Abstract
Prostaglandin F2α (PGF2α) induces luteolysis within a few days in cows, and immune cells increase in number in the regressing corpus luteum (CL), implying that luteolysis is an inflammatory-like immune response. We investigated the rapid change in polymorphonuclear neutrophil (PMN) numbers in response to PGF2α administration as the first cells recruited to inflammatory sites, together with mRNA of interleukin-8 (IL-8: neutrophil chemoattractant) and P-selectin (leukocyte adhesion molecule) in the bovine CL. CLs were collected by ovariectomy at various times after PGF2α injection. The number of PMNs was increased at 5 min after PGF2α administration, whereas IL-8 and P-selectin mRNA increased at 30 min and 2 h, respectively. PGF2α directly stimulated P-selectin protein expression at 5–30 min in luteal endothelial cells (LECs). Moreover, PGF2α enhanced PMN adhesion to LECs, and this enhancement by PGF2α was inhibited by anti-P-selectin antibody, suggesting that P-selectin expression by PGF2α is crucial in PMN migration. In conclusion, PGF2α rapidly induces the accumulation of PMNs into the bovine CL at 5 min and enhances PMN adhesion via P-selectin expression in LECs. It is suggested that luteolytic cascade by PGF2α may involve an acute inflammatory-like response due to rapidly infiltrated PMNs.
Introduction
The bovine corpus luteum (CL) secretes progesterone (P) to establish and maintain pregnancy. If pregnancy is not established, the CL regresses with rapid loss of the ability to secrete P (functional regression) followed by disruption of vascular vessels and luteal cells (structural regression) [1], [2]. Luteolysis is caused by prostaglandin F2α (PGF2α) secreted from the endometrium around days 17–19 of the estrous cycle or when exogenously given during the mid-luteal phase in the cow.
Various types of immune cells such as neutrophils, eosinophils, macrophages, and CD4-positive and CD8-positive T lymphocytes exist in the bovine CL and have essential roles in ovarian function [3], [4], [5]. During luteolysis, leukocytes, especially eosinophils, macrophages and T lymphocytes, are significantly increased in number, and 70% of all proliferating cells in the bovine CL are CD14-positive macrophages [5], [6]. Moreover, inflammatory cytokines such as tumor necrosis factor α (TNFα), interleukin 1β (IL-1β), and interferon γ (IFNγ), and chemokines such as monocyte chemoattractant protein-1 (MCP-1; recruitment of macrophages) are involved in luteal regression in cows [7], [8], [9], [10]. On the other hand, luteal cells express both class I and class II major histocompatibility complex (MHC) molecules (MHC molecules are essential to the recognition of cells by T lymphocytes as either self or non-self) [11], [12] and MHC class II expression on luteal cells is significantly increased when luteal regression is induced by PGF2α [13], indicating that immune response occur between luteal cells expressed MHC class II and increased macrophages and T lymphocytes in the regressing CL. Benyo et al, [13] suggested that the demise of the CL may be involved in local autoimmune response mechanisms facilitated by increased expression of class II MHC molecules at the time of luteolysis. Additionally, the CL regresses primarily through the loss of cells by apoptosis [14], [15]. These findings suggest that the luteolytic phenomenon is an inflammatory-like immune response [3], [4], [5].
In the ovary, neutrophils are detected during the life span of the CL, and it is well known that neutrophils and its major chemoattractant, interleukin-8 (IL-8) is important for ovarian function [16], [17], [18], [19]. The recruitment of neutrophils implies overlapping succession of continuous events encompassing neutrophil inducement, rolling, and firm adhesion onto endothelial cells [20], [21]. On endothelial cells, P-selectin and E-selectin interact with neutrophils to promote their rolling and transient adhesion [22]. Other critical endothelial cell adhesion molecules, intercellular adhesion molecule (ICAM) and vascular cell adhesion molecule (VCAM) also mediate firm adhesion [23]. Generally, inflammation can be either acute or chronic [20], and acute inflammation is characterized by the infiltration of neutrophils, occurs within minutes, and dissipates within a few days [20].
We hypothesized that the bovine luteolysis involves an “acute” inflammatory-like immune response characterized by massive recruitment of neutrophils within the CL, consequently triggering a local immune response in the regressing tissue. In the present study, we investigated the number of polymorphonuclear neutrophils (PMNs) and mRNA expression of PMN migration-related factors at the early stage of PGF2α-induced luteolysis, and further examined to clarify the mechanisms of the rapid PMN migration by PGF2α into the bovine CL.
Results
Number of PMNs in the bovine CL during PGF2α-induced luteolysis
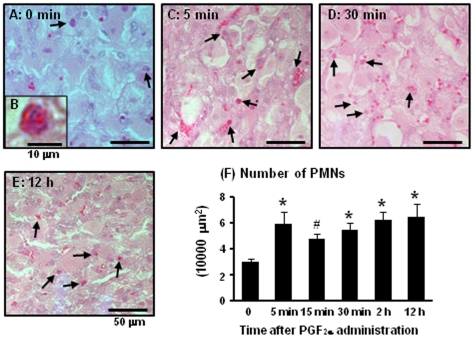
Fig. 1 show PMNs within the CL at 0 min (Fig. 1A), 5 min (Fig. 1C), 30 min (Fig. 1D) and 12 h (Fig. 1E) after PGF2α injection as detected by periodic acid-Schiff (PAS) staining. Fig. 1B indicate magnified figure of PMN which has 2–5 lobes of nuclear and finely-granular. The change in PMN number during PGF2α-induced luteolysis is shown in Fig. 1F. The number of PMNs within the CL was significantly increased (P<0.05) at 5 min, 30 min, 2 h, and 12 h after PGF2α injection, and tended to increase at 15 min (P<0.1).
Figure 1. PMN numbers in the bovine CL during PGF2α-induced luteolysis.
The typical images of PMNs within the CL at 0 min (Fig. 1A), 5 min (Fig. 1C), 30 min (Fig. 1D), and 12 h (Fig. 1E) during PGF2α-induced luteolysis. Fig. 1B indicates extended figure of PMN within the CL and Fig. 1F shows number of PMNs during PGF2α-induced luteolysis (n = 4−5 in each time), respectively. Black arrows show PMNs in the CL. Values are shown as the means ± SEM. Different superscripts indicate significant differences (P<0.05) as determined by ANOVA followed by Bonferroni's multiple comparison test.
