Abstract
Three cases of immune thrombocytopenia (ITP) associated with human immunodeficiency virus (HIV) infection prompted a review of community-acquired thrombocytopenia in Nova Scotia from January 1980 to December 1987. Two hundred and seven patients meeting the case definition of ITP were identified. The incidence of ITP rose from 2.0×105 in 1980 to 3.3×105 in 1987. More cases of ITP in the sexually active population occurred between 1984 and 1987 than in the previous four years (P=0.034). All three cases of known HIV associated ITP were captured in the retrospective surveillance system. The study concluded that increases in community-acquired ITP in a sexually active population may be a surrogate marker of the HIV epidemic, even in geographic areas with a low seroprevalence for HIV. Serological tests for HIV infection should be a routine part of the diagnostic investigation of ITP in all sexually active patients or those with other potential risk factors for HIV infection.
Keywords: Epidemiology, Human Immunodeficiency virus, Immune thrombocytopenia
RÉSUMÉ:
Trois cas de thrombocytopénie immune associée au virus de l’immunodéficience humaine (VIH) ont conduit les chercheurs à passer en revue les cas de thrombocytopénie acquise en Nouvelle-Écosse entre janvier 1980 et décembre 1987. Deux cent sept patients ont été identifiés porteurs d’une thrombocytopénie immune. L’incidence de thrombocytopénie immune s’est élevée de 2.0 × 105 en 1980 à 3,3 × 105 en 1987. Plus de cas de thrombocytopénie immune dans la population active sexuellement sont survenus entre 1984 et 1987 que dans les quatre années précédentes (p=0.034). Les trois cas de thrombocytopénie immune associée au VIH ont été décelés par un système de contrôle épidémiologique rétrospectif. L’étude a conclu que l’augmentation du nombre de cas de thrombocytopénie immune dans une population active pourraient constituer un indicateur substitut d’une épidémie au VIH, même dans les zones géographiques où la séroprévalence du VIH est faible. Les tests sérologiques pour l’infection au VIH doivent faire partie intégrale de la recherche diagnostique dans la thrombocytopénie immune chez tous les patients actifs sexuellement ou chez ceux qui présentent un autre facteur de risque à l’égard de l’infection au VIH.
Immune thrombocytopenia (itp) first was reported as a manifestation of the human immunodeficiency virus (HIV) epidemic in 1982 (1) and now is recognized widely as a common manifestation of acute and chronic HIV infection (2). Estimates of thrombocytopenia in human subjects of known HIV seropositive cohorts are as high as 10% at a single visit (3), and thrombocytopenia has been reported in all risk groups for HIV infection (3–7). However no studies of community-acquired ITP exist that would allow a direct comparison of the incidence of ITP in HIV infection versus that in the general population. Three cases of HIV-related ITP diagnosed in Nova Scotia prompted a study of the incidence of ITP in that province. The hypothesis was that the incidence of ITP – a relatively uncommon hematological condition but a common manifestation of HIV infection – would be increasing as an epiphenomenon of the spread of HIV infection in the community.
CASE PRESENTATIONS
Case 1:
A 22-year-old heterosexual female noted easy bruising and increased menstrual bleeding during September 1984. She was admitted in November 1984 with a platelet count of 13,000/mm3. White blood cell count was 4800/mm3 with a normal differential. A bone marrow examination demonstrated normal megakaryocytes, antinuclear antibody and anti-DNA and lupus erythematosis tests were negative. A diagnosis of ITP was made and the patient was treated with platelet transfusions and prednisone (100 mg daily); a rapid resolution of thrombocytopenia resulted. In September 1985 a human T cell lymphotrophic virus (HTVL)-III titre was positive by enzyme immunoassay and Western blot. The patient remained asymptomatic (Centers for Disease Control [CDC] group II) with a CD4 count of 500 in July 1989. The patient’s only sexual partner in 1984 had hemophilia A and had referred her for evaluation after finding out that her was HTLV-III positive. In July 1989 the partner had CDC group III HIV infection with a CD4 count of 300.
Case 2:
A 26-year-old male developed easy bruising in January 1985 and in July of that year was found to be thrombocytopenic. He was hospitalized in September 1985 with a platelet count of 67,000/mm3 because of failure to maintain an adequate platelet count while off prednisone. Total white blood cell count was 13,300/mm3 and the differential count was normal. A bone marrow aspirate revealed megakaryocytic hyperplasia, confirming the diagnosis of ITP. The patient was treated with vinblastine, and prednisone was continued. The thrombocytopenia resolved over six months. An HTLV-III titre was positive in September 1985. Other studies were not done. The patient had a single homosexual relationship two years prior to presentation while attending university in central Canada. There were no other risk factors for HIV infection.
