ABSTRACT
BACKGROUND
The number of hospitalists in the US is growing rapidly, yet little is known about their worklife to inform whether hospital medicine is a viable long-term career for physicians.
OBJECTIVE
Determine current satisfaction levels among hospitalists.
DESIGN
Survey study.
METHODS
A national random stratified sample of 3,105 potential hospitalists plus 662 hospitalist employees of three multi-state hospitalist companies were administered the Hospital Medicine Physician Worklife Survey. Using 5-point Likert scales, the survey assessed demographic information, global job and specialty satisfaction, and 11 satisfaction domains: workload, compensation, care quality, organizational fairness, autonomy, personal time, organizational climate, and relationships with colleagues, staff, patients, and leader. Relationships between global satisfaction and satisfaction domains, and burnout symptoms and career longevity were explored.
RESULTS
There were 816 hospitalist responses (adjusted response rate, 25.6%). Correcting for oversampling of pediatricians, 33.5% of respondents were women, and 7.4% were pediatricians. Overall, 62.6% of respondents reported high satisfaction (≥4 on a 5-point scale) with their job, and 69.0% with their specialty. Hospitalists were most satisfied with the quality of care they provided and relationships with staff and colleagues. They were least satisfied with organizational climate, autonomy, compensation, and availability of personal time. In adjusted analysis, satisfaction with organizational climate, quality of care provided, organizational fairness, personal time, relationship with leader, compensation, and relationship with patients predicted job satisfaction. Satisfaction with personal time, care quality, patient relationships, staff relationships, and compensation predicted specialty satisfaction. Job burnout symptoms were reported by 29.9% of respondents who were more likely to leave and reduce work effort.
CONCLUSIONS
Hospitalists rate their job and specialty satisfaction highly, but burnout symptoms are common. Hospitalist programs should focus on organizational climate, organizational fairness, personal time, and compensation to improve satisfaction and minimize attrition.
KEY WORDS: hospital medicine, survey research, workforce, satisfaction, worklife
INTRODUCTION
The increasing number of hospitalists in the United States indicates a sustained demand for dedicated inpatient generalist physicians.1 The estimated number of hospitalists in the US has swelled to around 30,000 over the last 15 years2, a growth comparable to that of the emergency medicine specialty between 1980 and 2007.3 In 2010, the American Board of Internal Medicine began offering certification for internists who focus in hospital medicine in recognition of the distinct knowledge and skills of hospital medicine practice.4 With the aging US population, health care anticipates an ever growing need for quality hospitalists. The recruitment and retention of excellent and experienced physicians in the field depends on hospitalist jobs designed to be sustainable and rewarding.
The work of hospital medicine is demanding because of its typically relentless pace, spanning the hospital from the emergency room to the intensive care units.5 High volumes of patients with active clinical management and difficult social issues are typical.6 As a young specialty, hospitalists struggle to define their role for patients and the medical staff7, and younger hospitalist group leaders may be less effective advocates within their organizations. Other site-based specialties such as emergency and critical care medicine that share the fast-paced, high-workload, complex care of hospital patients have seen high levels of burnout, which influences job turnover and attrition.8,9
The first and only large survey of hospitalist demographics and worklife occurred in 1999.10 Since then, concerns about the sustainability of the specialty grew as reports of burnout, job turnover, and the demand for new hospitalists were common in the specialty newsletters.11 Some hospitalists feel they are treated as glorified residents.12 Others have sought better worklife balance in administrative work.5 In 2005, the Society of Hospital Medicine (SHM) convened a Career Satisfaction Task Force to study job design and to promote hospital medicine as a long-lasting career. Our focus is to determine the current satisfaction and burnout levels of US hospitalists, identify potentially modifiable factors, and understand hospitalist job design that can maximize satisfaction and minimize stress, burnout, and turnover.
METHODS
Survey Instrument
Following the conceptual framework of the Physician Worklife Survey13,14, we created a multidimensional instrument of job and specialty satisfaction tailored to hospitalists. We first performed a systematic review of US physician satisfaction to identify previous relevant research and key study domains.15 The 16-member SHM Career Satisfaction Task Force served as a focus group to appraise physician job satisfaction measures and other worklife domains (e.g., workload, work-life balance) for their applicability to hospitalists. An expert panel (TBW, KH, CTW) synthesized the focus group’s discussion to generate 14 domains most pertinent to current hospitalist job satisfaction which were further refined through multiple discussions in the focus group.
Drawing from past studies of physician worklife and organizational research13,16–30, items relevant to identified predictors and satisfaction domains were nonparsimoniously compiled into a single item bank. Psychometrically validated attitude questions and scales for established domains of satisfaction were modified to be applicable, meaningful, and appropriate to hospitalists. To address issues related to survey administration and space limitations, we truncated scales to balance validity and economy of space. In general, 5-point Likert scales were used: 1 disagree, 2 somewhat disagree, 3 neither agree nor disagree, 4 somewhat agree, and 5 agree. For newly identified satisfaction domains, novel items were developed and cognitively tested. The reliability of altered scales was tested by piloting the instrument in the Task Force and confirming Cronbach’s alpha of greater than 0.7 for most scales.
