Abstract
Purpose
The present study aims to evaluate the prevalence of unmet needs among breast cancer survivors, to assess the relationships between unmet needs and depression and quality of life, and to explore the extent to which unmet needs of breast cancer patients relate to the time elapsed since surgery.
Materials and Methods
Among 1,250 eligible patients who participated in the study, 1,084 cases (86.7%) were used for analysis. Clinicopathological and social parameters were reviewed and the Supportive Care Needs Survey, Functional Assessment of Cancer Therapy-Breast cancer instrument, and Beck Depression Inventory were administered. The frequency of unmet needs, the association between unmet needs and depression and/or quality of life (QOL) and the impact of the time elapsed since surgery on the patients' unmet needs were analyzed.
Results
The highest levels of unmet needs were found to be in the health system and information domain. Patients with a survival duration of less than 1 year since surgery showed significantly higher unmet needs in all need domains except the sexuality domain (p<0.001) than participants in the other groups. Patients with a survival duration of 1-3 years also experienced significantly higher psychological and information needs than long-term survivors (>5 years). In addition, unmet needs were significantly associated with depression (p<0.001) and QOL (p<0.001).
Conclusion
The present study demonstrated that long-term breast cancer survivors had a significantly lower level of unmet needs than patients with survival duration of less than 3 years after surgery and patients with survival duration of less than 1 year since surgery suffered the greatest unmet needs. QOL might be enhanced if interventions are made for specific unmet needs of each patient group.
Keywords: Breast carcinoma, unmet needs, quality of life, depression
INTRODUCTION
The 5-year relative survival rate of breast cancer patients was as high as 89.5% between 2003 and 2007 in Korea1 and cancer survivorship issues have become a new concern for delivering quality cancer care.2
Because of early detection and advances in treatment, disease-free survival rate is increasing and quality of life (QOL) among breast cancer patients is a growing area of research and clinical considerations. Even though there is debate about the degree to which cancer patients experience psychopathology, some research has shown that severe psychopathology among cancer patients is no more prevalent than in the general population.3 According to the literature, the majority of cancer patients experience more psychological, interpersonal, health policy and system difficulties and other problems of living rather than psychiatric symptoms.3,4 Therefore, it is important to assess the magnitude and prevalence of these difficulities and problems among cancer patients systematically.
Psychological adaptation to breast cancer could be measured in many ways including quality of life, satisfaction with care and needs assessment. Needs assessment differs from other assessment constructs in that it directly identifies patients with higher levels of need and suggests specific interventions for them.5,6 It provides direct index of what patients perceive they need help with and also measures the perceived efficacy of a health services by its users.6 Therefore, evaluating patients' needs is important to offer timely, effective interventions.7 On the other hand, previous studies showed that time elapsed since diagnosis is a significant predictor of QOL and unmet needs.8,9 Many studies suggested that QOL of long-term, disease-free breast cancer survivors improve over time.10,11 They showed long-term, disease-free breast cancer survivors reported high levels of functioning on several dimensions of QOL and most of the limitations imposed by therapy and poor health improved with time.10,12 Other research reported that long-term survivors of breast cancer continue to experience psychological morbidities including increased depression and lower QOL.13,14 However, there is little research available regarding the needs of breast cancer survivors over time. Understanding the changing psychosocial needs of cancer patients across time is needed in order to provide interventions that reflect personal needs in their illness trajectory.
Thus, the present study aims to evaluate the prevalence of unmet needs among breast cancer survivors, to assess the relationships between unmet needs and depression and quality of life, and to explore the extent to which unmet needs relate to the time elapsed since surgery.
