Abstract
Objective
To determine visual acuity improvement in children with strabismic and combined strabismic-anisometropic (combined-mechanism) amblyopia treated with optical correction alone and to explore factors associated with improvement.
Design
Prospective multi-center cohort study
Participants
146 children 3 to <7 years old with previously untreated strabismic amblyopia (N=52) or combined-mechanism amblyopia (N=94).
Methods
Optical treatment was provided as spectacles (prescription based on a cycloplegic refraction) that were worn for the first time at the baseline visit. Visual acuity with spectacles was measured using the Amblyopia Treatment Study HOTV© visual acuity protocol at baseline and every 9 weeks thereafter until no further improvement in visual acuity. Ocular alignment was assessed at each visit.
Main outcome measure
Visual acuity 18 weeks after baseline.
Results
Overall, amblyopic eye visual acuity improved a mean of 2.6 lines (95% confidence interval: 2.3 to 3.0), with 75% of children improving ≥2 lines and 54% improving ≥3 lines. Resolution of amblyopia occurred in 32% (95% confidence interval: 24% to 41%) of the children. The treatment effect was greater for strabismic amblyopia than for combined-mechanism amblyopia (3.2 versus 2.3 lines, adjusted P=0.003). Visual acuity improved regardless of whether eye alignment improved.
Conclusions
Optical treatment alone of strabismic and combined-mechanism amblyopia results in clinically meaningful improvement in amblyopic eye visual acuity for most 3 to <7-year-old children, resolving in at least one quarter without the need for additional treatment. Consideration should be given to prescribing refractive correction as the sole initial treatment for children with strabismic or combined-mechanism amblyopia before initiating other therapies.
Introduction
Amblyopia is often treated with occlusion or pharmacological penalization initiated simultaneously or soon after a spectacle correction is prescribed. Patching and atropine penalization have been considered the cornerstone of amblyopia treatment, with spectacle correction considered an adjunct rather than a primary treatment. Nevertheless, recent studies of children with anisometropic amblyopia have found spectacle correction alone often results in significant improvement in amblyopic eye visual acuity beyond that found from the immediate optical correction of refractive error.1-4 While similar observations have been reported for children with strabismic and combined-mechanism (strabismic-anisometropic) amblyopia,1, 5, 6 these studies had small numbers of subjects and did not report eye alignment before and after refractive correction.
The present study was designed to quantify the visual acuity improvement in children 3 to < 7 years of age with strabismic or combined-mechanism amblyopia treated with spectacle correction alone. In addition, we sought to explore the time course of improvement and factors associated with visual acuity improvement, particularly changes in ocular alignment.
Methods
The study was supported through a cooperative agreement with the National Eye Institute of the National Institutes of Health and was conducted by the Pediatric Eye Disease Investigator Group (PEDIG) at 35 clinical sites. The protocol and Health Insurance Portability and Accountability Act (HIPAA) compliant informed consent forms were approved by institutional review boards, the parent or guardian of each child gave written informed consent, and children gave assent as required. Study oversight was provided by an independent data and safety monitoring committee. The study adhered to the tenets of the Declaration of Helsinki and is listed on www.clinicaltrials.gov, under identifier NCT00669539 (accessed May 12, 2011). The protocol, which is available on the PEDIG website (www.pedig.net accessed May 12, 2011), is summarized below.
Screening Visit/Eligibility/Prescription of Spectacles
At screening, visual acuity was measured in each eye by a certified examiner using the Amblyopia Treatment Study single-surround HOTV protocol (ATS-HOTV©)7 on the Electronic Visual Acuity Tester (EVA©).8 Testing was performed with refractive correction based on a refraction using cyclopentolate 1% completed no more than 2 months prior to the examination. The cover-uncover test and the simultaneous prism and cover test (SPCT) were used to assess and measure ocular alignment at distance and near without refractive correction at this screening visit.
Major eligibility criteria for the study included: age 3 to <7 years; amblyopia associated with strabismus (measurable heterotropia by SPCT at distance and/or near fixation without spectacles) with or without anisometropia; visual acuity 20/40 to 20/400 in the amblyopic eye and 20/40 or better in the fellow eye; an inter-ocular difference of 3 or more logarithm of the minimum angle of resolution (logMAR) lines; no previous spectacle correction or prior amblyopia treatment; no myopia (≥ -0.25D spherical equivalent); and refractive error meeting at least one of: ≥ 1.00D of astigmatism in the amblyopic eye, ≥ 1.00D spherical equivalent anisometropia, or ≥ +2.00D spherical equivalent hyperopia in either eye.
Refractive error correction in this study was provided with spectacles prescribed based on the cycloplegic refraction. The protocol required full correction of anisometropia and astigmatism. We allowed either full correction or symmetrical undercorrection of hyperopia by no more than +0.50D. Bifocals were not permitted prior to the assessment of strabismus at the baseline visit, and allowed thereafter only if there was persistent esotropia with a greater magnitude at near.
Baseline Visit
The prescribed spectacles were not worn prior to the baseline visit, which occurred within 30 days of the screening visit. At baseline, the spectacle prescription was verified with a lensometer, and if the sphere and cylinder power were not within 0.25D of the prescribed correction, the spectacles were re-made and the child returned for baseline examination. After the spectacles had been worn for 10 to 30 minutes, corrected visual acuity was measured in each eye by a certified examiner using the ATS-HOTV© protocol7 presented on the EVA©.8 To decrease the chance that persistent accommodative tone would adversely affect distance visual acuity, both eyes were retested on the same day with a -1.00D lens over the spectacles. Baseline visual acuity was the better of the two acuity measures.
A child remained eligible for the study at the baseline visit if the requirements for amblyopia while wearing the spectacles were still met (visual acuity criteria for amblyopic and fellow eyes and for inter-ocular difference), regardless of whether the strabismus persisted with spectacle correction. Testing at this baseline visit included ocular alignment measurements by SPCT and stereoacuity testing with the Titmus Fly and Randot Preschool Stereoacuity (Stereo Optical Co., Chicago, IL) tests, all measured in spectacle correction.
Follow-up Visits
Protocol-specified follow-up visits were conducted 9 and 18 weeks (±10 days) after the baseline visit, with the 18-week visit specified as the primary outcome visit. At each follow-up visit, visual acuity was measured in each eye without cycloplegia by a study-certified examiner with the ATS-HOTV© 7 protocol on the EVA.8 Visual acuity testing was repeated with a -1.00D lens over spectacles in the amblyopic eye (to account for persistent accommodative tone), and repeated in the fellow eye when visual acuity was reduced 1 or more lines from the previous visit. The better of the two measures was recorded as the acuity measure for that visit. Ocular alignment by SPCT and stereoacuity also were measured.