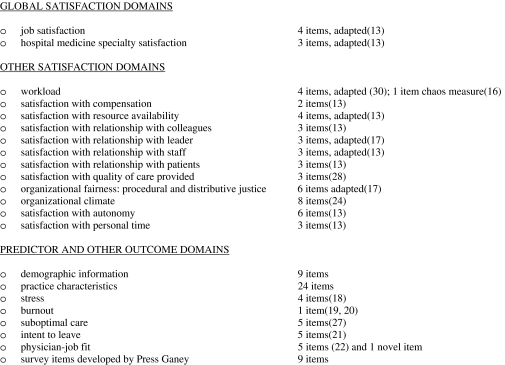
The final instrument consisted of 118 items and addressed the predictor and outcome domains shown in Figure 1. The published instrument was printed on a single double-sided 25.5 × 11-inch tri-fold form. The survey is available from the corresponding author.
Figure 1.
Survey item domains and sources addressed by the Hospital Medicine Physician Worklife Survey instrument.
Sampling Strategy
Our aims were to survey a nationally representative sample of hospitalists that allowed valid analyses of responses by gender, specialty training, and practice type. Our target population was all practicing self-identified hospitalist physicians in the US and Puerto Rico. We used the largest database of hospitalists currently available and maintained by the SHM as our sampling frame. In 2010, the database contained information on 24,000 individuals, representing both members of the organization and non-members who had participated in an organization event. In addition to practicing hospitalists, this database contains non-physicians, non-hospitalists, and trainees including some that are not specifically designated as such. Despite SHM’s efforts to keep the database information current, high job turnover and attrition led to outdated information. By linking employer information to hospital statistics from the American Hospital Association database31, we sampled from the frame based on four stratification variables: number of beds, geographic region, employment model, and specialty training. Due to small numbers, pediatric hospitalists were oversampled by including all physicians who indicated their specialty as either pediatrics or medicine-pediatrics. Adequate sample size was estimated using a two-sample comparison of means and background data from the PWS that suggested 2 cohorts of 216 each would provide 90% power to detect a 0.5-point difference in means of the global satisfaction measures at a significance level of 0.05. Without considering non-response, stratification, and clustering, 3 specialist cohorts totaling about 700 hospitalists was calculated to be adequate. However, anticipating traditionally low response rates with surveys of physicians and the likelihood of duplicate sampling and nondeliverable addresses from our sources, as well as non-hospitalists being included in the sampling frame, we sampled a total of 5,389 addresses. In addition, two multi-state hospitalist companies (EmCare, In Compass Health) and one for-profit hospital chain (HCA Inc.) sponsored this project with the stipulation that all of their hospitalist employees (n = 884) would be surveyed.
Data Collection
The health-care consulting firm Press Ganey provided support with survey layout and administration following the modified Dillman method.32 Three rounds of coded surveys and solicitation letters from the investigators were mailed 2 weeks apart in November and December 2009. Because of low response rates to the mailed survey, an online survey was created using Survey Monkey™. Two reminder e-mails containing a web link to the online survey were sent in January and February 2010 to 650 surveyees for whom e-mail addresses were available. To further increase the response rate, the online survey was also made available at a kiosk during the SHM annual meeting in April 2010 to be completed by physicians in the sampled pool who were among the attendees of the conference.
Data Analysis
Nonresponse bias was estimated by comparing demographic characteristics between respondents of separate survey waves.33 We assessed the quality of mailing addresses immediately following the survey period by mapping each address using Google™, and if the address was a hospital, researching online whether or not the intended recipient was currently employed there. Simple means, proportions, and medians were calculated for a descriptive table. Percentages of respondents whose satisfaction domain scores were 4 or greater on 5-point Likert scales were tabulated. Satisfaction with available resources (4 items), one of the 14 domains assessed, yielded a low reliability score (alpha = 0.35) and so was excluded from the analysis. Differences among specialties were examined for each of the remaining 11 satisfaction domains using the chi-square test. To permit comparison of results with the PWS, we also calculated the mean (95% confidence interval) of each satisfaction domain. Corrective weights were calculated to account for oversampling of pediatric hospitalists and applied to all applicable analyses including the calculation of weighted proportions and means. Correlations between each of the two global satisfaction outcomes (≥4 on 5-point scales vs. not) and the predictor satisfaction domains were derived using bivariate and multivariate logistic regression analyses. Respondents were defined as having burnout symptoms if they had a response of 3 or higher on a validated single-item 5-point scale.21,34 Weighted responses to the career longevity items were tabulated with burnout status, and significance was calculated using the chi-square test. Statistical significance was defined by alpha less than 0.05. All analyses were performed using STATA version 11.0 (College Station, TX). This study was approved by the Loyola University Institutional Review Board.
