Abstract
Purpose
We evaluated the effectiveness of microsurgical ligation for painful varicocele and predictive factors of pain resolution.
Materials and Methods
Between January 2006 and March 2009, a total of 114 patients (mean age, 30.2±8.9 years), who underwent microsurgical inguinal varicocelectomy for painful varicocele, were included and followed up for 1 year after the surgery. The quantity of preoperative and postoperative pain was assessed by means of 11-point numeric rating scale (NRS). We retrospectively analyzed the outcome of surgical ligation and predictive factors of pain resolution using patient age, height, weight, body mass index, grade and location of varicocele, duration, quantity and quality (dull, dragging, aching) of pain, and postoperative pain resolution.
Results
In 104 patients (91.2%), complete or marked resolution of pain was reported at follow-up 1 year after surgery. Only 10 patients (8.8%) had recurrent or persistent pain (≥3 points in NRS scores). On multivariate analysis, low quantity (≤6 points in NRS scores) and dull or dragging natured preoperative pain were independent factors associated with surgical success rates (p=0.004; odds ratio=1.62, p=0.012; odds ratio=1.76, respectively).
Conclusion
Microsurgical ligation is an effective treatment of painful varicocele. The quantity and quality of preoperative pain are independent predictive factors of pain resolution after surgery.
Keywords: Varicocele, ligation, pain
INTRODUCTION
Varicocele is the most commonly diagnosed peripubertal andrologic disease and the most commonly treatable cause of male-related impaired fertility potential.1 Also, varicocele is associated with chronic scrotal pain, but this relationship has been less widely investigated.2 It is evaluated that the prevalence of painful varicoceles is 2-10%. This pain was described as a dull, throbbing pain, worsening with exertion and strain.3
Varicocele ligation has been assessed as an effective treatment of painful varicocele.4 Other comparative reports have assessed different techniques, but at present there is no consensus as to which surgical method is best suited for varicocele treatment, although microsurgical techniques of varicocelectomy have gained popularity with minimal complication rates and good outcomes.4-7 Also, little data exists regarding the outcome of surgical treatment of painful varicoceles and factors able to predict success. This retrospective study, in a selected homogeneous population evaluated the effectiveness of microsurgical ligation against painful varicocele, including the predictive factors affecting pain resolution.
MATERIALS AND METHODS
Patients
Between January 2006 and March 2009, a total of 114 patients (mean age, 30.2±8.9 years) who underwent microsurgical inguinal varicocelectomy for pain were included and followed up for at least 1 year (mean; 15.8 months: range, 13-49) after surgery. Written consent from each patient was obtained. Diagnosis of varicocele was made using self-diagnosed symptoms, such as scrotal discomfort or pain, and on clinical grounds of both physical examination and Doppler ultrasound scan (USS). Patients whose cause of scrotal pain was ambiguous and who had a previous history of scrotal trauma or surgery were excluded from this study. Men with lower urinary tract symptoms were also excluded, as were men with a documented psychological disturbance.
Preoperative evaluations
Medical records were retrospectively investigated to document patient demographics [age, height, weight, body mass index (BMI), etc.], grade (I, II, III) and, location of varicocele (right, left or bilateral), duration (months) and quality (dull, dragging, aching) of pain before surgery. To evaluate the quantity of pain, we used a 11-point numeric rating scale (NRS) where 0 indicated no pain and 10 indicated the worst pain imaginable (0, 1-3, 4-6, 7-10: none, mild, moderate, severe; respectively).
Procedure
The microsurgical inguinal varicocelectomy was performed under general or spinal anesthesia by a single experienced surgeon using a similar technique previously described,8 except for we did not deliver the testicle or examine the gubernaculum. An operative microscope (10-25X) was used during spermatic cord dissection to identify and preserve the testicular artery and lymphatics.
