Abstract
Background:
Peptic ulcer disease can lead to serious complications including massive hemorrhage or bowel perforation. The modern treatment of peptic ulcer disease has transitioned from the control of gastric acid secretion to include antibiotic therapy in light of the identification of Helicobacter pylori as a causative infectious organism. We sought to determine trends related to this discovery by using a national database.
Materials and Methods:
Patient discharges with peptic ulcer disease and associated sequelae were queried from the Nationwide Inpatient Sample, 1993 to 2007, under the auspices of a data user agreement. To account for the Nationwide Inpatient Sample weighting schema, design-adjusted analyses were used. Standard error was calculated using SUDAAN software (Research Triangle International, NC, USA).
Results:
Decreases in the incidences of gastrointestinal perforation, gastrointestinal hemorrhage, and surgical procedures most specific to peptic ulcer disease were statistically significant over the study period [range of P value (two tailed) = 0.000 – 0.00353; significant at P < 0.001 to < 0.01]. The incidence of H. pylori rose dramatically, peaking at an estimated 97,823 cases in 1998 [SE = 3155; 95% CI = 6,184]. Since that time it has decreased and then stabilized.
Conclusions:
The identification of H. pylori as the causative agent in the majority of peptic ulcer disease has revolutionized the understanding and management of the disease. Medical conditions and surgical procedures associated with end-stage peptic ulcer disease have significantly decreased according to analysis of selected index categories. Resident physician education objectives may need to be modified in light of these trends.
Review Criteria:
We reviewed patients with peptic ulcer disease. The database used was the Nationwide Inpatient Sample, 1993 to 2007.
Message for the Clinic:
Medical therapy has resulted in decreased morbidity from H. pylori infection as it is the causative agent in the majority of peptic ulcer disease. Aggressive screening and treatment of this infection will lead to further reduction in morbidity.
Keywords: Dyspepsia, Helicobacter pylori, Hemorrhage, Peptic ulcer, Vagotomy
INTRODUCTION
Peptic ulcer disease (mucosal erosion of the gastrointestinal tract) is a common and serious condition that was once thought to be a result of emotional stress and diet. Morbidity and mortality from this condition are mainly related to abdominal discomfort and more seriously, hemorrhage and bowel perforation.[1] Two important developments have been associated with decrease in rates of peptic ulcer disease: The discovery of effective and potent acid suppressants and the identification of Helicobacter pylori.[2] Since H. pylori and non-steroidal anti-inflammatory drugs (NSAIDs) account for the majority of peptic ulcer disease, recent trends in disease can generally be related to these.[3,4]
The modern history of infectious peptic ulcer disease has followed a remarkable course. From the purposeful ingestion of bacteria, to the awarding of the Nobel Prize, Mashall and Warren laid the groundwork for a revolution in the medical and surgical arena.[5,6] Acceptance of their theory became widespread and the institution of treatments such as “triple therapy” began to have dramatic effects.[7,8] While several population-based studies have temporally analyzed the characteristics of peptic ulcer disease[9–16], none have assessed the effect of discovery of H. pylori on hospital admissions and surgical procedures performed as a result of end stage ulcer disease. We sought to identify trends in the incidence peptic ulcer disease, its complications, and treatments as surrogate markers for the influence of the identification of H. pylori as the major contributor to peptic ulcer disease by using a national database.
MATERIALS AND METHODS
We studied the practice patterns relating to peptic ulcer disease from 1993 to 2007, which we obtained from the Healthcare Cost and Utilization Project, Agency for Healthcare Research and Quality (AHRQ) Rockville, MD.[17] The nationwide inpatient sample (NIS) is a hospital discharge database that represents approximately 20% of all inpatient admission to nonfederal hospitals in the US. The NIS contains discharge data on 100% of discharges from 1993 to 2007. It is an expanding, stratified random sample of nonfederal hospitals now comprised of 1,044 hospitals in 40 states. Detailed information on the design of the NIS is available at http://www.hcup-us.ahrq.gov. The NIS includes >100 clinical and non-clinical variables for each hospital stay. These include diagnoses, procedures, admission and discharge status, demographics, charges, and lengths of stay.