At the time of the 18-week visit, if the better of the corrected amblyopic eye visual acuity with and without a -1.00D lens over the spectacles was not at least 1 line better than the visual acuity measure from the previous study visit, then study participation ended. Otherwise, follow up continued with visits every 9 weeks (±10 days) until amblyopic eye visual acuity was better than or equal to the best fellow eye acuity or visual acuity in the amblyopic eye did not improve at least 1 line (with or without a -1.00D lens) from the prior visit.
Statistical Methods
A sample size of 150 was chosen based upon the expected width of the 95% confidence intervals (CI) on mean improvement in visual acuity. Prior to starting the study, we planned to stratify all analyses by cause of amblyopia (strabismus only vs. combined-mechanism) at the time of screening because we hypothesized that factors associated with improvement might differ between groups based on different mechanisms of improvement. For analysis purposes, strabismic amblyopia was defined as amblyopia with any strabismus with the magnitude of anisometropia less than that specified for combined-mechanism amblyopia. Combined-mechanism amblyopia was defined as any strabismus (by SPCT at distance or near or a prior history of strabismus), and ≥0.75D difference between eyes in the vertical (J0) or the oblique (J45) Jackson cross cylinders or ≥1.41D vector difference in diopters (VDD).9, 10 Using this vector method for classification of cause resulted in 9 subjects who were classified as having strabismic amblyopia by the clinical criteria previously used by PEDIG11 to be classified as combined-mechanism amblyopia for the present analysis; we also analyzed these 9 subjects using the previous classification in a secondary sensitivity analysis. All visual acuity measures were converted to a logMAR score for analysis and all analyses were performed separately for the strabismic and combined-mechanism amblyopia groups.
The primary analysis consisted of estimation of the mean and 95% CI for change in visual acuity from baseline to 18 weeks. In addition, the proportion of subjects with 2 or more logMAR lines improvement in amblyopic eye visual acuity from baseline to 18 weeks and the proportion whose amblyopia resolved (defined as an improvement in amblyopic eye visual acuity to within 1 line of fellow eye visual acuity) and exact 95% CIs also were calculated. Sensitivity analyses were conducted using the last observation carried forward method for children missing their 18-week visual acuity measurement, or, for the analyses of the proportion of those with 2 or more lines improvement, imputing all missing values as ‘successes’ and, alternatively, as ‘failures.’ Parallel analyses were performed using best amblyopic eye visual acuity at any visit 18 weeks or later and amblyopic eye acuity at 9 weeks.
A longitudinal analysis using linear mixed models was used to evaluate if any of the following factors were independently associated with visual acuity improvement after adjustment for baseline amblyopic eye visual acuity: angle of deviation; amblyopic eye spherical equivalent refractive error; age at baseline; baseline stereoacuity level (categorized as 40-800, 3000, and >3000 seconds of arc); and amount of anisometropia defined as the vector difference in diopters (VDD) and the maximum of the Jackson cross cylinders at 0° and 45° (J0 and J45) in the amblyopic eye. Factors were treated as continuous unless indicated otherwise, with the linearity assumption checked using scatter plots. Angle of deviation was analyzed using ordinal scores based on the smallest of the distance and near angles using SPCT as follows: 1=orthotropia (0 prism diopters (Δ)), 2=microtropia (1 to 8 Δ), or 3=heterotropia (>8 Δ), to test whether angle size was associated with visual acuity improvement without assuming a strictly linear relationship. Initial models included the covariate of angle of deviation at baseline. In subsequent models, angle of deviation at screening and, as a time-dependent covariate, angle of deviation at the prior visit and angle of deviation at the current visit were evaluated together with the baseline angle. Each model was compared to a model containing no tropia variables to assess the statistical significance of the angle of deviation variables as a group, using the likelihood ratio test.
An analysis of covariance (ANCOVA) model including all children (not stratified by cause of amblyopia) adjusting for baseline factors (amblyopic spherical equivalent, maximum of J0 and J45, and VDD) was used to evaluate whether the mean change in amblyopic eye visual acuity from baseline to 18 weeks differed between the two causal groups. The exact Wilcoxon Signed-Rank test was used to test whether the changes in stereopsis and angle of deviation from screening to baseline and from baseline to 18 weeks differed from zero. Analyses were conducted using SAS Version 9.1 (SAS Institute, Cary, NC).
Results
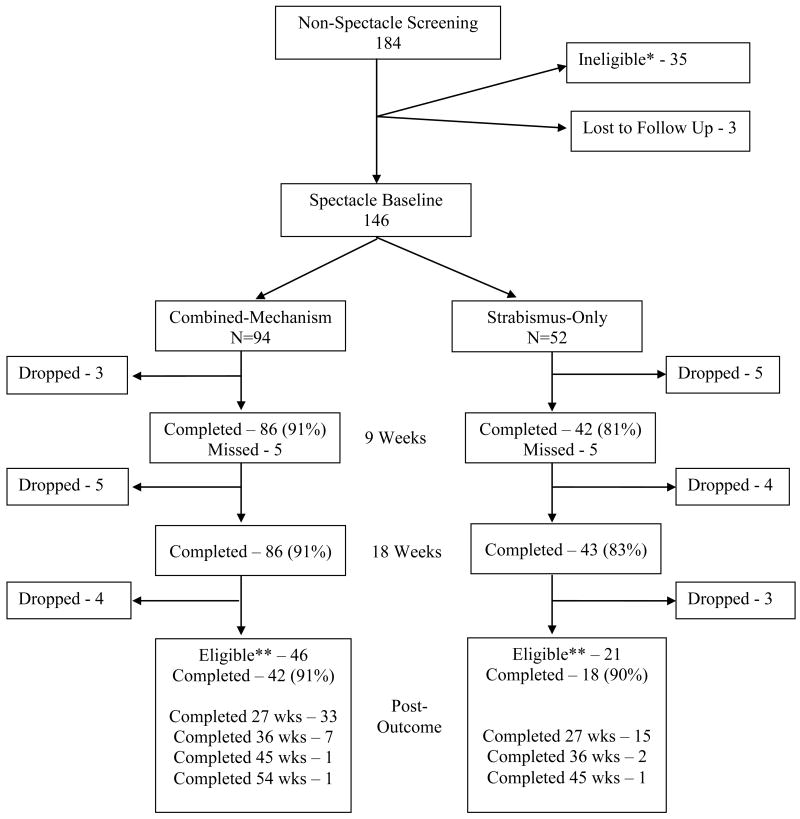
Between May 2008 and December 2009, 184 children were screened at 35 sites (Figure 1). Of these, 38 were not included in the analyses; 3 were lost to follow up and 35 were deemed ineligible because they no longer met visual acuity requirements at baseline (20), had no measureable heterotropia at screening by the SPCT (8), used spectacles or had other amblyopia treatment prior to baseline (4), and visual acuity was not measured according to study protocol (3). The remaining 146 children completed the spectacle baseline visit and were included in the analyses with 52 (36%) meeting criteria for strabismic amblyopia and 94 (64%) meeting criteria for combined-mechanism amblyopia. Overall, the mean improvement in amblyopic eye visual acuity at 18 weeks was 2.6 logMAR lines (95% CI= 2.3 to 3.0), with 75% (97 children; 95% CI= 67% to 82%) of the children improving ≥ 2 lines and 54% (70 children; 95% CI 45% to 63%) ≥ 3 lines. Resolution of amblyopia (defined as improvement in amblyopic eye visual acuity to within 1 line of fellow eye visual acuity) occurred in 32% (41 children; 95% CI 24% to 41%) by 18 weeks. The mean improvement was significantly greater in children with strabismic amblyopia compared with combined-mechanism amblyopia (3.2 versus 2.3 logMAR lines; P=0.003).
