Abstract
Adenosine has been implicated in suppressing the proinflammatory responses of classically activated macrophages induced by Th1 cytokines. Alternative macrophage activation is induced by the Th2 cytokines interleukin (IL)-4 and IL-13; however, the role of adenosine in governing alternative macrophage activation is unknown. We show here that adenosine treatment of IL-4- or IL-13-activated macrophages augments the expression of alternative macrophage markers arginase-1, tissue inhibitor of matrix metalloproteinase-1 (TIMP-1), and macrophage galactose-type C-type lectin-1. The stimulatory effect of adenosine required primarily A2B receptors because the nonselective adenosine receptor agonist 5′-N-ethylcarboxamidoadenosine (NECA) increased both arginase activity (EC50=261.8 nM) and TIMP-1 production (EC50=80.67 nM), and both pharmacologic and genetic blockade of A2B receptors prevented the effect of NECA. A2A receptors also contributed to the adenosine augmentation of IL-4-induced TIMP-1 release, as both adenosine and NECA were less efficacious in augmenting TIMP-1 release by A2A receptor-deficient than control macrophages. Of the transcription factors known to drive alternative macrophage activation, CCAAT-enhancer-binding protein β was required, while cAMP response element-binding protein and signal transducer and activator of transcription 6 were dispensable in mediating the effect of adenosine. We propose that adenosine receptor activation suppresses inflammation and promotes tissue restitution, in part, by promoting alternative macrophage activation.—Csóka, B., Selmeczy, Z., Koscsó, B., Németh, Z. H., Pacher, P., Murray, P. J., Kepka-Lenhart, D., Morris S. M., Jr., Gause, W. C., Leibovich, S. J., Haskó, G. Adenosine promotes alternative macrophage activation via A2A and A2B receptors.
Keywords: cancer, helminth infection, inflammation, wound healing, obesity
Macrophages are characterized by vast phenotypic plasticity, and investigating their heterogeneity has recently become the focus of a multitude of studies. This heterogeneity arises both during and after macrophage differentiation and is driven by specific tissue- and immune-related stimuli (1–3). In this regard, Th1 and Th2 effector T cells and their secretory products, microbial antigens, and tumor products all influence the phenotypic development of macrophage populations (4, 5). Macrophages can be categorized into two broad groups according to a classification scheme that is based on the cytokine environment that is present during macrophage activation (6, 7). Classic activation occurs in a Th1 cytokine environment that is replete with interferon (IFN)-γ or on recognition of pathogen-associated molecular patterns (PAMPs; LPS, lipoproteins, dsRNA, lipoteichoic acid, etc.) and endogenous “danger” signals (heat-shock proteins, etc.). The proinflammatory nature of these classically activated macrophages (caMφ)s is instrumental in protection against pathogens, and under certain conditions, also cancer cells. caMφs, which are also called M1 cells, exert antiproliferative and cytotoxic activities, which result partly from their ability to secrete reactive nitrogen and oxygen species (peroxynitrite, hydrogen peroxide, superoxide) and proinflammatory cytokines, such as IL-12 and tumor necrosis factor (TNF)-α.
Alternative activation takes place in a Th2 cytokine environment and imparts immunomodulatory and anti-inflammatory rather than proinflammatory properties on macrophages (7, 8). The term “alternatively activated macrophage” (aaMφ) sometimes is more widely used and includes various anti-inflammatory macrophage phenotypes induced by stimuli as diverse as immune complexes, IL-10, glucocorticoids, and apoptotic cells, which are collectively denoted M2 macrophages (9, 10). aaMφs are essential participants in tissue remodeling and the resolution of inflammation, and are prevalent in parasitic disease and during wound healing (11).
Exposure to Th2 cytokines, such as IL-4 and IL-13, triggers a specific gene expression pattern in macrophages, and the most prominent gene that is induced is arginase-1 (12, 13). Arginase-1 metabolizes arginine to urea and ornithine; ornithine can then be used for proline and collagen synthesis, which results in extracellular matrix deposition and fibrosis (14). Notably, arginase-1 can outcompete the other major arginine-utilizing enzyme, inducible nitric oxide (NO) synthase (iNOS), for the substrate in aaMφs and, thus, decrease NO production (8). Other genes that are often induced are genes whose products are involved in matrix remodeling, such as TIMP-1 (15). TIMP-1 regulates tissue remodeling by inhibiting extracellular matrix-degrading matrix metalloproteinases. In addition, TIMP-1 has complex effects on cell growth, and mutations in the matrix metalloproteinase-inhibitory domain of TIMP-1 fail to abrogate the effects of TIMP-1 on cell growth and survival. Finally, macrophage galactose-type C-type lectin (mgl)-1 (16), chitinase-like-3 (Ym1), and found in inflammatory zone (Fizz)1 (7) are also signature markers of aaMφs.
While the cytokine environment that leads to the development of aaMφs is well defined, much less is known about how “stressful” signals regulate the function of these cells. One of the most potent stress mediators present in an inflammatory environment is the purine nucleoside adenosine. Adenosine accumulates extracellularly in response to stresses, such as hypoxia and tissue injury, and increases in extracellular adenosine concentrations are detected during inflammation and wound healing (17–21). Extracellular adenosine accumulates at foci of injury and signals tissue injury to surrounding tissue in an autocrine and paracrine manner. In addition to its alarm signal function, adenosine elicits tissue responses that are generally organ protective (18). Adenosine triggers its cellular effects by binding to and activating one or more of 4 transmembrane adenosine receptors, designated A1, A2A, A2B, and A3 (22). Macrophages express adenosine receptors, which can dictate classical macrophage activation. For example, it has been shown that adenosine inhibits TNF-α, IL-6, and IL-12 release and augments IL-10 and vascular endothelial growth factor (VEGF) (23) production by LPS or bacteria-activated macrophages, and these effects are mediated through both A2A and A2B receptors (24–27). While the role of adenosine receptors in regulating classical macrophage activation has been studied in detail, the role of adenosine receptors in governing alternative macrophage activation remains unknown. Therefore, to address the role of adenosine in regulating alternative macrophage activation, we examined the effect of adenosine on arginase-1 and TIMP-1 expression in IL-4-activated macrophages. Our results demonstrate that extracellular adenosine promotes alternative macrophage activation.
MATERIALS AND METHODS
Drugs and reagents
Adenosine, the adenosine receptor agonists 2-chloro-N6-cyclopentyladenosine (CCPA), 2-p-(2-carboxyethyl)phenethyl-amino-5′-N-ethyl-carboxamidoadenosine (CGS21680), 1-[2-chloro-6-[[(3-iodophenyl)methyl]amino]-9H-purin-9-yl]-1-deoxy-N-methyl-β-d-ribofuranuron-amide (2-Cl-IB-MECA), and 5′-N-ethylcarboxamidoadenosine (NECA), as well as the A2B receptor antagonist 8-[4-[4-(4-chlorobenzyl)piperazide-1-sulfonyl)phenyl]]-1-propylxanthine (PSB0778), were purchased from Tocris Cookson (Ellisville, MO, USA). The p38 mitogen-activated protein kinase (MAPK) inhibitor SB203580 was purchased from Calbiochem (San Diego, CA, USA). Stock solutions of the various adenosine receptor ligands and SB203580 were prepared using dimethylsulphoxide. Murine recombinant IL-4 and IL-13 were from PeproTech (Rocky Hill, NJ, USA). Stock solutions of recombinant cytokines were prepared using sterile water.