Patients registered in the NIS from 1993 to 2007 were included in the analysis. Those with H. pylori infection as a primary diagnosis were identified using International Classification of Disease 9th Revision clinical modifier (ICD-9 CM) diagnostic code 041.86.
Patients with end stage complications of H. pylori infection (such as gastrointestinal ulcer, hemorrhage, and perforation) were identified by characteristic primary ICD-9 CM diagnostic codes: 531.0 acute gastric ulcer with hemorrhage, 531.1 acute gastric ulcer with perforation, 532.0 duodenal ulcer, 533.0 peptic ulcer, site unspecified, 533.4 chronic or unspecified with hemorrhage, 533.5 chronic or unspecified with perforation, and 533.9 unspecified as acute or chronic, without mention of hemorrhage or perforation. Then, patients undergoing surgical procedures with a high degree of specificity for end-stage peptic ulcer disease (vagotomy and gastrectomy) were identified by ICD-9 CM procedure codes: 43.6 partial gastrectomy with anastomosis to duodenum, 43.7 partial gastrectomy with anastomosis to jejunum, 44 vagotomy, not otherwise specified, 44.01 truncal vagotomy, 44.02 highly selective vagotomy, and 44.03 other selective vagotomy. No accounting could be made for the use of NSAIDs, aspirin, steroids, cigarettes, or alcohol as they do not exist in the NIS dataset.
To account for the Nationwide Inpatient Sample weighting schema, design-adjusted analyses were used. The estimates of standard errors were calculated using SUDAAN software (Research Triangle International, NC, USA). A Z-test was then used to determine the significance of the yearly incidence changes over the study period.
RESULTS
The incidence of H. pylori rose dramatically, peaking at an estimated 97,823 cases in 1998 (SE = 3,155; 95% CI = 6,184). Since that time it has decreased and then stabilized. In 2007, there were only 54,115 cases of H. pylori reported (SE = 1,784; 95% CI = 3,497).
Decreases in the incidences of bowel perforation, gastrointestinal hemorrhage, and surgical procedures most specific to peptic ulcer disease were statistically significant over the study period from 1993 to 2007 [Figure 1]. Acute gastric ulcer with hemorrhage (ICD-9 CM diagnosis code 531.0) decreased from an estimated incidence of 33,525 in 1993 (SE = 1,223; 95% CI = 2,397) to 8,716 in 2007 (SE = 449; 95% CI = 880); z statistic = 19.04, SE 1302.81, P value (two tailed) = 0.000. Other selected indexes included acute gastric ulcer with perforation (ICD-9 CM diagnosis code 531.1) that decreased from 2,816 in 1993 [SE = 150; 95% CI = 294] to 1,106 in 2007 (SE = 83; 95% CI = 163); z statistic= 9.97, SE 171.43, P value (two tailed) = 0.000, acute duodenal ulcer with hemorrhage (ICD-9 CM diagnosis code 532.0) that decreased from 28,820 in 1993 (SE = 956; 95% CI = 1,874) to 6,900 in 2007 (SE = 352; 95% CI = 690) z statistic= 21.51 SE 1018.74, P value (two tailed) = 0.000, and acute peptic ulcer with hemorrhage in an unspecified site (ICD-9 CM diagnosis code 533.0) that decreased from 2,393 in 1993 (SE = 176; 95% CI = 345) to 422 in 2007 (SE = 53; 95% CI = 104) z statistic= 10.72 SE 183.81, P value (two tailed) = 0.000. Other types of ulcers also saw a significant decrease in incidence over the study period, including chronic or unspecified type with hemorrhage (ICD-9 CM diagnosis code 533.40) that decreased from 6,063 in 1993 [SE = 327; 95% CI = 640.92] to 3,823 in 2007 [SE = 204; 95% CI = 399.84] z statistic= 5.81 SE 385.42, P value (two tailed) = 0.000, chronic or unspecified with perforation (ICD-9 CM diagnosis code 533.50) that decreased from 490 in 1993[SE = 55; 95% CI = 107.8] to 295 in 2007 [SE = 38; 95% CI = 74.48] z statistic= 2.92 SE 66.85, P value (two tailed) = 0.00353, and truly unspecified ulcers(ICD-9 CM diagnosis code 533.90) decreased from 6,845 in 1993 [SE = 332; 95% CI = 650.72] to 4,034 in 2007 [SE = 231; 95% CI = 452.76] z statistic= 6.95 SE 404.46, P value (two tailed) = 0.000.