Change of IL-8, P-selectin, E-selectin, ICAM and VCAM mRNA expression in the bovine CL and plasma P concentration during PGF2α-induced luteolysis
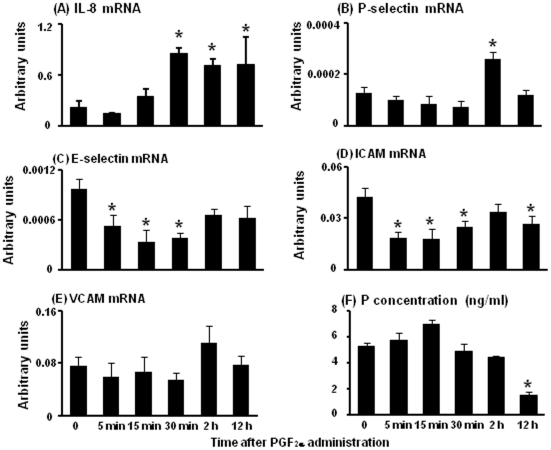
IL-8 mRNA levels were significantly increased at 30 min, 2 h and 12 h after PGF2α injection compared with 0 min (Fig. 2A). P-selectin mRNA levels were increased at 2 h after PGF2α injection (Fig. 2B). E-selectin mRNA levels were significantly decreased at 5 min, 15 min and 30 min after PGF2α injection compared with 0 min (Fig. 2C). ICAM mRNA levels were significantly decreased from 5 min to 30 min and 12 h after PGF2α injection compared with 0 min (Fig. 2D) whereas VCAM mRNA expression did not change during PGF2α-induced luteolysis (Fig. 2E). The plasma P concentration did not differ at 5 min, 15 min, 30 min, and 2 h after PGF2α injection compared with 0 min but significantly decreased at 12 h after PGF2α injection (Fig. 2F).
Figure 2. mRNA expression of IL-8, P-selectin, E-selectin, ICAM and VCAM in the bovine CL and plasma P concentration during PGF2α-induced luteolysis.
Fig. 2 indicates the change of mRNA expression of IL-8, P-selectin, E-selectin, ICAM and VCAM within the CL and plasma P concentration at 0 min, 5 min, 15 min, 30 min, 2 h and 12 h during PGF2α-induced luteolysis (n = 4−5 in each time), respectively. Values are shown as the means ± SEM. Different superscripts indicate significant differences (P<0.05) as determined by ANOVA followed by Bonferroni's multiple comparison test.
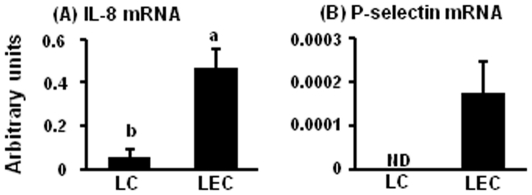
mRNA expression of IL-8 and P-selectin in luteal cells (LCs) and luteal endothelial cells (LECs)
Based on the results of Fig. 2, we investigated mRNA expression of IL-8 and P-selectin in LCs and LECs. The mRNA of IL-8 (Fig. 3A) and P-selectin (Fig. 3B) in LCs and LECs are shown in Fig. 3. IL-8 mRNA expression was higher in LECs compared with LCs. P-selectin mRNA expressed only LECs but not in LCs.
Figure 3. Expression of IL-8 and P-selectin mRNA in LCs and LECs.
Fig. 3 indicates mRNA expression of IL-8 (A) and P-selectin (B) in LCs and LECs (n = 5 in each group). All values are the means ± SEM. Different superscript indicate significant differences (P<0.05) as determined by Student's t-test.
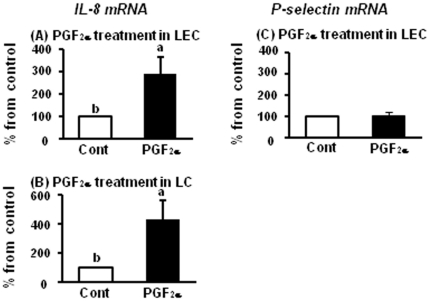
Effect of PGF2α for mRNA expression of IL-8 and P-selectin in LECs and LCs
Based on the results of Fig. 3, we investigated mRNA expression of IL-8 and P-selectin by PGF2α treatment in LECs and LCs. PGF2α treatment for 2 h increased IL-8 mRNA expression both in LECs and LCs (Fig. 4A and 4B) compared with those in control, but PGF2α treatment for 2 h did not effect on P-selectin mRNA expression in LECs (Fig. 4C).
Figure 4. Regulation on mRNA expression of IL-8 and P-selectin by PGF2α.
Fig. 4 indicates mRNA expression of IL-8 and P-selectin after PGF2α (10−6 M) treatment for 2 h in LECs and LCs (n = 5 in each group). All values are the means ± SEM. Different superscript indicate significant differences (P<0.05) as determined by Student's t-test.
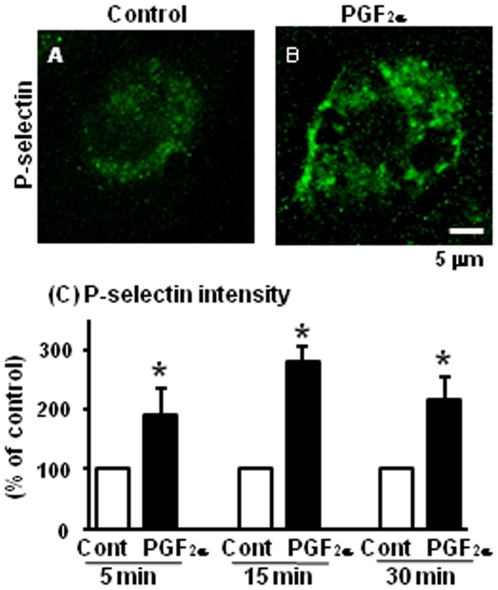
Acute effect of PGF2α for P-selectin expression in LECs
We focused on the effect of PGF2α for P-selectin protein expression in LECs since P-selectin is constitutively stored and the stimulation of endothelial cells by various mediators such as TNFα, can induce P-selectin translocation to cell surface membranes [24], [25], [26]. Fig. 5 displays typical images of P-selectin protein expression at 5 min in control (Fig. 5A) and after PGF2α treatment (Fig. 5B) and P-selectin intensity (Fig. 5C) in LECs. PGF2α treatment increased P-selectin expression (Fig. 5B) and its intensity (Fig. 5C) at 5, 15 and 30 min compared with those in control in LECs. We and other group previously confirmed that LECs used in the present study has PGF2α receptor in vitro and in vivo [27], [28].
Figure 5. Effect of PGF2α on P-selectin in LECs.
The levels of P-selectin expression after PGF2α (10−6 M) treatment in LECs. Fig. 5A shows P-selectin expression in LECs in control and Fig. 5B shows P-selectin expression in the PGF2α treatment group at 5 min (n = 4 in each group). Scale bars indicate 5 µm. Fig. 5C shows the intensity of P-selectin expression at 5, 15 and 30 after treatment, respectively (% of control). All values are the means ± SEM. Different superscript indicate significant differences (P<0.05) as determined by Student's t-test.
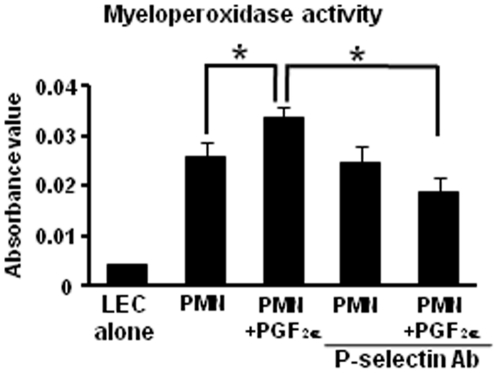
Involvement of PGF2α and P-selectin in the adhesion of PMNs to LECs
We investigated the impact of PGF2α and P-selectin for adhesion of PMNs to LECs (Fig. 6). Before the addition of PMNs, LECs were preincubated with or without anti-P-selectin (10 µg/mL) antibody for 30 min. PMNs were added to the cultures in the presence or absence of PGF2α (10−6 M) for 30 min because it took time for depression of PMNs on LECs. As shown in Fig. 6, the adhesion between PMNs and LECs was significantly enhanced by treatment with PGF2α as compared with untreated PMNs (without PGF2α). This enhancement by PGF2α of PMN adhesion to LECs was inhibited by pretreatment of LECs with anti-P-selectin antibody.
