Abstract
Background
Marijuana is the most frequently used illicit substance in the United States. Little is known of the role that macro-level factors, including community norms and laws related to substance use, play in determining marijuana use, abuse and dependence. We tested the relationship between state-level legalization of medical marijuana and marijuana use, abuse, and dependence.
Methods
We used the second wave of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), a national survey of adults aged 18+ (n=34,653). Selected analyses were replicated using the National Survey on Drug Use and Health (NSDUH), a yearly survey of ~68,000 individuals aged 12+. We measured past-year cannabis use and DSM-IV abuse/dependence.
Results
In NESARC, residents of states with medical marijuana laws had higher odds of marijuana use (OR: 1.92; 95% CI: 1.49-2.47) and marijuana abuse/dependence (OR: 1.81; 95% CI: 1.22-2.67) than residents of states without such laws. Marijuana abuse/dependence was not more prevalent among marijuana users in these states (OR: 1.03; 95% CI: 0.67-1.60), suggesting that the higher risk for marijuana abuse/dependence in these states was accounted for by higher rates of use. In NSDUH, states that legalized medical marijuana also had higher rates of marijuana use.
Conclusions
States that legalized medical marijuana had higher rates of marijuana use. Future research needs to examine whether the association is causal, or is due to an underlying common cause, such as community norms supportive of the legalization of medical marijuana and of marijuana use.
Keywords: marijuana, community norms, medical marijuana laws, substance use disorders, legalization
1.0. INTRODUCTION
Marijuana is the most frequently used illicit substance, and marijuana abuse and dependence are highly prevalent in the United States (American Psychiatric Association, 2000; Compton et al., 2007; Johnston et al., 2009; Johnston et al., 2010; Office of Applied Studies, 2008). Chronic, regular use is associated with DSM-IV diagnoses of marijuana use disorders (Grant and Pickering, 1998). Such disorders are associated with marijuana withdrawal, unemployment, personality dysfunction, crime, respiratory problems and other psychiatric disorders (Budney et al., 2004; Budney and Moore, 2002; Hall and Lynskey, 2009; Haney, 2005; Hasin et al., 2008; Pedersen and Skardhamar; Taylor et al., 2000).
Behaviors are determined, at least in part, by expectations about the costs and benefits of one’s actions, including social approval or disapproval (Akers et al., 1979; Bandura, 1977, 1986). However, individual behaviors are also likely to be influenced by group-level acceptance or approval, also known as group norms (Armitage and Conner, 2001). Regarding marijuana, more positive beliefs and greater likelihood of use are more likely among individuals in communities or geographic areas with more approving norms (Lipperman-Kreda and Grube, 2009; Lipperman-Kreda et al., 2010).
Studies of individual perceptions of norms suggest that such norms predict marijuana use (Beyers et al., 2004; Botvin et al., 2001; Elek et al., 2006; Hansen and Graham, 1991). These studies, while important, do not provide information on group-level norms, which is needed for several reasons. First, individual perceptions of societal norms may not always be accurate. Second, societal norms may influence behavior independently of individual beliefs. That is, other things being equal, a given individual may be more likely to use marijuana in an accepting than in a non-accepting society, as we recently showed (Keyes et al., In press). Third, policy and program interventions focused on societal norms may have a wider impact than interventions focused on individuals (Chilenski et al., 2010; Lipperman-Kreda and Grube, 2009; Lipperman-Kreda et al., 2010). Therefore, studying the influence of societal-level norms is increasingly important, especially during times such as the present when marijuana use, abuse and dependence are increasing. However, a difficulty in conducting this research is the scarcity of informative societal-level data on groups with differing norms.
