ABSTRACT
PURPOSE
To compare two techniques for eliciting and clarifying patient values for decision making about colorectal cancer (CRC) screening: choice-based conjoint analysis and a rating and ranking task.
METHODS
Using our decision lab registry and university e-mail lists, we recruited average risk adults ages 48–75 for a written, mailed survey. Eligible participants were given basic information about CRC screening and six attributes of CRC screening tests, then randomized to complete either a choice-based conjoint analysis with 16 discrete choice tasks or a rating and ranking task. The main outcome was the most important attribute, as determined from conjoint analysis or participant ranking. Conjoint analysis-based most important attribute was determined from individual patient-level utilities generated using multinomial logistic regression and hierarchical Bayesian modeling.
RESULTS
Of the 114 eligible participants, 104 completed and returned questionnaires. Mean age was 57 (range 48–73), 70% were female, 88% were white, 71% were college graduates, and 62% were up to date with CRC screening. Ability to reduce CRC incidence and mortality was the most frequent most important attribute for both the conjoint analysis (56% of respondents) and rating/ranking (76% of respondents) groups, and these proportions differed significantly between groups (absolute difference 20%, 95% CI 3%, 37%, p =0.03). There were no significant differences between groups in proportion with clear values (p = 0.352), intent to be screened (p = 0.226) or unlabelled test preference (p = 0.521)
CONCLUSIONS
Choice-based conjoint analysis produced somewhat different patterns of attribute importance than a rating and ranking task, but had little effect on other outcomes.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-011-1837-z) contains supplementary material, which is available to authorized users.
KEY WORDS: colorectal cancer (CRC) screening, conjoint analysis, rating/ranking , preferences
BACKGROUND
Cancer screening decision can be complex, and decision aids have been developed to assist patients and providers in these decisions.1–4 Consensus recommendations for high-quality decision aid design include the need to elicit, clarify, and incorporate patient values and preferences5 but the best method for doing so is not clear.6,7 Potential options include implicit techniques, in which patients receive information about different aspects of the decision and are able to consider their potential value on their own (or with a prompt to “consider which factors are most important to you”), and explicit techniques (e.g. rating, ranking, discrete choice methods including conjoint analysis) in which patients are asked specifically to compare the relative importance of several potentially relevant characteristics of a decision. The decision about which technique to use should ideally be guided by information about efficacy and feasibility.
Conjoint analysis and discrete choice experiments (DCE) are stated preference techniques developed in the fields of economics, marketing, and psychology.8 They offer many potential advantages for values elicitation and clarification and have been employed widely in transportation and environmental decision-making but have only recently been used commonly in health. Conjoint analysis and DCE are based on the theory that decision options can be described by sets of attributes, each made up of different levels.8,9
The relative value that patients attach to the different attributes can be estimated by constructing a series of hypothetical options made up of these attributes at different levels and asking patients to rate, rank, or (in the case of choice-based conjoint analysis and discrete choice experiments) make choices between a set of hypothetical options. These values can then be applied to real decision options to help patients and providers consider how their values might be reflected in actual decisions (e.g. which screening strategy to adopt), or they can be used to design new decision options, such as a new screening test.
Few previous studies have compared different techniques for values elicitation and clarification.10–12 We sought to compare, in a randomized trial, two explicit techniques for values clarification, choice-based conjoint analysis and a rating and ranking task, for decision making about colorectal cancer (CRC) screening. We chose to study CRC screening, because it requires consideration of several different potential screening strategies, each with different advantages and disadvantages that may be viewed differently by patients based on their personal values and preferences. We hypothesized that the conjoint analysis technique, which asks subjects to consider explicit trade-offs, might lead to greater engagement in the process of considering one’s values, and produce a more diverse pattern of most important attributes. Our main outcome of interest was the “most important attribute” determined from the conjoint analysis or the participant ranking task. Key secondary outcomes included the most important attribute based on a single post-task question, values clarity, intent to be screened, and unlabelled test preference.
METHODS
Study Participants
Participants were recruited from the UNC Decision Support Lab participant registry (made up of volunteers who have agreed to be available for decision making studies) and through the University of North Carolina’s mass informational electronic mail system for faculty, staff, and students. Participants recruited from the registry were contacted via their preferred contact method, either e-mail or postal mail. Those responding to the mass e-mail recruitment were contacted via email.