Figure 6. Effect of PGF2α and P-selectin for PMN adhesion to LECs.
The myeloperoxidase activity of PMNs was measured as an indicator of the number of PMNs (Fig. 6). Before the addition of PMNs, LECs were preincubated with or without anti-P-selectin (10 µg/mL) monoclonal antibody for 30 min. PMNs were added onto LECs with or without PGF2α (10−6 M) for 30 min (n = 4 in each group). All values are the means ± SEM. Different superscripts indicate significant differences (P<0.05).
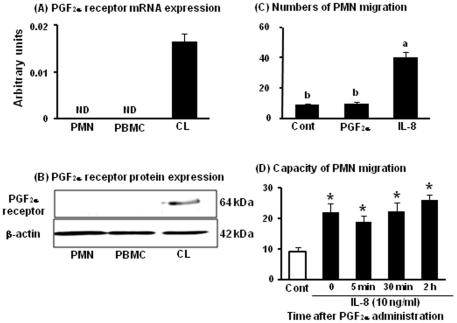
Expression of FPr in PMNs, PBMCs, and the mid CL and PMN migration stimulated by PGF2α and IL-8
We further investigated the possibility whether PGF2α directly stimulates the recruitment of neutrophils. The mRNA (Fig. 7A) and protein (Fig. 7B) expression of PGF2α receptor (FPr) in PMNs, PBMCs, and the mid CL tissue are shown in Fig. 7. Liptak et al. reported that the bovine immune cells did not express FPr mRNA [29]. Same with the previous study, both FPr mRNA and protein were detected in the mid CL tissue but not in PMNs or PBMCs. The number of migrating PMNs in the transmigration assay is shown in Fig. 7C. IL-8 (50 ng/ml) significantly increased PMN migration about 4-fold compared to control. However, PGF2α treatment (10−6 M) did not stimulate PMN migration. These findings suggest that PGF2α cannot induce the PMN migration directly.
Figure 7. Expression of FPr in PMNs, PBMCs, and the mid CL and transmigration assay of PMNs by PGF2α and IL-8.
The mRNA and protein levels of FPr (A and B) in PMNs, PBMCs and the mid CL tissue (n = 4 in each group). All values are the means ± SEM (relative to β-actin mRNA levels). Representative photograph of a western blot is shown for FPr and β-actin (B). The number of PMNs migration by PGF2α (10−6 M) and IL-8 (50 ng/ml) is shown in Fig 7C (n = 4 in each group). The number of migrating PMNs after PGF2α administration is shown in Fig 7D. White bar indicates control (PMNs before PGF2α administration, IL-8 un-stimulate) and black bars indicate IL-8 (10 ng/ml)-stimulated PMNs (at 0 min, 5 min, 30 min, and 2 h after PGF2α administration, n = 4 in each time point). Values are shown as the means ± SEM. Different superscript indicate significant differences (P<0.05) as determined by ANOVA followed by the Bonferroni's multiple comparison test.
Capacity of PMN migration during PGF2α-induced luteolysis
The number of migrating PMNs during PGF2α-induced luteolysis is shown in Fig. 7D. PMNs collected from before and at 5 min, 30 min, and 2 h after PGF2α administration were used for the transmigration assay. IL-8 (10 ng/ml of IL-8 is significantly effective dose to stimulate PMN migration (data not shown)) stimulated PMN migration in all of the experimental groups; however, the levels of PMN migration did not change after PGF2α administration relative to the levels before administration, suggesting that PGF2α injection did not change the capacity/sensitivity of PMN migration.
Discussion
In the present study, we hypothesized that the bovine luteolysis involves an “acute” inflammatory-like immune response characterized by massive recruitment of neutrophils within the CL. Regarding neutrophilic chemoattractants, mRNA expression of IL-8 started to increase at 30 min after PGF2α administration. Additionally, P-selectin mRNA expression was increased at 2 h after PGF2α administration. Surprisingly, the number of PMNs already increased at 5 min after PGF2α administration before the mRNA levels of IL-8 and P-selectin increased, suggesting that PGF2α injection may change the microenvironment of the CL to induce acute PMN accumulation in cows.
To clarify the mechanism of rapid PMN accumulation into the CL after PGF2α injection, we examined whether PGF2α affects adhesion system such as the rolling of immune cells via P-selectin. P-selectin mRNA was expressed in LECs but not in LCs (Fig. 3B) and increased at 2 h, but not earlier after PGF2α injection in vivo (Fig. 2B). Other PMN adhesion-related factors such as E-selectin, ICAM and VCAM did not increase during the experimental period in vivo. In the in vitro experiment in the present study, we showed that PGF2α treatment directly stimulated P-selectin expression at 5, 15 and 30 min in LECs (Fig. 5). Moreover, PGF2α enhanced PMN adhesion to LECs, and this enhancement by PGF2α of PMN adhesion was inhibited by anti-P-selectin antibody (Fig. 6). These findings suggest that P-selectin expression stimulated by PGF2α is a key event in PMN migration within the CL. It has been shown that P-selectin is constitutively stored within Weibel-Palade bodies (WPBs) and the stimulation of endothelial cells by various mediators such as TNFα, vascular endothelial growth factor, angiopoietins, histamine, and thrombin can induce the fusion of WPBs to cell surface membranes and P-selectin translocation [24], [25], [26]. Moreover, the expression of P-selectin peaked within 5 min after thrombin challenge, and neutrophil adhesion induced by thrombin was inhibited by P-selectin antibody in human endothelial cells [24]. These findings imply that a rapid induction of P-selectin is an essential process in tissue inflammation, and the bovine CL may have a similar system to induce an acute inflammatory-like response during PGF2α-induced luteolysis.
In addition, we examined the expression of IL-8 and the effect of PGF2α treatment in LCs and LECs in vitro. IL-8 mRNA was detected both in LCs and LECs. Actually, ovarian cells such as theca, granulosa and granulosa-lutein cells express IL-8 mRNA and produce IL-8 in cows [30], rabbits [31], rats [19] and human [16], [32]. In the in vitro cell culture experiment, PGF2α treatment for 2 h stimulated IL-8 mRNA expression both in LCs and LECs. Indeed, in endometrial adenocarcinoma cells transfected with the FPr, PGF2α promoted the synthesis and release of IL-8 in a time-dependent manner [33]. Additionally, the number of PMNs within the CL maintained high levels up to 12 h after PGF2α administration, suggesting that PGF2α may partly regulate the inflammatory microenvironment in the regressing CL via neutrophilic chemoattractant IL-8.