MATERIALS AND METHODS
Patients
The subjects in this cross-sectional study were outpatients with breast cancer at Yonsei University Severance Hospital Breast Cancer Clinic. They were all Koreans and attended regular follow-up medical appointments after surgery. The eligibility criteria for inclusion in the study were as follows: 1) between 20 and 80 years old, 2) stage I, II, and III cancers, 3) no evidence of systemic metastasis, 4) no evidence of psychosis, dementia, or suicidal behavior, and 5) no recurrence. After informed consent had been obtained, the patients were asked to complete the questionnaires. Among 1,250 eligible patients who consented to participate in the study, 1,084 (86.7%) returned completed surveys. No significant differences in demographic characteristics between those who returned the surveys and those who did not were observed. To explore the extent to which the unmet needs of breast cancer survivors relates to the time elapsed since surgery, we divided patients into four groups relative to the time since surgery: group I, less than 1 year; group II, 1-3 years; group III, 3-5 years; and group IV, more than 5 years. This division was based on the treatment and follow-up-care schedules after surgery. Most of the breast cancer patients received adjuvant therapy including chemotherapy. Adjuvant chemotherapy causes additional physical and psychological distress to the breast cancer patients. Adjuvant chemotherapy usually takes place 3-6 months after surgery and carryover effects can continue for a while. Recurrences mostly occur at 2 to 3 years after surgery, and most adjuvant endocrine therapies are recommended for 5 years. Five-year disease-free survival can predict long-term survival or cure, though not in all cases. This study was approved by the Institutional Review Board of Yonsei University Severance Hospital (4-2009-0269).
Measurements
Socio-demographic and medical background
Socio-demographic background including a patient's age, marital status, job, education, and economic status were included in the survey. Subjective economic status was assessed by asking respondents to circle what they considered an accurate reflection of their economic status from the lowest, lower, middle, upper-middle, to upper status. Medical/treatment variables were collected by reviewing the patients' medical records.
The supportive care needs survey
The supportive care needs survey (SCNS), a modified version of the Cancer Needs Questionnaire6 was used to assess the unmet supportive care needs of breast cancer patients. It was designed to provide a direct and comprehensive assessment of the multidimensional impact of cancer on the lives of cancer patients.15 It consists of 59 items covering five domains of needs and additional items: psychological (22 items), health system and information (15 items), physical and daily living (7 items), patient care and support (8 items), sexuality (3 items) and an additional 4 items. The study participants were asked to indicate their level of the need for help over the last month in relation to having cancer, ranging from 1, 'no need (not applicable)'; 2, 'no need (satisfied)'; 3, 'low need'; 4, 'moderate need'; to 5 'high need'. Domain scores were calculated by summing the responses to each of the items of need within each domain and dividing the total by the number of items in the domain. A higher score indicated a higher perceived need. The survey's psychometric properties and the reliability as well as the validity of this measurement have been well documented.5,9 We used the SCNS-LF59 survey in Korean, which had been translated and back-translated by Hwang and Park.9 The reliability coefficient was 0.968 in the psychological needs domain, 0.902 in the physical and daily activity domain, 0.906 in the sexuality domain, 0.946 in the health system and information domain, 0.930 in the patient care and support domain, and 0.795 in the additional items domain.
The Beck Depression Inventory
The Beck Depression Inventory (BDI) is a 21-item inventory that describes symptoms and attitudes. Each item describes a particular aspect of depression and has four self-evaluative statements. Subjects are instructed to circle the items that best describe how they have been feeling in the last week. The Korean version of the BDI was standardized,16 and its validity and reliability have been established.17 The reliability coefficient for BDI was 0.895 in this study.
Functional Assessment of Cancer Therapy-Breast
The Functional Assessment of Cancer Therapy-Breast (FACT-B) version 4 was used to assess health-related QOL. The FACT-B is composed of the FACT-General plus the Breast Cancer subscale, which complements the general scale with items specific to QOL in patients with breast carcinoma. The psychometric properties of the FACT-B are well documented,18 and the survey was validated in Korean.19 The α coefficients for the FACT-B total score was 0.855 in this study.
The Eastern Cooperative Oncology Group Performance Status
The performance status of the patients was assessed using the Eastern Cooperative Oncology Group Performance Status (ECOG-PS) scale. ECOG-PS assesses the level of functioning based on activity, ambulatory status, and need for care. The performance status grade 0 means normal activity; grade 1 means some symptoms but nearly fully ambulatory; grade 2 means less than 50% of daytime in bed; grade 3 means more than 50% of daytime in bed; and grade 4 means completely bedridden. ECOG-PS is widely used and well validated.20
Statistical analysis
For comparisons of socio-demographic and clinical characteristics in the four groups (less than 1 year, within 1-3 years, within 3-5 years, and more than 5 years since surgery), chi-square tests were employed for the statistical significance of categorical variables and a one-way analysis of variance was used to compare means of continuous variables. Multivariate regression analysis was used to examine the relationship between the patients' perceived needs and depression and/or QOL.
