and (in Orissa) also to traditional healers for first contact curative care. This evidence demonstrates that people seek a different type of primary curative care, which is not doctor-centric and is delivered not in a far away doctor's clinic, and for which clients are willing to pay.
The people did not choose their first contact provider by whether he was a “small doctor” or a “big doctor”. Frequently, factors like distance and cost determined people's care-seeking preferences more than providers’ skills or accreditation. This alternative treatment trail was mostly at odds with government policy, and people consulted professional doctors only when they, or their first contact NDAP, perceived a specific reason to do so.
Consistent with previous evidence10,11, staff shortages and low utilization of the public sector were found. However, our findings do not uphold the assumption that the need among rural communities for proximate all-in-one primary curative healthcare would disappear even if all the PHCs and CHCs were to become fully staffed and well equipped. Thus, if the public system should deliver such care, health planners would need to revise the objectives and deliverables of the various tiers in the public system.
Our evidence on practice of NDAPs not only confirms previous reports about their widespread presence in rural areas2,6, but also gives new details about the existence, in addition to private practitioners, of “public sector NDAPs”.
Some scholars have explained the recourse to traditional healers (accessed by 36% of care-seekers in Orissa) by reference to illiteracy and tribal cultures28; in our examination, this explanation was not confirmed, as there was no significant difference in the rate of consulting traditional healers across literate or illiterate HH heads and, interestingly, tribal households approached traditional healers less than non tribal households. However, our data suggested that there was a negative association between income and frequency of traditional healer care seeking that was most apparent in the richest quintile in Orissa.
It was found that private qualified doctors practiced in AP even at block level, but almost none could be found in Orissa, especially in Kalahandi and Malkangiri (the poorer and more remote districts of Orissa). In these districts, the PHCs and CHCs, were understaffed. The reason why fewer private doctors practiced in Orissa was people's lower ability to pay, demonstrated by lower median MPCE (pattern confirmed by National Sample Survey 2005-06:  460.32 for Orissa and
460.32 for Orissa and  704.17 in AP). Our findings provided additional evidence to support this conclusion, as the frequency of accessing qualified doctors increased significantly with income in Orissa.
704.17 in AP). Our findings provided additional evidence to support this conclusion, as the frequency of accessing qualified doctors increased significantly with income in Orissa.
Based on analysis of illnesses reported by people (juxtaposed against those reported by providers), it appears that NDAPs manage the most frequent illnesses, and thus fill a limited but essential gap in access to first contact curative healthcare in rural India. Similar to findings of others23, NDAPs in our study were mostly male, with long-established practices of allopathy close to where they live, typically dispensing small doses of medicines when consulting patients, and charging a flat fee for both consultation and medicines. A new feature of NDAP services i.e. “on-call” services to respond to clients’ needs for doorstep curative care as-and-when needed, anytime was also seen.
We found no signs of conflict of interests or “turf wars” between qualified doctors and NDAPs; on the contrary, we observed even some complementarity between the two categories of providers.
NDAPs referred complex cases to qualified doctors, often by accompanying the patients. This situation explains why, notwithstanding legal restrictions set out by the Indian Medical Council Act29 on the practice of medicine, some experts in the Indian public health community suggest that the role of NDAPs should be reviewed30. Even certain government commissions made similar recommendations. e.g. the National Commission for Macroeconomics and Health7, a Health Ministry Task Group on training and accreditation of rural practitioners31, and the NRHM. Additionally, a Task Force on Medical Education recommended a 3- year programme to train community health practitioners32, and the most recent official attempt is to design the curriculum for a Bachelor of Rural Health Care programme33. These programmes probably reflect the concern that the government should provide better than sub-optimal, first contact, primary curative care to rural populations.
NDAPs in our study treated with allopathic medicines and were familiar with not just one or two brand names of allopathic drugs, but with several, which they could access without any difficulties. This suggests that representatives and retailers of the pharmaceutical industry succeed in bringing drug related information (and drugs as well) to NDAPs in the same way as they reach qualified prescribers. As this study was not an empirical evaluation of the clinical quality of care of NDAPs, it is not possible to comment on the adequacy of use of the drugs they mentioned. However, the ease of access to drugs by persons lacking formal certification (like the NDAPs) and the absence of effective regulatory oversight of drug distribution in India raise some concern about practices of dispensing of medicines reported through this study.
The main study limitation was that due to resource constraints we could interview fewer first-contact providers than all those who were available. However, some of the providers most frequently approached as identified and located from people's descriptions in the FGDs were interviewed. Thus, these interviews provide a profile of providers that people accessed frequently in the study communities.