Experimental animals and cell cultures
Male C57BL/6 and TLR4-knockout (KO; C57BL/10ScNJ) and wild-type (WT; C57BL/10ScSnJ) mice were obtained from the Jackson Laboratory (Bar Harbor, ME, USA). A2B receptor-KO mice on a C57BL/6 genetic background were acquired from Deltagen (San Mateo, CA, USA) and were bred as described previously (24, 28). A2A receptor-KO mice on a C57BL/6 genetic background were kindly provided by Dr. Joel Linden (La Jolla Institute for Allergy and Immunology, La Jolla, CA, USA). All mice were maintained in accordance with the recommendations of the U.S. National Institutes of Health Guide for the Care and Use of Laboratory Animals, and the experiments were approved by the New Jersey Medical School Animal Care Committee. Thioglycollate (TG) elicited mouse peritoneal macrophages, C/EBPβ-deficient and control immortalized macrophages (kind gifts from Dr. Jorge A. Albina, Rhode Island Hospital and Brown Medical School, Providence, RI, USA; refs. 29, 30), and RAW 264.7 macrophages [American Type Culture Collection (ATCC), Manassas, VA, USA] were grown in Dulbecco's modified Eagle medium supplemented with 10% fetal bovine serum, 50 U/ml penicillin, 50 μg/ml streptomycin, and 1.5 mg/ml sodium bicarbonate in a humidified atmosphere of 95% air and 5% CO2.
RNA extraction, cDNA synthesis, and real-time polymerase chain reaction (PCR)
Total RNA was extracted from macrophages and reverse transcribed, as described previously (24). For detecting arginase-1, TIMP-1, and mgl-1 mRNA, a commercially available real-time PCR kit was used (Applied Biosystems, Foster City, CA, USA), and all data were normalized to constitutive rRNA (18S) values. Oligonucleotides used for real-time PCR are shown in Table 1. The Applied Biosystems 7700 sequence detector was used for amplification of target sequences, and quantitation of differences between treatment groups was determined using comparative threshold cycle (CT) method.
Table 1.
Oligonucleotide sequences for real-time PCR
| Primer | Sequence |
|---|---|
| arginase-1 | F :5′-CAGAAGAATGGAAGAGTCAG-3′ |
| R :5′CAGATATGCAGGGAGTCACC-3′ | |
| TIMP-1 | F :5′-TCCTCTTGTTGCTATCACTGATAGCTT-3′ |
| R :5′-CGCTGGTATAAGGTGGTCTCGTT-3′ | |
| mgl-1 | F :5′-CCTCCAGAACTCAAGGATGC-3′ |
| R :5′-GATCCAATCACGGAGACGAC-3′ | |
| 18S | F :5′-GTAACCCGTTGAACCCCATT-3′ |
| R :5′-CCATCCAATCGGTAGTAGCG-3′ |
F, forward; R, reverse.
Transient transfection of RAW 264.7 cells with arginase-1 promoter-luciferase construct, C/EBP luciferase construct, and luciferase assay
RAW 264.7 cells were transiently transfected using FuGene 6.0 transfection reagent (Roche, Indianapolis, IN, USA). For transfection, 0.5 × 106/ml cells were seeded in a 24-well plate. The next day, the cells were transfected with 0.4 μg of arginase-1 reporter plasmids or C/EBP reporter plasmid (Stratagene, Santa Clara, CA, USA). The arginase-1 luciferase reporter constructs were created by cloning −3810/−31 promoter fragment into the pGL3-basic vector (Promega, Madison, WI, USA; ref. 31). All transfections were performed at 37°C overnight, and the following day the cells were washed with medium and treated with IL-4 and adenosine for 4 or 8 h. For reporter assays, whole-cell extracts were prepared using 80 μl of 1× passive lysis buffer (Promega). Luciferase activity was determined using 20 μl of cell extract.
Lentiviral transduction and selection of stable CREB shRNA-expressing clones of RAW 264.7 cells
RAW 264.7 cells placed in 12-well plates (5×104 cells/well) were transduced with Mission lentiviral particles containing CREB-specific shRNA or nontargeting shRNA (Sigma-Aldrich, St. Louis, MO, USA) in the presence of 8 μg/ml hexadimethrine bromide. (shRNA nucleotide sequences are shown in Table 2). The multiplicity of infection was 4 for both transductions. After overnight incubation, the supernatants were replaced with complete cell culture medium, and the cells were incubated for an additional 48 h. Transduced cells were selected by culturing in the presence of 4 μg/ml puromycin. The efficacy of silencing was tested using Western blotting.
Table 2.
shRNA sequences for CREB down-regulation
| Target | Sequence |
|---|---|
| Region 32 | 5′-CCGGAGCAAGAGAATGTCGTAGAAACTCGAGTTTCTACGACATTCTCTTGCTTTTTTG-3′ |
| Region 33 | 5′-CCGGACTGATGGACAGCAGATTCTACTCGAGTAGAATCTGCTGTCCATCAGTTTTTTG-3′ |
| Nontargeting | 5′-CCGGCAACAAGATGAAGAGCACCAACTCGAGTTGGTGCTCTTCATCTTGTTGTTTTT-3′ |
Underscores indicate shRNA target or nontargeting sequences.
Analysis of phospho-p38, phospho-STAT-6, phospho-Jak1/3, phospho-Shc, phospho-PI3K, phospho-Akt, phospho-p42/44, phospho-JNK, CREB, and arginase-1 protein abundance using Western blotting
Detection of protein kinase activation and arginase-1 and CREB levels was conducted using Western blotting employing antibodies against the phosphorylated, active, or nonphosphorylated forms of the proteins. Phospho-p38, phospho-STAT-6, phospho-Janus kinase (Jak) 1/3, phospho-SHC-adaptor protein (Shc), phospho-phosphatidylinositol 3-kinase (PI3K), phospho-Akt, phospho-p42/44, phospho-c-jun terminal kinase (JNK), CREB and arginase-1 protein levels were analyzed using 20–30 μg of cellular extracts using antibodies raised against doubly phosphorylated phospho-p38 (Cell Signaling, Danvers, MA, USA), phospho-STAT6 (Abcam, Cambridge, MA, USA), doubly phosphorylated phospho-Jak1 (Cell Signaling), phospho-Jak3 (Abcam), phospho-Shc (Cell Signaling), phospho-Akt (Cell Signaling), phospho-PI3K (Cell Signaling), doubly phosphorylated phospho-p42/44 (Cell Signaling), doubly phosphorylated phospho-JNK (Cell Signaling), CREB (Cell Signaling), and arginase-1 (Santa Cruz Biotechnology, Santa Cruz, CA, USA).
Determination of arginase activity from macrophage cell extract
Macrophages in 96-well plates (2×106/ml) were treated with PSB0778 or with intracellular pathway inhibitors and then either with adenosine or various adenosine receptor agonists, followed by addition of IL-4 or IL-13. At the end of the incubation period, cell extracts were prepared from 2 × 105 cells in 50 μl of 10 mM Tris-HCl (pH 7.4) containing 0.4% Triton X-100. After centrifugation at 2500 g for 30 min, arginase activity in the supernatants of cell extracts was determined using a commercially available arginase assay kit (QuantiChrom arginase assay kit; Bioassy Systems, Hayward, CA, USA). The measured arginase activity was normalized for 2 × 105 cells.
TIMP-1 enzyme-linked immunosorbent assay (ELISA)
Murine macrophages in 96-well plates (2×106/ml) were treated with PSB0778 or with intracellular pathway inhibitors, and then either with adenosine or various adenosine receptor agonists, followed by addition of IL-4 or IL-13. TIMP-1 levels in cell supernatants were determined by ELISA (mouse TIMP-1 Duoset ELISA kit; R&D Systems, Minneapolis, MN, USA).
Statistical analysis
Values in the figures are expressed as means ± se of n observations. Statistical analysis of the data was performed by Student's t test or 1-way analysis of variance followed by the Dunnett test, as appropriate.