Figure 1. Visit Completion.
*Ineligible due to: improper method of evaluating visual acuity at screening (3), no measureable heterotropia at screening by Simultaneous Prism and Cover Test (8), no longer meeting eligibility requirement for visual acuity at baseline (20), and use of spectacles or other amblyopia treatment prior to baseline (4)
** Children who improved one or more lines from baseline were eligible to continue after 18-week primary outcome with visits every 9 weeks until no further improvement
Combined-mechanism Amblyopia
The mean age of the 94 children with combined-mechanism amblyopia was 5.1±1.1 years, 49% (46 children) were female, 87% (82 children) were white, and mean best-corrected visual acuity at baseline was 0.64 logMAR (approximately 20/80) in the amblyopic eye and 0.09 (approximately 20/25) in the fellow eye. Mean interocular difference in visual acuity at baseline was 5.4 lines. Table 1 provides additional baseline characteristics (Table 1, available at http://aaojournal.org).
Ocular Alignment Improvement with Spectacles at Baseline
Of the 85 children with heterotropia at distance at the screening visit, 12 (14%) improved to orthotropia at the spectacle-corrected baseline visit; the mean decrease between screening and baseline was 3.5Δ (quartiles 0.0, 5.0; Wilcoxon Signed-Rank Test P<0.001) (Table 2). Eight (9%) of the 88 children with heterotropia at near at the screening visit improved to orthotropia at the baseline visit, with a mean decrease of 4.6Δ (quartiles 0.0, 7.0; Wilcoxon Signed-Rank Test P<0.001) (Table 3).
Table 2. Ocular Alignment at Distance: Screening Visit (no correction) vs. Spectacle-corrected at Baseline Visit.
| Cause of Amblyopia | ||||||
|---|---|---|---|---|---|---|
| Combined (N=94) | Strabismus Only (N=52) | |||||
| Alignment at Baseline | Alignment at Baseline | |||||
| 0 Δ | 1-8 Δ | >8 Δ | 0 Δ | 1-8 Δ | >8 Δ | |
| N=18 | N=50 | N=26 | N=13 | N=16 | N=23 | |
| Alignment at Screening | ||||||
| 0 Δ n (%) | 6 (33%) | 3 (6%) | 0 | 1 (8%) | 0 | 0 |
| 1-8 Δ n (%) | 8 (44%) | 36 (72%) | 2 (8%) | 3 (23%) | 8 (50%) | 2 (9%) |
| >8 Δ n (%) | 4 (22%) | 11 (22%) | 24 (92%) | 9 (69%) | 8 (50%) | 21 (91%) |
| Mean Improvement in angle (SD) | 3.5 Δ (7.4) | 5.8 Δ (7.7) | ||||
| Median Improvement (P25, P75) | 1.0 Δ (0.0, 5.0) | 4.0 Δ (0.0, 10.0) | ||||
| Wilcoxon Signed Rank test P-value | P<0.001 | P<0.001 | ||||
Δ = prism diopter; SD = standard deviation; P25 = 25th percentile; P75 = 75th percentile
Table 3. Ocular Alignment at Near: Screening Visit (no correction) vs. Spectacle-corrected at Baseline Visit.
| Cause of Amblyopia | ||||||
|---|---|---|---|---|---|---|
| Combined (N=94) | Strabismus Only (N=52) | |||||
| Alignment at Baseline | Alignment at Baseline | |||||
| 0 Δ | 1-8 Δ | >8 Δ | 0 Δ | 1-8 Δ | >8 Δ | |
| N=12 | N=45 | N=37 | N=7 | N=11 | N=34 | |
| Alignment at Screening | ||||||
| 0 Δ n (%) | 4 (33%) | 1 (2%) | 1 (3%) | 0 | 0 | 0 |
| 1-8 Δ n (%) | 5 (42%) | 30 (67%) | 2 (5%) | 0 | 5 (45%) | 1 (3%) |
| >8 Δ n (%) | 3 (25%) | 14 (31%) | 34 (92%) | 7 (100%) | 6 (55%) | 33 (97%) |
| Mean Improvement in angle (SD) | 4.6 Δ (8.4) | 6.6 Δ (9.0) | ||||
| Median Improvement (P25, P75) | 2.0 Δ (0.0, 7.0) | 4.0 Δ (0.0, 11.0) | ||||
| Wilcoxon Signed Rank test P-value | P<0.001 | P<0.001 | ||||
Δ = prism diopter; SD = standard deviation; P25 = 25th percentile; P75 = 75th percentile
Amblyopic Eye Visual Acuity Improvement with Spectacles
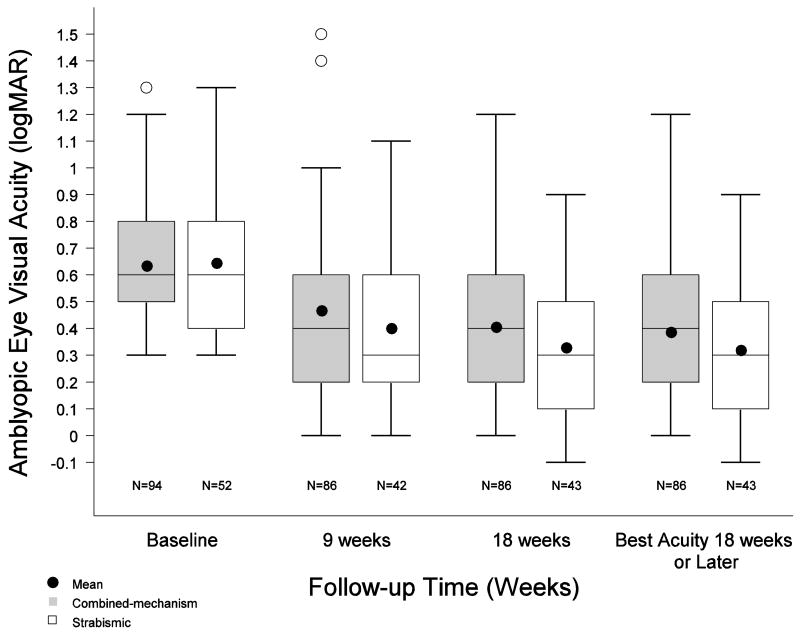
The 18-week primary outcome visit was completed by 86 of 94 (91%) of the combined-mechanism amblyopia cohort (Figure 1). At this visit, mean amblyopic eye visual acuity improved 2.3 logMAR lines (95% CI = 2.0 to 2.7) from baseline, with 69% (59 children; 95% CI= 58% to 78%) improving 2 or more lines, and 28% (24 children; 95% CI = 19% to 39%) meeting the definition for resolution (Table 4; Figure 2). There were no apparent differences in baseline amblyopic eye visual acuity or other baseline characteristics between those who completed the 18-week outcome visit and those who did not, with the exception that the children lost to follow-up tended to be older.
