A seven-year-old black boy born in Canada with perinatally acquired human immunodeficiency virus (HIV) infection presented with recurrent nausea, diarrhea and intolerance of gastric tube feeding. Additionally, there was a history of a 3 kg weight loss over the two weeks before admission and a history of persistent fatigue over the four weeks before admission.
Significant past medical history revealed cytomegalic virus (CMV)-retinitis diagnosed and treated three months previously, chronic sinusitis and moderate HIV encephalopathy. Approximately three months before admission, his CD4 count was 41/mm3, and his viral load was 4.6 log10 HIV RNA copies/mL of plasma. His medications included stavudine, lamivudine, saquinovir, granulocyte colony-stimulating factor, clarithromycin, fluconazole, intravenous ganciclovir, and monthly pentamidine and immune globulin.
On physical examination, he was a thin boy in the 25th percentile for weight. He was afebrile. His examination was remarkable for the absence of oral candidiasis, the presence of diffuse palpable lymph nodes less than 0.5 cm in the cervical, axillary and inguinal areas, and the absence of skin lesions. His abdominal exam revealed no masses, no tenderness and a palpable nontender liver edge 1 cm below the costal margin.
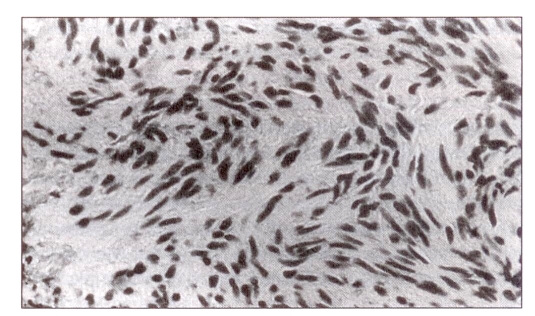
Blood for CMV polymerase chain reaction (PCR) was positive, while Epstein-Barr virus (EBV) PCR was negative; EBV serology (immunoglobulin [Ig] G) for capsid antigen was positive; EBV IgM was negative. A chest radiograph was normal. Examination of the stool was positive for adenovirus but negative for Clostridium difficile toxin, ova and parasites. Gastric and colonic biopsies were negative for parasites, mycobacteria or viral changes. An ultrasound of the liver demonstrated two well defined hypoechoic liver lesions, each measuring approximately 13 mm, located in the right lobe of the liver. A fine needle aspiration of one of the hepatic lesions was performed (Figure 1).
Figure 1.
Cytology (Papanicolaou stain) from fine needle aspiration of liver lesion
What is your diagnosis?
DIAGNOSIS
The pathologist reported fragments of spindled cells without significant pleomorphism of mitotic activity and the absence of granulomata (Figure 1). Specific stains for actin, myosin and desmin supported the cell of origin as smooth muscle and the diagnosis of a leiomyoma. No intervention was undertaken, and the lesion was monitored with serial ultrasounds. An ultrasound performed three months after the initial diagnosis revealed no change in one lesion and slow growth of the second lesion to 17 mm. Blood was positive for EBV PCR at that time. His antiretroviral regimen was changed to lamivudine, stavudine and ritonavir, resulting in improvement of his gastrointestinal symptoms, significant weight gain, modest improvement of his CD4 count to 247/mm3 and decline of HIV viral load to less than 2.2 log10 HIV RNA copies/mL of plasma.
DISCUSSION
The incidence of neoplasms is increased in all individuals with HIV infection, although this incidence is lower in children than adults. Arico et al (1) reported a 2% to 8% prevalence of malignancies in a series of children perinatally affected with HIV. The most common neoplasm in pediatric HIV and other immunodeficiency states is lymphoma (2).
Leiomyomata and leiomyosarcomata are very rare in normal children, with an estimated incidence of the latter of less than 1.6 per 10 million children (3). Conversely, children with HIV have an unusually high incidence of these benign and malignant tumours of smooth muscle. These tumours most commonly are found in the lungs, spleen and gastrointestinal tract (4).
EBV has been implicated as an etiological agent in leiomyomata and leiomyosarcomata in children with HIV. McClain et al (5) compared tissues from two leiomyomata and five leiomyosarcomata from five children and one young adult with HIV against samples of similar lesions from HIV-negative children. EBV genomes were present in all samples from HIV-infected individuals by in situ hybridization and EBV PCR, while EBV DNA was absent from specimens from HIV-negative patients. The therapy for malignant lesions includes surgery, chemotherapy, interferon-alpha and radiation therapy, although despite therapy these lesions tend to recur.
Tumours of smooth muscle should be included in the differential diagnosis of space occupying lesions of the liver, gut, spleen and lung in pediatric patients with HIV infection.
REFERENCES
- 1.Arico M, Castili D, D’argenio PD, et al. Malignancies in children with human immunodeficiency virus type 1 infection. Cancer. 1991;68:2373. doi: 10.1002/1097-0142(19911201)68:11<2473::aid-cncr2820681125>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 2.Filipovich A. Lymphoproliferative disorders associated with immunodeficiency. In: Magrath IT, editor. The Non-Hodgkin’s Lymphomas. London: Edward Arnold; 1990. p. 135. [Google Scholar]
- 3.Chadwick EG, Connor EJ, Hanson CG, et al. Tumours of smooth-muscle origin in HIV-infected children. JAMA. 1990;263:3182–4. [PubMed] [Google Scholar]
- 4.McClain KL, Joshi VV, Murphy SB. Cancers in children with HIV infection. Hematol Oncol Clin North Am. 1996;10:1189–201. doi: 10.1016/s0889-8588(05)70393-2. 5: [DOI] [PubMed] [Google Scholar]
- 5.McClain KL, Leach CT, Jenson HB, et al. Association of Epstein-Barr virus with leiomyosarcomas in young people with AIDS. N Engl J Med. 1995;332:12–8. doi: 10.1056/NEJM199501053320103. [DOI] [PubMed] [Google Scholar]