RESULTS
Adenosine augments IL-4- and IL-13-induced alternative macrophage activation by a TLR4-independent mechanism
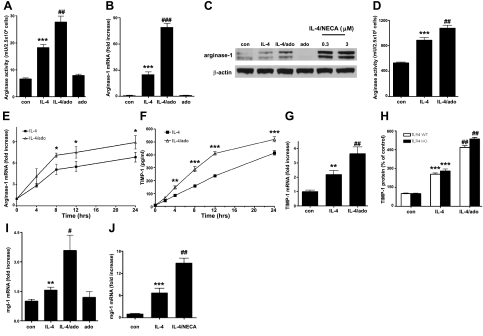
To begin to examine the effect of adenosine on alternative macrophage activation, RAW 264.7 macrophages were treated with adenosine immediately prior to treatment with IL-4. Figure 1 shows that adenosine augmented arginase activity (Fig. 1A) as well as mRNA and protein levels of arginase-1 (Fig. 1B, C) in IL-4-treated macrophages, but not in control cells. To explore the effect of adenosine on alternatively activated primary macrophages, TG elicited peritoneal macrophages from C57BL/6 mice were treated with adenosine and IL-4. Similar to RAW 264.7 macrophages, adenosine increased both IL-4-induced arginase activity (Fig. 1D) and mRNA expression (Fig. 1E) in peritoneal macrophages.
Figure 1.
Adenosine (ado) augments alternative macrophage activation. A) Adenosine up-regulates IL-4-induced arginase activity in RAW 264.7 macrophages. RAW 264.7 macrophages were stimulated with 5 ng/ml IL-4 and treated with 100 μM adenosine for 8 h, and then arginase activity was measured from the cell lysates. Results are representative of ≥3 experiments; n = 6/experiment. ***P < 0.001 vs. control (con) group, ##P < 0.01 vs. IL-4. B) Adenosine augments IL-4-stimulated arginase-1 mRNA accumulation in RAW 264.7 cells. RAW 264.7 macrophages were treated with 100 μM adenosine and 5 ng/ml IL-4, and arginase-1 mRNA levels were measured by real-time PCR using RNA isolated 3 h after stimulating with IL-4 and adenosine. Results are representative of ≥3 experiments; n = 6/experiment. ***P < 0.001 vs. con, ###P < 0.001 vs. IL-4. C) Adenosine or NECA enhances IL-4-stimulated arginase-1 protein expression in RAW 264.7 cells. RAW 264.7 cells were challenged with IL-4 in the presence or absence of adenosine or NECA for 8 h, and arginase-1 protein level was determined from cell extracts using Western blotting with antibodies raised against arginase-1. β-Actin was utilized as internal control. Blots are representative of 3 separate experiments. D) Adenosine increases arginase activity of IL-4-challenged peritoneal macrophages. Peritoneal macrophages were obtained from C57BL/6 mice, and were treated with 5 ng/ml IL-4 and 100 μM adenosine. After 24 h of incubation, arginase activity was determined from whole-cell lysates. Results are representative of ≥3 experiments; n = 6/experiment. ***P < 0.001 vs. con, ##P < 0.01 vs. IL-4. E) Adenosine up-regulates IL-4-induced arginase-1 mRNA accumulation in peritoneal macrophages. Peritoneal macrophages were obtained from male C57BL/6 mice and were treated with 5 ng/ml IL-4 and 100 μM adenosine. After 4, 8, 12, or 24 h of incubation, arginase-1 mRNA abundance was measured using real-time PCR. Results are representative of ≥3 experiments; n = 6/experiment. *P < 0.05 vs. IL-4. F) Adenosine enhances IL-4-induced TIMP-1 release by mouse peritoneal macrophages. Peritoneal macrophages were stimulated with IL-4 and treated with 100 μM adenosine for the indicated times, and then TIMP-1 was measured from the supernatants using ELISA. Results are representative of ≥3 experiments; n = 4/experiment. **P <0.01, ***P < 0.001 vs. IL-4. G) Adenosine increases IL-4-induced TIMP-1 mRNA accumulation. Peritoneal macrophages were stimulated with 100 μM adenosine and 5 ng/ml IL-4, and TIMP-1 mRNA levels were measured by real-time PCR using RNA isolated 8 h after adenosine/IL-4. Results are representative of ≥3 experiments; n = 6/experiment. **P < 0.01 vs. con, ##P < 0.01 vs. IL-4. H) Adenosine up-regulates IL-4-induced TIMP-1 production by both TLR4-WT and -KO macrophages. Peritoneal macrophages were obtained from TLR4-KO and WT mice and were treated with IL-4 or IL-4 and adenosine for 24 h, after which procedure TIMP-1 production was determined from the supernatants. Results are representative of ≥2 experiments; n = 4/experiment. ***P < 0.001, ##P < 0.01 vs. corresponding IL-4-treated groups. I, J) Adenosine (I) or NECA (J) augments IL-4-stimulated mgl-1 mRNA accumulation in RAW 264.7 cells. RAW 264.7 macrophages were treated with 100 μM adenosine or 3 μM NECA and 5 ng/ml IL-4, and mgl-1 mRNA levels were measured by real-time PCR using RNA isolated 3 h after stimulating with IL-4 and adenosine or NECA. Results are representative of ≥3 experiments; n = 4/experiment. **P < 0.01, ***P < 0.001 vs. con; #P < 0.05, ##P < 0.01 vs. IL-4. Results are shown as means ± se.
We next studied the effect of adenosine receptor activation on TIMP-1 production. We found that IL-4 induced both TIMP-1 release into the medium and TIMP-1 mRNA accumulation in peritoneal macrophages. In addition, adenosine increased both IL-4-induced TIMP-1 release and mRNA accumulation (Fig. 1F, G). The effect of IL-4 or adenosine/IL-4 did not require TLR4, because IL-4 induced, and adenosine enhanced IL-4-induced TIMP-1 release by both WT and TLR4-KO macrophages (Fig. 1H). In addition, adenosine or NECA augmented mgl-1 mRNA accumulation in IL-4-challenged macrophages (Fig. 1I, J).
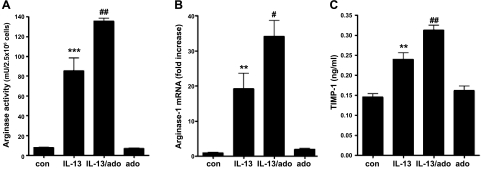
To confirm the stimulatory effect of adenosine on alternative macrophage activation, we studied the effect of adenosine on IL-13-induced arginase-1 mRNA accumulation and arginase activity in RAW 264.7 macrophages, as well as on IL-13-stimulated TIMP-1 expression in peritoneal macrophages. We found that adenosine up-regulated IL-13-induced arginase activity and arginase-1 mRNA expression (Fig. 2A, B) as well as TIMP-1 production (Fig. 2C).
Figure 2.
Adenosine (ado) enhances arginase activity and TIMP-1 production by IL-13-activated macrophages. A) Adenosine up-regulates IL-13-stimulated arginase activity in RAW 264.7 macrophages. RAW 264.7 macrophages were challenged with 5 ng/ml IL-13 and treated with 100 μM adenosine for 8 h, and then arginase activity was measured from the cell lysate. B) Adenosine augments IL-13-evoked arginase-1 mRNA accumulation. RAW 264.7 macrophages were challenged with 5 ng/ml IL-13 and treated with 100 μM adenosine for 4 h, and mRNA abundance was measured using real-time PCR. C) Adenosine enhances IL-13-induced TIMP-1 release by peritoneal macrophages. Peritoneal macrophages were stimulated with IL-13 and treated with adenosine for 24 h, and then TIMP-1 levels were measured from the supernatants using ELISA. Results are shown as means ± se and are representative of ≥3 experiments; n = 6/experiment. **P < 0.01, ***P < 0.001 vs. control (con); #P < 0.05, ##P < 0.01 vs. IL-13.