Follow-up evaluation
All patients were asked to visit the clinic at 1 month, 3 months and 1 year after surgery, at which time they were evaluated with a careful symptom review, scrotal examination at supine and standing positions, and 11-point NRS to assess the quantity of postoperative pain. Also, Doppler USS was performed when deemed clinically necessary for discovery of varicocele recurrence.
Definition
Varicocele was classified into the following grades: grade I, varicocele palpable during a Valsalva maneuver when upright; grade II, varicocele palpable when upright without Valsalva maneuver; and grade III, varicocele palpable and visually detectable.9 Surgical success was defined as the lack of palpable scrotal veins on physical examination and reporting of scores in the lowest range on the 11-point NRS scale (≤2 points) after surgery.
Analysis
Our primary objective was to analyze overall surgical success rates after microsurgical inguinal varicocelectomy. Our secondary objective was to determine which preoperative factors influenced the pain resolution after surgery by evaluation clinical factors. Normally distributed variables were compared using ANOVA and Student's t-tests. The Fisher's exact and chi-square tests were used for dichotomous variables. To determine the predictive factors affecting the resolution of pain, univariate analysis was performed using a logistic regression analysis. A 5% level of significance was used for all statistical testing and all statistical tests were two-sided. Analyse was performed using the statistical software SPSS (14.0KO for Windows, Release 14.0.2).
RESULTS
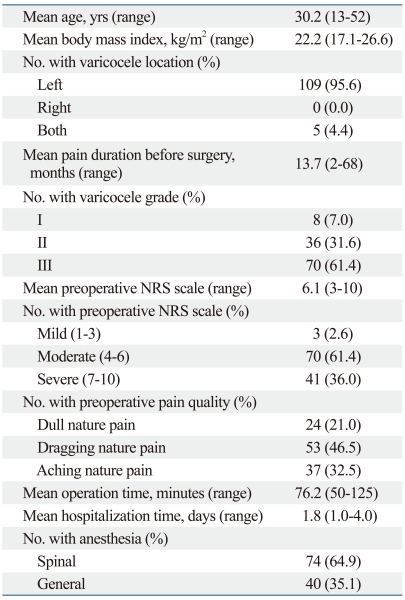
One hundred and fourteen patients with painful varicocele underwent microsurgical inguinal varicocelectomy with complete follow-up, and all patients who underwent surgery failed an initial conservative treatment (scrotal support, non-steroidal anti-inflammatory treatment and exercise limitation) for 4-24 weeks. Baseline characteristics of the 114 men are illustrated in Table 1.
Table 1.
Characteristics of 114 Patients
NRS, numeric rating scale.
Of the 114 patients, 104 (91.2%) reported complete or marked resolution of pain at follow-up 1 year after surgery. Only 10 (8.8%) had recurrent or persistent pain (≥3 points in 11-point NRS scores).
Four patients (3.5%) had recurrence of pain (mean points in 11-point NRS scores, 4.0±0.8 points) after an initial period of resolution (mean period, 1.8±0.5 months). All 4 patients with recurrent pain were subjected to Doppler USS and no patient had varicocele recurrence.
Six patients (5.3%) reported persistent pain (mean points in 11-point NRS scores, 4.7±1.4 points) at follow-up 1 year after surgery. Of those, one complained that his symptoms were worse. All 6 patients with persistent pain were also subjected to Doppler USS, and only one (0.8%) had varicocele recurrence. However, although successful radiographic embolization was performed in this patient, his pain persisted.
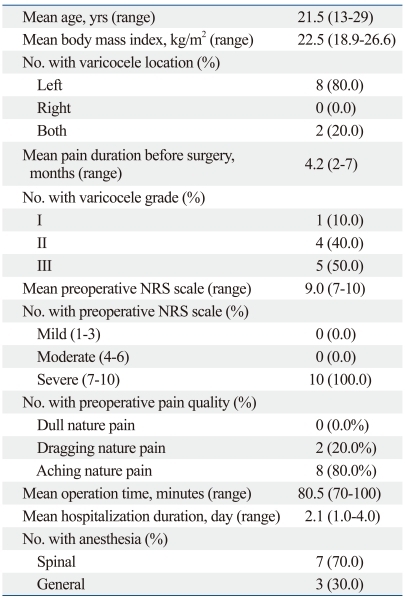
Table 2 shows the preoperative characteristics in the failure group of pain resolution. From the viewpoint of pain quality, all patients with recurrent or persistent pain had dragging or aching preoperative pain at follow-up 1 year after surgery.