Potential participants were ages 48–75 years with no personal or immediate family (mother, father, sister, or brother) history of colon cancer, polyps, or inflammatory bowel disease. We did not exclude participants based on a history of recent CRC screening, but instead asked everyone to respond as if their doctor currently wanted them to decide about a CRC screening test. Those who were eligible and agreed to participate were randomized to intervention (conjoint task) or control (rating and ranking task). Participants were then mailed a packet of written material. The packet contained a pre-task survey (identical across all groups), either the conjoint or rating and ranking task, and a post-task survey (identical across all groups). All participants who completed and returned the surveys received a $25 gift card.
Development of Attributes
We developed a set of six key CRC screening test attributes from literature reviews and our previous research: ability to reduce CRC incidence and mortality, discomfort from screening, nature of the screening test, frequency of screening, risk of major complications over 10 years, and out-of -pocket costs over 10 years.13,14 These attributes were used for both the choice-based conjoint analysis tasks and rating and ranking tasks.
Development of Attribute Levels
We then developed a plausible range of levels for each attribute to be used in the conjoint analysis task. (See Appendix Table 1-available online) The range of the levels for each attribute was designed to cover the range of plausible values for each attribute, based on previous studies.15,16 We described the risk reduction for CRC incidence and mortality in relative terms, but also provided both groups with lifetime absolute risk levels in the absence of screening. We described risk of complications and out of pocket costs over 10 years to allow more accurate comparisons of different programs of screening. We chose to combine test location, preparation time, and time spent having the test in a single attribute, as these characteristics are clustered together for actual test options. Levels for this attribute were based on our prior research using patient time diaries.17,18
Development of the Values Elicitation and Clarification Tasks
Conjoint Task To create the conjoint analysis scenarios, we used a fractional factorial design implemented with Sawtooth Software (www.sawtoothsoftware.com) to generate a balanced and efficient choice-based set of choice tasks from our chosen attributes and levels. Each choice task involved a comparison of two hypothetical options (“1” and “2”) made up of the six attributes with different combinations of levels. For each task, the participant was asked to choose between options 1 and 2 or state that they had no preference between the two. (See Appendix 2—available online)Based on previous research suggesting that participants may fatigue when the number of choice scenarios is too high19, we chose to use a 15 scenario design, which increased feasibility while still maintaining a high level of design efficiency (d-efficiency 93.4). We also included a 16th scenario with a clear dominant option to check whether respondents were attending carefully to the choice tasks rather than answering randomly.
Rating and Ranking Test To create the rating and ranking task, we used the same attributes as for the choice-based conjoint task. The rating exercise asked participants to rate, on a Likert scale of 1–6, the importance of each attribute (1 = not important; 6 = very important). The ranking task then asked the respondent to rank the three most important of the six attributes.To control for ordering bias for both the rating and ranking and conjoint analysis tasks, we randomized all participants to one of five questionnaire versions that differed in terms of the ordering of the attributes participants viewed.
Study Process
Prior to answering the pre-task survey questions, participants were presented with written instructions and general information about colon cancer and colon cancer screening. Participants were instructed to imagine that their doctor has asked them to make a decision about colon cancer screening. They then completed the pre-task survey. After the pre-task survey, participants received additional written information about CRC and CRC screening and an explanation of the six attributes of CRC screening tests. (See Appendix 3, available online)
Measures
Surveys were the same for each group. The pre-task survey included demographic and colon cancer risk perception questions. The post-task survey included a single question assessing the most important attribute for each participant; a single question on screening test preference, in which respondents selected from a set of four unlabeled screening tests (designed to simulate fecal occult blood testing, sigmoidoscopy, colonoscopy, or a radiological test such as CT colonography) or the option of no screening; the values clarity sub-scale of the Decision Conflict Scale (three questions addressing clarity about how benefits and adverse effects matter to the individual, scored on 0–100 scale, with clear values defined as a score less than 25);20 and intent to be screened, measured on a five-point Likert scale.