Figure 1.
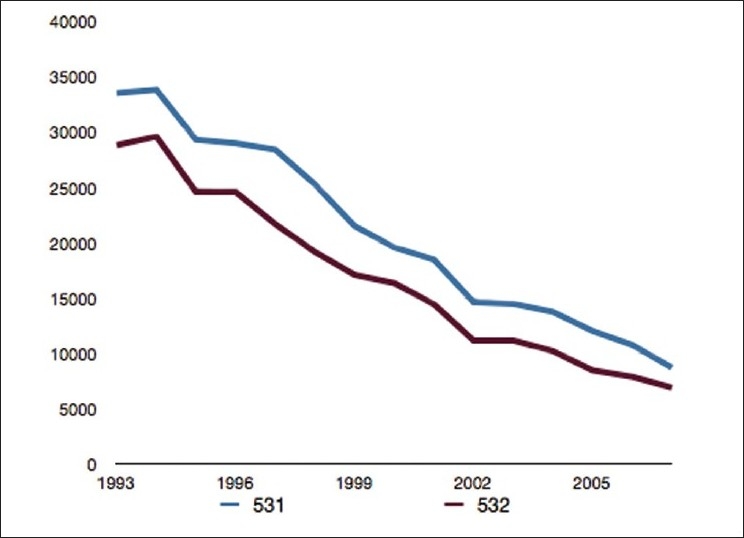
Time trends in incidence rates for selected procedures (1993-2007) according to ICD-9 CM code
The number of coded procedures that were felt to be specific for end stage complications of H. pylori infection dramatically decreased [Figure 2]. The incidence of partial gastrectomy with an anastomosis to the duodenum (ICD-9 CM procedure code 43.6) decreased from 6,040 in 1993 [SE = 287; 95% CI = 562.52] to 1,722 in 2007 [SE = 118; 95% CI = 231.28] z statistic= 13.92 SE 310.31, P value (two tailed) = 0.000. Similarly, the incidence of partial gastrectomy with an anastomosis to the jejunum (ICD-9 CM procedure code 43.7) decreased from 13,516 in 1993 [SE = 429; 95% CI = 840.84] to 8630 in 2007 [SE = 496; 95% CI = 972.16] z statistic= 7.45 SE 655.79, P value (two tailed) = 0.000. Combined, the trends in incidences of these procedures reflect a 47% decrease in selected anastomotic procedures during the study period.
Figure 2.
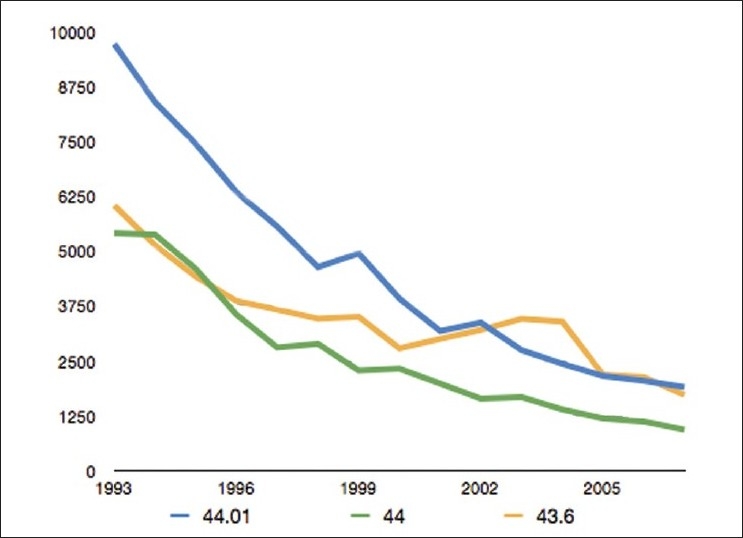
Time trends in incidence rates for selected diagnosis (1993-2007) according to ICD-9 CM code
Vagotomy (ICD-9 CM procedure code 44) saw a decrease in incidence from 5,409 cases in 1993 [SE = 276; 95% CI = 540.96] to 932 in 2007 [SE = 84; 95% CI = 164.64] z statistic= 15.52 SE 288.50, P value (two tailed) = 0.000. Other variants of this code included a truncal vagotomy (ICD-9 CM procedure code 44.01) that went from 9,718 cases in 1993 [SE = 387; 95% CI = 758.52] to 1,902 cases in 2007 [SE = 159; 95% CI = 311.64] z statistic= 18.68 SE 418.39, P value (two tailed) = 0.000, the highly selective vagotomy (ICD-9 CM procedure code 44.02) that went from 1,290 cases in 1993 [SE = 129; 95% CI = 252.84] to only 262 cases in 2007 [SE = 59; 95% CI = 115.64] z statistic= 7.25 SE 141.85, P value (two tailed) = 0.000, and other selective vagotomy (ICD-9 CM procedure code 44.03) that decreased from 2,015 cases in 1993 [SE = 156; 95% CI = 305.76] to 587 cases in 2007 [SE = 62; 95% CI = 121.52] z statistic= 8.51 SE 167.87, P value (two tailed) = 0.000.
DISCUSSION
We studied a population of patients diagnosed with H. pylori infection and conditions most specific for its sequaele undergoing inpatient admission by using a nationally representative hospital discharge database. The results of our analysis showed that generally the morbidity associated with this condition has dramatically decreased during the study period of 1993 to 2007.
A trend witnessed was that the incidence of H. pylori initially went up, rising from 11,592 diagnosis in 1995 to 97,823 diagnosis in 1998. It is highly likely that public awareness campaigns and a disseminating knowledge regarding the etiology of peptic ulcer disease are to credit.[18] Since 1998, the reported incidences of H. pylori infection have actually decreased and then stabilized. We hypothesize that empiric treatment protocols for dyspepsia are responsible.[19] It has recently been proven in a well designed study that empiric therapy is equally as effective as a “test and treat” protocol for the treatment of dyspepsia.[20]