Table 4. Amblyopic Eye Visual Acuity Over Time.
| Baseline Visit | 9-Week Visit | 18-Week Visit | Best Acuity 18-weeks or Later* | |||||
|---|---|---|---|---|---|---|---|---|
| Combined | Strabismus | Combined | Strabismus | Combined | Strabismus | Combined | Strabismus | |
| N= 94 | N= 52 | N=86 | N=42 | N=86 | N=43 | N=86 | N=43 | |
| Change from Baseline | ||||||||
| ≥3 lines worse | 1 (1%) | 0 | 0 | 0 | 0 | 0 | ||
| 2 lines worse | 3 (3%) | 1 (2%) | 2 (2%) | 0 | 2 (2%) | 0 | ||
| 1 line worse | 3 (3%) | 0 | 2 (2%) | 0 | 2 (2%) | 0 | ||
| 0 lines | 14 (16%) | 4 (10%) | 10 (12%) | 3 (7%) | 10 (12%) | 3 (7%) | ||
| 1 line better | 16 (19%) | 7 (17%) | 13 (15%) | 2 (5%) | 10 (12%) | 2 (5%) | ||
| 2 lines better | 25 (29%) | 10 (24%) | 16 (19%) | 11 (26%) | 15 (17%) | 10 (23%) | ||
| ≥3 lines better | 24 (28%) | 20 (48%) | 43 (50%) | 27 (63%) | 47 (55%) | 28 (65%) | ||
| Mean (SD) logMAR lines change | 1.5 (1.9) | 2.5 (1.9) | 2.3 (1.8) | 3.2 (1.9) | 2.5 (1.9) | 3.3 (2.1) | ||
|
| ||||||||
| Distribution of Visual Acuity | ||||||||
| 20/125 or worse (≥ 0.8 logMAR) | 24 (26%) | 16 (31%) | 14 (16%) | 6 (14%) | 8 (9%) | 3 (7%) | 7 (8%) | 3 (7%) |
| 20/100 (0.7 logMAR) | 17 (18%) | 6 (12%) | 3 (3%) | 3 (7%) | 8 (9%) | 5 (12%) | 7 (8%) | 5 (12%) |
| 20/80 (0.6 logMAR) | 16 (17%) | 8 (15%) | 12 (14%) | 2 (5%) | 13 (15%) | 1 (2%) | 14 (16%) | 1 (2%) |
| 20/63 (0.5 logMAR) | 14 (15%) | 7 (13%) | 12 (14%) | 4 (10%) | 8 (9%) | 3 (7%) | 8 (9%) | 3 (7%) |
| 20/50 (0.4 logMAR) | 13 (14%) | 11 (21%) | 15 (17%) | 5 (12%) | 11 (13%) | 3 (7%) | 8 (9%) | 3 (7%) |
| 20/40 (0.3 logMAR) | 10 (11%) | 4 (8%) | 7 (8%) | 7 (17%) | 4 (5%) | 8 (19%) | 6 (7%) | 7 (16%) |
| 20/32 (0.2 logMAR) | 0 | 0 | 12 (14%) | 11 (26%) | 15 (17%) | 9 (21%) | 16 (19%) | 8 (19%) |
| 20/25 (0.1 logMAR) | 0 | 0 | 8 (9%) | 1 (2%) | 10 (12%) | 8 (19%) | 8 (9%) | 9 (21%) |
| 20/20 (0.0 logMAR) | 0 | 0 | 3 (3%) | 3 (7%) | 9 (10%) | 2 (5%) | 12 (14%) | 3 (7%) |
| 20/16 (-0.1 logMAR) | 0 | 0 | 0 | 0 | 0 | 1 (2%) | 0 | 1 (2%) |
| Mean (SD) logMAR | 0.64 (0.24) | 0.65 (0.26) | 0.47 (0.30) | 0.40 (0.26) | 0.41 (0.29) | 0.33 (0.25) | 0.39 (0.29) | 0.32 (0.26) |
| Snellen Equivalent | 20/80-2 | 20/80-2 | 20/63+1 | 20/50 | 20/50-1 | 20/40-1 | 20/50+1 | 20/40-1 |
|
| ||||||||
| Distribution of IOD | ||||||||
| -1 line (fellow eye worse) | 0 | 0 | 1 (1%) | 0 | 1 (1%) | 0 | 1 (1%) | 0 |
| 0 lines | 0 | 0 | 3 (3%) | 5 (12%) | 5 (6%) | 5 (12%) | 8 (9%) | 7 (16%) |
| +1 line (amblyopic eye worse) | 0 | 0 | 7 (8%) | 8 (19%) | 18 (21%) | 12 (28%) | 16 (19%) | 11 (26%) |
| +2 lines (amblyopic eye worse) | 0 | 0 | 16 (19%) | 9 (21%) | 10 (12%) | 8 (19%) | 10 (12%) | 8 (19%) |
| +3 lines (amblyopic eye worse) | 24 (26%) | 17 (33%) | 16 (19%) | 7 (17%) | 12 (14%) | 8 (19%) | 15 (17%) | 7 (16%) |
| ≥ +4 lines (amblyopic eye worse) | 70 (74%) | 35 (67%) | 43 (50%) | 13 (31%) | 40 (47%) | 10 (23%) | 36 (42%) | 10 (23%) |
| Mean (SD) logMAR lines | 5.4 (2.4) | 4.9 (2.2) | 4.2 (2.8) | 2.9 (2.4) | 3.7 (2.8) | 2.7 (2.3) | 3.5 (2.8) | 2.6 (2.4) |
| Proportion Resolve** | - | - | 13% | 31% | 28% | 40% | 29% | 42% |
Visit at which best amblyopic eye acuity achieved at 18-weeks or later for those that continued on spectacles alone
Amblyopic eye visual acuity is within 1 line of fellow eye acuity at the same visit
SD = standard deviation; logMAR = logarithm of the minimum angle of resolution; IOD = inter-ocular difference
Figure 2. Amblyopic Eye Visual Acuity Over Time.
