Abstract
BACKGROUND
Provider and patient reminders can be effective in increasing rates of preventive screenings and vaccinations. However, the effect of patient-directed electronic reminders is understudied.
OBJECTIVE
To determine whether providing reminders directly to patients via an electronic Personal Health Record (PHR) improved adherence to care recommendations.
DESIGN
We conducted a cluster randomized trial without blinding from 2005 to 2007 at 11 primary care practices in the Partners HealthCare system.
PARTICIPANTS
A total of 21,533 patients with access to a PHR were invited to the study, and 3,979 (18.5%) consented to enroll.
INTERVENTIONS
Patients in the intervention arm received health maintenance (HM) reminders via a secure PHR “eJournal,” which allowed them to review and update HM and family history information. Patients in the active control arm received access to an eJournal that allowed them to input and review information related to medications, allergies and diabetes management.
MAIN MEASURES
The primary outcome measure was adherence to guideline-based care recommendations.
KEY RESULTS
Intention-to-treat analysis showed that patients in the intervention arm were significantly more likely to receive mammography (48.6% vs 29.5%, p = 0.006) and influenza vaccinations (22.0% vs 14.0%, p = 0.018). No significant improvement was observed in rates of other screenings. Although Pap smear completion rates were higher in the intervention arm (41.0% vs 10.4%, p < 0.001), this finding was no longer significant after excluding women’s health clinics. Additional on-treatment analysis showed significant increases in mammography (p = 0.019) and influenza vaccination (p = 0.015) for intervention arm patients who opened an eJournal compared to control arm patients, but no differences for any measure among patients who did not open an eJournal.
CONCLUSIONS
Providing patients with HM reminders via a PHR may be effective in improving some elements of preventive care.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-011-1859-6) contains supplementary material, which is available to authorized users.
KEY WORDS: health maintenance reminders, personal health record, preventive care, clinical decision support, Patient Gateway
Introduction
Adults in the United States receive only about half of recommended evidence-based care, including health maintenance (HM) care such as immunizations and cancer screening1. These deficiencies represent missed opportunities to provide preventive care and, in some instances, to decrease health care costs. Compounding these quality challenges, primary care physicians (PCPs) often have insufficient time to address preventive care recommendations2 and are generally paid on the volume of services provided, rather than the quality of care delivered3.
Responsibility for the management of HM care falls generally to a patient’s PCP. Clinical decision support (CDS) tools, in the form of electronic alerts or reminders provided to physicians, have demonstrated modest but limited improvements in adherence to care guidelines4–7. Given the substantial challenges that busy physicians face, provider-oriented alerts and reminders may continue to be insufficient tools for the improvement of HM care.
Encouraging patients to become more active participants in their health management has the potential to improve the quality of care and has been called for as a potentially valuable addition to requirements for EHR incentive payments (also known as “meaningful use” rules) under the HITECH Act8, although evidence to support the benefit of this practice has been lacking. Non-electronic reminders provided directly to patients have been shown to improve adherence to care guidelines9–12. The use of a secure, interactive personal health record (PHR) tethered to an EHR can provide an avenue for patients to review and update health information13, and has the potential to improve adherence to guidelines.
To determine the effect of HM reminders provided electronically via a secure PHR, we carried out a multi-practice cluster-randomized controlled trial using Patient Gateway (PG), a secure patient portal developed at Partners HealthCare in Boston, Massachusetts. The primary goal of this intervention was to improve adherence to HM guidelines by (1) engaging patients in HM care, (2) promoting patient-doctor communication and (3) providing CDS to patients.
Methods
Setting and Participants
Participating practices (n = 11) were primary care practices at Partners HealthCare, an integrated academic care network in Boston, MA. Participating practices were diverse, and included a mix of hospital and community-based practices, federally qualified health centers and women’s health practices. The practices were located in both urban and suburban settings, and served patients across a wide range of the socioeconomic spectrum. Each practice used the Longitudinal Medical Record (LMR), a internally developed, certified electronic health record (EHR)14, and made Patient Gateway (PG) available to patients.