We further investigated the possibility whether PGF2α directly stimulates the recruitment of PMNs into the CL. As Liptak et al. already showed that the bovine immune cells had no FPr mRNA [29], PMNs as well as PBMCs did not express PGF2α receptor mRNA and protein (Fig. 7). Moreover, PGF2α injection in vivo did not change the response level of PMN migration stimulated by IL-8 (Fig. 7D), suggesting that PGF2α injection did not change the capacity/sensitivity of PMN migration. Thus, PGF2α cannot directly attract immune cells into the CL, and the rapid and local induction such as P-selectin and IL-8 by PGF2α within the CL is the key component to induce PMN migration in cows.
Neutrophils are the first cells recruited to inflammatory sites, providing cytokines and proteolytic enzymes [21]. In rats, co-incubation of luteal cells with activated neutrophils by N-formyl-methionyl-leucyl-phenylalanine (fMLP) reduced LH-stimulated cAMP accumulation and P secretion, which was dependent upon the number of neutrophils [34]. Moreover, a pretreatment with antibody against CD18 (leukocyte integrin) significantly inhibited not only PGF2α-induced neutrophil accumulation but also the decrease in serum P concentrations [35]. Also, neutrophils accumulate in the equine CL after PGF2α administration [18]. Therefore, neutrophils infiltrated within the CL may also play a role in functional regression of the CL.
In the earliest phenomenon of luteolysis, oxytocin secretion in plasma from ovarian vein started to increase within 5 min after PGF2α administration [36]. We also found in the present study the rapid increase of PMNs within the CL examined at 5 min after PGF2α injection. Indeed, PGF2α can induce PMN increase following the peritoneum injection in rats [37]. Generally, an acute inflammation is characterized by the infiltration of PMNs within a few minutes and continuous occurrence of lymphocyte and macrophage migration. PMNs can produce various types of inflammatory cytokines recruiting lymphocytes and macrophages such as IL-8, TNFα and IFNγ[21], [38], [39], [40]. Also, a large number of lymphocytes and macrophages were observed within the bovine CL at 6–24 h after PGF2α administration, and these immune cells are considered to be essential for a rapid demise of the CL tissue [3], [4], [13], [41]. Indeed, inflammatory cytokines recruiting lymphocytes and macrophages such as TNFα and IFNγ clearly stimulate apoptosis in the bovine luteal cells and luteal endothelial cells [10], [42]. These findings suggest that acutely migrated PMNs have the potential to recruit other immune cells during luteolysis to progress structural regression in cows.
The mechanism of luteolysis is different depending on the species among cows, rodents and humans [43]. For example, although immune cells are also recruited into the CL to induce apoptosis and phagocytosis during luteolysis in rodents and humans same as cows, the initial signal of luteolytic mechanism seems to be different between these animals; as PGF2α is the trigger of the bovine luteolysis, preovulatory prolactin surges are the trigger in cycling rats whereas absence of human chorionic gonadotropin could be a signal for initiation of luteolysis in humans [43]. Further investigation is required to determine whether the rapid accumulation of PMNs into the CL by the luteolytic trigger is the bovine specific phenomenon or common phenomenon between species.
In conclusion, PGF2α rapidly induced the accumulation of PMNs within the bovine CL at 5 min after administration. PGF2α treatment directly stimulated P-selectin expression and enhanced PMN adhesion in LECs via P-selectin. It is suggested that luteolytic cascade by PGF2α involves an acute inflammatory-like response due to acute migrated PMNs in cows, and these PMNs may have a potential to recruit other immune cells in the regressing CL.
Materials and Methods
The collection of CL in the experiment of PGF2α-induced luteolysis was conducted at the Clinic for Cattle, University of Veterinary Medicine Hannover, Germany. The experimental procedures complied with guidelines of the ethics committee on animal right protection of Oldenburg, Germany in accordance with German legislation on animal rights and welfare and the protocol was approved by the committee on the Ethics of Animal Experiments of University of Veterinary Medicine Hannover (Permit number: 33.9-42502-04-07/1275). The blood collection experiments were conducted at the Field Center of Animal Science and Agriculture, Obihiro University, and all experimental procedures complied with the Guidelines for the Care and Use of Agricultural Animals of Obihiro University and the protocol was approved by the committee on the Ethics of Animal Experiments of Obihiro University (Permit number: 19–10).
In vivo study: PGF2α-induced luteolysis
For collecting the CL during luteolysis, 29 normal cyclic German Holstein cows were used for this study. The day of estrus was designated as day 0. Cows (n = 4−5 for each time point) at the mid luteal phase (days 10–12) were injected with PGF2α in intramuscular (0 h) (0.5 mg of cloprostenol, 2.0 mL of Estrumate™, Essex Tierarznei, Munich, Germany), and ovaries were collected by ovariectomy [44] through the vagina at 0 ( = before PGF2α injection), 5, 15, and 30 min and 2 and 12 h. Simultaneous plasma samples were collected by caudal venipuncture for P measurements, and were immediately frozen at −20°C until further analysis.
Processing of the corpus luteum
The CL was enucleated from the ovary and dissected free of connective tissue as previously described [28]. Subsequently, the CL was fixed with 10% formaldehyde and embedded in paraffin wax according to the standard histological technique. In addition, the remaining CL was prepared for molecular biological purposes. The CL tissue samples were collected, minced, immediately placed into a 1.5 mL microcentrifuge tube with or without 0.4 mL of TRIzol reagent (Invitrogen, Karlsruhe, Germany), and stored at −80°C until analysis.
In vitro study: Expression and regulation of IL-8 and P-selectin mRNA in steroidogenic luteal cells and luteal endothelial cells by PGF2α
Steroidogenic luteal cells (LCs) culture
The CLs of the mid luteal phase were collected at local slaughterhouse, and dispersed using collagenase IV (SIGMA, St. Louis, MO, USA). The luteal stages were classified as mid (days 10–12) by macroscopic observation of the ovary as described previously [45]. LCs were used in the present study using the method described by Klipper et al. [46]. Briefly, LCs were isolated from the bovine mid CL (Days 8–12 of the estrous cycle) using magnetic tosylactivated beads coating with BS-1 lectin (binds glycoproteins on the bovine endothelial cells), indicating BS-1 positive cells are endothelial cells. In the present study, BS-1 negative cells were assessed as LCs as described previously [46]. LCs were cultured in DMEM/F-12 medium (Invitrogen Corporation, Tokyo, Japan) containing 5% fetal bovine serum (FBS; Invitrogen Corporation), 2.2% NaHCO3, gentamicin solution (50 mg/L, SIGMA), and amphotericin B solution (2.5 mg/L, SIGMA).
Luteal endothelial cells (LECs) culture
LECs were used in the present study using the method described by Spanel-Borowski et al. [47]. Cytokeratin-negative LECs isolated from the CLs of the cows during the mid-luteal phase were used as described previously [47]. LECs were grown on plates pre-coated with 1% Vitrogen in DMEM/F-12 medium containing 5% FBS, 2.2% NaHCO3, gentamicin solution, and amphotericin B solution. All experiments in the present study were carried out on LECs from passages 5 to 8.