Analysis of covariance was performed for comparing the four groups regarding SCNS subscales. We adjusted for the following covariates: age, education, economic status, menopause, operation method, radiation therapy, hormone therapy, chemotherapy, and performance status. The p-values for pairwise group comparisons are based on F-tests for the simple contrasts (adjusting for all of the above-mentioned covariates).
Data analyses were conducted using the SPSS software version 17.0 (SPSS Inc., Chicago, IL, USA). p-values less than 0.05 were considered statistically significant.
RESULTS
Patient characteristics
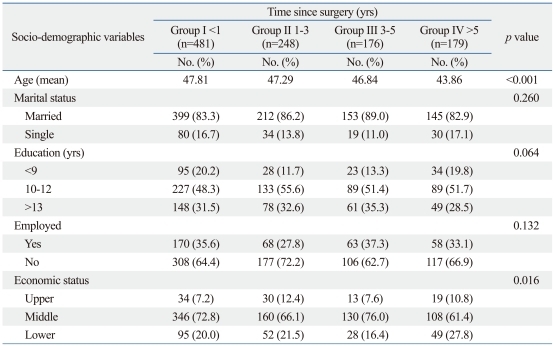
Socio-demographic and medical data are presented in Table 1 and Table 2. Patients in group IV were significantly younger than those in the other groups (p<0.001) and patients in group III were slightly higher in economic status than other groups (p<0.016). No significant differences among the four groups were observed for any of the other demographic variables.
Table 1.
Socio-Demographic Characteristics of the Sample
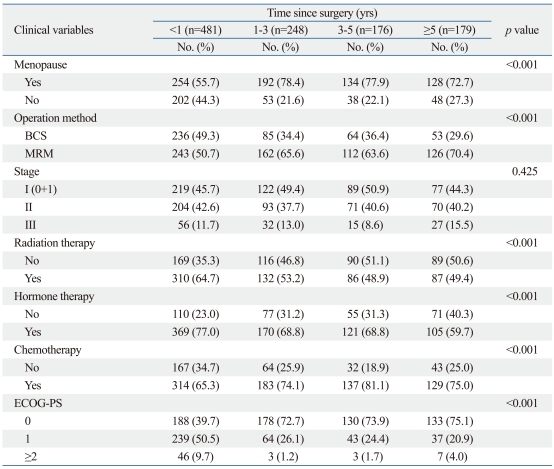
Table 2.
Medical Characteristics of the Sample
BCS, breast conservation surgery; MRM, modified radical mastectomy; ECOG-PS, Eastern Cooperative Oncology Group-Performance Status.
Medical characteristics are shown in Table 2. There were significant differences among the four groups concerning medical characteristics including menopause (p<0.001), operation method (p<0.001), radiation therapy (p<0.001), hormone therapy (p<0.001), chemotherapy (p<0.001), and level of daily activity (p<0.001).
Prevalence of unmet needs
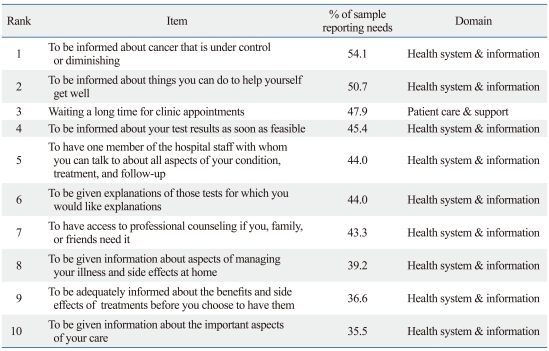
In order to identify specific issues or areas where patients required the most help, the 59 individual items of need were examined to assess the frequency of reports in each of the response categories. The 10 items with the highest frequency of moderate-to-high (3 or more on the 5-point Likert scale) are shown in Table 3. Of the 10 highest needs items, nine items were related to the health system and information domain and one item was related to the patient care and support domain. Specifically, 'To be informed about cancer that is under control or diminishing' was the commonest, followed by 'To be informed about things you can do to help yourself get well', 'Waiting a long time for a clinic appointment' 'To be informed about your test results as soon as feasible', and 'To have one member of the hospital staff with whom you can talk to about all aspects of your condition, treatment, and follow-up'. The prevalence of the ten most frequent unmet needs was over 35.3%.
Table 3.
