Abstract
We are studying the biologic (pseudointimal) lining that forms in the HeartMate (Thermo Cardiosystems, Inc.; Woburn, Massachusetts, USA), a left ventricular assist device with a pusher-plate blood pump, housed in solid titanium with uniquely textured blood-contacting surfaces. Sintered titanium microspheres cover the rigid surface, and integrally textured polyurethane lines the flexing diaphragm. The texture of the blood-contacting surfaces is designed to encourage formation of a biologic pseudointimal lining, which greatly reduces the risk of thromboembolic complications. We performed immunochemical analyses to characterize precisely the pseudointimal lining. Samples were taken from 2 explanted pumps; 1 had supported a patient for 132 days and the other, 189 days. The samples were cultured to detect factor-VIII-related antigen (von Willebrand factor), acetyl low-density lipoprotein receptors, smooth-muscle-cell actin, and surface adhesion molecules specific for monocytes/macrophages. Macrophage cells were predominant in both pumps, but in the 2nd pump, cultures from the center of the diaphragm were positive for acetyl low-density lipoprotein receptor and von Willebrand factor, indicating the presence of endothelial cells. We believe that blood-borne endothelial cells or endothelial cell precursors were deposited on the blood-contacting surfaces, which is an important clinical finding with regard to lowering the risk of thromboembolic complications and reducing the need for systemic anticoagulation in long-term left ventricular assist device patients.
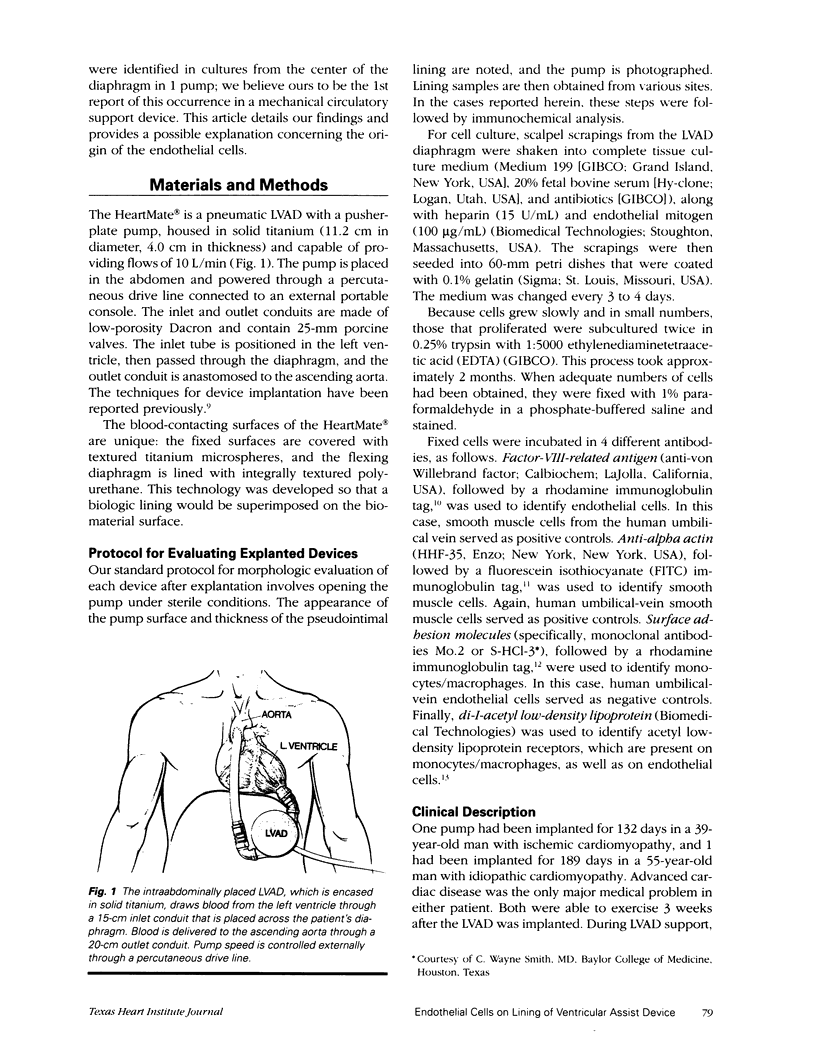
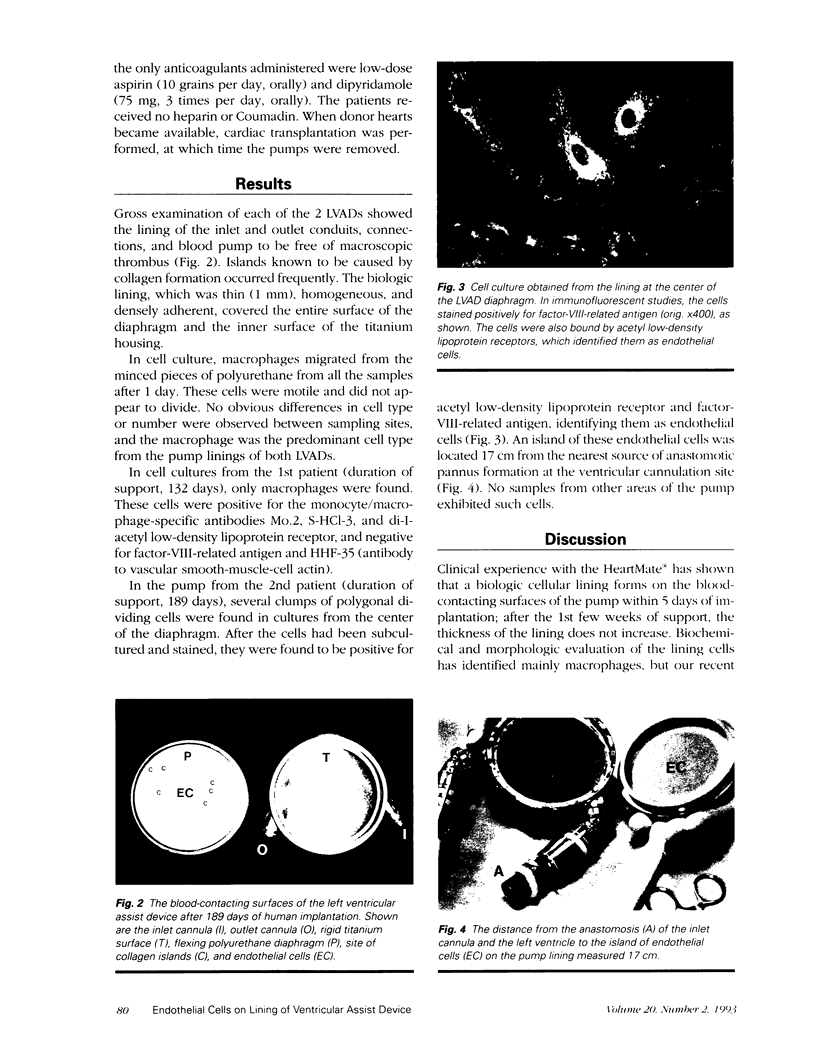
Full text
PDF


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Berger K., Sauvage L. R., Rao A. M., Wood S. J. Healing of arterial prostheses in man: its incompleteness. Ann Surg. 1972 Jan;175(1):118–127. doi: 10.1097/00000658-197201000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brieler H. S., Thiede A., Beck C. Monocytogenic endothelialization in dacron grafts. Experimental studies on rats. J Cardiovasc Surg (Torino) 1982 Nov-Dec;23(6):483–489. [PubMed] [Google Scholar]
- Clowes A. W., Kirkman T. R., Reidy M. A. Mechanisms of arterial graft healing. Rapid transmural capillary ingrowth provides a source of intimal endothelium and smooth muscle in porous PTFE prostheses. Am J Pathol. 1986 May;123(2):220–230. [PMC free article] [PubMed] [Google Scholar]
