Abstract
Background:
In a developing country, infectious disease remains the most important cause of fever, but the noncommunicable diseases, like malignancy, are fast becoming important differential diagnoses. An important clinical problem is the cases labeled as fever of unknown origin (FUO), which often evade diagnosis.
Objective:
The present study was undertaken to find the cause of FUO in a tertiary care hospital of eastern India.
Materials and Methods:
This is a prospective study of inpatients, with regard to both clinical signs and investigations.
Results:
The main diagnosis in the end was tuberculosis, closely followed by hematological malignancy. A substantial number of cases remained undiagnosed despite all investigations. The provisional diagnosis matched with the final in around two thirds of the cases. While for younger patients leukemia was a significant diagnosis, for older ones, extra-pulmonary tuberculosis was a main concern.
Interpretation:
In India, infectious disease still remains the most important cause of fever. Thus the initial investigations should always include tests for that purpose in a case of FUO.
Conclusion:
Geographic variations and local infection profiles should always be considered when investigating a case of FUO. However, some of the cases always elude diagnosis, although the patients may respond to empirical therapy.
Keywords: FUO, Infectious disease, Malignancy
INTRODUCTION
Fever remains the most enigmatic clinical symptom to treat. Although in a developing country infectious disease remains the most important cause of fever, the noncommunicable causes, like malignancy, are also becoming important. Preliminary investigations fail to find the etiology in many cases. This comprises a large group called “fever of unknown origin” (FUO), which can be a perplexing clinical puzzle. However, in many cases the cause for failure of diagnosis is lack of a proper protocol for investigation. If the investigation is based on the clinical findings, most of the cases can be easily diagnosed. The causes of fever change with the geographical distribution as also with time. The present study was undertaken to find the cause of FUO in a tertiary care hospital of eastern India.
Aims and Objectives
To investigate the cause of FUO in admitted patients
To find the relative incidence of different causes with special reference to infectious causes
To formulate a cost-effective working formula for approach to a case of FUO in our setting
MATERIALS AND METHODS
We examined patients with fever of at least 3 weeks’ duration who qualified for the definition of classical FUO, viz., (1) temperature of >38.3°C (>101°F) on several occasions; (2) a duration of fever of >3 weeks; and (3) failure to reach a diagnosis despite three outpatient visits or three days in the hospital without elucidation of a cause or one week of “intelligent and invasive” ambulatory investigation. Only the patients admitted to general medicine ward between 1st September 2008 and 30th July 2009 were examined and investigated after proper consent and ethical clearance. A rigorous selection process was adhered to [Figure 1].
Figure 1.
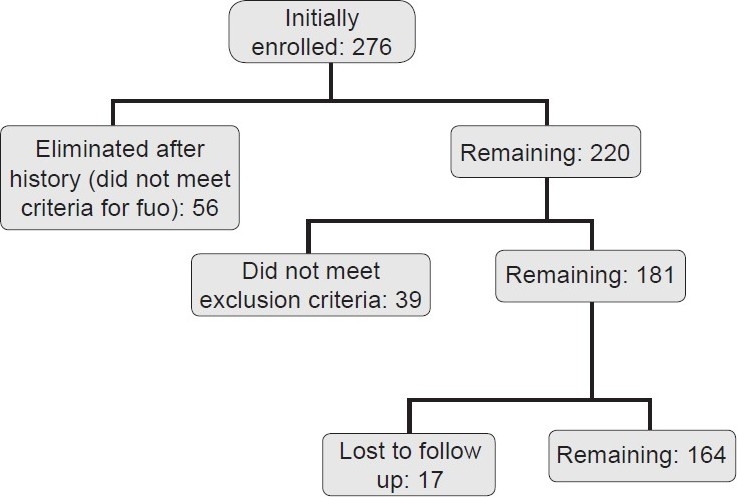
The selection process
Exclusion criteria were as follows:
Patients with known malignancy
Patients on steroids
Patients known to have HIV infection
Women in mid-menstrual cycle
Extremes of age
Patients having undergone any invasive procedure or surgery in the last three months
Patients taking anti-tubercular drug or having taken it in the last three years
After clinical examination, the patients were subjected to routine investigations. We formulated a protocol [Figure 2] and followed the algorithm after validation in a pilot study in our institution. Many tests like contrast enhanced computerized tomographic scan (CECT) abdomen were included in the second stage due to financial reasons. The investigations were done in the central laboratory of our college. Testing for malaria parasite has been part of routine examination in our endemic region. The samples were sent before starting of antibiotics. However, if fever persisted after three days, repeat of the cultures was done. The serologies were sent to the immunology lab of our college before any immuno-modifying drugs like steroids were started. We completed all investigations by two weeks. Patients remaining undiagnosed after that were referred to higher centers. However, specialized investigations like gallium scan, positron emission tomography (PET) scan and procalcitonin were largely under-utilized due to financial reasons. Data were arranged using Microsoft Excel worksheet. Then, statistical analysis was done using the freeware Epi-info™ version: 3.5.1 from centers for disease control (CDC). Also online statistical calculators were used in some cases (e.g., Graphpad).