Items of the Ten Highest Moderate-to- High Unmet Needs Responses
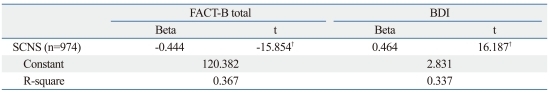
Relationship between patients' perceived needs and depression and/or QOL
Multivariate analysis revealed that unmet needs were significantly related with both QOL and depression as measured by BDI and FACT-B, respectively. Table 4 represents the results of the multivariate regression analyses. After adjusting for confounding variables including age, economic status, education, time since surgery, menopause, operation method, radiation therapy, hormone therapy, chemotherapy and performance status, SCNS was found to be a significant predictor of depression (t=-15.854, p<0.001) and QOL (t=16.187, p<0.001). Patients who reported higher unmet needs were more likely to be depressed and to have a lower QOL.
Table 4.
Regression Model with BDI and FACT-B as the Dependent Variables*
SCNS, Supportive Cancer Needs Survey; FACT-B, Functional Assessment of Cancer Therapy-Breast; BDI, Beck Depression Inventory.
*β coefficients from multiple regression are adjusted for age, economic status, education, time since surgery, menopause, operation method, radiation therapy, hormone therapy, chemotherapy and performance status.
†p<0.001.
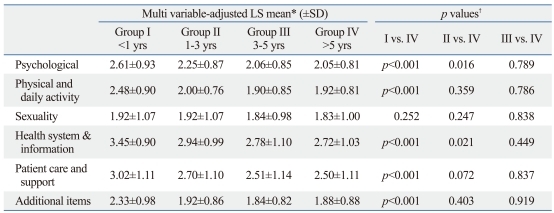
Assessment of unmet needs by survival duration
The results of the unmet needs subscales in the four groups are summarized in Table 5. Patients with a survival duration of less than 1 year since surgery (group I) exhibited a significantly greater level of unmet needs in the psychological domain (p<0.001), physical and daily living domain (p<0.001), health system and information domain (p<0.001) and the patient care and support domain (p<0.001), as well as the additional items domain (p<0.001) than patients whose survival duration was longer than 5 years since surgery (group IV). Patients with a survival duration of 1-3 years since surgery (group II) still exhibited significantly greater unmet needs than group IV in the psychological (p=0.016), and health system and information needs domain (p=0.021). Although it was not statistically significant, the adjusted mean of group II was higher than group IV (p=0.072). group III did not show a significant difference from group IV in any of the SCNS subscales. No significant difference in the sexuality domain was found relative to survival time.
Table 5.
Supportive Care Needs Survey (SCNS) Subscales for Time since Surgery
SD, standard deviation; ANCOVA, analysis of covariance.
*LS mean values from ANCOVA analyses are adjusted for age, economic status, education, time since surgery, menopause, operation method, radiation therapy, hormone therapy, chemotherapy and performance status.
†p-value represents the significance of group comparisons and is adjusted for age (at surgery), economic status, education, menopause, operation method, radiation therapy, hormone therapy, chemotherapy and performance status.
DISCUSSION
The present study showed that patients with a survival duration less than 1 year had a significantly higher level of needs than the other groups of patients, and those with a survival duration of 1-3 years still had higher needs than long-term survivors over 5 years since surgery. The highest levels of need were found to be in the health system and information domain, which accounted for 9 out of the top 10 unmet needs items, with 1 item in the patient care and support domain. Also, unmet needs were found to be significantly related with depression and QOL.
The prevalence of the ten highest moderate-to-high unmet needs among patients with breast cancer in this study was between 35.5% and 54.1%, which is higher than an Australian study,14 but lower than a Japanese study.8 An Australian study using SCNS found that the prevalence of the ten highest needs was between 30% and 40%,15 whereas it was between 40% and 63% in a Japanese study.8 In addition, the prevalence of unmet needs in this study was lower than that reported in our previous study with a different study sample.9 This finding may reflect improvement in the care of patients for the past few years.
Nine out of ten highest needs were found in the health system and information domain in our study. This is consistent with the results of studies assessing the unmet needs of breast cancer survivors,21,22 where they reported the greatest unmet needs in the information and medical communication domain. This could be an indication of dissatisfaction with information received at follow-up care. Research has shown that cancer patients were found to be less satisfied with information and support than clinical aspects of care they receive,15,23,24 which our study partly confirms.