PG is a secure online patient portal that allows patients limited access to their EHR, and gives them the ability to request appointments and referrals, securely communicate with their physician, request prescription renewals and access a health information library. PG is connected directly to the patient’s LMR record. Like many EHR systems, the LMR provides a variety of patient-specific HM reminders to physicians.
To participate in this study, patients had to have an active PG account and a PCP assigned in the LMR. Prior to the start of the study, we employed a variety of strategies to increase patient use of PG, including: postcard mailings, posters hung in waiting and exam rooms, and voicemail recordings on practice phone lines. We also employed strategies to increase physician engagement with PG, including (1) demonstrating study modules at practice meetings, (2) providing materials to practices and (3) identifying providers at each practice who could facilitate enrollment. Once the study commenced, eligible patients were invited to participate via a secure PG message (signed by principal investigators BM and JW) that included a link to a consent form.
Intervention
As part of the “Prepare for Care” study, the pre-visit electronic journal (eJournal), a new feature of the PG, was developed15. An eJournal is an interactive electronic communication and information-sharing tool. Patients in the intervention arm were invited to complete eJournals that let them review and modify family history and that provided views of several HM reminders. These reminders were displayed when the HM item was indicated and used the same logic as the LMR’s physician reminders, but with a display tailored for patients, explaining each item and asking questions like ‘How would you like to take care of this?’
Patients in the active control arm were invited to complete eJournals that allowed them to review and modify medication and allergy lists (with prompts like ‘Are you currently taking this medication?’) and diabetes management information (displaying recent tests results and asking questions such as ‘How satisfied are you with your blood sugar control’?).
eJournal invitations and reminders were identical across study arms. Both modules asked patients to review information from their medical record and to answer questions relevant to an upcoming visit. The primary difference between the arms was the content of the modules patients reviewed after opening an eJournal. All patients could view their PHRs via PG; however, there was no overlapping content between the eJournals associated with each arm. Details of the design and outcomes for the active control arm are described elsewhere16–20.
Practices were randomly allocated to either of two arms (after matching for practice setting, general medicine vs women’s health and number of enrolled patients), and patients received the intervention associated with their practice’s arm. Patients were not aware which arm their practice was assigned to until after the consent process. Randomization was carried out by the study statistician who had no further role in the project. Blinding was not possible due to the nature of this intervention.
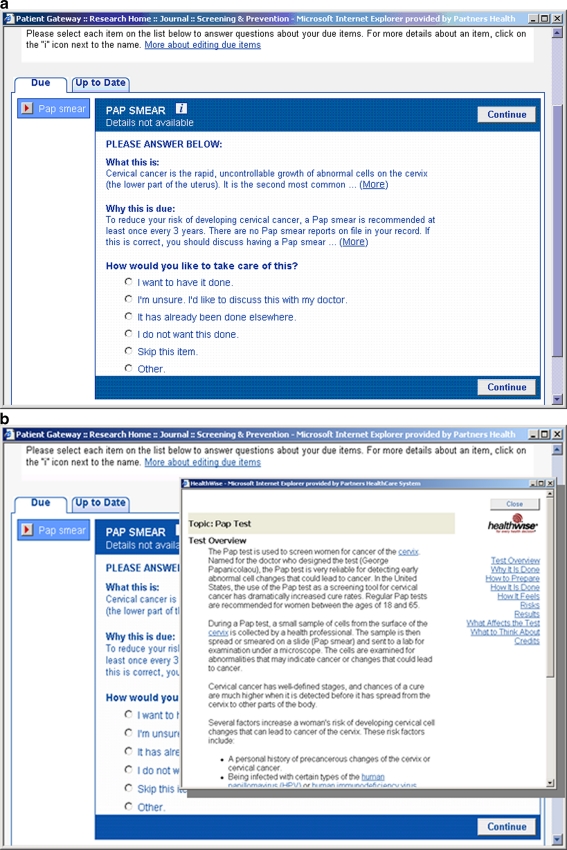
Patients in the intervention arm could receive any of six types of HM reminders as indicated: bone density testing, cholesterol testing, influenza vaccination, mammography, Pap smear and pneumococcal vaccination. HM procedures were identified as either ‘due’ or ‘up-to date,’ with prompts asking the patient how they would like to handle due items (e.g., ‘I want to have it done,’ ‘I’m unsure,’ or ‘It has already been done elsewhere’) (Fig. 1a). Patients were given a short explanation of the test and why it was being recommended (Fig. 1b). Information was transmitted to the LMR, through which the patient’s PCP could review eJournals and order screenings. Specific eligibility criteria for HM reminders are included in Appendix, which is available online. Invitations to complete eJournals were triggered by an upcoming appointment (3 weeks in advance to allow time for completion).