While new treatment regimens have likely decreased the morbidity and mortality associated with H. pylori infection, one must also consider the implications this has on the education of resident physicians and surgeons. In an era where work-hour restrictions have raised debate over the potential of their impact on resident operative volume and proficiency,[21–25] attention must also be paid to the effect of trends in disease and treatment patterns over relatively short periods of time. The Accreditation Council for Graduate Medical Education requires that in addition to compliance with work hour restrictions, general surgery residency programs are obligated to provide a minimum number of cases and demonstrate competence achievement.[26] Patterns in peptic ulcer disease, as a result of the identification of H. pylori as the causative agent, should be considered in evaluating and modifying general surgery residency educational objectives, particularly with respect to foregut surgery. The often cited correlation (or lack thereof) between work hour restrictions and operative volume is not direct; considerations must be included to compensate for major trends in disease specific practice patterns.
Study strengths
This is an analysis of over 15 years of data collected in a standardized fashion across the United States that includes hundreds of thousands of patients. No study of this size has ever been performed with respect to H. pylori incidence. Furthermore, this is the first study of its kind to specifically analyze hospital admissions and surgical procedures as a result of end stage ulcer disease. It should be emphasized that all patients indentified in this study were identified in the inpatient setting with having H. pylori infection as the primary admitting diagnosis. While the methods for detection are not available (nor do the authors suggest that this is pertinent for this analysis), the diagnoses identified in this study are definite.
Study limitations
Limitations of this analysis reflect inherent deficiencies of a nationwide, code based database. There is no accounting for other causes of ulcer disease such as malignancy, NSAIDs, steroids, and aspirin. Additionally, the surgical procedures described are not universally specific for the surgical management of ulcer disease and were determined at the discretion of the authors. Coding practices themselves may not reflect a completely accurate assessment of patient care rendered. Finally, it must be reinforced that we used trends in the incidence peptic ulcer disease, its complications, and treatments as surrogate markers for the influence of the identification of H. pylori as the major contributor to peptic ulcer disease. No direct link is possible to analyze.