RESULTS
Response Rate
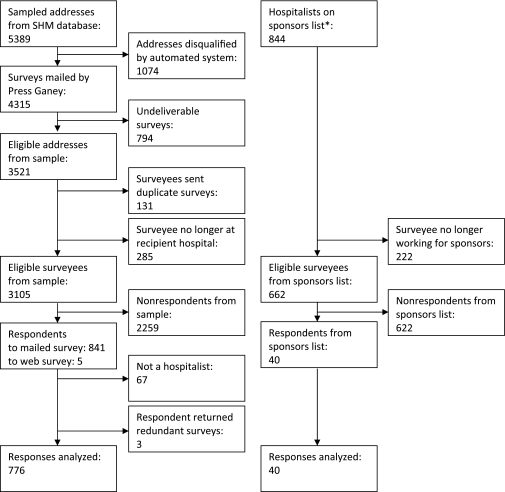
Of the 5,389 originally sampled addresses, 1,868 were undeliverable. Addresses were further excluded if they appeared in duplicate or were outdated. This yielded a total of 3,105 eligible surveyees in the sample. As shown in Figure 2, 841 responded to the mailed survey, while 5 responded to the web-based survey. Non-hospitalist respondents (67 surveys) and 3 duplicate surveys were rejected. In total, 776 surveys were included in the final analysis, for an adjusted response rate of 25.6% (776/3,035). An analysis of potential response bias found that members of SHM were more likely to return the survey than nonmembers. The adjusted response rate from hospitalists affiliated with our three sponsoring institutions was 6.0% (40/662). To augment the number of community hospitalists in our sample, we opted to analyze the responses from the sponsor hospitalists together with the sampled hospitalists. The resulting respondent pool was representative of the original survey frame.
Figure 2.
Sampling flow chart. *The three funding sponsors of this survey research were EmCare, In Compass Health, and HCA, Inc.
Demographics
Table 1 presents respondents’ demographic characteristics. After correcting for oversampling, 7.1% of hospitalists identified themselves as either a pediatric generalist or specialist-trained hospitalist. Among non-pediatric hospitalists, 75.7% were trained in general internal medicine, 3.7% in a medicine subspecialty, 7.0% in family medicine, and an additional 1.4% in another specialty. Women comprised 34.8% of respondents (33.5% correcting for pediatric oversampling). The mean age of hospitalists was 44.3 years, and the mean years of experience as a hospitalist and as a practicing physician were 6.9 and 12.6 years, respectively. Three quarters of hospitalists had graduated from US or Canadian medical schools.
Table 1.
Demographic Characteristics of Hospitalist Respondents
| Gender, n (%) | Total (n = 816) | NonPediatric hospitalists (n = 699) | Pediatric hospitalists (n = 117) |
|---|---|---|---|
| Male | 532 (65.2%) | 474 (67.8%) | 58 (49.6%) |
| Female | 284 (34.8%) | 225 (32.2%) | 59 (50.4%) |
| Age in years, mean (SD) | 44.3 (9.0) | 44.4 (9.0) | 43.6 (8.9) |
| Specialty, n (%) | |||
| General Internal Medicine or Pediatrics | 635 (77.8%) | 529 (75.7%) | 106 (90.6%) |
| Specialty Internal Medicine or Pediatrics | 37 (4.5%) | 26 (3.7%) | 11 (9.4%) |
| Family Medicine | 49 (6.0%) | 49 (7.0%) | na |
| Other | 10 (1.2%) | 10 (1.4%) | na |
| Unreported | 85 (10.5%) | 85 (12.2%) | 0 (0%) |
| Years experience as hospitalist, mean (SD) | 6.9 (4.5) | 6.7 (4.4) | 7.9 (5.1) |
| Years post residency experience, mean (SD) | 12.6 (8.7) | 12.6 (8.6) | 13.0 (9.8) |
| Medical School, n (%) | |||
| US or Canadian | 624 (76.5%) | 519 (74.2%) | 105 (89.7%) |
| Foreign | 141 (17.3%) | 130 (18.6%) | 11 (9.4%) |
| Unreported | 51 (6.2%) | 50 (7.2%) | 1 (0.9%) |
| Marital status, n (%) | |||
| Never married | 73 (8.9%) | 67 (9.6%) | 6 (5.1%) |
| Married | 645 (79.0%) | 541 (77.4%) | 104 (88.9%) |
| Divorced/separated | 41 (5.0%) | 34 (4.9%) | 7 (6.0%) |
| Other | 9 (1.1%) | 9 (1.3%) | 0 (0%) |
| Unreported | 48 (5.9%) | 48 (6.9%) | 0 (0%) |
Overall Satisfaction
Overall, 62.6% of respondents reported high satisfaction (≥4 on a 5-point scale) with their job and 69.0% with their specialty (Table 2). Overall, more hospitalists were satisfied with the quality of care they provide and their relationships with staff and colleagues (83.1%, 80.2%, 76.2%, respectively) than the other domains. The smallest proportion of hospitalists was satisfied with their organizational climate (10.5%). In fact, none of the hospitalists gave their organizational climate the maximum rating of 5 on the scale. Satisfaction with autonomy, compensation, and personal time also ranked relatively low.
Table 2.
