Abstract
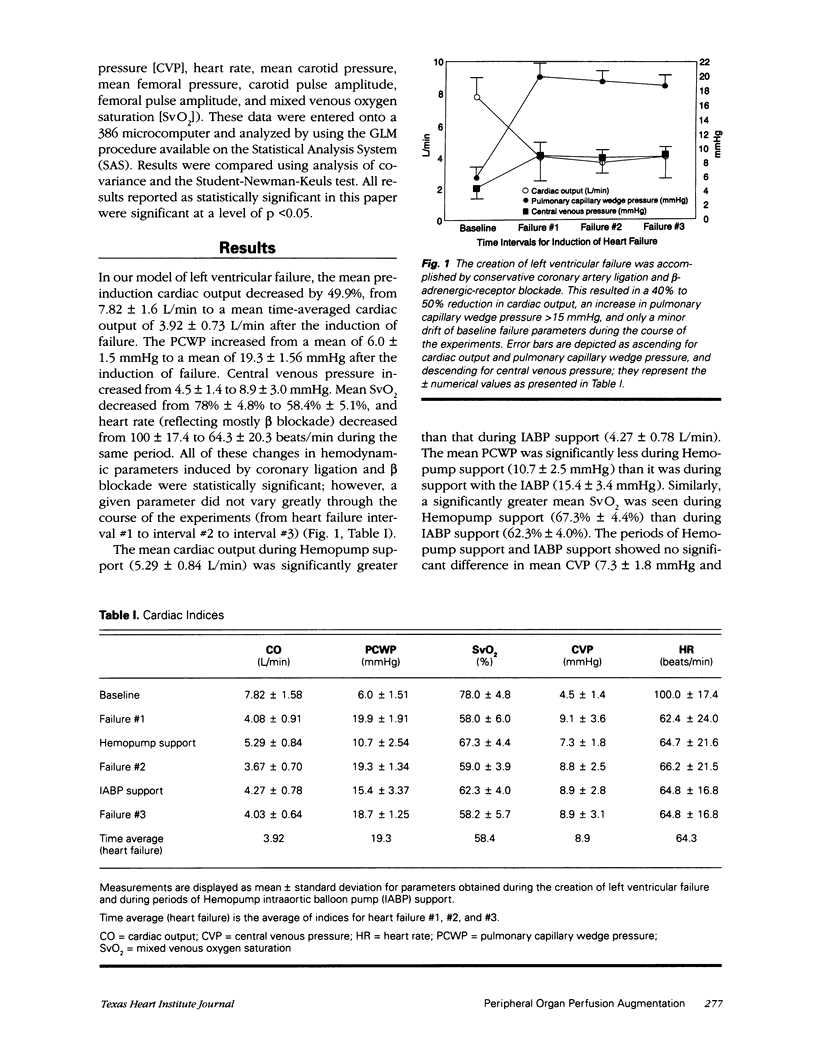
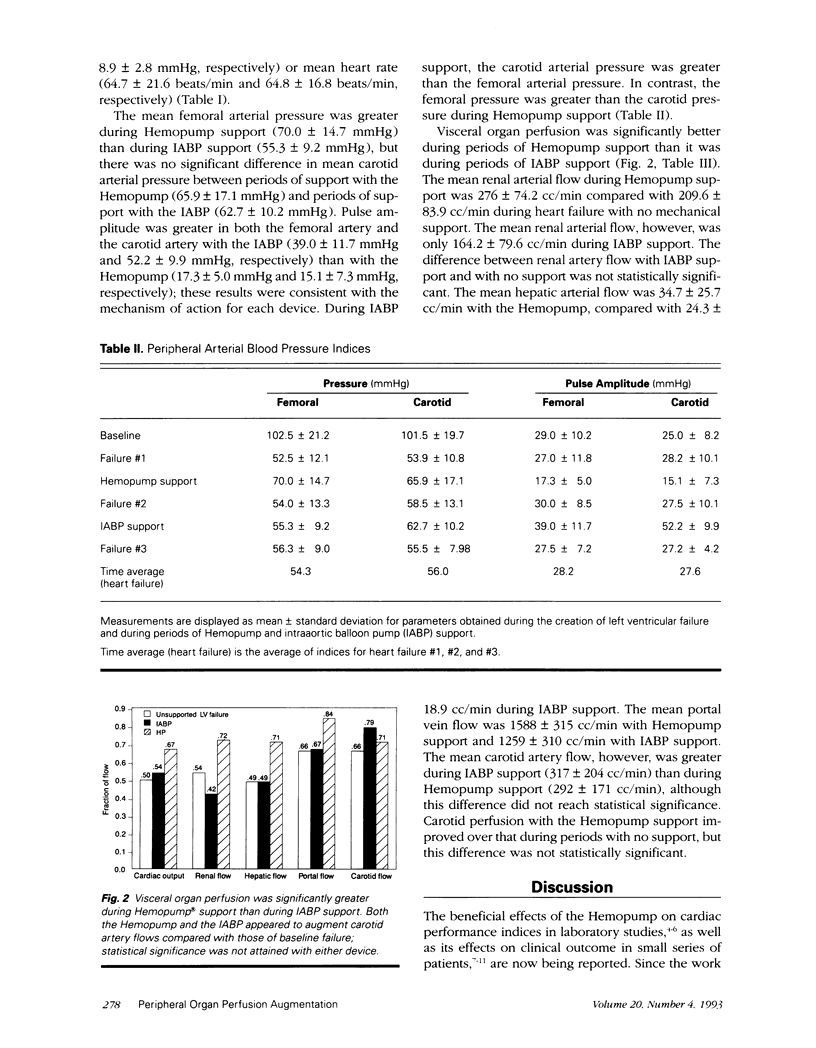
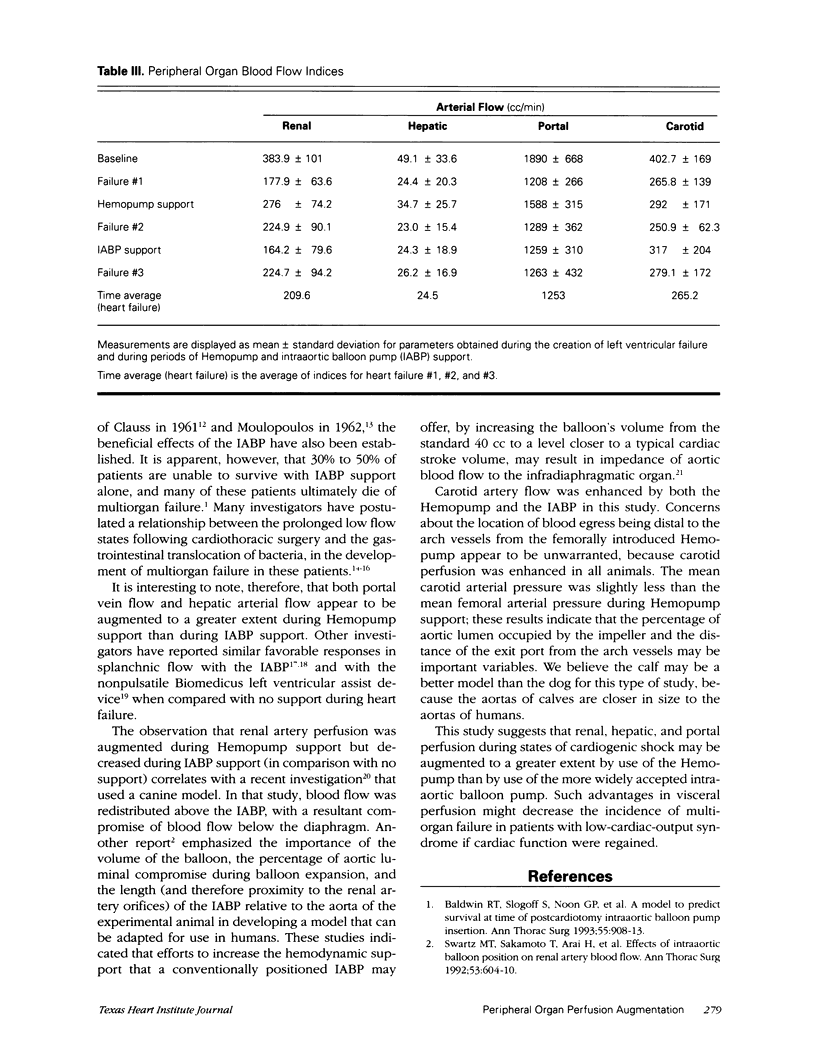
Despite the use of inotropic therapy and the intraaortic balloon pump (IABP), inadequate peripheral organ perfusion and subsequent multiorgan failure from left ventricular dysfunction is a major cause of death following cardiac surgery. To compare the end-organ perfusion provided by the IABP with that of the recently developed Hemopump Cardiac Assist System, blood flow from visceral organs was measured by ultrasonic flow probes during separate periods of support with each of these pumps. Ten calves underwent coronary artery ligations with beta-receptor blockade; hemodynamic parameters were recorded before the induction of failure, during unsupported cardiac failure, and during Hemopump and IABP support. Improvement in mean cardiac output, mixed venous oxygen saturation, and pulmonary artery wedge pressure was significantly greater (p < 0.05) during Hemopump support than during IABP support. Renal artery flow was significantly greater during Hemopump support (276 +/- 74.2 cc/min) than during IABP support (164 +/- 79.6 cc/min). Hepatic artery flow was significantly greater during Hemopump support (34.7 +/- 25.7 cc/min) than during IABP support (24.4 +/- 18.9 cc/min), and portal vein flow was significantly greater during Hemopump support (1588 +/- 315 cc/min) than IABP support (1259 +/- 310 cc/min). There were no significant differences, however, between carotid artery flow during Hemopump support (292 +/- 171 cc/min) and that during IABP support (317 +/- 204 cc/min). We conclude that renal, hepatic, and mesenteric perfusion provided by the nonpulsatile Hemopump is superior to that of the IABP in this bovine model of left ventricular failure. Therefore, the Hemopump may be more effective in preventing multiorgan failure during recovery of ventricular function.