Because adenosine was more efficacious in increasing arginase activity and failed to up-regulate TIMP-1 release (data not shown) in RAW macrophages, in the following experiments we used RAW and peritoneal macrophages to study the mechanisms of the adenosine-induced up-regulation of arginase and TIMP-1, respectively.
Role of A2A and A2B adenosine receptors in mediating the stimulatory effect of adenosine on alternative macrophage activation
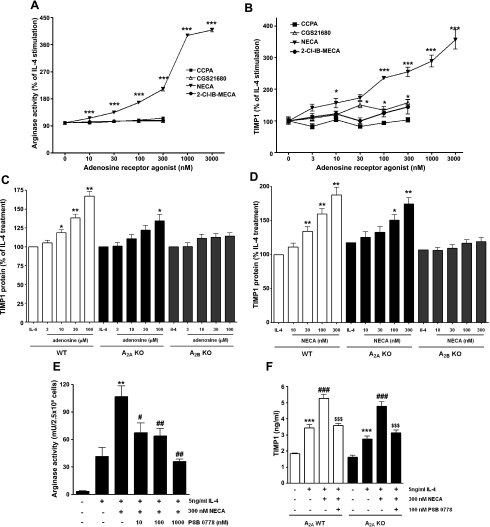
To investigate which adenosine receptors are responsible for mediating the stimulatory effect of adenosine on IL-4-induced arginase activity and TIMP-1 production, we pretreated macrophages with specific adenosine receptor agonists before IL-4 stimulation. We found that the nonselective adenosine receptor agonist NECA increased both arginase activity (EC50=261.8 nM) and TIMP-1 production (EC50=80.67 nM) by IL-4-stimulated macrophages (Fig. 3A, B). Furthermore, NECA increased IL-4-induced arginase-1 protein expression (Fig. 1C). The EC50 values of NECA were indicative of a role for A2B receptors (32, 33). In contrast, relevant concentrations of the A1 receptor agonist CCPA, and A3 receptor-specific agonist 2-Cl-IB-MECA failed to mimic the stimulatory effect of adenosine, and the A2A receptor agonist CGS21680 was marginally effective at increasing TIMP-1 release but not arginase activity (Fig. 3A, B). To further investigate the role of A2B receptors, we also employed A2B receptor-KO mice. The results confirmed that the A2B receptor is important for the stimulatory effect of adenosine on IL-4-induced TIMP-1 production, because both adenosine and NECA were incapable of up-regulating TIMP-1 production by macrophages isolated from A2B-KO mice (Fig. 3C, D). Similar to genetic blockade of A2B receptors, pharmacological antagonism by 100 nM PSB0778 inhibited both the NECA enhancement of arginase activity and TIMP-1 production (Fig. 3E, F). The effect of PSB0778 was independent of A2A receptors, because PSB0778 also prevented the NECA augmentation of TIMP-1 release in A2A receptor-KO macrophages (Fig. 3F).
Figure 3.
A2B and, to a lesser extent, A2A receptors mediate the stimulatory effect of adenosine on IL-4-induced arginase activity and TIMP-1 production. A) Effect of adenosine receptor agonists on IL-4-induced arginase activity in RAW 264.7 macrophages. RAW 264.7 macrophages were stimulated with IL-4 and treated with adenosine receptor agonists for 8 h, and then arginase activity was measured from the cell lysate. ***P < 0.001 vs. vehicle. B) Effect of adenosine receptor agonists on IL-4-stimulated TIMP-1 release by peritoneal macrophages. Peritoneal macrophages were treated with IL-4 and adenosine receptor agonists for 24 h, and TIMP-1 concentrations were determined in the supernatants. *P < 0.05, ***P < 0.001 vs. vehicle. C, D) Adenosine (C) and NECA (D) enhance TIMP-1 production by IL-4-challenged WT and, to a lesser extent, A2A-KO mice. Both adenosine and NECA are ineffective in A2B-KO peritoneal macrophages. A2A-KO, A2B-KO, and WT peritoneal macrophages were stimulated with 5 ng/ml IL-4 and treated with adenosine (C) or NECA (D) for 24 h, and then TIMP-1 levels were measured from the supernatants using ELISA. *P < 0.05, **P < 0.01 vs. IL-4. E) Pharmacological A2B receptor blockade using PSB0778 prevents the NECA enhancement of arginase activity in IL-4-stimulated RAW 264.7 macrophages. RAW 264.7 macrophages were pretreated for 30 min with 10–1000 nM PSB0778; following this time period, cells were treated with 300 nM NECA immediately before IL-4 stimulation. Cells were incubated for an additional 8 h, at which point cell lysates were prepared for arginase measurements. **P < 0.01 vs. IL-4; #P < 0.05, ##P < 0.01 vs. IL-4/NECA. F) Pharmacological A2B receptor blockade inhibits the NECA augmentation of TIMP-1 production by IL-4-induced WT and A2A-KO macrophages. WT and A2A-KO peritoneal macrophages were pretreated for 30 min with 100 nM PSB0778; following this time period, cells were treated with 300 nM NECA immediately before IL-4 stimulation. Cells were incubated for an additional 24 h, at which point supernatants were harvested. TIMP-1 levels were measured from the supernatants using ELISA. ***P < 0.001 vs. vehicle; ###P < 0.001 vs. IL-4; $$$P < 0.001 vs. IL-4/NECA. Results are shown as means ± se and are representative of ≥3 experiments; n = 6/experiment.
PSB0778 prevented the NECA enhancement of TIMP-1 release in WT cells (Fig. 3F), which could be construed as pointing to an exclusive role for the A2B receptor in mediating the effect of adenosine. However, because PSB0778 has not been pharmacologically characterized in murine systems in detail and because A2A receptors have been widely implicated in regulating macrophage function (34), we further studied the role of A2A receptors by employing A2A receptor-KO mice. Our results indicated that the A2A receptor contributed, although to a lesser degree, to the up-regulation of TIMP-1 production, as both adenosine and NECA were less efficacious in up-regulating TIMP-1 production by macrophages obtained from A2A-KO mice than from their WT littermates (Figs. 3C, D).
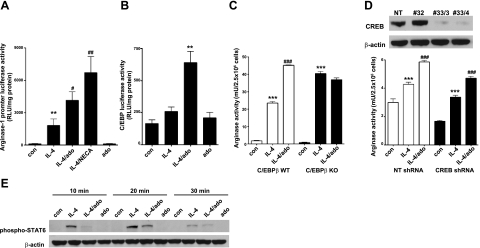
C/EBPβ is required but CREB and STAT-6 are dispensable for the stimulatory effect of adenosine on arginase-1 expression in IL-4-stimulated macrophages
Since the mechanisms of IL-4 activation of arginase-1 transcription have been investigated in detail (31, 35, 36), and because nothing is known about how IL-4 affects TIMP-1 transcription, we studied the mechanism of action of adenosine in enhancing arginase transcription. Using a previously described arginase promoter luciferase construct (31), we showed that adenosine as well as NECA enhanced IL-4-induced arginase-1 promoter activity, (Fig. 4A). We then focused our effort on 3 transcription factors that have been implicated in regulating alternative macrophage activation, C/EBPβ, CREB, and STAT-6 (31, 35, 36). Since we recently demonstrated that adenosine up-regulates bacteria-induced C/EBPβ activation (24), we first examined the role of C/EBPβ. We found that neither IL-4 nor adenosine alone was able to increase C/EBP transcriptional activity; however, adenosine and IL-4 together synergistically induced C/EBP transcriptional activity (Fig. 4B). To provide further insight into the role of C/EBPβ in regulating arginase-1 production, C/EBPβ-WT and -KO immortalized macrophage cell lines (29, 30) were stimulated with IL-4 and adenosine, and arginase activity was measured. As Fig. 4C shows, IL-4 increased arginase-1 activity by both WT and KO macrophages, and adenosine up-regulated this activity by ∼2-fold in WT but not KO macrophages. It is noteworthy that similar to results of a previous study (29), IL-4 induced a more pronounced increase in arginase activity in C/EBPβ-KO than WT cells, which may be a consequence of compensatory up-regulation of other C/EBP factors. These data together identify C/EBPβ as a major transcription factor mediating the stimulatory effect of adenosine on arginase-1 expression in IL-4-activated macrophages.