Analyses
To calculate each participant’s most important attribute for those who completed the choice-based conjoint analysis task, we used the hierarchical Bayesian (HB) analytic tool from Sawtooth Software. Using HB allows one to estimate individual level values for the attribute importance values and the part-worth utilities (i.e. a quantitative assessment of the appeal of attribute levels) when using a choice-based format. Hierarchical Bayesian analysis generates an algorithm that essentially compares each individual’s responses to the different choice tasks to the overall sample’s responses. This estimation is done using a multinomial logit model and applying the algorithm repeatedly until it stabilizes (or converges). The multinomial logit model estimates the probability of a specific scenario being chosen as a reflection of the total utility for the chosen scenario (based on the sample response) relative to the total utility for all scenarios including the chosen one.21–23
Main Outcome Our main outcome was the most important attribute based on the conjoint analysis importance score and ranking task results. For those in the rating and ranking group, we considered each participant’s most highly ranked attribute to be the most important attribute. For those in the conjoint analysis group, we considered the attribute with the highest importance score to be the most important attribute. We compared, across groups, the proportions of participants reporting an attribute as being most important (using Pearson’s chi-square tests.)
Secondary Outcomes We used chi-square tests to compare the most important attribute as expressed on the single question from the post-task survey. We then examined agreement, using the kappa statistic, between each participant’s most important attribute determined from the values clarification task and their most important attribute based on the single question response.We also used chi-square tests to compare the proportion of participants with clear values in each group.20 T-tests were used to compare intent to be screened between groups. Finally, we performed stratified analyses to determine if there were differences in our results based on prior history of screening. Analyses were conducted in STATA 9.0.
RESULTS
Participant Characteristics
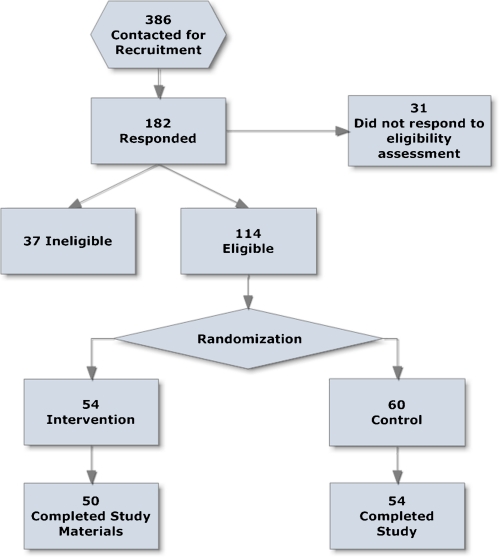
The study flow diagram is shown in the ase check if correct. Figure 1 and the characteristics of the 104 participants are shown in Table 1. There were few differences between groups in baseline characteristics, although the rating and ranking group had a somewhat higher proportion of participants who were up to date with screening than the conjoint analysis group (67% vs. 54%).
Figure 1.
Study flow.
Table 1.
Participant Characteristics
| Conjoint analysis Group (n = 50) | Rating/Ranking Group (n = 54) | |
|---|---|---|
| Mean age in years (SD) | 57.5 (5.7) | 56.9 (7.1) |
| % female | 68 | 72 |
| % Caucasian | 88 | 87 |
| % college graduate or higher | 74 | 68 |
| % Income < $45,000 | 20 | 25 |
| % up to date with any type of screening | 54 | 67 |
| % up to date with colonoscopy | 50 | 56 |
Responses
Among the 50 conjoint analysis respondents, two (4%) had one missing response each; 49 (98%) answered the dominant scenario correctly; and nine (18%) had at least one scenario in which they chose no preference. Of all 748 scenarios in which a response was recorded, 59 (7.8%) were “no preference”, with two respondents having six or more “no preference” responses. There were no missing responses to the rating and ranking task.
Most Important Attributes
For the conjoint analysis group, the most important attributes based on the calculated importance scores generated from the 16 choice tasks are shown in Table 2. The importance scores for each participant in the conjoint group are shown in Appendix 4—available online. The ability to reduce CRC incidence and mortality was the attribute most frequently determined (based on importance score) to be most important.
Table 2.