For each visit, the box on the left (gray) is the distribution of amblyopic eye visual acuity (in logarithm of minimum angle of resolution) for children with combined-mechanism amblyopia, while the box on the right (white) represents children with strabismic-only amblyopia. The top and bottom of each box represent the 25th and 75th percentiles of the data, the group medians are represented by the middle line in each box, and the group means are represented by a dot. The bars extending above and below each box represent 1.5 times the interquartile range (difference between the 25th and 75th percentiles). The open circles represent individuals whose values are statistical outliers.
logMAR = logarithm of the minimum angle of resolution
Improvement in amblyopic eye visual acuity was associated with better baseline stereoacuity (children with 800 arc seconds or better of stereoacuity improved an average of 3.6 lines from baseline to the 18-week outcome visit compared to 2.1 lines in those with worse than 800 arc seconds, adjusted P=0.002) (Table 5, available at http://aaojournal.org). In contrast, improvement in amblyopic eye visual acuity was not associated with baseline amblyopic eye visual acuity (P=0.34), amblyopic eye spherical equivalent refractive error (P=0.07), age (P=0.83), anisometropia expressed as VDD (P=0.17) and as a maximum of J0/J45 (P=0.32), and magnitude of strabismus at baseline (P=0.88) (Table 5; Figure 3, available at http://aaojournal.org). Analyses examining the effect of the magnitude of strabismus at screening, current visit, and prior visit (with the latter 2 as time-dependent covariates) on improvement in visual acuity in addition to baseline angle also found no association (Table 6, available at http://aaojournal.org).
Similar results for change in visual acuity and factors associated with change were seen when substituting the best amblyopic eye acuity at 18 weeks or beyond, when using imputation methods for missing data, and when using the clinical criteria previously used by PEDIG11 to classify cause of amblyopia (data not shown).
Forty-two children whose visual acuity at the 18-week visit had improved from the 9-week visit continued treatment in spectacles alone beyond 18 weeks. Follow up continued for one 9-week cycle in 33 children, two 9-week cycles in 7 children, three 9-week cycles in 1 child, and four 9-week cycles in 1 child. On average, there was little additional improvement in visual acuity among these children (mean decrease of 0.1 logMAR lines from the 18-week primary outcome); however, 2 children improved 2 logMAR lines. The time point for reaching best visual acuity varied, with some children demonstrating visual acuity improvement for up to 45 weeks (Figure 4A, available at http://aaojournal.org). Best visual acuity measured at or subsequent to the 18-week primary outcome visit improved from baseline an average of 2.5 logMAR lines (95% CI = 2.1 to 2.9, Table 4).
Course of Ocular Alignment and Visual Acuity in Spectacles after Baseline
Of the 69 children with heterotropia at distance at the spectacle-corrected baseline visit, 24 (35%) improved to orthotropia at the 18-week primary outcome visit; 20 (27%) of the 75 children with heterotropia at near at the baseline visit improved to orthotropia at 18 weeks. The overall improvement in ocular alignment from baseline to 18 weeks was modest, with a mean decrease of 1.7Δ (quartiles 0.0, 2.0; Wilcoxon Signed-Rank Test P=0.004) at distance (Table 7) and 2.5Δ (quartiles 0.0, 5.0; Wilcoxon Signed-Rank Test P<0.001) at near (Table 8).
Table 7. Ocular Alignment at Distance: Spectacle-corrected Baseline Versus 18-week Primary Outcome.
| Cause of Amblyopia | ||||||
|---|---|---|---|---|---|---|
| Combined (N=86) | Strabismus Only (N=43) | |||||
| Alignment at 18 Weeks | Alignment at 18 Weeks | |||||
| 0 Δ | 1-8 Δ | >8 Δ | 0 Δ | 1-8 Δ | >8 Δ | |
| N=38 | N=35 | N=13 | N=24 | N=9 | N=10 | |
| Alignment at Baseline | ||||||
| 0 Δ n (%) | 14 (37%) | 3 (9%) | 0 | 9 (38%) | 1 (11%) | 0 |
| 1-8 Δ n (%) | 18 (47%) | 26 (74%) | 1 (8%) | 8 (33%) | 6 (67%) | 1 (10%) |
| >8 Δ n (%) | 6 (16%) | 6 (17%) | 12 (92%) | 7 (29%) | 2 (22%) | 9 (90%) |
| Mean Improvement (SD) | 1.7 Δ (5.2) | 5.1 Δ (9.0) | ||||
| Median Improvement (P25, P75) | 0.0 Δ (0.0, 2.0) | 2.0 Δ (0.0, 9.0) | ||||
| Wilcoxon Signed-Rank test P-value | P=0.004 | P<0.001 | ||||
Δ = prism diopter; P25 = 25th percentile; P75 = 75th percentile
Table 8. Ocular Alignment at Near: Spectacle-corrected Baseline Versus 18-week Primary Outcome.