Satisfaction of Hospitalists by Specialty Training
| N (weighted%) ≥4 on scale from 1 to 5 | Total | Internal medicine | Family medicine | Pediatrics | p-value |
|---|---|---|---|---|---|
| Mean (95% CI) | (n = 816) | (n = 555) | (n = 49) | (n = 117) | (Chi2) |
| Care quality | 678 (82.3%) | 457 (82.3%) | 37 (75.5%) | 109 (93.2%) | 0.005 |
| 4.35 (4.30, 4.40) | 4.32 (4.26, 4.39) | 4.28 (4.08, 4.49) | 4.52 (4.41, 4.62) | ||
| Relationship with staff | 654 (79.5%) | 441 (79.5%) | 38 (77.6%) | 103 (88.0%) | 0.086 |
| 4.32 (4.26, 4.37) | 4.29 (4.22, 4.35) | 4.33 (4.11, 4.56) | 4.56 (4.43, 4.68) | ||
| Relationship with colleagues | 622 (76.2%) | 424 (76.4%) | 32 (65.3%) | 89 (76.1%) | 0.221 |
| 4.18 (4.12, 4.24) | 4.19 (4.11, 4.26) | 4.09 (3.83, 4.34) | 4.22 (4.06, 4.37) | ||
| Relationship with leader | 618 (75.4%) | 412 (74.2%) | 38 (77.6%) | 93 (79.5%) | 0.455 |
| 3.92 (3.83, 4.02) | 3.89 (3.77, 4.00) | 3.83 (3.35, 4.31) | 3.95 (3.64, 4.25) | ||
| Relationship with patients | 517 (62.6%) | 335 (60.4%) | 31 (63.3%) | 85 (72.7%) | 0.044 |
| 4.01 (3.95, 4.07) | 3.96 (3.89, 4.04) | 4.02 (3.76, 4.28) | 4.20 (4.08, 4.32) | ||
| Workload | 350 (43.7%) | 245 (44.1%) | 25 (51.0%) | 38 (32.5%) | 0.032 |
| 3.71 (3.66, 3.76) | 3.71 (3.64, 3.77) | 3.87 (3.66, 4.08) | 3.67 (3.55, 3.79) | ||
| Organizational fairness | 252 (31.2%) | 172 (31.0%) | 14 (28.6%) | 31 (26.5%) | 0.611 |
| 3.22 (3.15, 3.28) | 3.23 (3.15, 3.31) | 3.14 (2.85, 3.43) | 3.17 (3.01, 3.34) | ||
| Personal time | 228 (28.3%) | 159 (28.7%) | 19 (28.8%) | 27 (23.1%) | 0.120 |
| 3.16 (3.10, 3.23) | 3.19 (3.11, 3.27) | 3.24 (2.92, 3.55) | 3.13 (2.96, 3.30) | ||
| Compensation | 226 (27.9%) | 153 (27.6%) | 16 (32.7%) | 29 (24.8%) | 0.581 |
| 2.93 (2.85, 3.02) | 2.95 (2.85, 3.06) | 3.01 (2.62, 3.40) | 2.85 (2.63, 3.07) | ||
| Autonomy | 143 (17.4%) | 92 (16.6%) | 13 (26.5%) | 22 (18.8%) | 0.201 |
| 3.14 (3.09, 3.19) | 3.14 (3.07, 3.20) | 3.26 (3.02, 3.49) | 3.21 (3.06, 3.35) | ||
| Organizational climate | 86 (10.7%) | 54 (9.7%) | 4 (8.2%) | 10 (8.6%) | 0.879 |
| 3.09 (3.05, 3.13) | 3.06 (3.01, 3.11) | 3.00 (2.80, 3.20) | 3.20 (3.10, 3.29) | ||
| Job satisfaction | 305 (61.9%) | 345 (62.2%) | 29 (59.2%) | 84 (71.8%) | 0.117 |
| 3.96 (3.89, 4.03) | 3.94 (3.85, 4.03) | 3.85 (3.54, 4.16) | 4.14 (3.97, 4.32) | ||
| Specialty satisfaction | 563 (68.1%) | 379 (68.3%) | 31 (63.3%) | 94 (80.3%) | 0.021 |
| 4.09 (4.02, 4.16) | 4.06 (3.97, 4.15) | 3.91 (3.63, 4.20) | 4.40 (4.25, 4.56) |
Satisfaction by Specialty
There were no differences in proportion of the highest job satisfaction by specialty training (Table 2). Hospital medicine specialty satisfaction was highest among pediatric-trained hospitalists compared with those trained in internal and family medicine. More pediatric trained hospitalists also rated their satisfaction with the quality of care they deliver and their relationships with patients at the highest level than did their counterparts.
Relationship Between Global Satisfaction and Satisfaction Domains
As Table 3 illustrates, all of the satisfaction domains were strongly and positively associated with global job and specialty satisfaction except for workload, which was negatively associated. In multivariate analyses, organizational climate, satisfaction with care quality, organizational fairness, personal time, relationship with leader, compensation, and relationship with patients all predicted job satisfaction. Satisfaction with personal time, care quality, relationship with patients and staff, and compensation predicted specialty satisfaction.