- FLOREY H. W., GREER S. J., KISER J., POOLE J. C., TELANDER R., WERTHESSEN N. T. The development of the pseudointima lining fabric grafts of the aorta. Br J Exp Pathol. 1962 Dec;43:655–660. [PMC free article] [PubMed] [Google Scholar]
- Frazier O. H., Duncan J. M., Radovancevic B., Vega J. D., Baldwin R. T., Burnett C. M., Lonquist J. L. Successful bridge to heart transplantation with a new left ventricular assist device. J Heart Lung Transplant. 1992 May-Jun;11(3 Pt 1):530–537. [PubMed] [Google Scholar]
- Ghani A. R., Tibbs D. J. Role of Blood-borne Cells in Organization of Mural Thrombi. Br Med J. 1962 May 5;1(5287):1244–1238.1. doi: 10.1136/bmj.1.5287.1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham L. M., Vinter D. W., Ford J. W., Kahn R. H., Burkel W. E., Stanley J. C. Endothelial cell seeding of prosthetic vascular grafts: early experimental studies with cultured autologous canine endothelium. Arch Surg. 1980 Aug;115(8):929–933. doi: 10.1001/archsurg.1980.01380080025005. [DOI] [PubMed] [Google Scholar]
- Graham T. R., Dasse K., Coumbe A., Salih V., Marrinan M. T., Frazier O. H., Lewis C. T. Neo-intimal development on textured biomaterial surfaces during clinical use of an implantable left ventricular assist device. Eur J Cardiothorac Surg. 1990;4(4):182–190. doi: 10.1016/1010-7940(90)90002-h. [DOI] [PubMed] [Google Scholar]
- Greisler H. P. Arterial regeneration over absorbable prostheses. Arch Surg. 1982 Nov;117(11):1425–1431. doi: 10.1001/archsurg.1982.01380350029005. [DOI] [PubMed] [Google Scholar]
- Greisler H. P., Kim D. U., Price J. B., Voorhees A. B., Jr Arterial regenerative activity after prosthetic implantation. Arch Surg. 1985 Mar;120(3):315–323. doi: 10.1001/archsurg.1985.01390270055010. [DOI] [PubMed] [Google Scholar]
- Greisler H. P., Schwarcz T. H., Ellinger J., Kim D. U. Dacron inhibition of arterial regenerative activities. J Vasc Surg. 1986 May;3(5):747–756. [PubMed] [Google Scholar]
- JORDAN G. L., Jr, STUMP M. M., DE BAKEY M. E., HALPERT B. Endothelial lining of dacron prostheses of porcine thoracic aortas. Proc Soc Exp Biol Med. 1962 Jun;110:340–343. doi: 10.3181/00379727-110-27510. [DOI] [PubMed] [Google Scholar]
- Mackenzie J. R., Hackett M., Topuzlu C., Tibbs D. J. Origin of arterial prosthesis lining from circulating blood cells. Arch Surg. 1968 Dec;97(6):879–885. doi: 10.1001/archsurg.1968.01340060057005. [DOI] [PubMed] [Google Scholar]