Figure 4.
C/EBPβ is required, but CREB and STAT-6 are dispensable, for the stimulatory effect of adenosine (ado) on arginase-1 expression in IL-4-stimulated macrophages. A) Adenosine or NECA augments IL-4-induced arginase-1 promoter activity in macrophages. To measure arginase-1 promoter activity, RAW 264.7 cells were transiently transfected with a promoter-luciferase reporter construct containing −3810/−31 fragment of the arginase-1 promoter in a pGL3-basic vector. Cells were treated with IL-4 and adenosine or NECA for 8 h. Luciferase reporter activities were normalized to protein content. Results are representative of ≥3 experiments; n = 5/experiment. **P < 0.01 vs. control; #P < 0.05, ##P < 0.01 vs. IL-4. B) Adenosine synergizes with IL-4 to up-regulate C/EBP-driven promoter activity in RAW 264.7 macrophages. RAW 264.7 macrophages were transfected with a luciferase reporter vector driven by C/EBP (pC/EBP-luc). Cells were treated with IL-4 and adenosine (ado; 100 μM) for 4 h; cells were then lysed, and luciferase activity was determined. Luciferase reporter activities were normalized to protein concentration. Results are representative of ≥3 experiments; n = 4/experiment. **P < 0.01 vs. IL-4 or ado. C) Adenosine fails to increase arginase activity in IL-4-activated C/EBPβ-deficient macrophages. C/EBPβ-WT and -KO macrophages were activated with IL-4 or IL-4 plus adenosine, and arginase activity was determined from the cell lysate after 8 h of stimulation. Results are representative of ≥3 experiments; n = 6/experiment. ***P < 0.001 vs. control (con); ###P < 0.001 vs. IL-4 in C/EBPβ WT. D) Stimulatory effect of adenosine on arginase activity is CREB independent in IL-4-activated macrophages. Top panel: RAW 264.7 cells were transduced with Lentivirus particles containing either CREB-specific shRNA or nontargeting (NT) shRNA. CREB-silenced or NT-transduced cells were selected in the presence of puromycin. CREB protein levels were evaluated by Western blotting using protein extract isolated from NT shRNA- and CREB shRNA-transduced RAW 264.7 macrophages. Note that silencing of CREB expression was inefficient in clone 32. Blots are representative of ≥4 experiments. Bottom panel: CREB-silenced (clone 33/4 is shown) or NT-transduced macrophages were stimulated with IL-4 and adenosine, and arginase activity was measured from the cell extracts prepared at the end of the incubation period. Results are representative of ≥3 experiments; n = 6/experiment. ***P < 0.001 vs. con; ###P < 0.001 vs. IL-4. E) Adenosine diminishes IL-4-induced STAT-6 activation. Peritoneal macrophages were challenged with 5 ng/ml IL-4 in the presence or absence of adenosine for the indicated times, and STAT-6 phosphorylation, which is indicative of activation, was determined from cell extracts taken at the end of the incubation period, using Western blotting with antibodies raised against the active phosphorylated STAT-6. β-Actin was employed as internal control. Blots are representative of 3 separate experiments. Results are shown as means ± se.
A recent study documented that CREB-mediated C/EBPβ induction is required for the up-regulation of alternative activation-specific genes, including arginase-1 (35). Furthermore, adenosine activates CREB in macrophages (37). Therefore, utilizing lentivirally delivered shRNA to down-regulate CREB expression, we assessed whether CREB is required for the stimulatory effect of adenosine on IL-4-induced arginase expression. We first confirmed using Western blotting, that cells that were stably transduced with lentivirally delivered CREB shRNA expressed negligible levels of CREB protein (clones 33/3 and 33/4 but not clone 32) when compared to cells transduced with a control vector expressing nontargeting (NT) sequences (Fig. 4D, top panel). We then stimulated macrophages with IL-4 or adenosine plus IL-4 and measured arginase activity. As Fig. 4D (bottom panel) shows, arginase activity was induced by IL-4 and was further up-regulated by adenosine in both NT shRNA- and CREB shRNA-expressing macrophages. These results indicate that CREB is not necessary for the stimulatory effect of adenosine on arginase expression. In addition, we excluded a role for STAT-6 in mediating the augmenting effect of adenosine on arginase activity, as we found that IL-4-induced STAT-6 activation was not increased but actually decreased by adenosine (Fig. 4E).
Role of intracellular kinases in mediating the effect of adenosine on alternative macrophage activation
Previous studies have shown that both IL-4 and adenosine can activate various intracellular kinases, including Jak1, Jak 3, Shc, PI3K, and Akt, as well as p38, p42/44, and JNK MAPK. To dissect the role of these kinases in mediating the stimulatory effect of adenosine on alternative macrophage activation, we first sought to detect the active, phosphorylated forms of these kinases, using Western blot analysis. We found that both adenosine and IL-4, alone and in combination, failed to induce Jak1/3, Shc, PI3K, Akt, p42/44, and JNK activation (data not shown), but adenosine alone and in combination with IL-4, but not IL-4 alone, up-regulated p38 activation (Fig. 5A). We then pretreated macrophages with SB203580, a selective p38 pathway inhibitor, 30 min prior to adenosine and IL-4 exposure to examine the role of p38. SB203580 prevented the increasing effect of adenosine on both arginase activity (Fig. 5B) and TIMP-1 release (Fig. 5C), confirming that p38 mediates the stimulatory effect of adenosine on alternative macrophage activation.
Figure 5.
p38 activation is required for the stimulatory effect of adenosine on alternatively activated macrophages. A) Adenosine increases p38 activation. Macrophages were treated with IL-4 in the presence or absence of adenosine (ado) for 20 min. p38 activation was determined from cell extracts using immunoblotting with antibodies raised against the active, doubly phosphorylated form of p38. β-Actin was used as internal control (con). Blots are representative of 3 separate experiments. B) Inhibition of the p38 pathway prevents the stimulatory effect of adenosine on arginase activity in IL-4-activated macrophages. RAW 264.7 macrophages were pretreated for 30 min with SB203580 (p38 pathway inhibitor) before adding 100 μM adenosine and 5 ng/ml IL-4. After 8 h of incubation, arginase activities were assessed. ***P < 0.001 vs. IL-4; ##P < 0.01 vs. IL-4/adenosine. C) p38 pathway inhibition prevents the stimulatory effect of adenosine on TIMP-1 production by IL-4-stimulated macrophages. Peritoneal macrophages were pretreated for 30 min with SB203580 before adding adenosine and IL-4. After 24 h, supernatants were collected. TIMP-1 levels were assessed from the supernatants using ELISA. ***P < 0.001 vs. IL-4 alone; ##P < 0.01 vs. ado + IL-4. Results are shown as means ± se and are representative of ≥3 experiments; n = 6/experiment.