Future directions
Major trends in disease patterns are difficult to identify in studies such as prospective trials and case control series; they commonly lack the temporal strength and sample size necessary to appreciate longitudinal changes. Nationwide databases provide an excellent platform to investigate these changes and would be optimally utilized by a continuous surveillance mechanism. Responses to healthcare legislation and policy, basic scientific discovery, landmark trial findings, and public health efforts could all be gauged using a similar analysis to that described in this manuscript.
CONCLUSION
The identification of H. pylori as the causative agent in the majority of peptic ulcer disease has revolutionized the understanding and management of the disease. Estimates from the Nationwide Inpatient Sample indicate that selected medical conditions and surgical procedures thought to be most specific to end-stage peptic ulcer disease have significantly decreased. Resident physician education objectives may need to be modified in light of these trends.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Grendell JH, Friedman SL, McQuaid KR. New York City: McGraw-Hill Professional; 2003. Current diagnosis and treatment in gastroenterology. [Google Scholar]
- 2.Malfertheiner P, Chan FK, McColl KE. Peptic ulcer disease. The Lancet. 2009;374:1449–61. doi: 10.1016/S0140-6736(09)60938-7. [DOI] [PubMed] [Google Scholar]
- 3.Huang J, Sridhar S, Hunt R. Role of Helicobacter pylori infection and non-steroidal anti-inflammatory drugs in peptic-ulcer disease: A meta-analysis. The Lancet. 2002;359:14–22. doi: 10.1016/S0140-6736(02)07273-2. [DOI] [PubMed] [Google Scholar]
- 4.Henry D, Lim LL, Rodriguez LA, Gutthann SP, Carson JL, Griffin M, et al. Variability in risk of gastrointestinal complications with individual non-steroidal anti-inflammatory drugs: Results of a collaborative meta-analysis. BMJ. 1996;312:1563–6. doi: 10.1136/bmj.312.7046.1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marshall BJ, Warren JR. Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration. Lancet. 1984;1:1311–5. doi: 10.1016/s0140-6736(84)91816-6. [DOI] [PubMed] [Google Scholar]
- 6.Mégraud F. A humble bacterium sweeps this year's Nobel Prize. Cell. 2005;123:975–6. doi: 10.1016/j.cell.2005.11.032. [DOI] [PubMed] [Google Scholar]
- 7.Borody TJ, Cole P, Noonan S, Morgan A, Lenne J, Hyland L, et al. Recurrence of duodenal ulcer and Campylobacter pylori infection after eradication. Med J Aust. 1989;151:431–5. doi: 10.5694/j.1326-5377.1989.tb101251.x. [DOI] [PubMed] [Google Scholar]
- 8.Summary of the NIH consensus. Helicobacter pylori in peptic ulcer disease. Md Med J. 1994;43:923–4. [PubMed] [Google Scholar]
- 9.Sonnenberg A. Time trends of ulcer mortality in Europe. Gastroenterol. 2007;132:2320–7. doi: 10.1053/j.gastro.2007.03.108. [DOI] [PubMed] [Google Scholar]
- 10.Post PN, Kuipers EJ, Meijer GA. Declining incidence of peptic ulcer but not of its complications: A nation-wide study in The Netherlands. Aliment Pharmacol Ther. 2006;23:1587–93. doi: 10.1111/j.1365-2036.2006.02918.x. [DOI] [PubMed] [Google Scholar]
- 11.Pérez-Aisa MA, Del Pino D, Siles M, Lanas A. Clinical trends in ulcer diagnosis in a population with high prevalence of Helicobacter pylori infection. Aliment Pharmacol Ther. 2005;21:65–72. doi: 10.1111/j.1365-2036.2004.02297.x. [DOI] [PubMed] [Google Scholar]
- 12.Lewis JD, Bilker WB, Brensinger C, Farrar JT, Strom BL. Hospitalization and mortality rates from peptic ulcer disease and GI bleeding in the 1990s: Relationship to sales of nonsteroidal anti-inflammatory drugs and acid suppression medications. Am J Gastroenterol. 2002;97:2540–9. doi: 10.1111/j.1572-0241.2002.06037.x. [DOI] [PubMed] [Google Scholar]