| Cause of Amblyopia | ||||||
|---|---|---|---|---|---|---|
| Combined (N=86) | Strabismus Only (N=43) | |||||
| Alignment at 18 Weeks | Alignment at 18 Weeks | |||||
| 0 Δ | 1-8 Δ | >8 Δ | 0 Δ | 1-8 Δ | >8 Δ | |
| N=29 | N=40 | N=17 | N=13 | N=16 | N=14 | |
| Alignment at Baseline | ||||||
| 0 Δ n (%) | 9 (31%) | 2 (5%) | 0 | 5 (38%) | 0 | 0 |
| 1-8 Δ n (%) | 12 (41%) | 27 (68%) | 1 (6%) | 4 (31%) | 6 (38%) | 0 |
| >8 Δ n (%) | 8 (28%) | 11 (28%) | 16 (94%) | 4 (31%) | 10 (63%) | 14 (100%) |
| Mean Improvement (SD) | 2.5 Δ (5.4) | 6.3 Δ (7.6) | ||||
| Median Improvement (P25, P75) | 1.0 Δ (0.0, 5.0) | 6.0 Δ (0.0, 10.0) | ||||
| Wilcoxon Signed-Rank test P-value | P<0.001 | P<0.001 | ||||
Δ = prism diopter; P25 = 25th percentile; P75 = 75th percentile
Stereopsis and Fellow Eye Visual Acuity at Outcome
At 18 weeks, stereoacuity was within one level of baseline in 44 (51%) children, two or more levels better in 22 (26%), and two or more levels worse in 4 (5%); 16 (19%) children were unable to understand the test, and so could not be scored at either baseline or 18 weeks (11 at baseline and 9 at 18 weeks) (P<0.001; Wilcoxon Sign-Rank test). The mean change in fellow eye visual acuity from baseline to the 18-week outcome was 0.6 logMAR lines (95% CI, 0.4 to 0.8).
Strabismic Amblyopia
The mean age of the 52 children in the strabismic amblyopia group was 4.7±1.0 years, 44% (23 children) were female, 71% (37 children) were white, and the mean visual acuity at baseline with spectacles was 0.65 logMAR (approximately 20/80) in the amblyopic eye and 0.16 logMAR (approximately 20/32) in the fellow eye. Mean interocular difference in acuity at baseline was 4.9 lines. Table 1 provides additional baseline characteristics (Table 1, available at http://aaojournal.org).
Ocular Alignment Improvement with Spectacles at Baseline
Of the 51 children with heterotropia at distance at the screening visit, 12 (24%) improved to orthotropia at the spectacle-corrected baseline visit; the mean decrease between screening and baseline was 5.8Δ (quartiles 0.0, 10.0; Wilcoxon Signed-Rank Test P<0.001) (Table 2). Seven (13%) of the 52 children with heterotropia at near at the screening visit improved to orthotropia at the baseline visit, with a mean decrease of 6.6 Δ (quartiles 0.0, 11.0; Wilcoxon Signed-Rank Test P<0.001) (Table 3).
Amblyopic Eye Visual Acuity Improvement with Spectacles after Baseline
The 18-week primary outcome visit was completed by 43 of the 52 (83%) children in the strabismic amblyopia cohort (Figure 1). At this visit, mean amblyopic eye visual acuity improved 3.2 logMAR lines (95% CI 2.6 to 3.8) with 88% (38 children; 95% CI 75% to 96%) improving 2 or more logMAR lines, and 40% (17 children; 95% CI 25% to 56%) meeting the definition for resolution (Table 4). There were no apparent differences in baseline amblyopic eye visual acuity or other baseline characteristics between those who completed the 18-week outcome visit and those who did not.
Improvement in amblyopic eye visual acuity was associated with worse baseline visual acuity and better baseline stereoacuity. Children with 20/125 or worse baseline acuity improved an average of 3.9 lines by 18 weeks compared to 2.9 lines in those with 20/100 or better visual acuity (adjusted P=0.002); children with 800 or better arc seconds of stereoacuity improved an average of 3.4 lines at 18 weeks compared to 3.1 lines in those with worse than 800 arc seconds (adjusted P=0.03) (Table 5, available at http://aaojournal.org). In contrast, change in amblyopic eye visual acuity was not associated with magnitude of strabismus at baseline (P=0.53), amblyopic eye spherical equivalent (P=0.43), age (P=0.54), and anisometropia expressed as VDD (P=0.69) or expressed as maximum of J0/J45 (P=0.11) (Table 5, available at http://aaojournal.org). Additional analyses examining the effect of magnitude of strabismus at screening and current visit (as a time-dependent covariate) in addition to baseline angle on improvement in visual acuity also found no association (Table 6, available at http://aaojournal.org). Analysis of the effect of magnitude of strabismus at the prior visit (as a time-dependent covariate) and baseline angle of deviation on improvement in visual acuity also found no association when tested as a group. However, when tested individually, the data suggested children with larger angles of strabismus at the prior visit experienced more improvement in visual acuity at the current visit (adjusted P=0.04, Table 6, available at http://aaojournal.org).
Similar results for change in visual acuity and factors associated with change were seen when substituting the best amblyopic eye acuity at 18 weeks or beyond, when using imputation methods for missing data, and when using the clinical criteria previously used by PEDIG11 to classify cause of amblyopia (data not shown).
Eighteen children whose visual acuity at the 18-week visit improved from the 9-week visit continued on spectacles alone. Follow-up continued for one 9-week cycle in 15 children, two 9-week cycles in 2, and three 9-week cycles in 1. There was little additional improvement in visual acuity among these children (mean decrease of 0.4 logMAR lines from the 18-week primary outcome); however, one child improved 2 logMAR lines. The time point for reaching best visual acuity varied, with improvement in some children continuing for up to 36 weeks (Figure 4B, available at http://aaojournal.org). Best visual acuity measured at or subsequent to the 18-week primary outcome visit improved from baseline an average of 3.3 logMAR lines (95% confidence interval 2.6 to 3.9) from baseline (Table 4).
Course of Ocular Alignment and Visual Acuity in Spectacles
Of the 33 children with strabismus at distance at the spectacle-corrected baseline visit, 15 (45%) became orthotropic at the 18-week primary outcome visit; 8 (21%) of the 38 children with strabismus at near at the baseline visit improved to orthotropia at 18 weeks. The mean decrease between baseline and 18 weeks was 5.1Δ (quartiles 0.0, 9.0; Wilcoxon Signed-Rank Test P<0.001) at distance (Table 7) and 6.3Δ (quartiles 0.0, 10.0; Wilcoxon Signed-Rank Test P<0.001) at near (Table 8).