In conclusion, our study showed that the rural population in India indicates a need for “consult-cum-dispense” healthcare services for most common illnesses to be delivered most hours of the day and at doorstep (or at least served in or near their village). This treatment-trail for primary curative care has evolved unguided and unnoted by the formal system. The architecture of this treatment trail is crafted by the demand side, and has been solidified by the propagation of NDAPs practicing at village level. If the public sector should meet this health need, clearly the bottleneck would be not merely the insufficient number of doctors actually serving in PHCs and CHCs in rural areas. The policy conclusion is that services have to address the need expressed by people for more mobile, proximate - virtually doorstep - primary curative care that should combine consultation and dispensing of medicines, and would function many more hours. NDAPs fill a demand for primary curative care, with a new treatment-mix which the public system is not able to satisfy in rural India under existing operating conditions. The de-facto diffidence about (i) the need of rural populations for very different services than those planned under the existing 3-tier public system, and (ii) the important role of NDAPs in responding to the demand for these primary curative healthcare services, irrespective of policies or law, seems rather incongruous.
Acknowledgments
The authors acknowledge funding support from the Netherlands Organization for Scientific Research, under WOTRO Integrated Programme grant No. W01.65.309.00. Additional funding for the household survey in Orissa was obtained from the German Federal Ministry for Economic Cooperation and Development (through a contract between AWO International, Madhyam Foundation, Orissa and the Micro Insurance Academy, New Delhi). We benefited from logistical and research support from the Micro Insurance Academy, from Cooperative Development Foundation (CDF) in AP, and from Madhyam Foundation Bhubaneswar, Orissa and its 11 affiliated NGOs (Parivartan, PUSPAC, SOMKS, SDS, ODC, Mahashakti Foundation, DAPTA, Lok Yojana, Sanginee, MVPS, DSS). Authors thank all the respondents for their participation in the study.
References
- 1.National Health Accounts 2001-02. New Delhi: National Health Accounts Cell, Ministry of Health and Family Welfare, Government of India; 2005. MOHFW. [Google Scholar]
- 2.Berman PA. Rethinking health care systems: Private health care provision in India. World Development. 1998;26:1463–79. [Google Scholar]
- 3.Dror MD, van Putten-Radermaker O, Koren R. Cost of Illness: Evidence from a study in five resource-poor locations in India. Indian J Med Res. 2008;127:347–61. [PubMed] [Google Scholar]
- 4.Morbidity, health care and condition of the aged, NSS 60th Round (January-June 2004) New Delhi: National Sample Survey Organisation, Ministry of Statistics and Programme Implementation, Government of India; 2006. NSSO. [Google Scholar]
- 5.GOI. Census of India. Government of India. Available from: http://censusindia.gov.in/2001 .
- 6.De Costa A, Diwan V. Where is the public health sector?’ Public and private sector healthcare provision in Madhya Pradesh, India. Health Policy. 2007;84:269–76. doi: 10.1016/j.healthpol.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 7.Report of the National Commission on Macroeconomics and Health. New Delhi: Ministry of Health and Family Welfare, Government of India; 2005. GOI. [Google Scholar]
- 8.Bulletin On Rural Health Statistics In India, Updated as on March 2008. New Delhi: Ministry of Health and Family Welfare, Government of India; [accessed on May 3, 2010]. GOI. Available from: http://www.mohfw.nic.in/BulletinonRHS-March,2008-PDFversion/ [Google Scholar]
- 9.Bhore J. Report of the Health Survey and Development Committee, vol, II: Recommendations. New Delhi: Government of India Press; 1946. [Google Scholar]
- 10.Satpathy S. Public health infrastructure in rural India : Challenges and opportunities. Indian J Public Health. 2005;49:57–62. [PubMed] [Google Scholar]
- 11.Dalal K, Dawad S. Non-utilization of public healthcare facilities: examining the reasons through a national study of women in India. Rural Remote Health. 2009;9:1178. (Online), 2009:1-10. [PubMed] [Google Scholar]
- 12.Kotwani A, Ewen M, Dey D, Iyer S, Lakshmi PK, Patel A, et al. Prices and availability of common medicines at six sites in India using a standard methodology. Indian J Med Res. 2007;125:645–54. [PubMed] [Google Scholar]