Figure 1.
(a) A patient health maintenance reminder for an overdue Pap smear. (b) Patient-friendly information about the Pap smear.
Objectives & Outcomes
The primary outcomes of this study were the performance rates for the HM care items in the two study arms. Patients receiving reminders in the intervention arm were compared to patients in the active control arm who were also due for the same item. Physicians received the usual reminders in the LMR regardless of arm. The HM item was considered satisfied if performance of the corresponding service was documented in the LMR within 60 days following the reminder. Patients could receive multiple HM reminders within a single eJournal; however, since we only analyzed the first eJournal a patient received, they could not receive more than one reminder for any specific HM task.
We compared the proportion of patients eligible for a given HM item in the intervention arm to the same proportion in the active control arm without regard to whether the patient viewed or completed the eJournal or whether their PCP opened the eJournal (intention-to-treat analysis). In addition, we compared patients in the intervention arm who had opened an eJournal to patients in the active control arm who opened an eJournal, which would have been on a different topic (an on-treatment analysis), and also compared non-openers across the arms. Finally, to assess the characteristics of online PHR adopters, we also compared participants and non-participants across demographic and clinical variables.
Statistical Methods
Analysis was carried out using t-tests (for continuous variables) and chi-square tests (for discrete variables). Rates of preventive care were compared using chi-square tests. Logistic regression was also performed to control for differences in patient characteristics between study arms. The primary analysis in our study was intention-to-treat; however, we also performed on-treatment analysis to compare the HM performance for across the two arms for patients who opened their eJournal, as well as a cross-arm comparison of patients who did not open their journal.
Results
Participant Flow
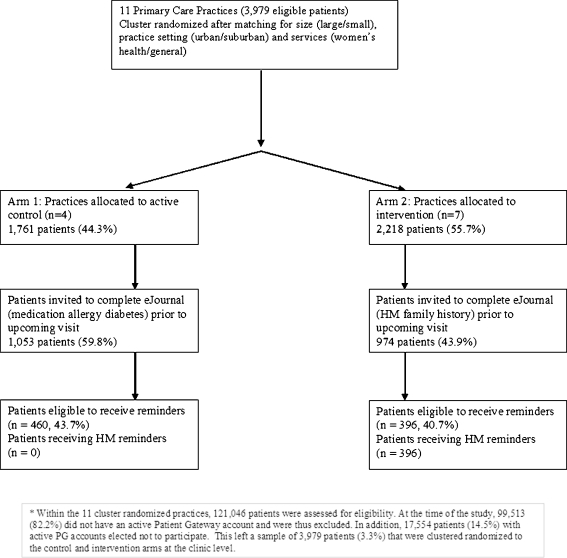
Of 121,046 active patients, 21,533 had a PG account and were invited to participate. A total of 3,979 patients consented and enrolled; the other 17,554 either did not respond or declined to participate. A total of 2,218 were in practices randomized to the intervention arm, and 1,761 were in practices randomized to the control arm; 974 patients in the intervention arm clinics had a visit and, thus, received an invitation to access an eJournal. Of these patients, 396 received one or more reminders. In the active control arm practices, 1,053 received invitations to access an eJournal. Of these patients, 460 were eligible to receive one or more reminders but were not shown HM reminders. Figure 2 shows the flow of practices and patients through the study. Practices were enrolled beginning September 30, 2005, and the study was closed March 22, 2007. For reminder-eligible patients who had appointments late in the study period, assessment of HM completion concluded 60 days after the end date.