DISCUSSION
Macrophages can respond to endogenously released mediators that are rapidly generated subsequent to infection or injury. Adenosine has been established as one of the most prominent endogenous mediators that regulate classical macrophage activation, and the current consensus is that the regulatory effects of adenosine on macrophages are mediated predominantly by A2A and A2B receptors (23, 24, 27, 34, 38–42). Adenosine has been shown to be a broad inhibitor of the proinflammatory consequences of classical macrophage activation. The inhibitory effects of adenosine include suppression of cytokine/chemokine production (25, 34, 43, 44) and iNOS induction (43, 45). In contrast, our results with IL-4- and IL-13-stimulated macrophages show, for the first time, that adenosine enhances alternative macrophage activation. The effects of adenosine in promoting alternative macrophage activation are less broad than the wide-ranging inhibitory effects of adenosine on classical macrophage activation, as adenosine increased the expression of key alternative markers arginase-1, TIMP-1, and mgl-1, but not that of Ym1 and Fizz1 (data not shown).
The stimulatory effects of adenosine on alternative macrophage activation are mediated predominantly by A2B receptors, which contrasts with the preeminent role of A2A receptors in regulating classical macrophage activation (34). This preeminent role of A2B receptors was confirmed by the observations that the stimulatory effects of adenosine and NECA on arginase expression and TIMP-1 release were completely prevented by both A2B-KO and pharmacological A2B antagonism. In addition, NECA was by far the most potent agonist of all the adenosine receptor agonists tested, which further incriminates the A2B receptor (46). A lesser involvement of A2A receptors is underscored by our results showing that both adenosine and NECA were less efficacious in increasing TIMP-1 production by macrophages isolated from A2A-KO mice as compared to their WT counterparts. It is noteworthy that although CGS21680 had a marginal, albeit significant, increasing effect on TIMP-1 production, it failed to augment arginase activity. Thus, A2A and A2B receptors differentially regulate distinct features of alternative macrophage activation.
We found that adenosine up-regulated IL-4-induced mRNA and protein accumulation of both arginase-1 and TIMP-1. In addition, similar to its stimulatory effect on arginase-1 mRNA accumulation (Fig. 1B, D), adenosine or NECA enhanced IL-4-induced arginase-1 promoter activity. Previous studies have proposed that arginase-1 promoter activity in macrophages is regulated by STAT-6 and C/EBPβ (31, 36, 47, 48). Since adenosine decreased IL-4-induced STAT-6 activation (Fig. 4E), we concluded that STAT-6 activation does not mediate the up-regulation of arginase-1 following adenosine treatment. In contrast, because IL-4-induced C/EBPβ-deficient macrophages failed to up-regulate arginase activity following adenosine exposure, we conclude that C/EBPβ mediates the stimulatory effect of adenosine on arginase-1 expression. This notion is supported by our data that adenosine synergizes with IL-4 to up-regulate C/EBP transcriptional activity. This conclusion, together with our previous observation that C/EBPβ is required for the enhancing effect of adenosine on Eschericia coli-induced IL-10 production (24), is consistent with the idea that C/EBPβ represents an important focal point, which orchestrates the effects of adenosine in macrophages (49).
It was reported recently that binding of CREB to C/EBPβ-promoter elements is critical for the activation of C/EBPβ-induced arginase-1 transcription in infiltrating macrophages following muscle injury (35). Moreover, we showed that adenosine enhances CREB transcriptional activity in macrophages (37). Based on these observations and previous data showing that cAMP can up-regulate arginase-1 expression (50), we hypothesized that adenosine should up-regulate IL-4-induced arginase activity via CREB activation. However, we excluded a role for CREB in this up-regulation, as shRNA-mediated CREB knockdown in macrophages failed to reverse the adenosine-increased arginase activity in IL-4-induced macrophages. Nevertheless, it is possible that cAMP contributed to the effect of adenosine in enhancing alternative macrophage activation in a CREB-independent fashion. Further studies are needed to determine the role of cAMP in mediating the stimulatory effect of adenosine receptor activation on alternative macrophage activation.
MAPKs are important for transmitting extracellular stressful signals toward the nucleus. IL-4 has been shown to induce p42/44 and JNK activation in certain cell types, including monocytes (51), airway epithelial cells (52), and neutrophils (53). In addition, adenosine stimulates p42/44 and JNK activation in various immune and nonimmune cell types (22, 49) However, we found that neither IL-4 nor adenosine activated p42/44 and JNK in macrophages. IL-4 also activates p38 MAPK signaling in a cell type-dependent manner; IL-4 increased p38 activation in a murine macrophage cell line but failed to influence p38 activation in B- and T-cell lines (54). In addition, both A2A and A2B receptors can activate MAPK signaling (46), and adenosine has been reported to be capable of activating p38 in macrophages (24, 37, 55). We found that although IL-4 had no effect on p38 activation, adenosine alone or in combination with IL-4 increased p38 activation (Fig. 5A). In addition, inhibition of the p38 pathway prevented the stimulatory effect of adenosine on IL-4-induced arginase activity and TIMP-1 release (Fig. 5B, C). Since p38 was also essential for the stimulatory effect of adenosine on IL-10 production by bacteria- and LPS-stimulated macrophages (24, 27), we propose that p38 is another central factor in mediating the regulatory effects of adenosine on both classical and alternative macrophage activation.
As noted in Results, due to the fact that adenosine failed to up-regulate TIMP-1 secretion by RAW 264.7 macrophages, we did not study in a detailed manner the intracellular mechanisms of how adenosine receptor activation augments TIMP-1 release. It is plausible that distinct intracellular pathways mediate the augmenting effect of adenosine on TIMP-1 production vs. arginase expression. Further studies are warranted to delineate the intracellular signaling pathways leading to the stimulatory effect of adenosine on TIMP-1 release by aaMφs.
aaMφs are important for defense against extracellular parasites (56). In this regard, our data that A2B receptors augment alternative macrophage activation are in agreement with our unpublished observations that A2B receptors are crucial for protection against Heligmosomoides polygyrus (unpublished results). In certain disease situations, however, aaMφs can contribute to the progression of disease. For example, it has been proposed that aaMφs activated by IL-4 and IL-13 during asthma and chronic obstructive pulmonary disease contribute significantly to airway remodeling and lung fibrosis leading to lung dysfunction (7, 8, 56). In addition, aaMφs are hijacked by tumor cells to function as suppressors of antitumor T-cell responses and stimulators of tumor angiogenesis (8, 57). In this study, we demonstrate that extracellular adenosine, acting through A2B and, to a lesser extent, A2A receptors, up-regulates alternative macrophage activation. Based on these observations, we propose adenosine receptors as therapeutic targets for disease states governed by alternative macrophage activation, such as parasite infection, asthma, cancer, and wound healing.
Acknowledgments
This work was supported by U.S. National Institutes of Health (NIH) grants R01GM66189 and R01GM57384, and the NIH Intramural Research Program, National Institute on Alcohol Abuse and Alcoholism, as well as the Hungarian Research Fund (CK 78275). The authors declare no competing financial interests.