Table 3.
Unadjusted and Adjusted Odds Ratio for Binary Global Satisfaction Outcomes and Satisfaction Domain Measures on 5-point Scales
| Job satisfaction | Specialty satisfaction | |||
|---|---|---|---|---|
| Unadjusted | Adjusted* | Unadjusted | Adjusted* | |
| Care quality | 3.57 (2.76, 4.62) | 2.36 (1.40, 3.99) | 2.53 (2.01, 3.18) | 1.61 (1.01, 2.48) |
| Relationship with staff | 1.97 (1.61, 2.41) | 1.10 (0.74, 1.65) | 1.90 (1.55, 2.33) | 1.43 (1.01, 2.01) |
| Relationship with colleagues | 2.20 (1.82, 2.65) | 0.84 (0.56, 1.25) | 1.60 (1.35, 1.91) | 1.19 (0.86, 1.64) |
| Relationship with leader | 2.15 (1.81, 2.56) | 1.58 (1.20, 2.08) | 1.45 (1.24, 1.68) | 1.14 (0.89, 1.47) |
| Relationship with patients | 1.74 (1.45, 2.08) | 1.52 (1.03, 2.24) | 2.01 (1.66, 2.43) | 1.52 (1.10, 2.11) |
| Workload | 0.53 (0.43, 0.66) | 0.80 (0.50, 1.26) | 0.68 (0.55, 0.84) | 1.05 (0.71, 1.57) |
| Organizational fairness | 3.55 (2.87, 4.39) | 1.92 (1.25, 2.96) | 1.94 (1.62, 2.33) | 1.15 (0.80, 1.66) |
| Personal time | 2.45 (2.04, 2.93) | 1.79 (1.27, 2.51) | 1.75 (1.47, 2.07) | 1.81 (1.35, 2.42) |
| Compensation | 1.67 (1.47, 1.90) | 1.54 (1.19, 2.01) | 1.54 (1.35, 1.75) | 1.33 (1.06, 1.66) |
| Autonomy | 2.71 (2.16, 3.42) | 1.36 (0.83, 2.20) | 1.95 (1.56, 2.44) | 1.02 (0.68, 1.55) |
| Organizational climate | 5.12 (3.75, 6.99) | 2.41 (1.28, 4.52) | 2.51 (1.90, 3.31) | 0.87 (0.51, 1.49) |
*Adjusted for age, gender, experience as a hospitalist, subspecialty, and each of the satisfaction domain measures
Burnout and Intent to Leave or Decrease Work Effort
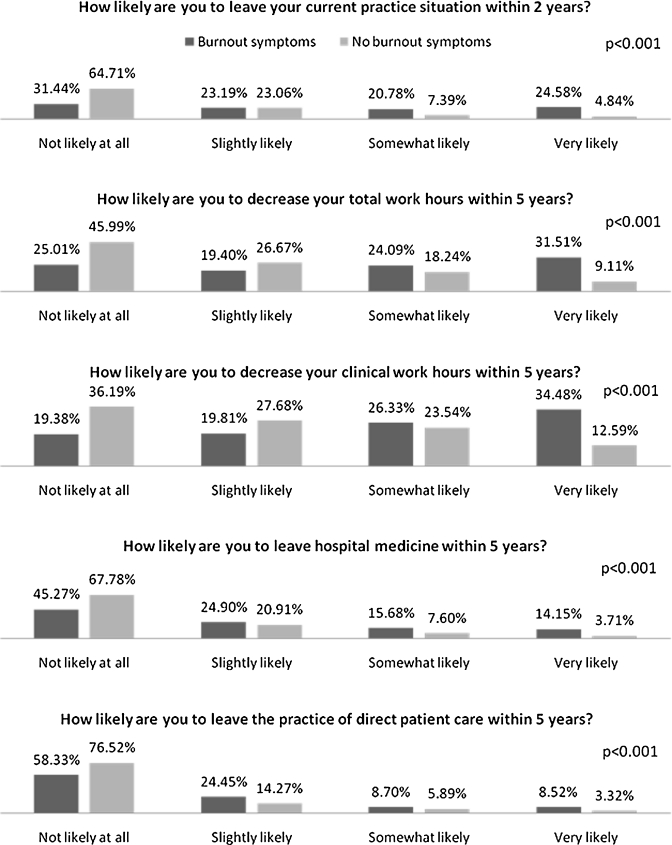
Burnout symptoms were reported in 29.9% of respondents. This was not different across specialty training. Hospitalists with burnout symptoms were much more likely to reduce work effort, leave their clinical situation, or abandon direct patient care altogether than those without burnout symptoms (Fig. 3).
Figure 3.
Responses to career longevity survey items by burnout symptoms. p < 0.001.