For analysis of mRNA expression, LCs and LECs were cultured for 24 h at 37°C, were placed into a 1.5 mL microcentrifuge tube with 400 µL of TRIzol reagent and stored at −80°C until analysis.
Treatment with PGF2α
LCs were cultured for 24 h after isolation and LECs were grown until confluent, rinsed with PBS twice, and stimulated with medium only (control) or PGF2α (10−6 M) for 2 h at 37°C in DMEM/F-12 medium containing 0.1% FBS, NaHCO3, gentamicin solution, and amphotericin B solution. At the end of the treatment period, cells were collected and stored at −80°C until the mRNA expression was analyzed. At least 5 experiments were performed, with each concentration of agents tested with 2 replicates/experiments.
Effect of PGF2α on P-selectin expression in LECs
Treatment with PGF2α and immunofluorescence
The experimental method was modified from that of Maliba et al. [26]. LECs were grown until confluent, rinsed with PBS twice, and stimulated with PGF2α (10−6 M, SIGMA) for 5, 15 and 30 min in DMEM/F-12 medium containing 0.1% FBS, 2.2% NaHCO3, gentamicin solution, and amphotericin B solution. LECs were fixed with 1% paraformaldehyde-PBS solution for 20 min at room temperature. Following fixation, the cells were washed with PBS 3 times and incubated with blocking solution (4% normal goat serum in PBS) for 15 min at room temperature. Cells were incubated with mouse anti-human P-selectin reacted with cow antibody (1∶100 dilution, AbD serotec) for 24 h at 4°C. Cells were rinsed with PBS and incubated with rabbit anti-mouse conjugated to Alexa 488 IgG (1∶400 dilution, Invitrogen) for 60 min at room temperature. The cells were observed with a confocal microscope (DMI6000B, Leica Microsystems, USA), and rabbit anti-mouse conjugated to Alexa 488 was visualized using a 488-nm argon laser. Intensity of P-selectin staining was calculated by pixel sum/area of LECs using accessory software for this microscopy. In each experiment, at least 20 LECs were calculated the intensity of P-selectin. At least 4 experiments were performed, with each concentration of agents tested with 2 replicates/experiments.
Effect of PGF2α and anti-P-selectin antibody for PMN adhesion to LECs
Isolation of PMNs and PBMC
PMNs and peripheral blood mononuclear cells (PBMCs) were isolated from whole blood collected via jugular veinipuncture on days 8–12 of the estrous cycle (day of ovulation = day 1) as described previous our study [48]. Blood samples were centrifuged at 1000×g for 30 min at 10°C over LymphoprepTM (Axis-Shield, Oslo, Norway) according to the manufacture's method. The plasma was removed and buffy coat were separated as PBMCs, and lower layer under buffy coat used for separation of PMNs. To remove red blood cells, hypotonic distilled water was added to PMNs and PBMCs for approximately 5 s. Isotonicity was restored by the addition of twice-concentrated PBS and centrifuged at 500×g for 10 min at 10°C. This lysis procedure was repeated twice on the cell pellet. Isolated PMNs and PBMCs were resuspended at a concentration of 2×106 cell/mL in RPMI 1640 (Invitrogen Corporation) containing 0.1% FBS, gentamicin solution, and amphotericin B solution. To check the purity of PMNs before using for the experiment, the purity of PMNs was >95% and these cells resulted in nearly pure granulocyte populations as determined by flow cytometric evaluation (Beckman Coulter, Inc., CA, UAS) [48]. Additionally, we observed giemsa-stained PMNs by microscope, these cells were clear granule and segmented nuclear. Although peripheral granulocytes include neutrophils, eosinophils and basophils in generally, the purity of neutrophils (2–5 lobes of nuclear and finely-granular) was >95% in these PMNs by microscope observation in the present study since character was different between neutrophils and eosinophils (double nuclear and coarsely-granular). Moreover, in the flow cytometric evaluation of PBMCs, the purity of PBMCs was >96% assessed by lower granular and these cell size [48].
PMNs-LECs adhesion assay
The experimental method was modified from that of Yasuda et al [49]. LECs were grown until confluent. Before the addition of PMNs, LECs were preincubated with or without anti-P-selectin (10 µg/mL) monoclonal antibody for 30 min. PMNs isolated from blood sample (n = 4) during the mid-luteal phase (1×106 cell/mL) were added to the cultures in the presence or absence of PGF2α (10−6 M) for 30 min in DMEM/F-12 medium containing 5% FBS, NaHCO3, gentamicin solution, and amphotericin B solution. After incubation, non-attached cells were washed out 3 times with PBS containing 2% FBS, and 100 µL of citrate buffer (SIGMA) containing 0.1% Triton X-100 was added to each well. After 10 min, 200 µL of o-phenylenediamine dihydrochloride (SIGMA)-citrate buffer solution containing 0.04% H2O2 was added to each well. After incubation at room temperature for 30 min, 50 µL of 4N-H2SO4 was added to stop the reaction, and the myeloperoxidase activity of neutrophils was measured at OD490. At least 4 experiments were performed, with each concentration of agents tested with 2 replications/experiments.
PGF2α receptor (FPr) mRNA and protein expression
Sample collection
PMNs and PBMCs were isolated from whole blood on days 10–12 of the estrous cycle (n = 4) as described above. Ovaries with the CL from Holstein cows were collected at a local slaughterhouse, and the mid CL were collected as described above (n = 4). For analysis of mRNA and protein expression, PMNs, PBMCs, and CL tissues were placed into a 1.5 mL microcentrifuge tube with or without 400 µL of TRIzol reagent and stored at −80°C until analysis.
Transmigration assay of PMNs by PGF2α and IL-8
Transmigration assay
PMN chemotaxis was evaluated using a 10-well microchemotaxis chamber (Neuro probe, Gaithersburg, MD, USA). In this instrument, test solutions in the bottom chamber are separated from leukocytes in the upper chamber by an 8- µm pore size filter (Neuro probe). The lower well was pre-filled with 100 µL of 100% isotonic Percoll (Pharmacia, Freiburg, Germany) to avoid adherence and loss of transmigrated PMNs to the bottom and wall of the lower well. The following solutions (300 µL) were pipetted onto the bottom chamber: (1) RPMI 1640 medium alone as a control, (2) PGF2α (10−6 M; SIGMA), and (3) 50 ng/ml of the recombinant bovine IL-8 (Kingfisher, Biotech, Inc. St. Paul, MN, USA) as a positive control. Fifty ng/ml of IL-8 is significantly maximal does to stimulate neutrophil migration (data not shown). After assembling the instrument, PMNs were added to the upper chamber (250 µL/well, 2×106 cell/mL). After incubation at 37 °C in 5% CO2 for 3 h, migrated cells in the bottom chamber were counted under light microscopy. At least 4 experiments were performed, with each concentration of agents tested with 2 replications/experiments.
Transmigration assay of PMNs before and after PGF2α administration
Blood sample collection
For collecting PMNs, 4 normal cyclic non-lactating Holstein cows were used for this study. The day of estrus was designated as day 0. Cows (n = 4 for each time point) at the mid luteal phase (days 10–12) were injected with PGF2α (0 h) and blood samples were collected before and 5 min, 30 min, and 2 h after PGF2α administration. Then, PMNs were separated as described above and set concentrations as 2×106 cell/mL in RPMI 1640 medium.