Case 3:
A 25-year-old homosexual male developed a widespread petechial rash and bleeding of the gums in April 1986. He had a positive HTLV-III antibody test, a platelet count of 8000/mm3 and a white blood cell count of 7600/mm3 with 25% atypical lymphocytes. The patient was hepatitis B surface antigen-positive and had a cytomegalovirus titre of 1:256 and a herpes simplex virus titre of 1:64. Bone marrow examination showed megakaryocytic hyperplasia, CD4 count was 480, and immunoglobulin (Ig) G level was 28.3 (normal 6.9 to 18.0). IgA 4.2 (0.9 to 4.0) and IgM 4.1 (0.6 to 3.6). A diagnosis of HTLV-III-associated ITP was made. Treatment with 100 mg prednisone daily resulted in rapid resolution of thrombocytopenia.
Case ascertainment:
Medical records at all Halifax hospitals were reviewed for ICD-9 codes 287.3 (primary thrombocytopenia), 287.4 (secondary thrombocytopenia) and 287.5 (thrombocytopenia, unspecified). A diagnosis of ITP was based on a platelet count of 120,000/mm3 or less on two determinations with evidence of peripheral destruction and no underlying explanatory disease or condition such as drug use, alcohol abuse, liver disease or other autoimmune diseases. Bone marrow examination was performed in all cases. Immune complex determinations, antiplatelet antibody and specific platelet-bound Ig determinations were not routinely performed. Cases meeting the case definition with dates of diagnosis between 1980 and 1987 were abstracted for demographic information including age. sex, date of onset, county of residence, initial platelet count, treatment regimen, HIV risk factors and out-come. Office records of all hematologists in Nova Scotia were reviewed and a mailing to internists and pediatricians soliciting cases of ITP was carried out. Consultations with hematologists and general practitioners in the province suggested that cases of suspected ITP would routinely be referred to practising hematologists (all located in Halifax) or internists by primary care physicians, and that review of office and hospital records of these specialists only would not significantly underestimate the number of ITP cases.
Nova Scotia census data obtained in 1980 with population projections through 1987 were used to establish ITP incidence by year. No attempt was made to contact patients identified during the survey to determine risk factors for HIV infection or to determine whether serological evaluation for HIV would be warranted.
RESULTS
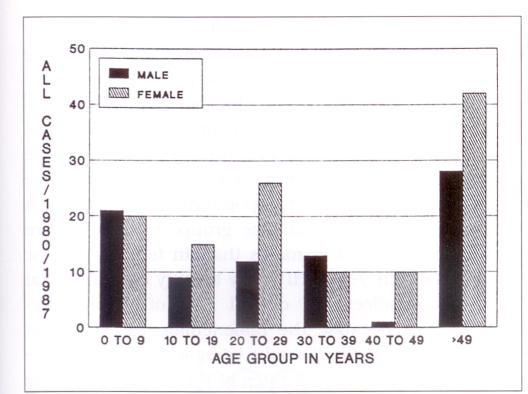
Two hundred and seven cases of ITP were identified between January 1980 and December 1987 in Nova Scotia. Ages ranged from one month to 93 years, with 86 cases occurring in males and 121 in females (male: female ratio 1:1.4). The age distribution of reported cases is illustrated in Figure 1.
Figure 1.
Total number (n=207) of cases of immune thrombocytopenia in Nova Scotia by age group and sex from 1980 to 1987. The overall pattern shows higher incidences in the groups aged zero to nine and over 49
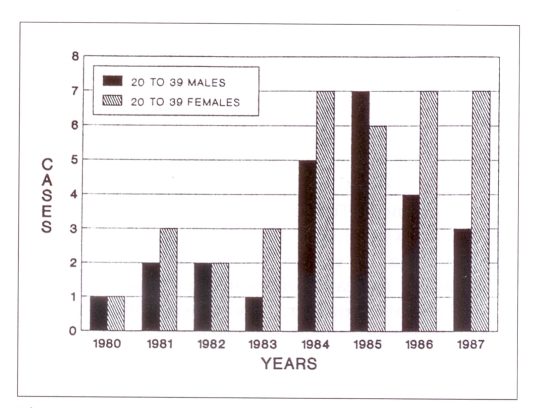
Rates of ITP per 100,000 population were determined in each of the age groups (Table 1). In the first four years of the survey (1980–83), rates were highest in the first decade of life and in patients over 49 years of age. Rates did not significantly change for these groups during the last four years of the survey (1984–87). Between 1984 and 1987. rates of ITP for the second through fourth decades of life significantly increased (P=0.034) (χ2 test = 1.9 [confidence interval 1.1 to 3.6]). For the age group presumed to be most sexually active (ages 20 to 39), the increase was even more striking (P=0.002) (χ2 test = 2.9 [confidence interval 1.4 to 6.0]) (Figure 2). There was little change in the male:female ratio between the two time periods in this group although in the 30- to 39-year-old group, the ratio changed from 1:1 to 0.7:1 in favour of males. .All three cases of known HIV-related ITP described above were in this age group and were identified during the retrospective surveillance. Cases were reported from Nova Scotia’s 18 counties with no differences in ITP rates between counties. There were 14 deaths, for a case fatality rate of 6.8%. No deaths were due to possible HIV-related conditions.