Table 2.
Preoperative Characteristics in the Failure Group of Pain Resolution (n=10)
NRS, numeric rating scale.
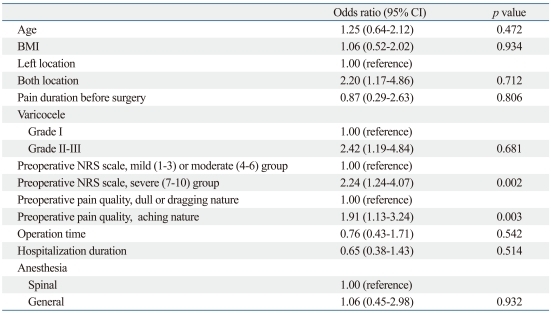
Univariate analysis of the preoperative factors demonstrated that the quality and quantity of preoperative pain were associated with surgical success rates (Table 3). When we divided the patients into three groups according to preoperative pain qualities, we found that the success rates were 78.4% in men with aching pain, 96.2% with dragging pain and 100% with dull pain (p=0.003, OR 1.91). There was also a significant difference in success rates among patients' groups according to preoperative NRS scores (1-3, 4-6, 7-10: mild, moderate, severe group) (p=0.002, OR 2.24).
Table 3.
Univariate Analysis of Preoperative and Intraoperative Parameters of Determinants for Surgical Success Rates at 1 Year Follow Up State
95%CI, 95% confidence interval; BMI, body mass index; NRS, numeric rating scale.
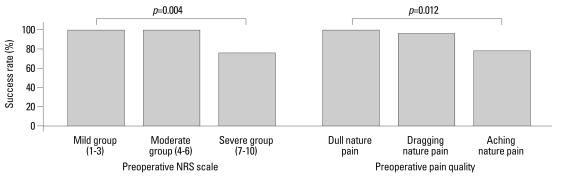
Multivariate analysis indicated that quality and quantity of preoperative pain were independent factors related to success rates (p=0.012, OR 1.76 and p=0.004, OR 1.62, respectively) (Fig. 1). However, when the relationships between pain resolution and patient age, height, weight, BMI, duration of pain before surgery, grade and location of varicocele were examined, none of these factors significantly predicted the resolution of pain (p>0.05).
Fig. 1.
Success rates by preoperative NRS scale and pain quality. The multivariate analysis of preoperative factors demonstrated that NRS scale and pain quality might predict the success rates of microsurgical ligation in painful varicocele patients. NRS, numeric rating scale.
There were no intraoperative or early postoperative complications, such as orchitis, infection, or scrotal hematoma. At 1 year follow-up, as aforementioned, 10 patients had recurrent or persistent scrotal pain and 1 had varicocele recurrence; but no patients had hydrocele formation, evidence of testicular loss or progressive hypotrophy.
DISCUSSION
The most common grievance in men with varicocele is a dull and throbbing scrotal pain that aggravated during straining and exercise.1 Urologists often meet patients with painful varicocele, whose jobs need working mostly in standing positions or vigorous physical effort. However, most urologists cannot form an objective opinion based on their own experience.