Transmigration assay
The following solutions and PMNs (250 µL/well, 2×106 cell/mL) were pipetted onto the bottom and upper chamber: (1) RPMI 1640 medium in the bottom and neutrophils (before PGF2α injection) in the upper chamber as a control and (2) 10 ng/ml of IL-8 in the bottom and PMNs (at 0 min, 5 min, 30 min, and 2 h after PGF2α injection) in the upper chamber as experimental groups. Ten ng/ml of IL-8 is significantly effective does to stimulate PMN migration (data not shown). After incubation at 37 °C in 5% CO2 for 3 h, migrated cells in the bottom chamber were counted under light microscopy.
P determination
The plasma P concentration was determined by direct enzyme immunoassays (EIA) [45]. The minimum detectable concentration of the assay was 0.3 ng/mL. The intra- and interassay coefficients of variation were 6.2% and 12.5%, respectively. P was extracted using diethyl ether as described previously [45]. The recovery rate of P was 88%. The intra- and interassay coefficients of variation were 6.2% and 9.3%, respectively.
Detection of neutrophils in the CL using periodic acid-Schiff (PAS) reaction
Formalin-fixed sections (5 µm) of the CL samples were stained with PAS reagent (Sigma) for 10 min and then counterstained with hematoxylin described as previous study [18], [48]. In general, it is recognized that PAS staining is useful method to detect granulophilic leukocytes. Although red blood cells and other immune cells such as macrophages are stained in the CL tissue, therefore in addition to positive cells by PAS staining, we checked the shape of nuclear of cells and assessed segmented granulocytes as PMNs. Thus, we could distinguish PMNs especially neutrophils from other PAS stained positive cells such as red blood cells and macrophages. This PAS stain was used on each tissue block, and 5 fields per section were examined at x 400 magnification. Quantification of the number of PMNs was performed independently by 3 observers. The results were expressed as means ± SEM per unit area.
RNA extraction and cDNA production
Total RNA was extracted from leukocytes following the protocol of Chomczynski and Sacchi with TRIzol reagent [50] as described in our previous study [51]. The extracted total RNA was stored in RNA storage solution (Ambion, Texas, USA) at –80°C until being used for cDNA production. RNA samples were then used to produce cDNA as described in our previous study [51]. The synthesized cDNA was stored at −30°C.
Quantitative real-time reverse transcription-polymerase chain reaction
Quantification of mRNA expression for IL-8, P-selectin, E-selectin, ICAM, FPr and β-actin was performed using synthesized cDNA via real-time PCR with a LightCycler (Roche Diagnostics Corp. Mannheim, Germany) with a commercial kit (QuantiTectTM SYBR Green PCR, QIAGEN GmbH, Hilden, Germany). The amplification program consisted of 15 min of activation at 95°C followed by 40 cycles of PCR steps (15 sec of denaturation at 94°C, 30 sec of annealing at 60°C, and 20 sec of extension at 72°C). For quantification of the target genes, a series of standards was constructed by amplifying a fragment of DNA (150–250 bp) that contains the target sequence for real-time PCR. The primers used for real-time PCR were as follows: 5′-cctcttgttcaatatgacttcca-3′, forward, and 5′- ggcccactctcaataactctc-3′, reverse for IL-8 (Accession No. NM_173925); 5′-gccacctaggaacatacggagtt-3′, forward, and 5′-gattggacgaggtcaccaaga-3′, reverse for P-selectin (Accession No. NM_174183.2); 5′- actcccttggcagttggactt-3′, forward, and 5′-aggcgtttcagaagccagaa-3′, reverse for E-selectin (Accession No. NM_174181); 5′-ctctgtccatgggattctgaca-3′, forward, and 5′-gtttcatgtgaccctgtggtgtag-3′, reverse for ICAM (Accession No. NM_174348); 5′-ttggatggtgtttgcagtttct-3′, forward, and 5′-agtcagtgaaacagagtcaccaatct-3′, reverse for VCAM (Accession No. NM_001101158.1); 5′-tcagccctcacccagataagt-3′, forward, and 5′-ggccatttcactgttcagg-3′, reverse for FPr (Accession No. NM_181025.2); and 5′-ccaaggccaaccgtgagaaaat-3′, forward,and5′-ccacattccgtgaggatcttca-3′, reverse forβ-actin (Accession No. NM_173979.3). The values were normalized using β-actin as the internal standard.
Western blotting
Detection of FPr in PMNs, PBMCs, and the mid CL were analyzed as described in our previous study [28]. We used polyclonal antibodies for FPr (64 kDa, Cayman Chemical, Michigan, USA. 1∶1000 dilution) an anti-β-actin antibody (42 kDa, SIGMA, 1∶5000 dilution), and horseradish peroxidase (HRP)-conjugated anti-rabbit (GE Healthcare, 1∶5000 dilution) and anti-mouse IgG antibodies (Rockland Immunochemicals, Inc. USA, 1∶10000 dilution). The signals were detected using an ECL Western Blotting Detection System (GE Healthcare UK Ltd., Little Chalfont, UK). The optical density of the immunospecific bands was quantified by means of an imageJ computer-assisted analysis system.
Statistical analysis
All data are presented as means ± SEM. The statistical significance of differences was assessed by one-way ANOVA followed by Bonferroni's multiple comparison test or Student's t-test. Probabilities less than 5% (P<0.05) were considered significant.