Conjoint Analysis-Based Most Important Attribute (n = 50)
| Highest importance score | 2nd highest importance score | 3rd highest importance score | % in top three | |
|---|---|---|---|---|
| Ability to reduce colorectal incidence and mortality | 56% | 20% | 10% | 86% |
| Discomfort | 2% | 0% | 2% | 4% |
| Nature of test | 18% | 24% | 32% | 74% |
| Frequency | 20% | 27% | 16% | 63% |
| Complications | 4% | 0% | 26% | 30% |
| Out of pocket costs | 0% | 29% | 14% | 43% |
The results of the rating and ranking tasks are shown in Table 3. Ratings were generally high (mean score > 4.0) for all attributes. The ability to reduce CRC incidence and mortality was again most frequently ranked as the most important attribute. Only four of the 54 participants (7.4%) in this group had clearly discordant ratings and rankings for most important attribute (i.e. their highest ranked attribute was rated lower than one or more other attributes).
Table 3.
Rating and Ranking of Attributes (n = 54)
| Attribute | Rating* | Ranking | |||
|---|---|---|---|---|---|
| Mean rating (SD) | Most important | 2nd most important | 3rd most important | % in top 3 | |
| Ability to reduce colorectal cancer incidence and mortality | 5.9 (0.4) | 76% | 11% | 9% | 96% |
| Discomfort | 4.1 (1.5) | 9% | 17% | 17% | 43% |
| Nature of test | 4.1 (1.6) | 4% | 7% | 13% | 24% |
| Frequency | 4.7 (1.4) | 2% | 22% | 15% | 39% |
| Complications | 4.7 (1.6) | 6% | 30% | 30% | 66% |
| Out of pocket costs | 4.3 (1.4) | 4% | 13% | 17% | 34% |
*Rated on 1–6 scale (1 = not at all important, 6 = very important)
The proportion of participants for whom reduction in CRC incidence and mortality was most important was lower for the conjoint analysis group (56%) than for the rating and ranking group (76%). (difference 20% points, 95% CI 3, 37; p < 0.001) Adjusting for baseline differences in being up to date with screening had little effect on the odds of choosing ability to reduce CRC as most important attribute (unadjusted OR 2.5 (95% CI 1.1,5.7); adjusted OR 2.1 (95% CI 0.9,5.1)).
Results for the most important attribute as assessed by a single question on the post-task questionnaire are shown in Table 4. Ability to reduce CRC incidence and mortality was the most frequent response in each group, and there were no differences between groups in the proportion of participants choosing that attribute as most important (56% vs. 61%, p = 0.597). Agreement between the most important attributes from the values clarification task and most important attribute from the single question on the post-task survey was moderate, and slightly higher for the rating and ranking group (simple agreement 65%, kappa 0.32) than for the conjoint analysis group (simple agreement 52%, kappa 0.26), suggesting the conjoint analysis may provide distinct information compared with a single question.
Table 4.
Most Important Attribute-Direct Question on Post-Survey
| Conjoint analysis group (n = 50) | Rating / Ranking (n = 54) | |
|---|---|---|
| Ability to reduce colorectal incidence and mortality | 56% | 61% |
| Discomfort | 12% | 7% |
| Nature of test | 8% | 6% |
| Frequency | 12% | 6% |
| Risk of major complications | 2% | 4% |
| Out of pocket costs | 10% | 17% |
Other Outcomes
There were no statistically significant differences between groups in the proportion of participants having clear values (based on a values clarity sub-scale score < 25): 76% for those completing the conjoint analysis task and 83% for those completing the ranking and rating task (p = 0.63). Intent to be screened was also similar between groups (4.2 for conjoint group vs. 4.4 for rating and ranking group, p = 0.22). Finally, unlabeled test preferences were also similar between groups: the set of attributes corresponding to screening colonoscopy every 10 years was most frequently chosen in each group, but the sets of attributes corresponding to FOBT and radiological testing were also popular; only 3% of respondents answered that they would choose “no testing.” (See Table 5)
Table 5.