- McGee M. G., Parnis S. M., Nakatani T., Myers T., Dasse K., Hare W. D., Duncan J. M., Poirier V. L., Frazier O. H. Extended clinical support with an implantable left ventricular assist device. ASAIO Trans. 1989 Jul-Sep;35(3):614–616. doi: 10.1097/00002480-198907000-00145. [DOI] [PubMed] [Google Scholar]
- Miller L. J., Schwarting R., Springer T. A. Regulated expression of the Mac-1, LFA-1, p150,95 glycoprotein family during leukocyte differentiation. J Immunol. 1986 Nov 1;137(9):2891–2900. [PubMed] [Google Scholar]
- Nomura Y. The ultra-structure of the pseudointima lining synthetic arterial grafts in the canine aorta with special reference to the origin of the endothelial cell. J Cardiovasc Surg (Torino) 1970 Jul-Aug;11(4):282–291. [PubMed] [Google Scholar]
- POOLE J. C., SABISTON D. C., Jr, FLOREY H. W., ALLISON P. R. Growth of endothelium in arterial prosthetic grafts and following endarterectomy. Surg Forum. 1962;13:225–227. [PubMed] [Google Scholar]
- STUMP M. M., JORDAN G. L., Jr, DEBAKEY M. E., HALPERT B. ENDOTHELIUM GROWN FROM CIRCULATING BLOOD ON ISOLATED INTRAVASCULAR DACRON HUB. Am J Pathol. 1963 Sep;43:361–367. [PMC free article] [PubMed] [Google Scholar]
- Sauvage L. R., Berger K. E., Wood S. J., Yates S. G., 2nd, Smith J. C., Mansfield P. B. Interspecies healing of porous arterial prostheses: observations, 1960 to 1974. Arch Surg. 1974 Nov;109(5):698–705. doi: 10.1001/archsurg.1974.01360050092020. [DOI] [PubMed] [Google Scholar]
- Sauvage L. R., Berger K., Beilin L. B., Smith J. C., Wood S. J., Mansfield P. B. Presence of endothelium in an axillary-femoral graft of knitted Dacron with an external velour surface. Ann Surg. 1975 Dec;182(6):749–753. doi: 10.1097/00000658-197512000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skalli O., Ropraz P., Trzeciak A., Benzonana G., Gillessen D., Gabbiani G. A monoclonal antibody against alpha-smooth muscle actin: a new probe for smooth muscle differentiation. J Cell Biol. 1986 Dec;103(6 Pt 2):2787–2796. doi: 10.1083/jcb.103.6.2787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voyta J. C., Via D. P., Butterfield C. E., Zetter B. R. Identification and isolation of endothelial cells based on their increased uptake of acetylated-low density lipoprotein. J Cell Biol. 1984 Dec;99(6):2034–2040. doi: 10.1083/jcb.99.6.2034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WESOLOWSKI S. A., SAUVAGE L. R. Comparison of the fates of orlon mesh prosthetic replacement of the thoracic aorta and aortic bifurcation. Ann Surg. 1956 Jan;143(1):65–72. doi: 10.1097/00000658-195601000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]