Conventional treatment of painful varicocele is conservative treatment followed by surgery. Generally used conservative methods are scrotal elevation, nonsteroidal anti-inflammatory medication and decreased physical activity, that often lead to unacceptable lifestyle restrictions.10 Also, percutaneous embolization or various surgical options, such as high inguinal, inguinal, subinguinal, laparoscopic, and microsurgical ligation, might be implemented to relieve pain of varicoceles.2
Surgical treatment of painful varicocele is controversial, because a few literature supports its use and surgical ligation is only recommended in men who have specific pain complaints and in whom conservative treatments has failed.4-6 The studies by Peterson, et al.11 and by Yaman, et al.3 reported complete resolution of pain in 86% and 88% of patients, respectively. Yaman, et al.3 suggested that the failure rate was associated with preoperative varicocele grade. Also, Karademir, et al.1 reported similar results using inguinal and subinguinal ligation and suggested that surgical approaches may influence outcomes with best outcomes achieved with inguinal or sub-inguinal ligation. However, Al-Buheissi, et al.12 showed that although surgical ligation is an effective treatment of painful varicocele, there was no correlation between the surgical approach used and failure of pain resolution. They also reported that the quality of pain was a detrimental factor when selecting patients for varicocele ligation.
In our study, of the 114 patients, 104 (91.2%) reported complete or marked resolution of pain at follow-up 1 year after surgery. We also found that the quality and quantity of preoperative pain were independent factors related to success rates (p=0.012, OR 1.76 and p=0.004, OR 1.62, respectively) in the present multivariate analysis. Accordingly, the degree of postoperative pain resolution was related with low quantity [≤6 points in visual analogue scale (VAS) scores] and dragging or dull natured preoperative pain. However, when the relationships between pain resolution and patient age, BMI, duration of pain before surgery, grade and location of varicocele were investigated, none of these factors significantly predicted the resolution of pain (p>0.05).
With regard to varicocele recurrence as postoperative complications, microsurgical varicocelectomy is better than non-microsurgical methods.13,14 It has been reported that varicocele recurrence generally results from incomplete ligation of collateral veins,2 and that magnification of the spermatic vessels by operating microscope reduces the possibility of such complications.15 Levine, et al.16 also reported that complete dissection of the spermatic cord using operative microscope might be effective for chronic scrotal pain because that procedure might result in partial denervation of the testis.
In this study, we used microsurgical inguinal varicocelectomy with complete dissection of the spermatic cord, such that it only included the spermatic artery, lymphatics, and the vas deferens and its accompanying artery. As a result, 10 patients (8.8%) had recurrent or persistent scrotal pain and only one (0.8%) had varicocele recurrence at 1 year of follow-up; however, no patients had hydrocele formation, evidence of testicular loss or progressive hypotrophy.
In our study, the 11-point NRS was used to evaluate the quantity of pain. Although the VAS and the NRS have been reported that they provide almost identical results in the same patient at several times after surgery, the NRS, with numbers from 0 to 10 ('no pain' to 'worst pain imaginable'), is more practical and easier to understand than the VAS.17 Therefore, in our study, response criteria is based on subjective patients against other most studies.
In conclusion, microsurgical ligation has a high success rate (91.2%) with low recurrence rate (0.8%) for the treatment of painful varicocele. Also, we show that the quantity and quality of preoperative pain are independent predictive factors of pain resolution after surgery. A prospective randomized study with long term follow-up comparing surgical treatments of painful varicocele using different surgical approaches is needed to support the present data.