State medical marijuana laws can be seen as one indicator of group-level approval of marijuana use. These laws legalize marijuana use, when authorized by a physician, for medical purposes such as alleviation of nausea and vomiting from chemotherapy, wasting in AIDS patients, and chronic pain unresponsive to opioids (Procon.org). Between 1996 and 2011, 16 states passed laws legalizing marijuana use for medical purposes. Medical marijuana laws can be used to represent state-level norms on marijuana use because generally, a substantial relationship exists between public opinion and policy decisions (Brooks, 2006; Burstein, 2003, 2006; Nielsen, 2010) and specifically, because community norms regarding substance use (e.g., drinking and cigarette smoking) are directly related to policy and enforcement efforts (Lipperman-Kreda and Grube, 2009; Lipperman-Kreda et al., 2010). For example, Khatapoush et al. found that among individuals aged 16-25 in California, marijuana use did not increase in 1996 after legalization of medical marijuana, but marijuana use was higher in California than in other 10 comparison states in 1995, 1997 and 1999 (Khatapoush and Hallfors, 2004). This suggests that state-level norms may have contributed to both the legalization of medical marijuana and to higher rates of use in California in comparison to other states.
We used data from a national, population-based study to examine the relationship between state-level legalization of marijuana, and state- and individual-level population-based rates of marijuana use and marijuana abuse/dependence. We addressed the following questions: (1) did states that legalized medical marijuana by 2004 exhibit higher rates of past-year marijuana use and abuse/dependence in 2004-2005 than states that did not legalize it?; (2) were individuals living in states that legalized medical marijuana at higher risk for marijuana use, abuse and dependence in the past year than individuals who live in states that did not legalize medical marijuana?; and (3) among marijuana users, was residence in a state that legalized medical marijuana associated with increased risk for meeting criteria for marijuana abuse and dependence?
2.0. METHODS
2.1. Primary exposure variable: State-level medical marijuana laws
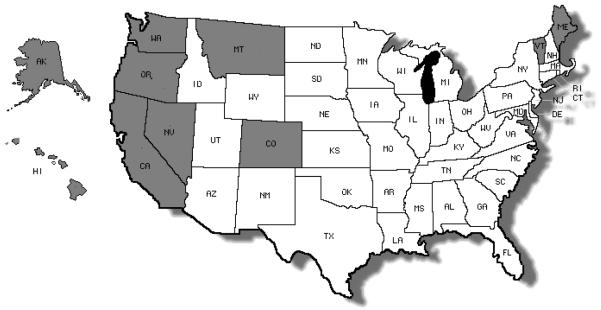
Our primary exposure variable was whether a state had legalized the medical use of marijuana by 2004. This year was chosen to coincide with the period in which our main data source was collected. The following states were defined as “exposed”: Alaska, California, Colorado, Hawaii, Maine, Montana, Nevada, Oregon, Vermont and Washington (Figure 1). The remaining 40 states were “unexposed” in 2004.
Figure 1.
Map of states that legalized medical marijuana by 2004
2.2. Outcome data
For our outcome variables, we analyzed data from two surveys that used different methods to collect data on marijuana use. The main data source was the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), which used face-to-face interviews (Grant et al., 2009; Grant et al., 2004). Using NESARC data, we examined state-level differences in rates of non-medical marijuana abuse/dependence, and in use. As a secondary data source, we analyzed data from the National Survey on Drug Use and Health (NSDUH). The NSDUH used respondent self-administration procedures to collect data on marijuana use (Grucza et al., 2007; US Department of Health and Human Services). Given the difference between interview and self-administration methodology in the NESARC and the NSDUH, the latter survey provides valuable replication of an important component of our study. We focus on state legalization of medical marijuana up until 2004 because NESARC data were collected primarily during that year.
2.3. Primary outcome data: NESARC
Data were drawn from the 2004-2005 NESARC, a national survey of non-institutionalized adults aged 18+ in the United States residing in homes or group quarters. In 2001-2002, NESARC participants (N=43,093; response rate, 81% of those eligible) were initially interviewed. In 2004-2005, 34,653 were re-interviewed (86.7% of original sample; ineligible respondents included deceased, n=1403; deported, mentally or physically impaired, n=781; or on active duty in the armed forces, n=950). The cumulative response rate for the Wave 2 sample was therefore 70.2%. We used the data from Wave 2 because two additional states (Vermont and Montana) legalized medical marijuana between 2002 and 2004. More detail on the study methods is found elsewhere(Grant et al., 2009; Grant et al., 2004). The research protocol, including written informed consent procedures, received full ethical review and approval from the U.S. Census Bureau and the U.S. Office of Management and Budget.