DISCUSSION
In this nationally representative sample, US hospitalists reported a relatively high degree of satisfaction overall with their job and with the hospital medicine specialty. They were most satisfied with the quality of care they were able to provide and with relationships with patients, staff, and colleagues, but had a low degree of satisfaction with personal time, autonomy, organizational climate, organizational fairness, and compensation. Across the subspecialties, pediatric-trained hospitalists had higher levels of hospitalist specialty satisfaction compared to those with internal and family medicine training. Organizational climate, care quality, fairness, personal time, relationship with leader, compensation, and relationship with patients all predicted job satisfaction. Satisfaction with personal time, relationship with patients and staff, and compensation predicted specialty satisfaction. Satisfaction with compensation had the weakest impact on specialty satisfaction of all of the significant predictors. Job burnout symptoms were reported by about 30 percent of hospitalists, a greater proportion of whom were more likely to reduce work efforts and leave their job or the profession than their colleagues without burnout symptoms.
While the high levels of hospitalist job and specialty satisfaction are positive signs for the longevity of the profession, there are several concerning risks to the sustainability of hospitalist work. First and foremost is the high rate of hospitalists reporting burnout symptoms and its strong relationship with the intent to decrease effort and to abandon clinical medicine. Unfortunately, we cannot directly compare burnout rates between this study and the 1999 hospitalist worklife study as different measures were used. However, the prior study found that only 13% of hospitalists were burned out and 25% were at risk of burnout.10 A 2002 and 2003 study of academic hospitalists using the same single-item burnout measure found burnout rates of 13% and 21% in respective years.21 Thus, the number of burned-out hospitalists may have increased over time.
As a career, hospital medicine is known for better compensation than similarly trained outpatient practicing physicians, and better lifestyle with flexibility in the number of hours worked and scheduling.10 Our study shows that hospitalists with higher satisfaction with personal time and compensation also had higher job and specialty satisfaction, yet most hospitalists in our study reported relatively low levels of satisfaction in these two domains. This indicates that current hospitalist work models may be less flexible in work hours than desired and that compensation has a relatively weak influence over global satisfaction.
Hospitalists also have unique relationships with their organizations given that they are site-based specialists. Our findings suggest that sufficient hospital resources are allowing hospitalists to deliver the highest quality care possible, but also indicate the need for hospitalist employers and organizations to address climate and fairness issues in hospitalist programs to improve satisfaction and retention. Recently, SHM worked with the American Medical Association, the American Hospital Association, and the Joint Commission to draft a set of principles for a sustainable and successful hospitalist program.35 These principles, which focus on organizational structure, communications, operations, and management, address the areas of deficiency elucidated in this study and may be a useful place for hospitalist programs to start.
There are notable differences in the current hospitalist workforce and in satisfaction compared to the last time hospitalist satisfaction was measured in 1999.10 The proportion of women in hospital medicine has risen from 26% to 33.5%, while the mean age has risen from 40.2 to 44.3 years (p < 0.001). In 1999, only 15.1% had been hospitalists for greater than 5 years, but half of practicing hospitalists today have made hospital medicine their careers for at least 6 years. This shows that many physicians are staying in the profession. Whether burnout and attrition are affecting hospitalists earlier or later in their careers remains an important question to be answered.
Although variations in survey scale preclude direct comparisons, hospitalists rated satisfaction comparably or higher than office-based physicians surveyed in the Physician Worklife Survey.13 These include satisfaction with the relationship with patients (mean, hospitalists 4.18 vs PWS 3.59–3.80), personal time (3.16 vs 2.66–2.92), job (3.96 vs 3.52–3.77), and specialty (4.18 vs 3.59–3.80). Autonomy alone appears lower in hospitalists (3.14 vs 3.27–3.50), possibly because of their often subordinate role with consultants. Hospitalist burnout rates were comparable to those of emergency medicine physicians and internist intensivists8,9, but lower than those for surgeons.36
This study has several limitations. First, the response rate of 25.6% is low for survey research in general, but is not unusual of physician surveys, which have seen declining participation over the years.36,37 Traditionally utilized sources of physician lists such as the AMA physician masterfile do not yet designate hospitalists. To further complicate the matter, hospital medicine is a transitional career for some physicians, and job turnover even among career hospitalists is believed to be high. Although SHM has made major efforts to assure the accuracy and currentness of the database, a simple post hoc analysis of data quality found many outdated addresses. We believe an unknown but significant proportion of nonresponse is due to surveys being sent to recipients that would be excluded from the survey population (invalid addresses and non-hospitalists) and that the true response rate may be higher than reported. Our assessment of nonresponse bias suggests that nonmembers compared to members of SHM were less likely to complete the survey. While this could have lead to a systematic oversampling of hospitalists engaged with the specialty, the known distributions of demographic characteristics were matched between our respondents and other surveys of hospitalists. Additionally, despite our efforts to capture a representative sample of all hospitalists, there may be categories of practicing hospitalists who were excluded from our sampling frame. Whether or not these hospitalists share attitudes and experiences of our respondents remains a valid question.
Hospital medicine jobs and careers are only continuing to grow in the US, making this specialty the fastest growing specialty in medicine. Of vital importance is creating hospitalist jobs and careers that are sustainable and successful. Although hospitalists have relatively high levels of overall job and specialty satisfaction, there are several areas of immediate concern that could impact hospitalist satisfaction and longevity in the profession, including high levels of burnout and organizational climate and fairness issues. Further studies are warranted to evaluate the job and workplace factors that are associated with low satisfaction and burnout, and can be remediated through hospitalist program and job redesign.