- 13.Ager A, Pepper K. Patterns of health service utilization and perceptions of needs and services in rural Orissa. Health Policy Planning. 2005;20:176–84. doi: 10.1093/heapol/czi021. [DOI] [PubMed] [Google Scholar]
- 14.Purohit B. Inter-State disparities in health care and financial burden on the poor in India. J Health Social Policy. 2004;18:37–60. doi: 10.1300/J045v18n03_03. [DOI] [PubMed] [Google Scholar]
- 15.Kaushal M, Aggarwal R, Singal A, Shukla H, Kapoor SK, Paul VK. Breastfeeding practices and health-seeking behavior for neonatal sickness in a rural community. J Trop Pediatr. 2005;51:366–76. doi: 10.1093/tropej/fmi035. [DOI] [PubMed] [Google Scholar]
- 16.Deshmukh P, Dongre AR, Sinha N, Garg BS. Acute childhood morbidities in rural Wardha: some epidemiological correlates and health care seeking. Indian J Med Sci. 2009;63:345–54. [PubMed] [Google Scholar]
- 17.Chaturvedi HK, Mahanta J, Pandey A. Treatment-seeking for febrile illness in north-east India: an epidemiological study in the malaria endemic zone. Mal J. 2009;8:301. doi: 10.1186/1475-2875-8-301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fochsen G, Deshpande K, Diwan V, Mishra A, Diwan VK, Thorson A. Health care seeking among individuals with cough and tuberculosis: a population-based study from rural India. Int J Tuberc Lung Dis. 2006;10:995–1000. [PubMed] [Google Scholar]
- 19.Rani M, Bonu S. Rural Indian women's care-seeking behavior and choice of provider for gynecological symptoms. Study Family Plann. 2003;34:173–85. doi: 10.1111/j.1728-4465.2003.00173.x. [DOI] [PubMed] [Google Scholar]
- 20.Kamat VK. Reconsidering the popularity of primary health centers in India: A case study from rural Maharashtra. Soc Sci Med. 1995;41:87–98. doi: 10.1016/0277-9536(94)00309-h. [DOI] [PubMed] [Google Scholar]
- 21.Dongre AR, Deshmukh PR, Garg BS. Perceptions and health care seeking about newborn danger signs among mothers in rural Wardha. Indian J Pediatr. 2008;75:325–9. doi: 10.1007/s12098-008-0032-7. [DOI] [PubMed] [Google Scholar]
- 22.Bhatia JC, Vir D, Timmappaya A, Chuttani CS. Traditional healers and modern medicine. Soc Sci Med. 1967;9:15–21. doi: 10.1016/0037-7856(75)90153-5. [DOI] [PubMed] [Google Scholar]
- 23.Rohde J, Vishwanathan H. The rural private practitioner. Health Millions. 1994;2:13–6. [PubMed] [Google Scholar]
- 24.Singh P, Yadav RJ, Pandey A. Utilization of indigenous systems of medicine & homoeopathy in India. Indian J Med Res. 2005;122:137–42. [PubMed] [Google Scholar]
- 25.National Rural Health Mission: Meeting people's health needs in rural areas. Framework for Implementation 2005-2012. New Delhi: Ministry of Health and Family Welfare, Government of India; 2005. GOI. [Google Scholar]
- 26.MPAct. The Madhya Pradesh Ayurvigyan Parishad Adhiniyam (Schedule) 1987. [accessed on May 10, 2010]. weblink: http://www.mpmedicalcouncil.net/mpapa.html. 1990.
- 27.CIMS India. Central Index of Medical Specialties, Druginfo. 2010. [accessed on May 10, 2010]. website: http://cimsasia.com/index.aspx# .
- 28.Vijayakumar KN, Gunasekaran K, Sahu SS, Jambulingam P. Knowledge, attitude and practice on malaria: A study in a tribal belt of Orissa state, India with reference to use of long lasting treated mosquito nets. Acta Trop. 2009;112:137–42. doi: 10.1016/j.actatropica.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 29.The Indian Medical Council Act, 1956, Section 15 (2b) Delhi: Universal Law Publishing Co Pvt Ltd; 1956. IMC. [Google Scholar]
- 30.Yadav K, Jarhyan P, Gupta V, Pandav CS. Revitalizing rural health care delivery: Can rural health practitioners be the answer? Indian J Community Med. 2009;34:3–5. doi: 10.4103/0970-0218.45368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Recommendations of task-group set up to examine accreditation, training and integration of private rural medical practitioners, under National Rural Health Mission. New Delhi: Ministry of Health and Family Welfare, Government of India; 2007. GOI. [Google Scholar]
- 32.Task force on medical education for the National Rural Health Mission. New Delhi: Ministry of Health and Family Welfare, Government of India; [accessed on May 3, 2010]. GOI. http://www.mohfw.nic.in/NRHM/Documents/Task_Group_Medical_Education.pdf . [Google Scholar]
- 33.Dhar A. The Hindu. New Delhi: Jul 19, [accessed on July 20, 2010]. Task Force to design curriculum for rural health cadre. http://www.thehindu.com/news/national/article522247.ece . [Google Scholar]