- 13.Lassen A, Hallas J, Schaffalitzky de Muckadell OB. Complicated and uncomplicated peptic ulcers in a Danish county 1993-2002: A population-based cohort study. Am J Gastroenterol. 2006;101:945–53. doi: 10.1111/j.1572-0241.2006.00518.x. [DOI] [PubMed] [Google Scholar]
- 14.Kang J, Tinto A, Higham J, Majeed A. Peptic ulceration in general practice in England and Wales 1994-98: Period prevalence and drug management. Aliment Pharmacol Ther. 2002;16:1067–74. doi: 10.1046/j.1365-2036.2002.01261.x. [DOI] [PubMed] [Google Scholar]
- 15.Kang JY, Elders A, Majeed A, Maxwell JD, Bardhan KD. Recent trends in hospital admissions and mortality rates for peptic ulcer in Scotland 1982-2002. Aliment Pharmacol Ther. 2006;24:65–79. doi: 10.1111/j.1365-2036.2006.02960.x. [DOI] [PubMed] [Google Scholar]
- 16.Higham J, Kang J, Majeed A. Recent trends in admissions and mortality due to peptic ulcer in England: Increasing frequency of haemorrhage among older subjects. Gut. 2002;50:460–4. doi: 10.1136/gut.50.4.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.HCUP Nationwide Inpatient Sample (NIS) Healthcare Cost and Utilization Project (HCUP) [Last cited on 1992]. Available from: http://www.hcup-us.ahrq.gov/nisoverview.jsp .
- 18.MMWR Morb Mortal Wkly Rep. Knowledge about causes of peptic ulcer disease - United States, March-April 1997. Centers for Disease Control and Prevention (CDC) 1997;46:985–7. [PubMed] [Google Scholar]
- 19.Delaney BC, Moayyedi P, Forman D. Initial management strategies for dyspepsia. Cochrane Database Syst Rev. 2003;2:CD001961. doi: 10.1002/14651858.CD001961. [DOI] [PubMed] [Google Scholar]
- 20.Delaney BC, Qume M, Moayyedi P, Logan RF, Ford AC, Elliott C, et al. Helicobacter pylori test and treat versus proton pump inhibitor in initial management of dyspepsia in primary care: Multicentre randomised controlled trial (MRC-CUBE trial) BMJ. 2008;336:651–4. doi: 10.1136/bmj.39479.640486.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hutter MM, Kellogg KC, Ferguson CM, Abbott WM, Warshaw AL. The impact of the 80-hour resident workweek on surgical residents and attending surgeons. Ann Surg. 2006;243:864–75. doi: 10.1097/01.sla.0000220042.48310.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Durkin E, Mcdonald R, Munoz A, Mahvi D. The impact of work hour restrictions on surgical resident education. J Surg Educ. 2008;65:54–60. doi: 10.1016/j.jsurg.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 23.Bland K, Stoll D, Richardson J, Britt L. Brief communication of the Residency Review Committee-Surgery (RRC-S) on residents’ surgical volume in general surgery. Am J Surg. 2005;190:345–50. doi: 10.1016/j.amjsurg.2005.06.036. [DOI] [PubMed] [Google Scholar]
- 24.Ferguson C, Kellogg K, Hutter M, Warshaw A. Effect of Work-hour Reforms on Operative Case Volume of Surgical Residents. Curr Surg. 2005;62:535–8. doi: 10.1016/j.cursur.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 25.Damadi A, Davis A, Saxe A, Apelgren K. ACGME duty-hour restrictions decrease resident operative volume: A 5-year comparison at an ACGME-accredited university general surgery residency. J Surg Educ. 2007;64:256–9. doi: 10.1016/j.jsurg.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 26.ACGME Program Requirements for Graduate Medical Education in Surgery. [Last cited 2009, Dec 31]. Available from: http://www.acgme.org/acWebsite/downloads/RRC_progReq/440_general_surgery_01012008_u08102008.pdf .