2.3.1. NESARC outcome variables: non-medical marijuana use, abuse, and dependence
Participants were interviewed with the Alcohol Use Disorder and Associated Disabilities Interview Schedule DSM-IV version (AUDADIS-IV) (Grant et al., 2001), a fully-structured instrument designed for experienced lay interviewers. The AUDADIS covers non-medical cannabis use and also detailed questions on the criteria for DSM-IV cannabis abuse and dependence, combined through computer algorithms (Compton et al., 2004) to generate DSM-IV(American Psychiatric Association, 1994) diagnoses. (While the term “cannabis” includes marijuana and other forms, e.g., hashish, we use the term “marijuana abuse/dependence” throughout given the small proportion of hashish relative to all cannabis used in the U.S. (~1%) (Mehmedic et al.)). Good to excellent reliability and validity of marijuana abuse/dependence diagnoses (κ=0.62-0.78) in the AUDADIS-IV have been extensively documented in both U.S. and international samples, including clinical reappraisals conducted by psychiatrists in clinical and general population samples, and in several countries as part of the World Health Organization/National Institutes of Health International Study on Reliability and Validity (Chatterji et al., 1997; Cottler et al., 1997; Grant et al., 1995; Hasin et al., 1997; Nelson et al., 1999; Pull et al., 1997; Ustun et al., 1997; Vrasti et al., 1998). Using the timeframe of the last 12 months, the outcome variables were defined as marijuana use, marijuana use disorder (meeting criteria for abuse or dependence). We then examined the outcome of marijuana abuse/dependence among the subset of current marijuana users.
We combined abuse and dependence into one outcome, since empirical findings indicate that it better captures the underlying prevalence of cannabis use disorders than dependence or abuse alone. While substance use disorders were originally conceived as a bi-axial syndrome with dependence capturing more physiologic dimensions of addiction and abuse capturing more behavioral consequences, there is now substantial evidence to indicate that abuse and dependence criteria, including cannabis use disorder criteria, represent a unidimensional construct (Beseler and Hasin, 2010; Helzer et al., 2007; Li et al., 2007; Martin et al., 2006; Martin et al., 2008; Saha et al., 2006).
2.3.2. NESARC individual-level covariates
At the individual level, covariates included self-reported sex, race/ethnicity (non-Hispanic White, non-Hispanic Black, non-Hispanic Native American/Alaska Native, non-Hispanic Asian/Native Hawaiian/Pacific Islander, Hispanic), age (20-29, 30-39, 40-49, 50+), past-year personal income ($0-19,999, $20-34,999, $35-69,999, >$70,000), education (some college versus high school or less), marital status (married versus single/widowed/separated/divorced), and urbanicity (living within a metropolitan statistical area versus not). Previous studies in these data have shown associations between these individual-level factors and marijuana use/disorder (Compton et al., 2005; Compton et al., 2004).
2.4. Secondary data source: National Survey on Drug Use and Health (NSDUH)
State-level rates of marijuana use but not DSM-IV abuse/dependence are publicly available from the NSDUH. The NSDUH collects information from residents aged 12 and older of households, noninstitutional group quarters, and civilians living in military bases, using a 50-state design with an independent, multistage probability area sample for each state. To maximize comparability with the NESARC, we combined 2004 and 2005 NSDUH data and included only respondents aged 18 or older (US Department of Health and Human Services). In 2004, the sample size was 67,760, and in 2005, 68,308 individuals responded to the survey. Each year, NSDUH allocates the sample size equally across three age groups: persons aged 12-17, persons aged 18-25, and persons aged 26 or older, yielding approximately 45,000 in our sample of 18 and older in both years. However, since we conducted state-level analyses with NSDUH, our effective sample size was 50 states per year.