Figure 2.
Flow diagram of a multi-clinic trial comparing a Health Maintenance/Family History personal health record (intervention) to an active control arm receiving access to a Medications/Allergies/Diabetes personal health record. To be eligible for the personal health record study, patients had to have an active Patient Gateway (PG) secure Internet access account with the health network.
Baseline Data
The mean age of participants was 48.9 (SD = 12.9), and 60.2% were female. Participants were older (48.9 versus 46.7 years; p < 0.0001), lived in higher income neighborhoods (median: $54,617 versus $52,012; p < 0.0001), and a greater proportion were white (87.1% versus 69.8%; p < 0.0001), male (39.8% versus 35.3%; p < 0.0001) and privately insured (84.7% versus 74.7%; p < 0.0001) compared with non-participants (n = 117,067). Participants also visited doctors other than their PCP more frequently than non-participants (4.2 versus 3.0 visits; p < 0.0001) during a 12-month baseline evaluation period.
Compared to the intervention group, the active control arm group was older (51.2 versus 47.0; p < 0.0001), had higher median neighborhood incomes ($55,385 versus $54,024; p < 0.0001), had a lower proportion of women (54.8% versus 64.5%; p < 0.0001) and had less private insurance (80.7% versus 87.8%; p < 0.0001) (Table 1).
Table 1.
Comparison of Study Participants in the Active Control and Intervention Arms
| Study participants (n = 3,979) | |||
|---|---|---|---|
| Characteristics | Active control arm | Intervention Arm | P-value |
| Patients, n | 1,760 | 2,219 | |
| Mean age (SD) | 51.2 (12.8) | 47.0 (12.7) | <0.0001 |
| Women (%) | 965 (54.8) | 1,432 (64.5) | <0.0001 |
| Mean median neighborhood income (SD) | 55,385 (9,748) | 54,024 (10,406) | <0.0001 |
| Race | 0.099 | ||
| Black (%) | 37 (2.1) | 69 (3.1) | |
| Hispanic (%) | 17 (1.0) | 33 (1.5) | |
| White (%) | 1543 (87.7) | 1923 (86.6) | |
| Other (%) | 163 (9.3) | 194 (8.7) | |
| Insurance | <0.0001 | ||
| Private (%) | 1421 (80.7) | 1948 (87.8) | |
| Medicare (%) | 321 (18.2) | 241 (10.9) | |
| Medicaid/free care (%) | 3 (0.2) | 11 (0.5) | |
| Self-pay/none (%) | 14 (0.8) | 17 (0.8) | |
| Unknown (%) | 1 (0.1) | 2 (0.1) | |
Of the 974 patients in the intervention arm, 396 received at least one reminder in their eJournal, and a total of 546 reminders were provided (1.38 reminders/patient). Of the patients in the active control arm who received journals, 460 of 1,053 patients were eligible to receive a total of 640 HM reminders in their first eJournal (1.39 reminders/patient), but were not shown these reminders.
There were 272 total physicians at participating practices (average age: 41 years, 68% female). Overall, 222 had patients with active PG accounts, 167 had patients who participated in the study, 89 had one or more patients invited to complete an eJournal in either of the two study arms, and 80 opened and reviewed one or more eJournals. Additional information on providers is presented in a separate publication15.
Outcomes
Patients in the intervention arm who received HM reminders were more likely to receive influenza vaccines (22.0% vs 14.%%, p = 0.018), mammography (48.6% vs 29.5%, p = 0.006) and Pap smears (41.0% vs 10.4%, p < 0.001) (Table 2). In addition, we employed logistic regression to control for differences in study arm populations. The results of these multivariate analyses were consistent with the unadjusted results, with the same HM items showing statistically significant improvements (Table 2).