Unlabeled Test Preference
| Conjoint analysis (n = 50) | Rating/Ranking (n = 54) | |
|---|---|---|
| FOBT-Based attributes and levels | 26% | 20% |
| Sigmoidoscopy-based attributes and levels | 0% | 0% |
| Colonoscopy-based attributes and levels | 44% | 39% |
| Radiologic test-based attributes and levels | 26% | 39% |
| No test | 4% | 2% |
FOBT = fecal occult blood test
DISCUSSION
We found that a choice-based conjoint analysis task produced somewhat different patterns of attribute importance compared with a rating and ranking task, but had little effect on other key outcomes, including values clarity, intent to be screened, and unlabelled screening test preference. This finding suggests that a choice-based method, which requires consideration of trade-offs between attributes, may provide distinct information about how patients value different test features compared with other simpler explicit methods like rating and ranking. However, completing the more involved conjoint analysis choice tasks does not appear to have large effects on more distal and global outcomes such as clarity about the decision, preferences about decision options, or intent to engage in health behaviors. Clinically, our findings suggest that the ability to reduce CRC incidence and mortality is the most important attribute for a majority, but not all, participants. The importance of other attributes differed across our sample, suggesting that providing information about each domain may be important in counseling patients.
Few prior studies have compared different techniques for values elicitation and clarification. O’Connor and colleagues found no difference in values clarity or treatment preference when comparing an implicit technique (provision of a balance sheet) versus an explicit rating task in 201 women deciding about hormone replacement therapy.10 In a trial of 137 participants considering a hypothetical heart disease prevention scenario, we found that rating and ranking did not produce differences in decisional conflict or intent to adopt risk-reducing interventions compared with an implicit approach, but the two approaches did produce somewhat different patterns of preferred labeled treatments.11 In another study of 113 volunteers, we found that a conjoint analysis task produced different patterns of preferences and treatment choices than direct elicitation for a hypothetical heart disease prevention scenario.12 Finally, Sheridan and colleagues found no difference in decisional conflict when they compared a prostate cancer screening decision aid without values clarification versus the decision aid with one of two different values clarification exercises (social matching and ranking / rating). However, participants differed in their intent to be screened, suggesting the method of values clarification may be important.24
Although we are not aware of other published studies that have compared different methods of values elicitation for CRC screening, several have used explicit techniques to assess key decisional attributes.13,25–28 (Details of these studies are provided in Appendix 5-available online) Most studies have found test accuracy (ability to detect cancer and polyps) to be the most common most important attribute, but the order of importance of other attributes has varied considerably across studies.
Our study has several limitations. First, we enrolled a relatively small sample population drawn from our decision laboratory registry and university e-mail lists. The small sample size limits our ability to detect small differences between groups with precision. Moreover, the size of a clinically meaningful effect for values clarification has not been well-defined, and will require further research to help design future studies. Second, our sample was not representative of the full population of adults ages 48–74, being more highly educated and predominantly female, although the proportion who were up to date with screening was similar (slightly lower) than the general population of North Carolinians of the same age range.29
Third, we studied a hypothetical scenario; real-world screening decisions (and evaluation of actual test completion) may produce different results. Fourth, a more extensive or different set of attributes may have produced different patterns of attribute importance. Similarly, choosing different levels may have produced different results for the conjoint task. Fifth, our use of a mail-based survey made it infeasible to examine the effect of giving conjoint results back to patients to determine the effect of such feedback. Sixth, information about absolute risk was provided in the introductory materials only; whether using absolute risks within the conjoint task would have affected results further is unclear.
We only provided limited information about CRC screening to both groups, and we did not provide the specific range of levels for each attribute to those in the rating and ranking group. Providing such information might have changed attribute preferences. However, our choice of information in the rating and ranking group was meant to provide a parsimonious approach to values elicitation, as might be performed in clinical encounters. Future studies might compare the conjoint analysis approach versus a rating and ranking task in which the range of levels was included in the attribute descriptions or against another technique like “max diff” scaling.28 We did not assess knowledge, so we cannot determine the extent to which the expressed values are representative of informed consumers. Finally, we measured our outcomes only after the values elicitation tasks. Measuring changes from pre-task to post-task might have provided more sensitive assessment of changes.
In conclusion, we found that attribute importance scores derived from a choice-based conjoint analysis produced somewhat different patterns of attribute importance than those derived from rating and ranking tasks for the decision about which strategy to use for CRC screening. Whether the differences in attribute values observed here are meaningful enough to warrant the additional time and effort required to complete the conjoint analysis / discrete choice tasks, compared with rating and ranking, or even implicit values clarification techniques, remains unclear and will require additional research.