Acknowledgement
Supported in part by funding from Emcare, HCA Inc., In Compass Health, and SHM. Dr. Wetterneck was supported by K08-HS17014 from the Agency for Healthcare Research and Quality. Press-Ganey Associates assisted with survey layout and administration. The authors thank Kenneth A. Rasisnski and members of the SHM Career Satisfaction Task Force for their assistance in survey development. RJW is employed by Press Ganey Associates. JAM is employed by the Society of Hospital Medicine.
Conflict of Interest None disclosed.
Footnotes
(Supported by K08-HS17014 from the Agency for Healthcare Research and Quality) for the Society of Hospital Medicine Career Satisfaction Task Force
REFERENCES
- 1.Pham HH, Devers KJ, Kuo S, Berenson R. Health care market trends and the evolution of hospitalist use and roles. J Gen Intern Med. 2005;20(2):101–7. doi: 10.1111/j.1525-1497.2005.40184.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.2010 Media Kit. Society of Hospital Medicine; 2010 [updated 2010; cited 2011 April 12]; Available from: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Home&CONTENTID=23077&TEMPLATE=/CM/ContentDisplay.cfm.
- 3.U.S. Census Bureau: Physicians by Sex and Specialty: 1980 to 2007. [cited 2011 April 12]; Available from: http://www.census.gov/compendia/statab/2010/tables/10s0158.pdf.
- 4.Hospital Medicine, Focused Practice. American Board of Internal Medicine; [cited 2011 April 12]; Available from: http://www.abim.org/specialty/hospital-medicine.aspx.
- 5.Wachter RM, Goldman L. The hospitalist movement 5 years later. Jama. 2002;287(4):487–94. doi: 10.1001/jama.287.4.487. [DOI] [PubMed] [Google Scholar]
- 6.Wachter RM. The state of hospital medicine in 2008. Med Clin North Am. 2008;92(2):265–73. doi: 10.1016/j.mcna.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 7.Schneller ES, Epstein KR. The hospitalist movement in the United States: agency and common agency issues. Health Care Manage Rev. 2006;31(4):308–16. doi: 10.1097/00004010-200610000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Goldberg R, Boss RW, Chan L, Goldberg J, Mallon WK, Moradzadeh D, et al. Burnout and its correlates in emergency physicians: four years’ experience with a wellness booth. Acad Emerg Med. 1996;3(12):1156–64. doi: 10.1111/j.1553-2712.1996.tb03379.x. [DOI] [PubMed] [Google Scholar]
- 9.Guntupalli KK, Fromm RE., Jr Burnout in the internist-intensivist. Intensive Care Med. 1996;22(7):625–30. doi: 10.1007/BF01709737. [DOI] [PubMed] [Google Scholar]
- 10.Hoff TH, Whitcomb WF, Williams K, Nelson JR, Cheesman RA. Characteristics and work experiences of hospitalists in the United States. Arch Intern Med. 2001;161(6):851–8. doi: 10.1001/archinte.161.6.851. [DOI] [PubMed] [Google Scholar]
- 11.McCook A. Tackling burnout before it’s too late. Today’s Hospitalist. 2004;11:2010. [Google Scholar]
- 12.Holton L. Put more than money on the table when recruiting hospitalists. American College of Physicians; 2007 [updated 2007; cited 2011 April 12]; Available from: http://www.acphospitalist.org/archives/2007/02/recruiting.htm.