TABLE 1.
Rates of immune thrombocytopenia per 100,000 population
| Age group | 1980 | 1981 | 1982 | 1983 | 1984 | 1985 | 1986 | 1987 |
|---|---|---|---|---|---|---|---|---|
| 0 to 9 | 3.8 | 1.5 | 3.8 | 6.8 | 4.5 | 4.5 | 3.7 | 2.9 |
| 10 to 19 | 0.6 | 1.3 | 3.2 | 1.3 | 1.4 | 2.1 | 2.1 | 4.3 |
| 20 to 29 | 1.3 | 1.9 | 2.5 | 1.2 | 4.3* | 3.7* | 3.6* | 4.8* |
| 30 to 39 | 0.0 | 1.6 | 0.0 | 0.7 | 3.6* | 4.8* | 3.3* | 1.3* |
| 40 to 49 | 2.4 | 0.0 | 2.3 | 2.2 | 1.1 | 0.0 | 3.1 | 1.0 |
| > 49 | 3.4 | 3.4 | 4.8 | 4.8 | 3.8 | 3.3 | 5.1 | 4.2 |
| Mean | 2.0 | 1.9 | 3.0 | 3.1 | 3.3 | 3.5 | 3.7 | 3.3 |
Rates significantly different from previous four years (P=0.002) (χ2 test for trend = 2.9 (confidence interval 1.4 to 6.0)
Figure 2.
Immune thrombocytopenia (ITP) cases for the group aged 20 to 39 by year of diagnosis. The increase in ITP between 1984 and 1987 is significant (P=0.002, χ2 test for trend). Numbers did not significantly change for the groups aged zero to nine and over 49. There was a reversal in the male:female ratio in 1985, but not in subsequent years
DISCUSSION
Before the identification of the causative agent of acquired immune deficiency syndrome (aids), surrogate markers of HIV infection – such as Pneumocystis carinii pneumonia (8) and Kaposi’s sarcoma (9) – identified groups of patients subsequently determined to have HIV infection. These conditions primarily are seen in immunosuppressed hosts and reflect advanced disease. The epidemiology of tuberculosis, which can occur in both normal and immunosuppressed patients, has clearly been affected by the spread of HIV infection, with increased rates of tuberculosis occurring in hyper-endemic areas for HIV infection (10). The present authors postulated that another potential marker for HIV infection in a community may be an increase in ITP, a common and often early manifestation of HIV infection.
Previous studies of community-acquired ITP have not been reported. The province of Nova Scotia provided a unique opportunity to perform a retrospective study of ITP incidence because of the referral patterns for this condition.
The population of Nova Scotia has been relatively stable, growing from 850,000 to 900,000 during the period of the present study. Access to health care is excellent, with regular and rapid referral to consultants for uncommon disorders. The first case of aids in a Nova Scotia resident was identified in 1983; 72 cases have been reported to December 1990 with a peak incidence in 1987 of 1.8 per 100,000 population. The incidence and prevalence of HIV infection in the province is unknown, although mandatory reporting requirements for HIV infection are in place. Cross-matching ITP files with reported aids cases did not produce additional cases of ITP or aids.
The study supports the hypothesis that increases in the ITP rate in sexually active age groups may parallel the spread of HIV infection. Automated platelet counts were introduced before and during the survey, and although they may report artefactually low platelet counts, this would not account for the differences in rates seen between age groups. In addition, all patients identified in the survey had clinical findings (easy bruising or petechia) resulting in referral for diagnosis and management. The mean platelet count at onset for the patients was 13,000/mm3. Increased availability of automated platelet counts therefore seems an unlikely bias towards increased rates in the study’s last four years. The data, however, may underestimate asymptomatic thrombocytopenia, of which some cases may be due to immune thrombocytopenia associated with HIV infection.
Changes in referral patterns with increased availability of hematological or internal medicine consultations could also account for increased recognition in the latter part of the survey. However, this bias would be reflected in increased rates of ITP in all age groups; clinically significant thrombocytopenia should not have been systematically under-reported in any age group in the study’s first four years. Increased reporting of known HIV-related ITP did not occur, and cases 1 and 2 were recognized only in retrospect after epidemiological risk factors for HIV infection were ascertained. Despite this delayed diagnosis, all three cases of known HIV-related ITP were captured in the survey.