Electronic supplementary material
(PDF 56 kb)
Acknowledgements
Grant support: Dr. Pignone was supported by an Established Investigator Award from the National Cancer Institute (K05 CA129166) and by the Foundation for Informed Medical Decision Making.
Prior Presentations: We presented this research as an oral presentation at the Society for Medical Decision Making 2010 National Meeting in Toronto.
Conflict of Interest None disclosed.
REFERENCES
- 1.Braddock CH, 3rd, Edwards KA, Hasenberg NM, Laidley TL, Levinson W. Informed decision making in outpatient practice: time to get back to basics. JAMA. 1999;282(24):2313–20. doi: 10.1001/jama.282.24.2313. [DOI] [PubMed] [Google Scholar]
- 2.Sheridan SL, Harris RP, Woolf SH. Shared Decision-Making Workgroup of the U.S. Preventive Services Task Force. Shared decision making about screening and chemoprevention. A suggested approach from the U.S. Preventive Services Task Force. Am J Prev Med. 2004;26(1):56–66. doi: 10.1016/j.amepre.2003.09.011. [DOI] [PubMed] [Google Scholar]
- 3.O’Connor AM, Bennett CL, Stacey D, Barry M, Col NF, Eden KB, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2009;8(3):CD001431. doi: 10.1002/14651858.CD001431.pub2. [DOI] [PubMed] [Google Scholar]
- 4.Pignone M, Harris R, Kinsinger L. Videotape-based decision aid for colon cancer screening. A randomized, controlled trial. Ann Intern Med. 2000;133(10):761–9. doi: 10.7326/0003-4819-133-10-200011210-00008. [DOI] [PubMed] [Google Scholar]
- 5.Elwyn G, O’Connor A, Stacey D, Volk R, Edwards A, Coulter A, et al. Developing a quality criteria framework for patient decision aids: online international Delphi consensus process. BMJ. 2006;333(7565):417. doi: 10.1136/bmj.38926.629329.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Connor AM, Bennett C, Stacey D, Barry MJ, Col NF, Eden KB, et al. Do patient decision aids meet effectiveness criteria of the international patient decision aid standards collaboration? A systematic review and meta-analysis. Med Decis Mak. 2007;27(5):554–74. doi: 10.1177/0272989X07307319. [DOI] [PubMed] [Google Scholar]
- 7.Elwyn G, O’Connor AM, Bennett C, Newcombe RG, Politi M, Durand MA, et al. Assessing the quality of decision support technologies using the International Patient Decision Aid Standards instrument (IPDASi) PLoS One. 2009;4(3):e4705. doi: 10.1371/journal.pone.0004705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ryan M, Gerard K. Using discrete choice experiments to value health care programmes: current practice and future research reflections. Appl Health Econ Health Policy. 2003;2(1):55–64. [PubMed] [Google Scholar]
- 9.Ryan M, Farrar S. Using conjoint analysis to elicit preferences for health care. BMJ. 2000;320:1530–1533. doi: 10.1136/bmj.320.7248.1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O’Connor AM, Wells GA, Tugwell P, Laupacis A, Elmslie T, Drake E. The effects of an ‘explicit’ values clarification exercise in a woman’s decision aid regarding postmenopausal hormone therapy. Health Expect. 1999;2(1):21–32. doi: 10.1046/j.1369-6513.1999.00027.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sheridan SL, Griffith J, Behrend L, Gizlice Z, Cai J, Pignone MP. Effect of adding a values clarification exercise to a decision aid on heart disease prevention: a randomized trial. Med Decis Mak. 2010;30(4):E28–39. doi: 10.1177/0272989X10369008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Griffith JM, Lewis CL, Hawley S, Sheridan SL, Pignone MP. Randomized trial of presenting absolute v. relative risk reduction in the elicitation of patient values for heart disease prevention with conjoint analysis. Med Decis Mak. 2009;29(2):167–74. doi: 10.1177/0272989X08327492. [DOI] [PubMed] [Google Scholar]
- 13.Hawley ST, Volk RJ, Krishnamurthy P, Jibaja-Weiss M, Vernon SW, Kneuper S. Preferences for colorectal cancer screening among racially/ethnically diverse primary care patients. Med Care. 2008;46(9 Suppl 1):S10–6. doi: 10.1097/MLR.0b013e31817d932e. [DOI] [PubMed] [Google Scholar]