ACKNOWLEDGEMENTS
This research was supported by the Yeungnam University research grants in 2009.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Karademir K, Senkul T, Baykal K, Ateş F, Işeri C, Erden D. Evaluation of the role of varicocelectomy including external spermatic vein ligation in patients with scrotal pain. Int J Urol. 2005;12:484–488. doi: 10.1111/j.1442-2042.2005.01063.x. [DOI] [PubMed] [Google Scholar]
- 2.Chawla A, Kulkarni G, Kamal K, Zini A. Microsurgical varicocelectomy for recurrent or persistent varicoceles associated with orchalgia. Urology. 2005;66:1072–1074. doi: 10.1016/j.urology.2005.05.052. [DOI] [PubMed] [Google Scholar]
- 3.Yaman O, Ozdiler E, Anafarta K, Göğüş O. Effect of microsurgical subinguinal varicocele ligation to treat pain. Urology. 2000;55:107–108. doi: 10.1016/s0090-4295(99)00374-x. [DOI] [PubMed] [Google Scholar]
- 4.Gontero P, Pretti G, Fontana F, Zitella A, Marchioro G, Frea B. Inguinal versus subinguinal varicocele vein ligation using magnifying loupe under local anesthesia: which technique is preferable in clinical practice? Urology. 2005;66:1075–1079. doi: 10.1016/j.urology.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 5.Riccabona M, Oswald J, Koen M, Lusuardi L, Radmayr C, Bartsch G. Optimizing the operative treatment of boys with varicocele: sequential comparison of 4 techniques. J Urol. 2003;169:666–668. doi: 10.1097/01.ju.0000047086.34953.82. [DOI] [PubMed] [Google Scholar]
- 6.Amelar RD. Early and late complications of inguinal varicocelectomy. J Urol. 2003;170:366–369. doi: 10.1097/01.ju.0000074975.79734.17. [DOI] [PubMed] [Google Scholar]
- 7.Shin JH, Lim JS. Surgical repair of varicocele: a comparative study of the retroperitoneal approach of palomo, the modified palomo technique and the microsurgical inguinal approach of ivanisseivich's technique. Korean J Urol. 2006;47:1086–1092. [Google Scholar]
- 8.Lipshultz LI, Thomas AJ, Jr, Khera M. Surgical management of male infertility. In: Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh Urology. 9th ed. Philadelphia: WB Saunders; 2007. pp. 654–717. [Google Scholar]
- 9.Ishikawa T, Fujisawa M. Effect of age and grade on surgery for patients with varicocele. Urology. 2005;65:768–772. doi: 10.1016/j.urology.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 10.Ribé N, Manasia P, Sàrquella J, Grimaldi S, Pomerol JM. Clinical follow-up after subinguinal varicocele ligation to treat pain. Arch Ital Urol Androl. 2002;74:51–53. [PubMed] [Google Scholar]
- 11.Peterson AC, Lance RS, Ruiz HE. Outcomes of varicocele ligation done for pain. J Urol. 1998;159:1565–1567. doi: 10.1097/00005392-199805000-00043. [DOI] [PubMed] [Google Scholar]
- 12.Al-Buheissi SZ, Patel HR, Wazait HD, Miller RA, Nathan S. Predictors of success in surgical ligation of painful varicocele. Urol Int. 2007;79:33–36. doi: 10.1159/000102910. [DOI] [PubMed] [Google Scholar]
- 13.Cayan S, Kadioglu TC, Tefekli A, Kadioglu A, Tellaloglu S. Comparison of results and complications of high ligation surgery and microsurgical high inguinal varicocelectomy in the treatment of varicocele. Urology. 2000;55:750–754. doi: 10.1016/s0090-4295(99)00603-2. [DOI] [PubMed] [Google Scholar]
- 14.Lee JW, Paick JS, Kim SW. Microsurgical subinguinal varicocelectomy: comparison of pediatric and adult patients. Korean J Urol. 2008;49:1029–1034. [Google Scholar]
- 15.Yaman O, Soygur T, Zumrutbas AE, Resorlu B. Results of microsurgical subinguinal varicocelectomy in children and adolescents. Urology. 2006;68:410–412. doi: 10.1016/j.urology.2006.02.022. [DOI] [PubMed] [Google Scholar]
- 16.Levine LA, Matkov TG, Lubenow TR. Microsurgical denervation of the spermatic cord: a surgical alternative in the treatment of chronic orchialgia. J Urol. 1996;155:1005–1007. doi: 10.1016/s0022-5347(01)66369-9. [DOI] [PubMed] [Google Scholar]
- 17.Breivik H, Borchgrevink PC, Allen SM, Rosseland LA, Romundstad L, Hals EK, et al. Assessment of pain. Br J Anaesth. 2008;101:17–24. doi: 10.1093/bja/aen103. [DOI] [PubMed] [Google Scholar]