However, considering that increased levels of depression, anxiety, and concern about future health predicted significantly increased needs of information and medical communication,21 patients in our study could have expressed their psychological anxiety in the form of practical information and support needs instead of psychological needs. The fact that patient education programs are regularly provided and cyber information is so easily accessible these days indicates they might need not just information but direct, face-to face explanation and psychological assurance from clinicians. Also, this could be explained by cultural differences, as Asian depressive people are generally more likely to be somatized.22 It is known that Caucasian cancer patients report more unmet psychological needs,22,25,26 reflecting desire for psychological support than Asian patients. In addition, the current study results showed lower mean scores on the sexuality needs across time, which could be another aspect of cultural differences. This warrants further exploration.
Unmet needs were found to have a significantly negative effect on QOL of breast cancer patients, which confirms a Japanese study27 and another study with brain tumor patients.28 Our findings suggest that interventions based on specific unmet needs could result in ameliorating depression of breast cancer survivors and enhancing their QOL.
Time since surgery was found to be a strong predictor of unmet needs of breast cancer survivors. Patients in the group with a survival duration of less than 1 year since surgery reported significantly higher mean scores in the psychological, physical and daily living, health system and information, patient care and support, and additional items domains than other patient groups. This result is understandable, considering that patients in the early phase after surgery are known to have reduced QOL14 and therefore, they might have more needs to be met because of treatment- related impairments. However, patients in the group with a survival duration between 1-3 years since surgery also reported significantly higher needs in the psychological domain and health system and information domain than those over 5 years since surgery. This might reflect that patients with a survival time of 1-3 years after surgery are still under the influence of psychosocial morbidities. This result suggests that oncologic professionals should pay more attention to psychological and information needs of patients even after 1 year since surgery. On the other hand, the mean scores of unmet needs of patients with a survival duration between 3-5 years did not significantly differ from those of long-term survivors of over 5 years since surgery. This result confirms other research, which showed long-term breast cancer survivors reported high levels of functioning on several dimensions of QOL,10-12 and shorter time elapsed since surgery was associated with low QOL.29 This suggests that if future prospective studies confirm the present findings, then psychosocial interventions and services could be designed to focus on improving health system and information services and should target patients with a survival duration of less than 3 years since surgery. Especially, considering that patients reported high needs for counseling or to have someone to talk with concerning all aspects of their condition, treatment, and follow-up, a greater multidisciplinary oncologic care approach including mental health professionals and social workers as well as oncologic surgeons is suggested. Breast cancer survivors should discuss their needs and concerns with their cancer specialists during follow-up. However, many studies have reported the difficulties health professionals face in identifying and satisfying the informational and emotional needs of patients in cancer settings.30 That being so, they could simply ask patients to complete unmet needs assessment tools such as SCNS-Short Form31 at follow-up visits. This could help the professionals tailor psychosocial services to meet the needs of the patients.
This study has several limitations. First, as our study was of a cross-sectional design, we cannot be sure of cause-effect relationships. Distress may create unmet needs, or unmet needs may generate distress. In addition, changes in unmet needs over time could only be determined indirectly. Third, because the study sample represents only one urban university hospital, the study results cannot be generalized to all breast cancer survivors over the country.
In conclusion, the present study demonstrated that patients with a survival duration of less than 1 year had a significantly higher level of needs than the other groups of patients and those with survival duration of 1-3 years still had higher needs than long-term survivors over 5 years since surgery. In addition, the current study result that the health system and information needs were found to be the highest suggests various strategies are needed, such as systemic changes to the multidisciplinary provision of care, improvement of the interactional skills of health professionals, or providing feedback to clinicians by simple needs assessment. Consequently, psychosocial interventions aimed at meeting specific unmet needs may improve QOL of breast cancer patients.