Figure 2.
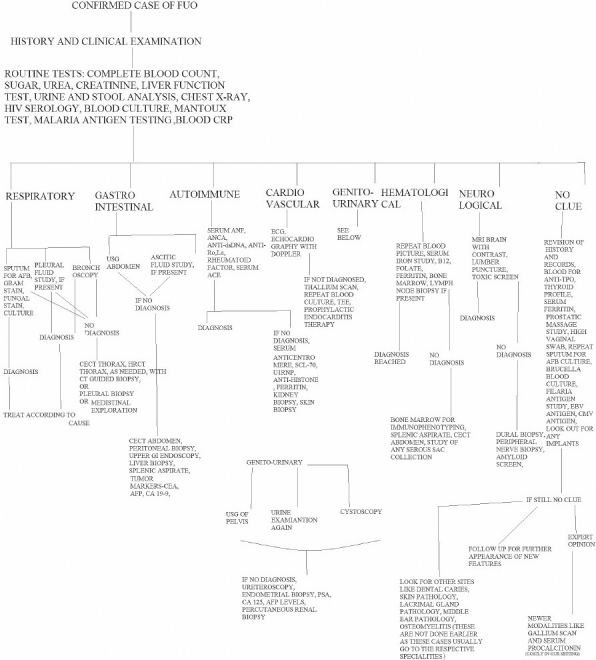
The study investigation protocol. Potential diagnostic clues were given much importance initially
RESULTS
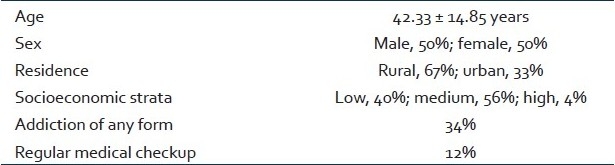
In our study, a total of 164 patients were included. In the study period, a total of 24 variables, including age, sex, addiction history and various laboratory test results, were measured [Table 1]. In our initial clinical examination, symptomatically 28.6% (n=47) of patients were found to have lymphoreticular system involvement, and 14.3% (n=23) of the patients had symptoms relating to the nervous system. Patients above 50 years of age had significantly lower average temperature than younger ones (P<0.05, by the Student t test).
Table 1.
Demographic characteristics of the patients
Based on these data, before starting the investigations we formed a provisional diagnosis for each patient. This diagnosis was later compared with the final one to assess the predictive value (by kappa statistic), as shown in Table 2. The bulk of the provisional diagnosis was hematological malignancy (n=34, 20.73%). It was closely followed by tuberculosis (n=38, 23.17%). This provisional diagnosis formed the basis of further tests. We needed serology tests in 26.83% of the cases, histology was sent in 36.11% of the cases, imaging in different forms was done in 76.83% of the cases and microbiological support was needed in 63.41% of the cases. Average Hb of the patients at admission was 8.26 g%, average total count was 16,610 and average ESR was 59.71 mm at the end of the first hour. The average length of stay was 14.47 days (±7.06 days). Average time needed for reaching a diagnosis was 5.64 days (±3.2 days). After diagnosis the patients stayed for therapy or were transferred to other specialties.
Table 2.