Stereopsis and Fellow Eye Visual Acuity at Outcome
At 18 weeks, stereoacuity was within one level of baseline in 25 (58%) children, two or more levels better in 10 (23%), and two or more levels worse in none; 8 (19%) children were unable to understand the test, and so could not be scored at either baseline or 18 weeks (7 at baseline and 5 at 18 weeks) (P<0.001 from Wilcoxon Signed-Rank test). The mean change from baseline to 18-weeks in fellow eye visual acuity was 0.9 logMAR line (95% CI 0.6 to 1.3).
Discussion
In this prospective study of 146 children 3 to <7 years of age with previously untreated strabismic and combined-mechanism amblyopia, we found that refractive correction with spectacles alone resulted in a clinically meaningful improvement in amblyopic eye visual acuity in the majority of children. Overall, a mean improvement of 2.6 lines occurred in the amblyopic eye, with 75% of children improving ≥ 2 lines and 54% by ≥ 3 lines. Resolution of amblyopia occurred in 32%. The magnitude of the treatment effect was significantly greater in those with strabismic amblyopia than those with combined-mechanism amblyopia (3.2 versus 2.3 logMAR lines).
This beneficial effect of refractive error correction on amblyopia has been previously termed “refractive adaptation” by another investigator group.1, 12, 13 We prefer the term “optical treatment” of amblyopia,2 because it emphasizes that optical correction of refractive error alone has a true treatment effect on amblyopia beyond the immediate visual acuity gains from simply eliminating optical blur.
The magnitude of the overall mean amblyopic eye visual acuity improvement in our study (2.6 logMAR lines) is comparable to several smaller studies of newly diagnosed strabismic, anisometropic, and combined-mechanism amblyopia.1, 2, 5, 6, 12 While a study by Chen and coworkers3 reported a greater improvement (3.8 logMAR lines), their cohort included only children with anisometropic amblyopia who were compliant with treatment.
Improvement in amblyopic eye visual acuity with spectacles alone in pure anisometropic amblyopia is readily understandable because the refractive correction provides equally clear retinal images. The mechanism by which visual acuity improves in strabismic amblyopia, with or without anisometropia, is not apparent unless the optical correction eliminates the strabismus at one position of gaze allowing binocular vision. Without elimination of the tropia, the underlying amblyogenic condition of a manifest strabismus is still present, and active cortical inhibition presumably remains.
It is possible that a reduction in the angle of strabismus to a microtropia allows binocularity as opposed to when a larger magnitude strabismus persists.14 During the planning of our study, we considered two possible hypotheses for improvements in amblyopic eye visual acuity. Visual acuity improvement might be associated with improvement in ocular alignment (particularly to orthotropia or microtropia) or alternatively, it might be associated with improved retinal image clarity, despite persistent strabismus.
Our results indicate that the gains in amblyopic eye visual acuity were similar for all children regardless of angle of deviation, even for children with strabismus that remained >8Δ at baseline wearing their spectacles, as well as those who had a residual strabismus >8Δ at the 18-week outcome visit. We found no association between visual acuity improvement and ocular alignment at baseline and at the current visit. It is uncertain why there is an association between worse angle of deviation at the prior visit and more improvement in visual acuity in the group with strabismic amblyopia; the association could be a product of chance. Amblyopic eye visual acuity improved regardless of the residual angle of strabismus.
The mechanism for improvement of amblyopic eye visual acuity with optical treatment alone in strabismic and combined-mechanism amblyopia, in the absence of elimination of the strabismus is unknown. It is possible that the amblyopic eye fixates during some activities, and thus takes advantage of the newly focused image. This speculative mechanism may be analogous to that occurring in amblyopic children treated with atropine or a Bangerter filter who have no evidence of fixation switch to the amblyopic eye, yet still experience improved visual acuity.15-17 Our finding of greater improvement in strabismic amblyopia than combined-mechanism amblyopia might be explained by the presence of a more profound insult induced from two amblyogenic factors (strabismus and anisometropia) in combined-mechanism amblyopia, in contrast to a single insult in strabismic amblyopia. Nevertheless, we have not found such a difference in response to patching,11, 18, 19 atropine11, 16, 20 or Bangerter filters.17
The time course of maximum improvement in amblyopic eye visual acuity varied with approximately 50% of the children having achieved their best acuity by 9 weeks, 90% by 18 weeks, and all by 45 weeks. It is possible that the definition of visual acuity “stability” (i.e., not improved at least 1 line from the previous study visit) used to determine study completion at the 18-week outcome and subsequent follow-up examinations underestimated the time course of maximum improvement in some patients.2 Nevertheless, these results are similar to previous reports of optical treatment of amblyopia1-3, 5, 21 Given this variability and that nearly one-third will resolve with spectacles alone, it is reasonable to monitor visual acuity in spectacles until no further improvement has occurred prior to instituting additional amblyopia treatment.
Similar to previous reports,1-3 the beneficial effect of spectacle correction was consistent throughout the 3 to <7 years age range in children with strabismic and combined-mechanism amblyopia. Furthermore, there was no relationship between the degree of refractive error in the amblyopic eye and visual acuity improvement.
The primary limitation of our study is the lack of control subjects not prescribed spectacles. Although our original intent was to perform a randomized clinical trial, during the planning of the study we determined that most of our investigators were reluctant to randomize hyperopic children with esotropia to “no optical correction” because of the possibility of an accommodative component of the strabismus. Thus, the reported treatment effect could be an overestimate because of possible learning effects or regression to the mean. Nevertheless, we believe that optical treatment was primarily responsible for the improvement in visual acuity found in this study for several reasons. First, the magnitude of improvement in our study exceeded any expected learning effect,8 and the length of the study was not sufficient for visual maturation to play a role. Second, visual acuity change in the fellow eye was modest over the duration of the study and the decrease in interocular difference paralleled the improvement measured in the amblyopic eye. Third, it is unlikely that regression toward the mean from repeated measures would fully account for the magnitude of improvement found. Last, to guard against reduced acuity at baseline from incomplete relaxation of accommodation when wearing new hyperopic spectacles, we retested visual acuity with -1.00 D over the spectacles and used the better of the two baseline measures.
This study has a number of strengths. It was performed prospectively, included a large cohort of children with both strabismic and combined-mechanism amblyopia, and enrolled children with a wide range of amblyopic eye visual acuity. None of the children wore spectacles prior to their baseline acuity measurement, certified examiners performed the outcome visual acuity assessments using a standardized visual acuity testing protocol, and ocular alignment was measured at each visit.
In conclusion, we found that treatment of strabismic and combined-mechanism amblyopia with spectacles alone resulted in a clinically meaningful improvement in amblyopic eye visual acuity 3 to < 7-year-old children, with nearly one third resolving without the need for additional treatment. Improvement occurred whether or not the spectacles improved ocular alignment. Consideration should be given to prescribing refractive correction as the sole initial treatment for children with strabismic or combined-mechanism amblyopia before initiating other therapy.