Table 2.
Differences in Preventive Procedure Rates Between Study Arms (Intention-to-treat Analysis)
| Active control arm | Intervention arm | All clinics (n = 11) | Excluding women’s health clinics (n = 9) | ||||
|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | Adjusted | |||||
| Completed/not completed (prop†) | Completed/not completed (prop†) | p | Odds ratio | p | Odds ratio | p | |
| Bone density | 3/29 (9.4%) | 2/22 (8.3%) | 0.892 | 1.86 | 0.600 | 5.67 | 0.286 |
| Cholesterol | 14/34 (29.2%) | 20/23 (46.5%) | 0.088 | 2.25 | 0.113 | 1.20 | 0.776 |
| Influenza vaccine | 40/245 (14.0%) | 50/177 (22.0%) | 0.018* | 1.83 | 0.016* | 1.87 | 0.023* |
| Mammogram | 28/67 (29.5%) | 51/54 (48.6%) | 0.006* | 2.45 | 0.006* | 2.84 | 0.010* |
| Pap smear | 7/60 (10.4%) | 25/36 (41.0%) | <0.001* | 5.18 | 0.001* | 1.74 | 0.342 |
| Pneumovax | 10/103 (8.8%) | 11/75 (12.8%) | 0.370 | 1.47 | 0.454 | 1.25 | 0.698 |
*p < 0.05
†proportion
Because the significant associations observed were concentrated among screening procedures specific to women, we carried out additional analysis to assess the potential for confounding by receiving care in a women’s health center. Practices were randomized on the basis of services offered (one women’s health clinic to each arm); however, the population size of study-enrolled patients at each practice differed substantially (122 in the control arm vs 586 patients in the intervention arm).
To control for this effect, we repeated the regression analysis, excluding women’s health clinics. Under this analysis, there were still significant increases in influenza vaccination (adjusted OR = 1.87, p = 0.023) and mammography (adjusted OR = 2.84, p = 0.010). However, there was no longer a significant improvement in Pap smear completion (adjusted OR = 1.74, p = 0.342) (Table 2).
In order to further validate the results, we performed an on-treatment analysis to test whether the differences observed were associated with having viewed an eJournal. Complete results of the on-treatment analysis are shown in Table 3. For patients who opened an eJournal, we found that differences in mammography and influenza vaccination persisted (p = 0.019 and p = 0.015, respectively); however, for patients who did not open an eJournal, there were no significant differences observed across any of the six HM items.
Table 3.
Differences in Preventive Procedure Rates Between Study Arms—Opened vs. Unopened eJournals (on-treatment analysis)
| Opened eJournal | Unopened eJournal | All clinics (n = 11) | Excluding women’s health clinics (n = 9) | |||||
|---|---|---|---|---|---|---|---|---|
| Control | Intervention | Control | Intervention | Opened | Unopened | Opened | Unopened | |
| Completed/not completed (prop†) | Completed/not completed (prop†) | Completed/not completed (prop†) | Completed/not completed (prop†) | Odds ratio | Odds ratio | Odds ratio | Odds ratio | |
| Bone density | 1/22 (4.3%) | 2/17 (10.5%) | 2/7 (22.2%) | 0/5 (0.0%) | 3.88 | N/A‡ | 14.59 | N/A‡ |
| Cholesterol | 11/24 (31.4%) | 16/16 (50.0%) | 3/10 (23.1%) | 4/7 (36.4%) | 2.60 | 2.38 | 0.51 | 1.79 |
| Influenza vaccine | 32/178 (15.2%)* | 46/138 (25.0%)* | 8/67 (10.7%) | 4/39 (9.3%) | 1.88* | 1.49 | 1.91* | 1.59 |
| Mammogram | 23/47 (32.9%)* | 41/38 (51.9%)* | 5/20 (20.0%) | 10/16 (38.5%) | 2.38* | 2.17 | 3.33* | 1.21 |
| Pap smear | 6/46 (11.5%)* | 21/28 (42.9%)* | 1/14 (6.7%) | 4/8 (33.3%) | 4.97* | 5.74 | 1.72 | N/A‡ |
| Pneumovax | 7/75 (8.5%) | 9/58 (13.4%) | 3/28 (9.7%) | 2/17 (10.5%) | 2.18 | 0.85 | 1.84 | 0.54 |
*p < 0.05
†Proportion
‡Insufficient sample size to calculate odds ratio
Discussion
We found that HM reminders, when provided directly to patients via a secure EHR-connected PHR, improved the rates of some preventive screenings and vaccinations, but not others. These results were robust under a variety of analytical approaches, including logistic regression to control for potential confounding and on-treatment analysis to measure the specificity of the apparent effect.