Comparison between diagnoses from clinical examination at presentation and diagnoses after laboratory investigations
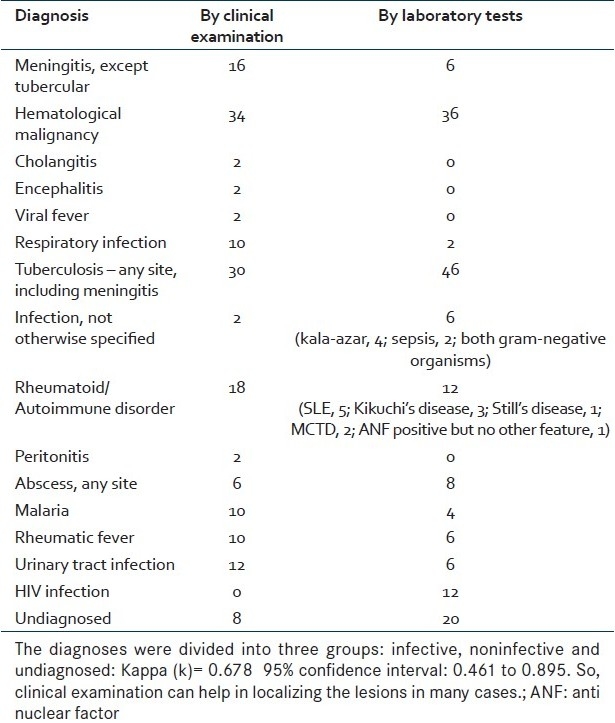
After all the tests [Table 2], 28.04% of the patients (n=46) were found to have tuberculosis, while 22% of the patients (n=36) were found to have a hematological malignancy, either leukemia or lymphoma. Among the tuberculosis cases, 71.72% (n=33) were extra-pulmonary, with lymph node tuberculosis topping the list (50% of the total tuberculosis cases, n=23); closely followed by peritoneal tuberculosis (29%, n=13). Among the younger patients (age <30 years), we found leukemia in 27.77% (n=13) of the cases; while in older patients (age >45 years), tuberculosis was found in 30% of the cases. Among the autoimmune causes, systemic lupus erythematosus (SLE) topped the list (n=5), followed by Still's disease, Mixed Connective Tissue Disease and 3 cases of Kikuchi's disease. Time needed for diagnosis varied according to etiology. For infective causes like malaria and bacterial meningitis, the time taken was much less (average, 1.75 days) compared to the malignant causes (average, 10 days). Autoimmune diseases also took up much time (average, 9.25 days) [P<0.05 by ANOVA]. The variables were analyzed in a logistic regression model. The final diagnoses were divided into two groups: infectious and noninfectious. It was found that 55% (n=90) of the diagnoses were of infectious diseases, while malignant and autoimmune diseases constituted 22% (n=36) and 11% (n=18) of the diagnoses, respectively. It was found that low eosinophil count (<100/mm3) was associated with greater chance of infectious disease (P=0.0433). A high neutrophil count was associated with marginally greater chance of infectious causes (OR=1.6; P=0.002). C-Reactive Protein (CRP) levels ≥6 mg/L had a sensitivity of 68.18% [confidence interval (CI), 54.4% to 81.9%) and specificity of 60% (CI, 45% to 76.1%) in predicting infections. Overall, a positive CRP (>6) was associated with increased likelihood that final diagnosis can be made (P=0.000727; OR=5.25). In older persons (>50 years), we found a combination of increased lymphocyte (> 1800/mm3) with increased ESR (>50 mm) to be a predictor of malignancy, although individually they did not have that predicative value for malignancy. In abdominal pathologies, CECT abdomen had high yield (P<0.05) in reaching a final diagnosis.
At the end of two weeks, 12.2% (n=20) of the cases remained undiagnosed. However, at the one-month follow-up, 6 (30% of the undiagnosed cases) more cases were diagnosed.
DISCUSSION
Fever is one of the most perplexing clinical signs. It may occur in such diverse conditions as infections, malignancy and drug effect and due to environmental toxicity. Even after intensive search, the etiology of a sizeable proportion of fevers remains unclear. Fever of unknown origin (FUO) was defined by Petersdorf and Beeson in 1961. While this definition has stood for more than 30 years, Durack and Street have proposed a new system for classification of FUO. In India infectious disease remains the main cause of fever.[1] In our study, 58.53% of the fevers had infectious causes. Tuberculosis was at the top of the list, constituting 41.6% of the infectious causes. This is true for other developing regions of the world.[2,3] Malignancy occupies a high proportion of the causes of fever. In one study from Kolkata, it was found that[4] malignancies caused fever in 17% of the cases; in our series, this figure was 22%. However, in our series the malignancies were all hematological. Malignancies of other sites did not present as FUO in our study. Autoimmune diseases were present in 11% of the patients. In a similar study from eastern India, the investigators found 9% of the cases were with these disorders.[4]
In our study, we could establish the diagnosis in 88% of the cases. This is similar to a study from eastern India.[4] For diagnosis of tuberculosis, we depended on sputum examinations, chest X-ray and adenosine deaminase (ADA) levels. Tuberculosis polymerase chain reaction (TB-PCR) was used in suspected cases not diagnosed otherwise. Also in some cases, a therapeutic trial with anti-tubercular drugs (ATDs) was used. Thus the approach to a case of fever in our country should always include infectious causes. Although in elderly patients malignancy is a more important possibility, yet infectious causes should be ruled out first.[5] With the current upsurge of HIV infection, especially in developing countries, HIV is a major cause of FUO.[6] In some studies,[7] lymphoma is found as a more prevalent hematological malignancy; but in our case, we found leukemia was more prevalent [14.6% vs. 7.3%]. However, like in other regions of Southeast Asia,[8] we also found SLE as the most prevalent autoimmune disease. The cause of FUO varies with age.[9] A recently published similar study found serum ferritin, eosinophil count and CRP levels as predictors of infectious disease.[10] We also found significant relation of infectious disease with CRP levels and eosinophil count. However, ferritin was not done in all the cases in our study [Figure 1].