Full text
PDF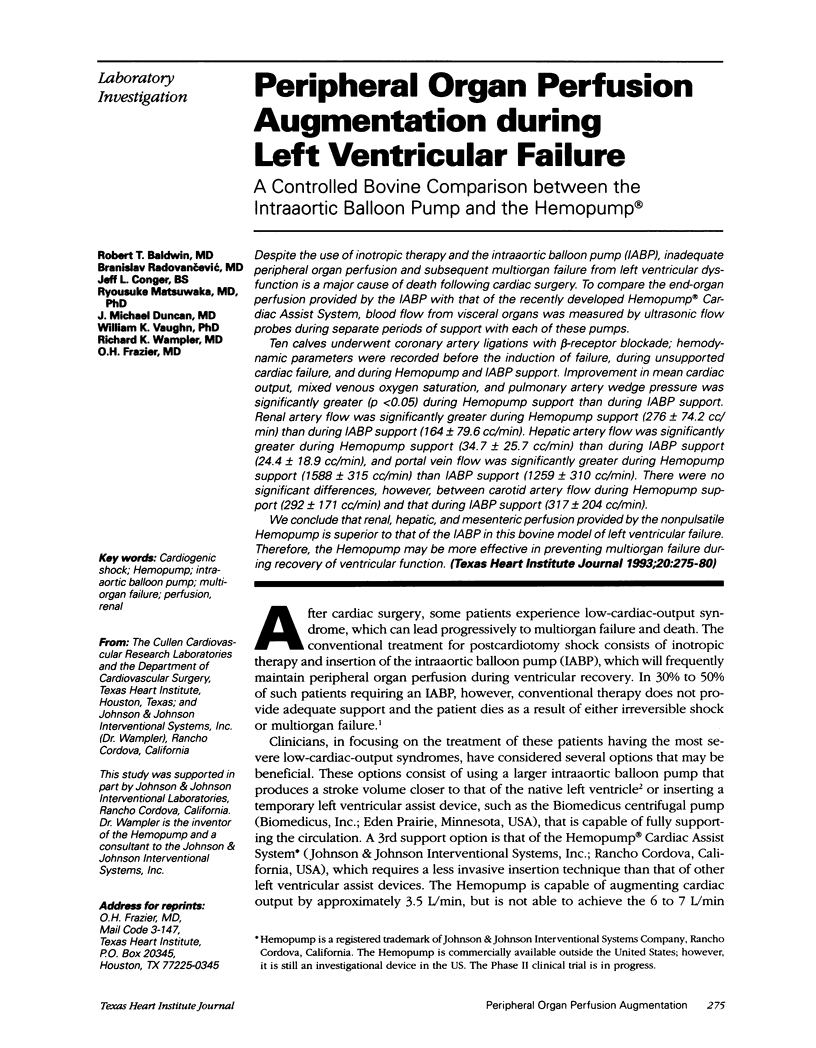


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baldwin R. T., Radovancevic B., Duncan J. M., Ford S., Lonquist J. L., Munoz E., Abou-Awdi N. L., Frazier O. H. Quality of life in long-term survivors of the Hemopump left ventricular assist device. ASAIO Trans. 1991 Jul-Sep;37(3):M422–M423. [PubMed] [Google Scholar]
- Baldwin R. T., Radovancević B., Duncan J. M., Wampler R. K., Frazier O. H. Management of patients supported on the Hemopump cardiac assist system. Tex Heart Inst J. 1992;19(2):81–86. [PMC free article] [PubMed] [Google Scholar]
- Baldwin R. T., Slogoff S., Noon G. P., Sekela M., Frazier O. H., Edelman S. K., Vaughn W. K. A model to predict survival at time of postcardiotomy intraaortic balloon pump insertion. Ann Thorac Surg. 1993 Apr;55(4):908–913. doi: 10.1016/0003-4975(93)90115-x. [DOI] [PubMed] [Google Scholar]
- Baue A. E. The role of the gut in the development of multiple organ dysfunction in cardiothoracic patients. Ann Thorac Surg. 1993 Apr;55(4):822–829. doi: 10.1016/0003-4975(93)90098-3. [DOI] [PubMed] [Google Scholar]
- Bhayana J. N., Scott S. M., Sethi G. K., Takaro T. Effects of intraaortic balloon pumping on organ perfusion in cardiogenic shock. J Surg Res. 1979 Feb;26(2):108–113. doi: 10.1016/0022-4804(79)90086-6. [DOI] [PubMed] [Google Scholar]
- Burnett C. M., Vega J. D., Radovancevic B., Lonquist J. L., Birovljev S., Sweeney M. S., Duncan J. M., Frazier O. H. Improved survival after Hemopump insertion in patients experiencing postcardiotomy cardiogenic shock during cardiopulmonary bypass. ASAIO Trans. 1990 Jul-Sep;36(3):M626–M629. [PubMed] [Google Scholar]
- CLAUSS R. H., BIRTWELL W. C., ALBERTAL G., LUNZER S., TAYLOR W. J., FOSBERG A. M., HARKEN D. E. Assisted circulation. I. The arterial counterpulsator. J Thorac Cardiovasc Surg. 1961 Apr;41:447–458. [PubMed] [Google Scholar]
- Deeb G. M., Bolling S. F., Nicklas J., Walsh R. S., Steimle C. N., Shea M. J., Meagher J. S. Clinical experience with the Nimbus pump. ASAIO Trans. 1990 Jul-Sep;36(3):M632–M636. [PubMed] [Google Scholar]
- Feola M., Adachi M., Akers W. W., Ross J. N., Jr, Wieting D. W., Kennedy J. H. Intraaortic balloon pumping in the experimental animal. Effects and problems. Am J Cardiol. 1971 Feb;27(2):129–136. doi: 10.1016/0002-9149(71)90249-9. [DOI] [PubMed] [Google Scholar]