ACKNOWLEDGEMENTS
This work was supported by the Duksung Women's University Research Grant 3000001085.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Ministry of Health, Welfare & Family Affairs. Annual Report of Cancer Incidence (2007), Cancer Prevalence (2007) and Survival (1993-2007) in Korea. Seoul: Ministry of Health, Welfare & Family Affairs; 2009. [Google Scholar]
- 2.Rowland JH, Hewitt M, Ganz PA. Cancer survivorship: a new challenge in delivering quality cancer care. J Clin Oncol. 2006;24:5101–5104. doi: 10.1200/JCO.2006.09.2700. [DOI] [PubMed] [Google Scholar]
- 3.Cella DF. Cancer survival: psychosocial and public issues. Cancer Invest. 1987;5:59–67. doi: 10.3109/07357908709020308. [DOI] [PubMed] [Google Scholar]
- 4.Welch-McCaffrey D, Hoffman B, Leigh SA, Loescher LJ, Meyskens FL., Jr Surviving adult cancers. Part 2: psychosocial implications. Ann Intern Med. 1989;111:517–524. doi: 10.7326/0003-4819-111-6-517. [DOI] [PubMed] [Google Scholar]
- 5.Bonevski B, Sanson-Fisher R, Girgis A, Burton L, Cook P, Boyes A Supportive Care Review Group. Evaluation of an instrument to assess the needs of patients with cancer. Cancer. 2000;88:217–225. doi: 10.1002/(sici)1097-0142(20000101)88:1<217::aid-cncr29>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 6.Foot G, Sanson-Fisher R. Measuring the unmet needs of people living with cancer. Cancer Forum. 1995;19:131–135. [Google Scholar]
- 7.Yang HC, Thornton LM, Shapiro CL, Andersen BL. Surviving recurrence: psychological and quality-of-life recovery. Cancer. 2008;112:1178–1187. doi: 10.1002/cncr.23272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akechi T, Okuyama T, Endo C, Sagawa R, Uchida M, Nakaguchi T, et al. Patient's perceived need and psychological distress and/or quality of life in ambulatory breast cancer patients in Japan. Psychooncology. 2011;20:497–505. doi: 10.1002/pon.1757. [DOI] [PubMed] [Google Scholar]
- 9.Hwang SY, Park BW. The perceived care needs of breast cancer patients in Korea. Yonsei Med J. 2006;47:524–533. doi: 10.3349/ymj.2006.47.4.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ganz PA, Desmond KA, Leedham B, Rowland JH, Meyerowitz BE, Belin TR. Quality of life in long-term, disease-free survivors of breast cancer: a follow-up study. J Natl Cancer Inst. 2002;94:39–49. doi: 10.1093/jnci/94.1.39. [DOI] [PubMed] [Google Scholar]
- 11.Ahn SH, Park BW, Noh DY, Nam SJ, Lee ES, Lee MK, et al. Health-related quality of life in disease-free survivors of breast cancer with the general population. Ann Oncol. 2007;18:173–182. doi: 10.1093/annonc/mdl333. [DOI] [PubMed] [Google Scholar]
- 12.Cui Y, Shu XO, Gao Y, Cai H, Wen W, Ruan ZX, et al. The long-term impact of medical and socio-demographic factors on the quality of life of breast cancer survivors among Chinese women. Breast Cancer Res Treat. 2004;87:135–147. doi: 10.1023/B:BREA.0000041620.76871.97. [DOI] [PubMed] [Google Scholar]
- 13.Weitzner MA, Meyers CA, Stuebing KK, Saleeba AK. Relationship between quality of life and mood in long-term survivors of breast cancer treated with mastectomy. Support Care Cancer. 1997;5:241–248. doi: 10.1007/s005200050067. [DOI] [PubMed] [Google Scholar]
- 14.Holzner B, Kemmler G, Kopp M, Moschen R, Schweigkofler H, Dünser M, et al. Quality of life in breast cancer patients--not enough attention for long-term survivors? Psychosomatics. 2001;42:117–123. doi: 10.1176/appi.psy.42.2.117. [DOI] [PubMed] [Google Scholar]
- 15.Sanson-Fisher R, Girgis A, Boyes A, Bonevski B, Burton L, Cook P Supportive Care Review Group. The unmet supportive care needs of patients with cancer. Cancer. 2000;88:226–237. doi: 10.1002/(sici)1097-0142(20000101)88:1<226::aid-cncr30>3.3.co;2-g. [DOI] [PubMed] [Google Scholar]
- 16.Hahn HM, Yum TH, Shin YW, Kim KU, Yoon DJ, Chung KJ. A standardization study of Beck Depression Inventory in Korea. J Korean Neuropsychiatr Assoc. 1986;25:487–501. [Google Scholar]