Although not all reminders resulted in a significant improvement, increases in the rates of influenza vaccination and mammography in the intervention arm indicate that patient reminders could be a useful tool for improving adherence to preventive care guidelines. Such tools could potentially enhance patient self-efficacy—a patient’s individual perception of how their actions and choices impact their care and health outcomes. Increased patient self-efficacy has been associated with better self-care and health management21–23.
As part of the LMR, providers receive reminders to indicate when a patient is due for a HM procedure. However, even in places where these reminders are available, not all providers use them24. One potential reason may be that providers can suffer from “alert fatigue,” frustration with an abundance of alerts, which can make them more likely to ignore recommendations25. Patient-oriented reminders are a tool that could potentially mitigate “alert fatigue” by engaging patients directly. By offering patients the opportunity to become more involved in their care, it may be possible to increase self-efficacy and improve adherence to care guidelines. However, it is important to note that patients may too be susceptible to “alert fatigue” and focusing heavily in one area (e.g., health maintenance) may lead them to neglect another area (e.g., diabetes management).
With further improvements in PHR technology and utilization, it may eventually be possible to relieve PCPs of some of the burden of completing their patients’ basic HM care, although this must remain a partnership, and some guidance from the PCP will always be needed. A robust patient-oriented HM reminder system could allow patients to review needed preventive care and schedule basic screenings themselves, improving not only patient adherence, but potentially their physician’s performance metrics as well. Given the well-defined risk groups for certain HM procedures, it may prove more efficient to streamline completion of these procedures using actionable patient-oriented reminders.
Limitations
Our approach has several potential limitations. First, our study was limited by the relatively low penetration of our PHR. At the time of the study, only 21,533 of eligible patients were enrolled in PG. Given the significant differences between PHR users and non-PHR users, the low penetration in our sample and the passive nature of the intervention, it is uncertain whether this intervention, in its current form, could affect HM screening rates in a significant and cost-effective manner. However, given our findings of improved rates of certain screenings, it may be possible to generate greater improvement by expanding PHR enrollment, addressing access issues and designing a more directly actionable intervention. Since the time of the study, the total PG enrollment has increased significantly, recently surpassing 100,000. As usage of PHRs increases, the reach and effect of interventions such as ours may likewise expand.
As PHR usage grows, special care will need to be paid to potential issues of the “digital divide.” Our demographic information suggests that participants were from higher income areas and more likely to be white than non-participants. Other studies have reported similar disparities in access to and use of PHRs26–28. Unless these disparities can be corrected, there is a risk that overreliance on PHR-delivered reminders might contribute to health disparities.
Related to penetration of PHRs is a second limitation of our study: the small number of patients due for some of the reminders limited the statistical power to assess the intervention. The study was designed to have 90% power to detect differences of 5–7% in endpoints across the arms; however, given the low incidence of certain reminders, the study may a be underpowered to detect differences between the arms. It is possible that a larger study population, longer window of observation or wider PHR adoption within the study population would have provided power to uncover other significant differences across HM reminder categories.
An additional limitation of our study design is that the intervention was tested within a single health-care network using one type of “home-grown” PHR. It is possible that a similar intervention may be more or less effective using another system. Broader investigation of these types of interventions is needed.