REFERENCES
- 1. Gordon S., Taylor P. R. (2005) Monocyte and macrophage heterogeneity. Nat. Rev. Immunol. 5, 953–964 [DOI] [PubMed] [Google Scholar]
- 2. Kuroda E., Kito T., Yamashita U. (2002) Reduced expression of STAT4 and IFN-gamma in macrophages from BALB/c mice. J. Immunol. 168, 5477–5482 [DOI] [PubMed] [Google Scholar]
- 3. Mills C. D., Kincaid K., Alt J. M., Heilman M. J., Hill A. M. (2000) M-1/M-2 macrophages and the Th1/Th2 paradigm. J. Immunol. 164, 6166–617310843666 [Google Scholar]
- 4. Elgert K. D., Alleva D. G., Mullins D. W. (1998) Tumor-induced immune dysfunction: the macrophage connection. J. Leukoc. Biol. 64, 275–290 [DOI] [PubMed] [Google Scholar]
- 5. Munder M., Eichmann K., Modolell M. (1998) Alternative metabolic states in murine macrophages reflected by the nitric oxide synthase/arginase balance: competitive regulation by CD4+ T cells correlates with Th1/Th2 phenotype. J. Immunol. 160, 5347–5354 [PubMed] [Google Scholar]
- 6. Martinez F. O., Helming L., Gordon S. (2009) Alternative activation of macrophages: an immunologic functional perspective. Annu. Rev. Immunol. 27, 451–483 [DOI] [PubMed] [Google Scholar]
- 7. Gordon S. (2003) Alternative activation of macrophages. Nat. Rev. Immunol. 3, 23–35 [DOI] [PubMed] [Google Scholar]
- 8. Van Ginderachter J. A., Movahedi K., Hassanzadeh Ghassabeh G., Meerschaut S., Beschin A., Raes G., De Baetselier P. (2006) Classical and alternative activation of mononuclear phagocytes: picking the best of both worlds for tumor promotion. Immunobiology 211, 487–501 [DOI] [PubMed] [Google Scholar]
- 9. Goerdt S., Orfanos C. E. (1999) Other functions, other genes: alternative activation of antigen-presenting cells. Immunity 10, 137–142 [DOI] [PubMed] [Google Scholar]
- 10. Gough M. J., Melcher A. A., Ahmed A., Crittenden M. R., Riddle D. S., Linardakis E., Ruchatz A. N., Emiliusen L. M., Vile R. G. (2001) Macrophages orchestrate the immune response to tumor cell death. Cancer Res. 61, 7240–7247 [PubMed] [Google Scholar]
- 11. Kreider T., Anthony R. M., Urban J. F., Jr., Gause W. C. (2007) Alternatively activated macrophages in helminth infections. Curr. Opin. Immunol. 19, 448–453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Corraliza I. M., Soler G., Eichmann K., Modolell M. (1995) Arginase induction by suppressors of nitric oxide synthesis (IL-4, IL-10 and PGE2) in murine bone-marrow-derived macrophages. Biochem. Biophys. Res. Commun. 206, 667–673 [DOI] [PubMed] [Google Scholar]
- 13. Murray P. J., Wynn T. A. (2011) Obstacles and opportunities for understanding macrophage polarization. J. Leukoc. Biol. 89, 557–563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Albina J. E., Mills C. D., Henry W. L., Jr., Caldwell M. D. (1990) Temporal expression of different pathways of 1-arginine metabolism in healing wounds. J. Immunol. 144, 3877–3880 [PubMed] [Google Scholar]
- 15. Welch J. S., Escoubet-Lozach L., Sykes D. B., Liddiard K., Greaves D. R., Glass C. K. (2002) TH2 cytokines and allergic challenge induce Ym1 expression in macrophages by a STAT6-dependent mechanism. J. Biol. Chem. 277, 42821–42829 [DOI] [PubMed] [Google Scholar]
- 16. Raes G., Brys L., Dahal B. K., Brandt J., Grooten J., Brombacher F., Vanham G., Noel W., Bogaert P., Boonefaes T., Kindt A., Van den Bergh R., Leenen P. J., De Baetselier P., Ghassabeh G. H. (2005) Macrophage galactose-type C-type lectins as novel markers for alternatively activated macrophages elicited by parasitic infections and allergic airway inflammation. J. Leukoc. Biol. 77, 321–327 [DOI] [PubMed] [Google Scholar]
- 17. Sitkovsky M., Lukashev D. (2005) Regulation of immune cells by local-tissue oxygen tension: HIF1 alpha and adenosine receptors. Nat. Rev. Immunol. 5, 712–721 [DOI] [PubMed] [Google Scholar]
- 18. Linden J. (2001) Molecular approach to adenosine receptors: receptor-mediated mechanisms of tissue protection. Annual Rev. Pharmacol. Toxicol. 41, 775–787 [DOI] [PubMed] [Google Scholar]
- 19. Hart M. L., Jacobi B., Schittenhelm J., Henn M., Eltzschig H. K. (2009) Cutting edge: A2B adenosine receptor signaling provides potent protection during intestinal ischemia/reperfusion injury. J. Immunol. 182, 3965–3968 [DOI] [PubMed] [Google Scholar]
- 20. Yang D., Zhang Y., Nguyen H. G., Koupenova M., Chauhan A. K., Makitalo M., Jones M. R., St Hilaire C., Seldin D. C., Toselli P., Lamperti E., Schreiber B. M., Gavras H., Wagner D. D., Ravid K. (2006) The A2B adenosine receptor protects against inflammation and excessive vascular adhesion. J. Clin. Invest. 116, 1913–1923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Blackburn M. R., Vance C. O., Morschl E., Wilson C. N. (2009) Adenosine receptors and inflammation. Handb. Exp. Pharmacol. 215–269 [DOI] [PubMed] [Google Scholar]
- 22. Jacobson K. A., Gao Z. G. (2006) Adenosine receptors as therapeutic targets. Nat. Rev. Drug Discov. 5, 247–264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Pinhal-Enfield G., Ramanathan M., Hasko G., Vogel S. N., Salzman A. L., Boons G. J., Leibovich S. J. (2003) An angiogenic switch in macrophages involving synergy between Toll-like receptors 2, 4, 7, and 9 and adenosine A(2A) receptors. Am. J. Pathol. 163, 711–721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Csoka B., Nemeth Z. H., Virag L., Gergely P., Leibovich S. J., Pacher P., Sun C. X., Blackburn M. R., Vizi E. S., Deitch E. A., Hasko G. (2007) A2A adenosine receptors and C/EBPbeta are crucially required for IL-10 production by macrophages exposed to Escherichia coli. Blood 110, 2685–2695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hasko G., Kuhel D. G., Chen J. F., Schwarzschild M. A., Deitch E. A., Mabley J. G., Marton A., Szabo C. (2000) Adenosine inhibits IL-12 and TNF-α production via adenosine A2a receptor-dependent and independent mechanisms. FASEB J. 14, 2065–2074 [DOI] [PubMed] [Google Scholar]
- 26. Kreckler L. M., Wan T. C., Ge Z. D., Auchampach J. A. (2006) Adenosine inhibits tumor necrosis factor-alpha release from mouse peritoneal macrophages via A2A and A2B but not the A3 adenosine receptor. J. Pharmacol. Exp. Ther. 317, 172–180 [DOI] [PubMed] [Google Scholar]
- 27. Nemeth Z. H., Lutz C. S., Csoka B., Deitch E. A., Leibovich S. J., Gause W. C., Tone M., Pacher P., Vizi E. S., Hasko G. (2005) Adenosine augments IL-10 production by macrophages through an A2B receptor-mediated posttranscriptional mechanism. J. Immunol. 175, 8260–8270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Csoka B., Nemeth Z. H., Rosenberger P., Eltzschig H. K., Spolarics Z., Pacher P., Selmeczy Z., Koscso B., Himer L., Vizi E. S., Blackburn M. R., Deitch E. A., Hasko G. (2010) A2B adenosine receptors protect against sepsis-induced mortality by dampening excessive inflammation. J. Immunol. 185, 542–550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Albina J. E., Mahoney E. J., Daley J. M., Wesche D. E., Morris S. M., Jr., Reichner J. S. (2005) Macrophage arginase regulation by CCAAT/enhancer-binding protein beta. Shock 23, 168–172 [DOI] [PubMed] [Google Scholar]