- 17.Lee YH, Song JY. A study of reliability and the validity of the BDI, SDS, and MMPI-D scale. Korean J Clin Psychol. 1991;10:98–113. [Google Scholar]
- 18.Brady MJ, Cella DF, Mo F, Bonomi AE, Tulsky DS, Lloyd SR, et al. Reliability and validity of the Functional Assessment of Cancer Therapy-Breast quality-of-life instrument. J Clin Oncol. 1997;15:974–986. doi: 10.1200/JCO.1997.15.3.974. [DOI] [PubMed] [Google Scholar]
- 19.Yoo HJ, Ahn SH, Eremenco S, Kim H, Kim WK, Kim SB, et al. Korean translation and validation of the functional assessment of cancer therapy-breast (FACT-B) scale version 4. Qual Life Res. 2005;14:1627–1632. doi: 10.1007/s11136-004-7712-1. [DOI] [PubMed] [Google Scholar]
- 20.Sørensen JB, Klee M, Palshof T, Hansen HH. Performance status assessment in cancer patients. An inter-observer variability study. Br J Cancer. 1993;67:773–775. doi: 10.1038/bjc.1993.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thewes B, Butow P, Girgis A, Pendlebury S. Assessment of Unmet Needs among Survivors of Breast Cancer. J Psychosocial Oncol. 2004;22:51–73. doi: 10.1002/pon.710. [DOI] [PubMed] [Google Scholar]
- 22.Lam WW, Au AH, Wong JH, Lehmann C, Koch U, Fielding R, et al. Unmet supportive care needs: a cross-cultural comparison between Hong Kong Chinese and German Caucasian women with breast cancer. Breast Cancer Res Treat. 2011;130:531–541. doi: 10.1007/s10549-011-1592-1. [DOI] [PubMed] [Google Scholar]
- 23.Wiggers JH, Donovan KO, Redman S, Sanson-Fisher RW. Cancer patient satisfaction with care. Cancer. 1990;66:610–616. doi: 10.1002/1097-0142(19900801)66:3<610::aid-cncr2820660335>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 24.Tierney AJ, Taylor J, Closs SJ. Knowledge, expectations and experiences of patients receiving chemotherapy for breast cancer. Scand J Caring Sci. 1992;6:75–80. doi: 10.1111/j.1471-6712.1992.tb00128.x. [DOI] [PubMed] [Google Scholar]
- 25.Beesley V, Eakin E, Steginga S, Aitken J, Dunn J, Battistutta D. Unmet needs of gynaecological cancer survivors: implications for developing community support services. Psychooncology. 2008;17:392–400. doi: 10.1002/pon.1249. [DOI] [PubMed] [Google Scholar]
- 26.Harrison JD, Young JM, Price MA, Butow PN, Solomon MJ. What are the unmet supportive care needs of people with cancer? A systematic review. Support Care Cancer. 2009 doi: 10.1007/s00520-009-0615-5. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 27.Uchida M, Akechi T, Okuyama T, Sagawa R, Nakaguchi T, Endo C, et al. Patients' supportive care needs and psychological distress in advanced breast cancer patients in Japan. Jpn J Clin Oncol. 2011;41:530–536. doi: 10.1093/jjco/hyq230. [DOI] [PubMed] [Google Scholar]
- 28.Bunston T, Mings D, Laperriere N, Malcolm J, Williams D. The impact of psychosocial need and needs resolution on quality of life in patients with brain tumors. Neurosurg Focus. 1998;4:e7. doi: 10.3171/foc.1998.4.6.10. [DOI] [PubMed] [Google Scholar]
- 29.Park BW, Lee S, Lee AR, Lee KH, Hwang SY. Quality of life differences between younger and older breast cancer patients. J Breast Cancer. 2011;14:112–118. doi: 10.4048/jbc.2011.14.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maguire P, Booth K, Elliott C, Jones B. Helping health professionals involved in cancer care acquire key interviewing skills--the impact of workshops. Eur J Cancer. 1996;32A:1486–1489. doi: 10.1016/0959-8049(96)00059-7. [DOI] [PubMed] [Google Scholar]
- 31.Boyes A, Girgis A, Lecathelinais C. Brief assessment of adult cancer patients' perceived needs: development and validation of the 34-item Supportive Care Needs Survey (SCNS-SF34) J Eval Clin Pract. 2009;15:602–606. doi: 10.1111/j.1365-2753.2008.01057.x. [DOI] [PubMed] [Google Scholar]