Rates of ITP did not differ between counties for any study period, and disproportionate cases of aids have not been reported from Halifax county, the major urban centre in the province with 30% of the total population. (Nova Scotia may be atypical in that respect, compared with other Canadian provinces, as two of the three ITP cases cited in this report were not from Halifax county.) The authors believe that referral patterns did not significantly change between 1980–83 and 1984–87, making it likely that changes in ITP rates represent true changes in the incidence of disease in the community.
HIV infection in Nova Scotia has been seen principally in homosexual men (85% of reported aids cases). The authors expected a change over time in the male:female ratio for ITP in sexually active age groups. This change was not noted in the overall population, but was seen in the 30- to 39-year-old age group, in which more cases were reported in males than in females for the study’s last four years. HIV may be only one of several factors that affect the overall rate of community-acquired ITP because the male:female ratio did not change dramatically. It might be easier to identify the effect of HIV infection on rates of ITP and male:female ratio change in areas of high prevalence. The authors are unaware of similar studies to support the conclusion that ITP cases may be surrogate markers for HIV transmission, although anecdotal case reports and case series show a male predominance in HIV-positive ITP patients.
The study provided support for the outlined hypothesis but other population-based studies of ITP in areas of both high and low HIV prevalence are needed for confirmation. Review of ITP’s clinical features in the chart review of patients in the sexually active age group supports the hypothesis: cases of ITP exhibited the typical chronic, autoimmune form of ITP reported in HIV-positive patients. Independent confirmation through serological investigation of the cases would have strengthened the observation but would have been intrusive. However the authors recommend, on the basis of the study, that serological tests for HIV infection should be a routine part of the diagnostic investigation of ITP, particularly in age groups that are likely to be sexually active.
Acknowledgments
The authors are grateful to Drs Ormille Hayne, Vincent Ing, G Ross Langley and Allan Pysemany for access to patient records for review, and to the physicians in Nova Scotia who responded to the survey. The authors also thank Daureen Stover and Janice Flynn for preparation of the manuscript.
REFERENCES
- 1.Morris L, Distenfeld A, Amorosi E, Karpatkin S. Autoimmune thrombocytopenia in homosexual men. Ann Intern Med. 1982;96:714–7. doi: 10.7326/0003-4819-96-6-714. [DOI] [PubMed] [Google Scholar]
- 2.Ratner L. Human immunodeficiency virus-associated autoimmune thrombocytopenic purpura: A review. Am J Med. 1989;86:194–8. doi: 10.1016/0002-9343(89)90268-4. [DOI] [PubMed] [Google Scholar]
- 3.Kaslow RA, Phair JP, Freedman HB, et al. Infection with the human immunodeficiency virus: Clinical manifestations and their relationship to immune deficiency. A report of the multicenter aids cohort study. Ann Intern Med. 1987;107:474–80. doi: 10.7326/0003-4819-107-4-474. [DOI] [PubMed] [Google Scholar]
- 4.Savona S, Nardi MA, Lennette ET, Karpatkin S. Thrombocytopenic purpura in narcotics addicts. Ann Intern Med. 1985;102:737–41. doi: 10.7326/0003-4819-102-6-737. [DOI] [PubMed] [Google Scholar]
- 5.Ratnoff OD, Menitove JE. Aster RH, Lederman MM. Coincident classic hemophilia and ‘idiopathic’ thrombocytopenic purpura in patients under treatment with concentrates of antihemophiliac (factor VIII) N Engl J Med. 1983;308:439–42. doi: 10.1056/NEJM198302243080808. [DOI] [PubMed] [Google Scholar]
- 6.Saulsbury TJ, Boyle RJ, Wykoff RF, Howard TH. Thrombocytopenia as the presenting manifestation of human T-lymphotropic virus type III infection in infants. J Pediatr. 1986;109:30–4. doi: 10.1016/s0022-3476(86)80567-4. [DOI] [PubMed] [Google Scholar]
- 7.Karpatkin S, Nardi MA, Hymes KB. Immunologic thrombocytopenic purpura after heterosexual transmission of human immunodeficiency virus (HIV) Ann Intern Med. 1988;109:190–3. doi: 10.7326/0003-4819-109-3-190. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control Pneumocystis pneumonia –Los Angeles. MMWR. 1981;30:250–2. [PubMed] [Google Scholar]
- 9.Centers for Disease Control Update on Kaposi’s sarcoma and pneumocystis pneumonia among homosexual men – New York City and California. MMWR. 1981;30:305–8. [PubMed] [Google Scholar]
- 10.Centers for Disease Control Tuberculosis – United States, 1985 – and the possible impact of human T-lymphotropic virus type III/lymphadenopathy associated virus infections. MMWR. 1986;35:74–6. [PubMed] [Google Scholar]