- 30. Gorgoni B., Maritano D., Marthyn P., Righi M., Poli V. (2002) C/EBP beta gene inactivation causes both impaired and enhanced gene expression and inverse regulation of IL-12 p40 and p35 mRNAs in macrophages. J. Immunol. 168, 4055–4062 [DOI] [PubMed] [Google Scholar]
- 31. Pauleau A. L., Rutschman R., Lang R., Pernis A., Watowich S. S., Murray P. J. (2004) Enhancer-mediated control of macrophage-specific arginase I expression. J. Immunol. 172, 7565–7573 [DOI] [PubMed] [Google Scholar]
- 32. Feoktistov I., Biaggioni I. (1993) Characterization of adenosine receptors in human erythroleukemia cells and platelets: further evidence for heterogeneity of adenosine A2 receptor subtypes. Mol. Pharmacol. 43, 909–914 [PubMed] [Google Scholar]
- 33. Feoktistov I., Biaggioni I. (1998) Pharmacological characterization of adenosine A2B receptors: studies in human mast cells co-expressing A2A and A2B adenosine receptor subtypes. Biochem. Pharmacol. 55, 627–633 [DOI] [PubMed] [Google Scholar]
- 34. Hasko G., Pacher P., Deitch E. A., Vizi E. S. (2007) Shaping of monocyte and macrophage function by adenosine receptors. Pharmacol. Ther. 113, 264–275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ruffell D., Mourkioti F., Gambardella A., Kirstetter P., Lopez R. G., Rosenthal N., Nerlov C. (2009) A CREB-C/EBPbeta cascade induces M2 macrophage-specific gene expression and promotes muscle injury repair. Proc. Natl. Acad. Sci. U. S. A. 106, 17475–17480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Gray M. J., Poljakovic M., Kepka-Lenhart D., Morris S. M., Jr. (2005) Induction of arginase I transcription by IL-4 requires a composite DNA response element for STAT6 and C/EBPbeta. Gene 353, 98–106 [DOI] [PubMed] [Google Scholar]
- 37. Nemeth Z. H., Leibovich S. J., Deitch E. A., Sperlagh B., Virag L., Vizi E. S., Szabo C., Hasko G. (2003) Adenosine stimulates CREB activation in macrophages via a p38 MAPK-mediated mechanism. Biochem. Biophys. Res. Commun. 312, 883–888 [DOI] [PubMed] [Google Scholar]
- 38. Csoka B., Nemeth Z. H., Selmeczy Z., Koscso B., Pacher P., Vizi E. S., Deitch E. A., Hasko G. (2007) Role of A(2A) adenosine receptors in regulation of opsonized E. coli-induced macrophage function. Purinergic Signal 3, 447–452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hasko G., Csoka B., Nemeth Z. H., Vizi E. S., Pacher P. (2009) A(2B) adenosine receptors in immunity and inflammation. Trends Immunol. 30, 263–270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Chen H., Yang D., Carroll S. H., Eltzschig H. K., Ravid K. (2009) Activation of the macrophage A2b adenosine receptor regulates tumor necrosis factor-alpha levels following vascular injury. Exp. Hematol. 37, 533–538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Belikoff B. G., Hatfield S., Georgiev P., Ohta A., Lukashev D., Buras J. A., Remick D. G., Sitkovsky M. (2011) A2B adenosine receptor blockade enhances macrophage-mediated bacterial phagocytosis and improves polymicrobial sepsis survival in mice. J. Immunol. 186, 2444–2453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Wilson J. M., Ross W. G., Agbai O. N., Frazier R., Figler R. A., Rieger J., Linden J., Ernst P. B. (2009) The A2B adenosine receptor impairs the maturation and immunogenicity of dendritic cells. J. Immunol. 182, 4616–4623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hasko G., Szabo C., Nemeth Z. H., Kvetan V., Pastores S. M., Vizi E. S. (1996) Adenosine receptor agonists differentially regulate IL-10, TNF-alpha, and nitric oxide production in RAW 264.7 macrophages and in endotoxemic mice. J. Immunol. 157, 4634–4640 [PubMed] [Google Scholar]
- 44. Ryzhov S., Zaynagetdinov R., Goldstein A. E., Novitskiy S. V., Blackburn M. R., Biaggioni I., Feoktistov I. (2008) Effect of A2B adenosine receptor gene ablation on adenosine-dependent regulation of proinflammatory cytokines. J. Pharmacol. Exp. Ther. 324, 694–700 [DOI] [PubMed] [Google Scholar]
- 45. Xaus J., Mirabet M., Lloberas J., Soler C., Lluis C., Franco R., Celada A. (1999) IFN-gamma up-regulates the A2B adenosine receptor expression in macrophages: a mechanism of macrophage deactivation. J. Immunol. 162, 3607–3614 [PubMed] [Google Scholar]
- 46. Feoktistov I., Biaggioni I. (1997) Adenosine A2B receptors. Pharmacol. Rev. 49, 381–402 [PubMed] [Google Scholar]
- 47. El Kasmi K. C., Qualls J. E., Pesce J. T., Smith A. M., Thompson R. W., Henao-Tamayo M., Basaraba R. J., Konig T., Schleicher U., Koo M. S., Kaplan G., Fitzgerald K. A., Tuomanen E. I., Orme I. M., Kanneganti T. D., Bogdan C., Wynn T. A., Murray P. J. (2008) Toll-like receptor-induced arginase 1 in macrophages thwarts effective immunity against intracellular pathogens. Nat. Immunol. 9, 1399–1406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Qualls J. E., Neale G., Smith A. M., Koo M. S., DeFreitas A. A., Zhang H., Kaplan G., Watowich S. S., Murray P. J. (2010) Arginine usage in mycobacteria-infected macrophages depends on autocrine-paracrine cytokine signaling. Sci. Signal. 3, ra62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Hasko G., Linden J., Cronstein B., Pacher P. (2008) Adenosine receptors: therapeutic aspects for inflammatory and immune diseases. Nat. Rev. Drug Discov. 7, 759–770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Erdely A., Kepka-Lenhart D., Clark M., Zeidler-Erdely P., Poljakovic M., Calhoun W. J., Morris S. M., Jr. (2006) Inhibition of phosphodiesterase 4 amplifies cytokine-dependent induction of arginase in macrophages. Am. J. Physiol. Lung Cell. Mol. Physiol. 290, L534–L539 [DOI] [PubMed] [Google Scholar]
- 51. Deszo E. L., Brake D. K., Kelley K. W., Freund G. G. (2004) IL-4-dependent CD86 expression requires JAK/STAT6 activation and is negatively regulated by PKCdelta. Cell. Signal. 16, 271–280 [DOI] [PubMed] [Google Scholar]
- 52. Kim C. H., Kim K. E., Yoon J. H., Song K. S. (2009) Upregulation of MUC5AC gene expression by IL-4 through CREB in human airway epithelial cells. J. Cell Biochem. 108, 974–981 [DOI] [PubMed] [Google Scholar]
- 53. Ratthe C., Pelletier M., Chiasson S., Girard D. (2007) Molecular mechanisms involved in interleukin-4-induced human neutrophils: expression and regulation of suppressor of cytokine signaling. J. Leukoc. Biol. 81, 1287–1296 [DOI] [PubMed] [Google Scholar]
- 54. Hunt A. E., Williams L. M., Lali F. V., Foxwell B. M. (2002) IL-4 regulation of p38 MAPK signalling is dependent on cell type. Cytokine 18, 295–303 [DOI] [PubMed] [Google Scholar]
- 55. Feoktistov I., Goldstein A. E., Biaggioni I. (1999) Role of p38 mitogen-activated protein kinase and extracellular signal-regulated protein kinase kinase in adenosine A2B receptor-mediated interleukin-8 production in human mast cells. Mol. Pharmacol. 55, 726–734 [PubMed] [Google Scholar]
- 56. Noel W., Raes G., Hassanzadeh Ghassabeh G., De Baetselier P., Beschin A. (2004) Alternatively activated macrophages during parasite infections. Trends Parasitol. 20, 126–133 [DOI] [PubMed] [Google Scholar]
- 57. Mantovani A., Sica A., Sozzani S., Allavena P., Vecchi A., Locati M. (2004) The chemokine system in diverse forms of macrophage activation and polarization. Trends Immunol. 25, 677–686 [DOI] [PubMed] [Google Scholar]