Finally, due to the use of cluster randomization in this study, there were small but significant differences between study arms. Although these differences were statistically significant due to the large sample size, the magnitudes of the differences were small, and we believe they are unlikely to have affected our findings. In addition, minimal data were available on the potential difference between physicians and practice environments across the arms. However, the study was cluster randomized by clinic (with matching for practice setting, general vs women’s health and number of patients enrolled) and included all PCP clinics in the Partners HealthCare system; thus, we believe that there should be baseline similarity between the provider participants in both arms. Further, the previously described supplemental on-treatment analysis suggests that the observed effect is likely an intervention-specific effect rather than simply attributable to baseline differences.
Conclusion
Providing patients with HM reminders may be effective in improving care for certain conditions. We found that eligible patients who received HM reminders via an EHR-connected PHR were more likely to receive mammography and influenza vaccinations. More research is needed to evaluate and improve upon the efficacy of this intervention and to engage more patients in the use of PHRs in general.
Electronic supplementary material
(DOC 44 kb)
Acknowledgements
This work was partially supported by AHRQ Grant R01-HS013660-02: Shared Online Health Records for Patient Safety and Quality. AHRQ was not involved in the design, execution or analysis of the study, or in the preparation of this manuscript. The study protocol was approved by the Partners HealthCare Human Research Committee and registered at ClinicalTrials.gov (NCT00251875).
Conflicts of Interest None disclosed.
References
- 1.McGlynn EA, Asch SM, Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 2.Yarnall KS, Pollak KI, Ostbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention? Am J Public Health. 2003;93(4):635–641. doi: 10.2105/AJPH.93.4.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.IOM. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001. [PubMed]
- 4.Shea S, DuMouchel W, Bahamonde L. A meta-analysis of 16 randomized controlled trials to evaluate computer-based clinical reminder systems for preventive care in the ambulatory setting. J Am Med Inform Assoc. 1996;3(6):399–409. doi: 10.1136/jamia.1996.97084513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tierney WM, Overhage JM, Murray MD, et al. Effects of computerized guidelines for managing heart disease in primary care. J Gen Intern Med. 2003;18(12):967–976. doi: 10.1111/j.1525-1497.2003.30635.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sequist TD, Gandhi TK, Karson AS, et al. A randomized trial of electronic clinical reminders to improve quality of care for diabetes and coronary artery disease. J Am Med Inform Assoc. 2005;12(4):431–437. doi: 10.1197/jamia.M1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shojania KG, Jennings A, Mayhew A, Ramsay CR, Eccles MP, Grimshaw J. The effects of on-screen, point of care computer reminders on processes and outcomes of care. Cochrane Database Syst Rev. 2009(3):CD001096. [DOI] [PMC free article] [PubMed]
- 8.Blumenthal D, Tavenner M. The Meaningful Use Regulation for Electronic Health Records. N Engl J Med. 2010;363(6):501–4. [DOI] [PubMed]
- 9.Taplin SH, Anderman C, Grothaus L, Curry S, Montano D. Using physician correspondence and postcard reminders to promote mammography use. Am J Public Health. 1994;84(4):571–574. doi: 10.2105/AJPH.84.4.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.King ES, Rimer BK, Seay J, Balshem A, Engstrom PF. Promoting mammography use through progressive interventions: is it effective? Am J Public Health. 1994;84(1):104–106. doi: 10.2105/AJPH.84.1.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thomas RE, Russell M, Lorenzetti D. Interventions to increase influenza vaccination rates of those 60 years and older in the community. Cochrane Database Syst Rev. 2010(9):CD005188. [DOI] [PubMed]