- 13.Konrad TR, Williams ES, Linzer M, McMurray J, Pathman DE, Gerrity M, et al. Measuring physician job satisfaction in a changing workplace and a challenging environment SGIM Career Satisfaction Study Group. Society of General Internal Medicine. . Med Care. 1999;37(11):1174–82. doi: 10.1097/00005650-199911000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Williams ES, Konrad TR, Linzer M, McMurray J, Pathman DE, Gerrity M, et al. Refining the measurement of physician job satisfaction results from the physician worklife survey. Med Care. 1999;37(11):1140–54. doi: 10.1097/00005650-199911000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Scheurer D, McKean S, Miller J, Wetterneck T. US physician satisfaction: a systematic review. Journal of hospital medicine. 2009;4(9):560–8. doi: 10.1002/jhm.496. [DOI] [PubMed] [Google Scholar]
- 16.Linzer M, Manwell LB, Williams ES, Bobula JA, Brown RL, Varkey AB, et al. Working conditions in primary care: physician reactions and care quality. Ann Intern Med. 2009;151(1):28–U48. doi: 10.7326/0003-4819-151-1-200907070-00006. [DOI] [PubMed] [Google Scholar]
- 17.Colquitt JA. On the dimensionality of organizational justice: A construct validation of a measure. J Appl Psychol. 2001;86(3):386–400. doi: 10.1037/0021-9010.86.3.386. [DOI] [PubMed] [Google Scholar]
- 18.Yang CL, Carayon P. Effect of Job Demands and Social Support on Worker Stress—a study of VDT users. Behav Inform Technol. 1995;14(1):32–40. doi: 10.1080/01449299508914623. [DOI] [Google Scholar]
- 19.Schmoldt RA, Freeborn DK, Klevit HD. Physician burnout: recommendations for HMO managers. HMO Pract. 1994;8(2):58–63. [PubMed] [Google Scholar]
- 20.Rohland BM, Kruse GR, Rohrer JE. Validation of a single-item measure of burnout against the Maslach Burnout Inventory among physicians. Stress Health. 2004;20(2):75–9. doi: 10.1002/smi.1002. [DOI] [Google Scholar]
- 21.Wetterneck T, Linzer M, Gangnon RE, Auerbach AD, Kaboli P, Schnipper JL, et al. Burnout and intent to leave in academic hospitalist and non-hospitalist general medical ward attendings. J Gen Intern Med. 2005;20:141. [Google Scholar]
- 22.Xie JL. Karasek’s model in the People’s Republic of China: Effects of job demands, control, and individual differences. Acad Manage J. 1996;39(6):1594–618. doi: 10.2307/257070. [DOI] [Google Scholar]
- 23.Wetterneck TB, Linzer M, McMurray JE, Douglas J, Schwartz MD, Bigby J, et al. Worklife and satisfaction of general internists. Arch Intern Med. 2002;162(6):649–56. doi: 10.1001/archinte.162.6.649. [DOI] [PubMed] [Google Scholar]
- 24.Linzer M, Manwell LB, Mundt M, Williams ES, Maguire A, McMurray JE, et al. Organizational Climate, Stress, and Error in Primary Care: The MEMO Study. Advances in Patient Safety. 2005;1:65–77. [PubMed] [Google Scholar]
- 25.Lindenauer PK, Pantilat SZ, Katz PP, Wachter RM. Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians. Ann Intern Med. 1999;130(4 Pt 2):343–9. doi: 10.7326/0003-4819-130-4-199902161-00003. [DOI] [PubMed] [Google Scholar]
- 26.Auerbach AD, Nelson EA, Lindenauer PK, Pantilat SZ, Katz PP, Wachter RM. Physician attitudes toward and prevalence of the hospitalist model of care: results of a national survey. Am J Med. 2000;109(8):648–53. doi: 10.1016/S0002-9343(00)00597-0. [DOI] [PubMed] [Google Scholar]
- 27.Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136(5):358–67. doi: 10.7326/0003-4819-136-5-200203050-00008. [DOI] [PubMed] [Google Scholar]
- 28.Carayon P, Hundt AS, Alvarado CJ, Springman SR, Ayoub P. Patient safety in outpatient surgery: The viewpoint of the healthcare providers. Ergonomics. 2006;49(5–6):470–85. doi: 10.1080/00140130600568717. [DOI] [PubMed] [Google Scholar]
- 29.Fields DL. Taking the measure of work: a guide to validated scales for organizational research and diagnosis. Thousand Oaks: Sage Publications; 2002. [Google Scholar]
- 30.Caplan RD, Cobb S, French JRP, Harrison R, Penneau SR. Job demands and worker health. Ann Arbor: University of Michigan, Institute for Social Research; 1980. [Google Scholar]
- 31.AHA Hospital Statistics. American Hospital Association; 2009 [updated 2009; cited 2011 April 12]; Available from: http://www.ahadata.com/ahadata/html/AHAStatistics.html.
- 32.Thorpe C, Ryan B, McLean SL, Burt A, Stewart M, Brown JB, et al. How to obtain excellent response rates when surveying physicians. Fam Pract. 2009;26(1):65–8. doi: 10.1093/fampra/cmn097. [DOI] [PubMed] [Google Scholar]
- 33.Armstrong JS, Overton TS. Estimating nonresponse bias in mail surveys. J Marketing Res. 1977;14(3):396–402. doi: 10.2307/3150783. [DOI] [Google Scholar]
- 34.McMurray JE, Linzer M, Konrad TR, Douglas J, Shugerman R, Nelson K, et al. The work lives of women physicians—results from the physician work life study. J Gen Intern Med. 2000;15(6):372–80. doi: 10.1111/j.1525-1497.2000.im9908009.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Principles for a sustainable and successful hospitalist program. American Medical Association; [cited 2011 April 12]; Available from: http://www.ama-assn.org/ama1/pub/upload/mm/21/sustainable-hospitalist-program.pdf.
- 36.Shanafelt TD, Balch CM, Bechamps GJ, Russell T, Dyrbye L, Satele D, et al. Burnout and career satisfaction among American surgeons. Ann Surg. 2009;250(3):463–71. doi: 10.1097/SLA.0b013e3181ac4dfd. [DOI] [PubMed] [Google Scholar]
- 37.Halpern SD, Hussen SA, Metkus TS, Ward NS, Luce JM, Curtis JR. Development of an e-mail database of US intensive care physicians. J Crit Care. 2007;22(1):28–31. doi: 10.1016/j.jcrc.2006.12.006. [DOI] [PubMed] [Google Scholar]