Acknowledgments
The authors thank Professor Dr. K Okuda, Okayama University, Japan, for the P antiserum.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This study was supported in part by a grant from Global Centers of Excellence (GCOE) Program from Japanese Ministry of Education, Science, Sports, Culture and Technology and by the Grant-in-Aid for Scientific Research of the Japan Society for the Promotion of Science (JSPS), Japan. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Nett TM, McClellan MC, Niswender GD. Effects of prostaglandins on the ovine corpus luteum: blood flow, secretion of progesterone and morphology. Biol Reprod. 1976;15:66–78. doi: 10.1095/biolreprod15.1.66. [DOI] [PubMed] [Google Scholar]
- 2.McCracken JA, Schramm W, Barcikowski B, Wilson L., Jr The identification of prostaglandin F2α as a uterine luteolytic hormone and the hormonal control of its synthesis. Acta Vet. 1981;Scand(Suppl 77):71–88. [PubMed] [Google Scholar]
- 3.Penny LA, Armstrong D, Bramley TA, Webb R, Collins RA, et al. Immune cells and cytokine production in the bovine corpus luteum throughout the oestrous cycle and after induced luteolysis. J Reprod Fertil. 1999;115:87–96. doi: 10.1530/jrf.0.1150087. [DOI] [PubMed] [Google Scholar]
- 4.Pate JL, Landis Keyes P. Immune cells in the corpus luteum: friends or foes? Reproduction. 2001;122:665–676. doi: 10.1530/rep.0.1220665. [DOI] [PubMed] [Google Scholar]
- 5.Bauer M, Reibiger I, Spanel-Borowski K. Leucocyte proliferation in the bovine corpus luteum. Reproduction. 2001;121:297–305. [PubMed] [Google Scholar]
- 6.Murdoch WJ, Steadman LE, Belden EL. Immunoregulation of luteolysis. Med Hypotheses. 1988;27:197–199. doi: 10.1016/0306-9877(88)90141-7. [DOI] [PubMed] [Google Scholar]
- 7.Pate JL. Involvement of immune cells in regulation of ovarian function. J Reprod. 1995;Fertil(Suppl 49):365–377. [PubMed] [Google Scholar]
- 8.Brannstrom M, Friden B. Immune regulation of corpus luteum function. Semin Reprod Endocrinol. 1997;15:363–370. doi: 10.1055/s-2008-1068374. [DOI] [PubMed] [Google Scholar]
- 9.Townson DH, O'Connor CL, Pru JK. Expression of monocyte chemoattractant protein-1 and distribution of immune cell populations in the bovine corpus luteum throughout the estrous cycle. Biol Reprod. 2002;66:361–366. doi: 10.1095/biolreprod66.2.361. [DOI] [PubMed] [Google Scholar]
- 10.Okuda K, Sakumoto R. Multiple roles of TNF super family members in corpus luteum function. Reprod Biol Endocrinol. 2003;95:1–10. doi: 10.1186/1477-7827-1-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fairchild DL, Pate JL. Interferon-gamma induction of major histocompatibility complex antigens on cultured bovine luteal cells. Biol Reprod. 1989;40:453–457. doi: 10.1095/biolreprod40.3.453. [DOI] [PubMed] [Google Scholar]
- 12.Khoury EL, Marshall LA. Luteinization of human granulosa cells in vivo is associated with expression of MHC class II antigens. Cell Tissue Res. 1990;262:217–224. doi: 10.1007/BF00309876. [DOI] [PubMed] [Google Scholar]
- 13.Benyo DF, Haibel GK, Laufman HB, Pate JL. Expression of major histocompatibility complex antigens on the bovine corpus luteum during the estrous cycle, luteolysis, and early pregnancy. Biol Reprod. 1991;45:229–234. doi: 10.1095/biolreprod45.2.229. [DOI] [PubMed] [Google Scholar]
- 14.Sawyer HR, Niswender KD, Braden TD, Niswender GD. Nuclear changes in ovine luteal cells in response to PGF2α. Domest Anim Endocrinol. 1990;7:229–237. doi: 10.1016/0739-7240(90)90029-y. [DOI] [PubMed] [Google Scholar]
- 15.Juengel JL, Garverick HA, Johnson AL, Youngquist RS, Smith MF. Apoptosis during luteal regression in cattle. Endocrinology. 1993;132:249–254. doi: 10.1210/endo.132.1.8419126. [DOI] [PubMed] [Google Scholar]
- 16.Arici A, Oral E, Bukulmez O, Buradagunta S, Engin O, et al. Interleukin-8 expression and modulation in human preovulatory follicles and ovarian cells. Endocrinology. 1996;137:3762–3769. doi: 10.1210/endo.137.9.8756544. [DOI] [PubMed] [Google Scholar]
- 17.Brannstrom M, Bonello N, Norman RJ, Robertson SA. Reduction of ovulation rate in the rat by administration of a neutrophil-depleting monoclonal antibody. J Reprod Immunol. 1995;29:265–270. doi: 10.1016/0165-0378(95)00941-d. [DOI] [PubMed] [Google Scholar]
- 18.Al-Zi'abi MO, Fraser HM, Watson ED. Cell death during natural and induced luteal regression in mares. Reproduction. 2002;123:67–77. [PubMed] [Google Scholar]
- 19.Goto J, Suganuma N, Takata K, Kitamura K, Asahina T, et al. Morphological analyses of interleukin-8 effects on rat ovarian follicles at ovulation and luteinization in vivo. Cytokine. 2002;20:168–173. doi: 10.1006/cyto.2002.1987. [DOI] [PubMed] [Google Scholar]
- 20.Kumar V, Cortran RS, Robbins SL. Robbins Basic Pathology. SAUNDERS Philadelphia. 2002.
- 21.Paape MJ, Bannerman DD, Zhao X, Lee JW. The bovine neutrophil: Structure and function in blood and milk. Vet Res. 2003;34:597–627. doi: 10.1051/vetres:2003024. [DOI] [PubMed] [Google Scholar]
- 22.Sako D, Chang XJ, Barone KM, Vachino G, White HM, et al. Expression cloning of a functional glycoprotein ligand for P-selectin. Cell. 1993;75:1179–1186. doi: 10.1016/0092-8674(93)90327-m. [DOI] [PubMed] [Google Scholar]
- 23.Carlos TM, Harlan JM. Leukocyte-endothelial adhesion molecules. Blood. 1994;84:2068–2101. [PubMed] [Google Scholar]
- 24.Sugama Y, Tiruppathi C, offakidevi K, Andersen TT, Fenton JW, 2nd, et al. Thrombin-induced expression of endothelial P-selectin and intercellular adhesion molecule-1: a mechanism for stabilizing neutrophil adhesion. J Cell Biol. 1992;119:935–944. doi: 10.1083/jcb.119.4.935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaur J, Woodman RC, Ostrovsky L, Kubes P. Selective recruitment of neutrophils and lymphocytes by thrombin: a role for NF-kappaB. Am J Physiol Heart Circ Physiol. 2001;281:H784–795. doi: 10.1152/ajpheart.2001.281.2.H784. [DOI] [PubMed] [Google Scholar]
- 26.Maliba R, Brkovic A, Neagoe PE, Villeneuve LR, Sirois MG. Angiopoietin-mediated endothelial P-selectin translocation: cell signaling mechanisms. J Leukoc Biol. 2008;83:352–360. doi: 10.1189/jlb.0107056. [DOI] [PubMed] [Google Scholar]
- 27.Meidan R, Levy N, Kisliouk T, Podlovny L, Rusiansky M, et al. The yin and yang of corpus luteum-derived endothelial cells: balancing life and death. Domest Anim Endocrinol. 2005;29:318–328. doi: 10.1016/j.domaniend.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 28.Shirasuna K, Watanabe S, Asahi T, Wijagunawardane MPB, Sasahara K, et al. Prostaglandin F2α increases endothelial nitric oxide synthase in the periphery of the bovine corpus luteum: the possible regulation of blood flow at an early stage of luteolysis. Reproduction. 2008;135:527–539. doi: 10.1530/REP-07-0496. [DOI] [PubMed] [Google Scholar]