- 12.Szilagyi PG, Bordley C, Vann JC, et al. Effect of patient reminder/recall interventions on immunization rates: A review. Jama. 2000;284(14):1820–1827. doi: 10.1001/jama.284.14.1820. [DOI] [PubMed] [Google Scholar]
- 13.Tang PC, Ash JS, Bates DW, Overhage JM, Sands DZ. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc. 2006;13(2):121–126. doi: 10.1197/jamia.M2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Poon EG, Wald J, Bates DW, Middleton B, Kuperman GJ, Gandhi TK. Supporting patient care beyond the clinical encounter: three informatics innovations from partners health care. AMIA Annu Symp Proc. 2003:1072. [PMC free article] [PubMed]
- 15.Wald J, Businger A, Gandhi T, et al. Implementing practice-linked pre-visit electronic journals in primary care: patient and physician use and satisfaction. J Am Med Inform Assoc. 2010. [DOI] [PMC free article] [PubMed]
- 16.Grant RW, Wald JS, Poon EG, et al. Design and implementation of a web-based patient portal linked to an ambulatory care electronic health record: patient gateway for diabetes collaborative care. Diabetes Technol Ther. 2006;8(5):576–586. doi: 10.1089/dia.2006.8.576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grant RW, Wald JS, Schnipper JL, et al. Practice-linked online personal health records for type 2 diabetes mellitus: a randomized controlled trial. Arch Intern Med. 2008;168(16):1776–1782. doi: 10.1001/archinte.168.16.1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schnipper JL, Gandhi TK, Wald JS, et al. Design and implementation of a web-based patient portal linked to an electronic health record designed to improve medication safety: the Patient Gateway medications module. Inform Prim Care. 2008;16(2):147–155. doi: 10.14236/jhi.v16i2.686. [DOI] [PubMed] [Google Scholar]
- 19.Siteman E, Businger A, Gandhi T, et al. Physicians value patient review of their electronic health record data as a means to improve accuracy of medication list documentation. AMIA Annu Symp Proc. 2007:1116. [PubMed]
- 20.Wald JS, Grant RW, Schnipper JL, et al. Survey analysis of patient experience using a practice-linked PHR for type 2 diabetes mellitus. AMIA Annu Symp Proc. 2009;2009:678–682. [PMC free article] [PubMed] [Google Scholar]
- 21.Aljasem LI, Peyrot M, Wissow L, Rubin RR. The impact of barriers and self-efficacy on self-care behaviors in type 2 diabetes. Diabetes Educ. 2001;27(3):393–404. doi: 10.1177/014572170102700309. [DOI] [PubMed] [Google Scholar]
- 22.Marks R, Allegrante JP, Lorig K. A review and synthesis of research evidence for self-efficacy-enhancing interventions for reducing chronic disability: implications for health education practice (part II) Health Promot Pract. 2005;6(2):148–156. doi: 10.1177/1524839904266792. [DOI] [PubMed] [Google Scholar]
- 23.Holloway A, Watson HE. Role of self-efficacy and behaviour change. Int J Nurs Pract. 2002;8(2):106–115. doi: 10.1046/j.1440-172x.2002.00352.x. [DOI] [PubMed] [Google Scholar]
- 24.Simon SR, Kaushal R, Cleary PD, et al. Correlates of electronic health record adoption in office practices: a statewide survey. J Am Med Inform Assoc. 2007;14(1):110–117. doi: 10.1197/jamia.M2187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ash JS, Sittig DF, Campbell EM, Guappone KP, Dykstra RH. Some unintended consequences of clinical decision support systems. AMIA Annu Symp Proc. 2007:26–30. [PMC free article] [PubMed]
- 26.Roblin DW, Houston TK, 2nd, Allison JJ, Joski PJ, Becker ER. Disparities in use of a personal health record in a managed care organization. J Am Med Inform Assoc. 2009;16(5):683–689. doi: 10.1197/jamia.M3169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim EH, Kim Y. Digital divide: Use of electronic personal health record by different population groups. Conf Proc IEEE Eng Med Biol Soc. 2010;1:1759–1762. doi: 10.1109/IEMBS.2010.5626732. [DOI] [PubMed] [Google Scholar]
- 28.Kim EH, Stolyar A, Lober WB, et al. Challenges to using an electronic personal health record by a low-income elderly population. J Med Internet Res. 2009;11(4):e44. doi: 10.2196/jmir.1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC 44 kb)