- Landreneau R. J., Horton J. W., Cochran R. P. Splanchnic blood flow response to intraaortic balloon pump assist of hemorrhagic shock. J Surg Res. 1991 Oct;51(4):281–287. doi: 10.1016/0022-4804(91)90108-x. [DOI] [PubMed] [Google Scholar]
- Loisance D., Dubois-Randé J. L., Deleuze P., Okude J., Rosenval O., Geschwind H. Prophylactic intraventricular pumping in high-risk coronary angioplasty. Lancet. 1990 Feb 24;335(8687):438–440. doi: 10.1016/0140-6736(90)90666-s. [DOI] [PubMed] [Google Scholar]
- MOULOPOULOS S. D., TOPAZ S., KOLFF W. J. Diastolic balloon pumping (with carbon dioxide) in the aorta--a mechanical assistance to the failing circulation. Am Heart J. 1962 May;63:669–675. doi: 10.1016/0002-8703(62)90012-1. [DOI] [PubMed] [Google Scholar]
- Phillips S. J., Barker L., Balentine B., Vanderhaar J., Slonine D., Core M., Zeff R. H., Kongtahworn C., Skinner J. R., Grignon A. Hemopump support for the failing heart. ASAIO Trans. 1990 Jul-Sep;36(3):M629–M632. [PubMed] [Google Scholar]
- Rosemurgy A. S., McAllister E., Karl R. C. The acute surgical abdomen after cardiac surgery involving extracorporeal circulation. Ann Surg. 1988 Mar;207(3):323–326. doi: 10.1097/00000658-198803000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiiya N., Zelinsky R., Deleuze P. H., Loisance D. Y. Effects of Hemopump support on left ventricular unloading and coronary blood flow. ASAIO Trans. 1991 Jul-Sep;37(3):M361–M362. [PubMed] [Google Scholar]
- Sukehiro S., Flameng W. Effects of left ventricular assist for cardiogenic shock on cardiac function and organ blood flow distribution. Ann Thorac Surg. 1990 Sep;50(3):374–383. doi: 10.1016/0003-4975(90)90478-o. [DOI] [PubMed] [Google Scholar]
- Swartz M. T., Sakamoto T., Arai H., Reedy J. E., Salenas L., Yuda T., Standeven J. W., Pennington D. G. Effects of intraaortic balloon position on renal artery blood flow. Ann Thorac Surg. 1992 Apr;53(4):604–610. doi: 10.1016/0003-4975(92)90318-x. [DOI] [PubMed] [Google Scholar]
- Wampler R. K., Moise J. C., Frazier O. H., Olsen D. B. In vivo evaluation of a peripheral vascular access axial flow blood pump. ASAIO Trans. 1988 Jul-Sep;34(3):450–454. [PubMed] [Google Scholar]