CONCLUSION
In India, infectious disease still remains the most important cause of fever. Thus the initial investigations should always include tests for ruling out or confirming diagnosis of infectious disease. Signs and symptoms can guide us to the final diagnosis in majority of the cases.[11] The aim of this study was to provide a working formula for diagnosis and treatment of FUO in a resource-limited setup. So, although advanced techniques like fluorodeoxy glucose-PET were largely unused in this study, yet diagnosis was reached in 88% of the cases. This shows the importance of a proper protocol of investigations that can be cost-effective.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Jung A, Singh MM, Jajoo U. Unexplained fever-analysis of 233 cases in a referral hospital. Indian J Med Sci. 1999;53:535–44. [PubMed] [Google Scholar]
- 2.Colpan A, Onguru P, Erbay A, Akinci E, Cevik MA, Eren SS, et al. Fever of unknown origin: Analysis of 71 consecutive cases. AM. 2007;334:92–6. doi: 10.1097/MAJ.0b013e31812f5642. [DOI] [PubMed] [Google Scholar]
- 3.Chin C, Chen YS, Lee SS, Wann SR, Lin HH, Lin WR, et al. Fever of unknown origin in Taiwan. Infection. 2006;34:75–80. doi: 10.1007/s15010-006-5010-2. [DOI] [PubMed] [Google Scholar]
- 4.Kejariwal D, Sarkar N, Chakraborti SK, Agarwal V, Roy S. Pyrexia of unknown origin: A prospective study of 100 cases. J Postgrad Med. 2001;47:104–7. [PubMed] [Google Scholar]
- 5.Knockaert DC, Vanneste LJ, Bobbaers HJ. Fever of unknown origin in elderly patients. J Am Geriatr Soc. 1993;41:1187–92. doi: 10.1111/j.1532-5415.1993.tb07301.x. [DOI] [PubMed] [Google Scholar]
- 6.Molina-Gamboa J, Rivera-Morales I, Camacho-Mezquita E, Ponce-de-León S. The changing spectrum of fever of unknown origin: Trends and comparison with previous series at the Salvador Zubirán National Institute of Nutrition. Rev Invest Clin. 1994;46:177–85. [PubMed] [Google Scholar]
- 7.Arce-Salinas CA, Morales-Velázquez JL, Villaseñor-Ovies P, Muro-Cruz D. Classical fever of unknown origin [FUO]: Current cases In Mexico. Rev Invest Clin. 2005;57:762–9. [PubMed] [Google Scholar]
- 8.Ma XJ, Wang AX, Deng GH, Sheng RY. A clinical review of 449 cases of fever of unknown origin. Zhonghua Nei Ke Za Zhi. 2004;43:682–5. [PubMed] [Google Scholar]
- 9.Joshi N, Rajeshwari K, Dubey AP, Singh T, Kaur R. Clinical spectrum of fever of unknown origin among Indian children. Ann Trop Paediatr. 2008;28:261–6. doi: 10.1179/146532808X375413. [DOI] [PubMed] [Google Scholar]
- 10.Efstathiou SP, Pefanis AV, Tsiakou AG, Skeva II, Tsioulos DI, Achimastos AD, Mountokalakis TD. Fever of unknown origin: Discrimination between infectious and non-infectious causes. Eur J Intern Med. 2010;21:137–43. doi: 10.1016/j.ejim.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 11.Cunha BA. Fever of unknown origin: Clinical overview of classic and current concepts. Infect Dis Clin North Am. 2007 Dec;21:867–915. doi: 10.1016/j.idc.2007.09.002. [DOI] [PubMed] [Google Scholar]