- 29.Liptak AR, Sullivan BT, Henkes LE, Wijayagunawardane MP, Miyamoto A, et al. Cooperative expression of monocyte chemoattractant protein 1 within the bovine corpus luteum: evidence of immune cell-endothelial cell interactions in a coculture system. Biol Reprod. 2005;72:1169–1176. doi: 10.1095/biolreprod.104.032953. [DOI] [PubMed] [Google Scholar]
- 30.Murayama C, Kaji A, Miyauchi K, Matsui M, Miyamoto A, et al. Effect of VEGF (vascular endothelial growth factor) on expression of IL-8 (interleukin-8), IL-1beta and their receptors in bovine theca cells. Cell Biol Int. 2010;34:531–536. doi: 10.1042/CBI20090498. [DOI] [PubMed] [Google Scholar]
- 31.Belayet HM, Kanayama N, Khatun S, Asahina T, Okada Y, et al. Pharmacologic doses of interleukin 8 suppositories induce follicular maturation in rabbits. Cytokine. 2000;12:361–367. doi: 10.1006/cyto.1999.0553. [DOI] [PubMed] [Google Scholar]
- 32.Runesson E, Ivarsson K, Janson PO, Brannstrom M. Gonadotropin- and cytokine-regulated expression of the chemokine interleukin 8 in the human preovulatory follicle of the menstrual cycle. J Clin Endocrinol Metab. 2000;85:4387–4395. doi: 10.1210/jcem.85.11.6954. [DOI] [PubMed] [Google Scholar]
- 33.Sales KJ, Maldonado-Perez D, Grant V, Catalano RD, Wilson MR, et al. Prostaglandin F2α-F-prostanoid receptor regulates CXCL8 expression in endometrial adenocarcinoma cells via the calcium-calcineurin-NFAT pathway. Biochim Biophys Acta. 2009;1793:1917–1928. doi: 10.1016/j.bbamcr.2009.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pepperell JR, Wolcott K, Behrman HR. Effects of neutrophils in rat luteal cells. Endocrinology. 1992;130:1001–1008. doi: 10.1210/endo.130.2.1310272. [DOI] [PubMed] [Google Scholar]
- 35.Minegishi K, Tanaka M, Nishimura O, Tanigaki S, Miyakoshi K, et al. Reactive oxygen species mediate leukocyte-endothelium interactions in prostaglandin F2α-induced luteolysis in rats. Am J Physiol Endocrinol Metab. 2002;283:E1308–1315. doi: 10.1152/ajpendo.00240.2002. [DOI] [PubMed] [Google Scholar]
- 36.Flint AP, Sheldrick EL. Ovarian secretion of oxytocin is stimulated by prostaglandin. Nature. 1982;297:587–588. doi: 10.1038/297587a0. [DOI] [PubMed] [Google Scholar]
- 37.de Menezes GB, dos Reis WG, Santos JM, Duarte ID, de Francischi JN. Inhibition of prostaglandin F2α by selective cyclooxygenase 2 inhibitors accounts for reduced rat leukocyte migration. Inflammation. 2005;29:163–169. doi: 10.1007/s10753-006-9013-z. [DOI] [PubMed] [Google Scholar]
- 38.Schruefer R, Lutze N, Schymeinsky J, Walzog B. Human neutrophils promote angiogenesis by a paracrine feedforward mechanism involving endothelial interleukin-8. Am J Physiol Heart Circ Physiol. 2005;288:H1186–1192. doi: 10.1152/ajpheart.00237.2004. [DOI] [PubMed] [Google Scholar]
- 39.Diez-Fraile A, Meyer E, Duchateau L, Paape MJ, Burvenich C. In vitro regulation of Mac-1 expression on bovine polymorphonuclear leukocytes by endotoxin and tumor necrosis factor-alpha at different stages of lactation. Can J Vet Res. 2004;68:232–235. [PMC free article] [PubMed] [Google Scholar]
- 40.Sohn EJ, Paape MJ, Connor EE, Bannerman DD, Fetterer RH, et al. Bacterial lipopolysaccharide stimulates bovine neutrophil production of TNF-alpha, IL-1beta, IL-12 and IFN-gamma. Vet Res. 2007;38:809–818. doi: 10.1051/vetres:2007033. [DOI] [PubMed] [Google Scholar]
- 41.Bowen JM, Towns R, Warren JS, Landis Keyes P. Luteal regression in the normally cycling rat: apoptosis, monocyte chemoattractant protein-1, and inflammatory cell involvement. Biol Reprod. 1999;60:740–746. doi: 10.1095/biolreprod60.3.740. [DOI] [PubMed] [Google Scholar]
- 42.Hojo T, Oda A, Lee SH, Acosta TJ, Okuda K. Effects of tumor necrosis factor alpha and Interferon gamma on the viability and mRNA expression of TNF receptor type I in endothelial cells from the bovine corpus luteum. J Reprod Dev. 2010;56:515–519. doi: 10.1262/jrd.10-056t. [DOI] [PubMed] [Google Scholar]
- 43.Sugino N, Okuda K. Species-related differences in the mechanism of apoptosis during structural luteolysis. J Reprod Dev. 2007;53:977–986. doi: 10.1262/jrd.19047. [DOI] [PubMed] [Google Scholar]
- 44.Shirasuna K, Sasahara K, Matsui M, Shimizu T, Miyamoto A. Prostaglandin F2α differentially affects mRNA expression relating to angiogenesis, vasoactivation and prostaglandins in the early and mid corpus luteum in the cow. J Reprod Dev. 2010;56:428–436. doi: 10.1262/jrd.10-004o. [DOI] [PubMed] [Google Scholar]
- 45.Miyamoto A, Okuda K, Schweigert FJ, Schams D. Effects of basic fibroblast growth factor, transforming growth factor-beta and nerve growth factor on the secretory function of the bovine corpus luteum in vitro. J Endocrinol. 1992;135:103–114. doi: 10.1677/joe.0.1350103. [DOI] [PubMed] [Google Scholar]
- 46.Klipper E, Gilboa T, Levy N, Kisliouk T, Spanel-Borowski K, et al. Characterization of endothelin-1 and nitric oxide generating systems in corpus luteum-derived endothelial cells. Reproduction. 2004;128:463–473. doi: 10.1530/rep.1.00271. [DOI] [PubMed] [Google Scholar]
- 47.Spanel-Borowski K. Diversity of ultrastructure in different phenotypes of cultured microvessel endothelial cells isolated from bovine corpus luteum. Cell Tissue Res. 1991;266:37–49. doi: 10.1007/BF00678709. [DOI] [PubMed] [Google Scholar]
- 48.Jiemtaweeboon S, Shirasuna K, Nitta A, Kobayashi A, Schuberth HJ, et al. Evidence that polymorphonuclear neutrophils infiltrate into the developing corpus luteum and promote angiogenesis with interleukin-8 in the cow. Reprod Biol Endocrinol. 2011;9 doi: 10.1186/1477-7827-9-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yasuda M, Shimizu S, Tokuyama S, Watanabe T, Kiuchi Y, et al. A novel effect of polymorphonuclear leukocytes in the facilitation of angiogenesis. Life Sci. 2000;66:2113–2121. doi: 10.1016/s0024-3205(00)00537-3. [DOI] [PubMed] [Google Scholar]
- 50.Chomczynski P, Sacchi N. Single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction. Anal Biochem. 1987;162:156–159. doi: 10.1006/abio.1987.9999. [DOI] [PubMed] [Google Scholar]
- 51.Watanabe S, Shirasuna K, Matsui M, Yamamoto D, Berisha B, et al. Effect of intraluteal injection of endothelin type A receptor antagonist on PGF2α-induced luteolysis in the cow. J Reprod Dev. 2006;52:551–559. doi: 10.1262/jrd.18018. [DOI] [PubMed] [Google Scholar]