- 14.Kim J, Whitney A, Hayter S, Lewis C, Campbell M, Sutherland L, et al. Development and initial testing of a computer-based patient decision aid to promote colorectal cancer screening for primary care practice. BMC Med Inform Decis Mak. 2005;28(5):36. doi: 10.1186/1472-6947-5-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pignone M, Rich M, Teutsch SM, Berg AO, Lohr KN. Screening for colorectal cancer in adults at average risk: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2002;137(2):132–41. doi: 10.7326/0003-4819-137-2-200207160-00015. [DOI] [PubMed] [Google Scholar]
- 16.Pignone M, Saha S, Hoerger T, Mandelblatt J. Cost-effectiveness analyses of colorectal cancer screening: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2002;137(2):96–104. doi: 10.7326/0003-4819-137-2-200207160-00007. [DOI] [PubMed] [Google Scholar]
- 17.Jonas DE, Russell LB, Sandler RS, Chou J, Pignone M. Patient time requirements for screening colonoscopy. Am J Gastroenterol. 2007;102(11):2401–10. doi: 10.1111/j.1572-0241.2007.01387.x. [DOI] [PubMed] [Google Scholar]
- 18.Jonas DE, Russell LB, Sandler RS, Chou J, Pignone M. Value of patient time invested in the colonoscopy screening process: time requirements for colonoscopy study. Med Decis Mak. 2008;28(1):56–65. doi: 10.1177/0272989X07309643. [DOI] [PubMed] [Google Scholar]
- 19.Johnson RM, Orme BK. how many questions should you ask in choice-based conjoint studies? Sawtooth software research paper series 1996.
- 20.Barratt A, Howard K, Irwig L, Salkeld G, Houssami N. Model of outcomes of screening mammography: information to support informed choices. BMJ. 2005;23(330):7497–936. doi: 10.1136/bmj.38398.469479.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Johnson R. Monotonicity constraints in choice-based conjoint with hierarchical Bayes Sawtooth software technical paper series 2000, available at www.sawtoothsoftware.com.
- 22.Bryan Orme, John Howell. Application of covariates within Sawtooth software’s CBC/HB program: theory and practical example. Sawtooth software technical paper series 2009, available at www.sawtoothsoftware.com.
- 23.Huber J. Achieving individual-level predictions from CBC data: comparing ICE and hierarchical bayes. Sawtooth technical paper series 1998, available at www.sawtoothsoftware.com.
- 24.Sheridan SL, Golin C, Harris RP, Driscoll D, Deal AM, Enemchukwu E, et al. A pilot randomized trial of two types of values clarification exercises to facilitate informed decision making for prostate cancer screening. Society of general internal medicine meeting (poster). Pittsburgh, PA. April 2008.
- 25.Marshall DA, Johnson FR, Phillips KA, Marshall JK, Thabane L, Kulin NA. Measuring patient preferences for colorectal cancer screening using a choice-format survey. Value Health. 2007;10(5):415–30. doi: 10.1111/j.1524-4733.2007.00196.x. [DOI] [PubMed] [Google Scholar]
- 26.DeBourcy AC, Lichtenberger S, Felton S, Butterfield KT, Ahnen DJ, Denberg TD. Community-based preferences for stool cards versus colonoscopy in colorectal cancer screening. J Gen Intern Med. 2008;23(2):169–74. doi: 10.1007/s11606-007-0480-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shokar NK, Carlson CA, Weller SC. Informed decision making changes test preferences for colorectal cancer screening in a diverse population. Ann Fam Med. 2010;8(2):141–50. doi: 10.1370/afm.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Imaeda A, Bender D, Fraenkel L. What is most important to patients when deciding about colorectal screening? J Gen Intern Med. 2010;25(7):688–93. doi: 10.1007/s11606-010-1318-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention (CDC) Vital signs: colorectal cancer screening among adults aged 50–75 years - United States, 2008. MMWR Morb Mortal Wkly Rep. 2010;59(26):808–12. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 56 kb)