Supplementary Material
Acknowledgments
Supported through a cooperative agreement from the National Eye Institute of the National Institute of Health EY011751 and EY018810. The funding organization had no role in the design or conduct of this research.
Footnotes
LensCrafters provided spectacles to some patients at a reduced cost.
No conflicting relationship exists for any author.
The manuscript material was submitted as an abstract paper for presentation at the May 2011 ARVO Annual Meeting. This paper has not been submitted elsewhere for publication.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Stewart CE, Moseley MJ, Fielder AR, Stephens DA, MOTAS Cooperative Refractive adaptation in amblyopia: quantification of effect and implications for practice. Br J Ophthalmol. 2004;88:1552–6. doi: 10.1136/bjo.2004.044214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pediatric Eye Disease Investigator Group. Treatment of anisometropic amblyopia in children with refractive correction. Ophthalmology. 2006;113:895–903. doi: 10.1016/j.ophtha.2006.01.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen PL, Chen JT, Tai MC, et al. Anisometropic amblyopia treated with spectacle correction alone: possible factors predicting success and time to start patching. Am J Ophthalmol. 2007;143:54–60. doi: 10.1016/j.ajo.2006.09.027. [DOI] [PubMed] [Google Scholar]
- 4.Agervi P, Kugelberg U, Kugelberg M, et al. Treatment of anisometropic amblyopia with spectacles or in combination with translucent Bangerter filters. Ophthalmology. 2009;116:1475–80. doi: 10.1016/j.ophtha.2009.02.023. [DOI] [PubMed] [Google Scholar]
- 5.Cotter SA, Edwards AE, Arnold RW, et al. Pediatric Eye Disease Investigator Group Treatment of strabismic amblyopia with refractive correction. Am J Ophthalmol. 2007;143:1060–3. doi: 10.1016/j.ajo.2007.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Awan M, Proudlock FA, Gottlob I. A randomized controlled trial of unilateral strabismic and mixed amblyopia using occlusion dose monitors to record compliance. Invest Ophthalmol Vis Sci. 2005;46:1435–9. doi: 10.1167/iovs.04-0971. [DOI] [PubMed] [Google Scholar]
- 7.Holmes JM, Beck RW, Repka MX, et al. Pediatric Eye Disease Investigator Group The Amblyopia Treatment Study visual acuity testing protocol. Arch Ophthalmol. 2001;119:1345–53. doi: 10.1001/archopht.119.9.1345. [DOI] [PubMed] [Google Scholar]
- 8.Moke PS, Turpin AH, Beck RW, et al. Computerized method of visual acuity testing: adaptation of the Amblyopia Treatment Study visual acuity testing protocol. Am J Ophthalmol. 2001;132:903–9. doi: 10.1016/s0002-9394(01)01256-9. [DOI] [PubMed] [Google Scholar]
- 9.Thibos LN, Wheeler W, Horner D. Power vectors: an application of Fourier analysis to the description and statistical analysis of refractive error. Optom Vis Sci. 1997;74:367–75. doi: 10.1097/00006324-199706000-00019. [DOI] [PubMed] [Google Scholar]
- 10.Miller JM. Clinical applications of power vectors. Optom Vis Sci. 2009;86:599–602. doi: 10.1097/OPX.0b013e3181a6a211. [DOI] [PubMed] [Google Scholar]
- 11.Pediatric Eye Disease Investigator Group. A randomized trial of atropine vs patching for treatment of moderate amblyopia in children. Arch Ophthalmol. 2002;120:268–78. doi: 10.1001/archopht.120.3.268. [DOI] [PubMed] [Google Scholar]
- 12.Stewart CE, Stephens DA, Fielder AR, Moseley MJ, ROTAS Cooperative Objectively monitored patching regimens for treatment of amblyopia: randomised trial [report online] [Accessed May 31, 2011];BMJ. 2007 335:707. doi: 10.1136/bmj.39301.460150.55. Available at: http://www.bmj.com/content/335/7622/707.full.pdf. [DOI] [PMC free article] [PubMed]
- 13.Moseley MJ, Fielder AR, Stewart CE. The optical treatment of amblyopia. Optom Vis Sci. 2009;86:629–33. doi: 10.1097/OPX.0b013e3181a7b3e5. [DOI] [PubMed] [Google Scholar]
- 14.Leske DA, Holmes JM. Maximum angle of horizontal strabismus consistent with true stereopsis. J AAPOS. 2004;8:28–34. doi: 10.1016/j.jaapos.2003.08.010. [DOI] [PubMed] [Google Scholar]
- 15.Pediatric Eye Disease Investigator Group. The course of moderate amblyopia treated with atropine in children: experience of the Amblyopia Treatment Study. Am J Ophthalmol. 2003;136:630–9. doi: 10.1016/s0002-9394(03)00458-6. [DOI] [PubMed] [Google Scholar]
- 16.Pediatric Eye Disease Investigator Group. A randomized trial of atropine regimens for treatment of moderate amblyopia in children. Ophthalmology. 2004;111:2076–85. doi: 10.1016/j.ophtha.2004.04.032. [DOI] [PubMed] [Google Scholar]
- 17.Pediatric Eye Disease Investigator Group Writing Committee. A randomized trial comparing Bangerter filters and patching for the treatment of moderate amblyopia in children. Ophthalmology. 2010;117:998–1004. doi: 10.1016/j.ophtha.2009.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pediatric Eye Disease Investigator Group. A randomized trial of prescribed patching regimens for treatment of severe amblyopia in children. Ophthalmology. 2003;110:2075–87. doi: 10.1016/j.ophtha.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 19.Pediatric Eye Disease Investigator Group. A randomized trial of patching regimens for treatment of moderate amblyopia in children. Arch Ophthalmol. 2003;121:603–11. doi: 10.1001/archopht.121.5.603. [DOI] [PubMed] [Google Scholar]
- 20.Pediatric Eye Disease Investigator Group. Pharmacological plus optical penalization treatment for amblyopia: results of a randomized trial. Arch Ophthalmol. 2009;127:22–30. doi: 10.1001/archophthalmol.2008.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moseley MJ, Neufeld M, McCarry B, et al. Remediation of refractive amblyopia by optical correction alone. Ophthalmic Physiol Opt. 2002;22:296–9. doi: 10.1046/j.1475-1313.2002.00034.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.