2.4.1. NSDUH outcome variable
The outcome measure of interest was the proportion of respondents in each state who reported marijuana use for nonmedical purposes in the previous year.
2.5. State-level covariates
In all NESARC and NSDUH analyses, we adjusted for a series of state-level characteristics that might have differed between states that legalized vs. those that did not legalize medical marijuana, and that might also relate to marijuana use and abuse/dependence, including the proportion of state residents who were male, white or other race/ethnicity, without a high school diploma, and under 30 years of age (Subramanian and Kawachi, 2004). These covariates were obtained for the year 2004 from the American Community Survey (ACS) [http://factfinder.census.gov/], which provides publicly available estimates of state populations ascertained between the decennial census excluding populations living in institutions, college dormitories, and other group quarter facilities.
2.6. Analyses
The NESARC sample and its associated sampling weights were originally constructed in order to provide nationally representative estimates. Nevertheless, the sample included individuals from all 50 states with sample sizes ranging from 69 in Vermont to 3932 in California (median sample size across states, 490 persons). The use of nationally representative data to address associations at the state-level can be accomplished through multilevel regression (Gelman, 2007; Lax and Phillips, 2009; Park et al., 2004) where potential lack of representativeness of samples within states is accounted for by controlling for individual-level covariates in the model. To lessen concerns regarding the representativeness (or lack thereof) of NESARC data at the state-level, an investigation was conducted to compare the demographic representation of the sample at the state level. Correlations and Bland-Altman plots (Bland and Altman, 1986, 1999) were used to compare weighted and unweighted state-level NESARC demographic variables with the ACS state demographics. Since correlations between NESARC demographic variables and the ACS were higher using completely unweighted state estimates rather than the weighted estimates, we concluded that the NESARC was representative at the state level, and we performed the state- and multi-level NESARC analyses without the sampling weights.
The association between our exposure variable (state-level medical marijuana law) and marijuana outcomes was examined two ways: 1) a state-level regression and 2) a multilevel regression model of individual-level data nested within states. Using the NESARC, we performed both types of analyses for these three outcomes: past year marijuana use, marijuana abuse/dependence, and marijuana abuse/dependence among current marijuana users. Using the NSDUH, we performed a state-level analysis of past year marijuana use.
The NESARC and NSDUH state-level analyses used linear regression (SAS 9.2 Proc GLM) of state-level prevalence estimates (n=50) of the outcomes regressed on an indicator of whether the state had a law legalizing medical marijuana use, controlling for state-level covariates. Regression-adjusted mean prevalence and 95% confidence intervals are presented for comparison between states with and without medical marijuana laws.
The NESARC multilevel analyses used hierarchical logistic regression (SAS 9.2 Proc GLIMMIX) of individual marijuana outcomes (n=34,520 for marijuana use and abuse/dependence, n=1453 for abuse/dependence among users) regressed on individual- and state-level covariates, including state-level medical marijuana law. The hierarchical logistic regression included a random intercept for state to account for possible correlation of individuals within state not explained by state-level covariates. In addition, a random effect for the primary sampling units (nested within states) was included to account for the complex clustered NESARC sampling design.
3.0. RESULTS
3.1. State-level results
The first two columns of Table 1 present mean state-level prevalence of past-year marijuana use and abuse/dependence, obtained as predicted values from our state-level linear regression models. Using NESARC, the average state-level prevalence of past-year marijuana use differed significantly between states with (7.13%) and without (3.57%) medical marijuana laws (P<0.0001). The average NESARC state-level prevalence of marijuana abuse/dependence also differed significantly between states with (2.61%) and without (1.27%) medical marijuana laws (P=0.0009). Using NSDUH data (not noted in Table), the average state-level prevalence of past-year marijuana use differed significantly between states with (12.17%) and without (9.77%) medical marijuana laws (p=0.0006).
Table 1.
Marijuana Use and Marijuana Abuse/Dependence by State Legalization of Medical Marijuana Use Up to 2004, NESARC
| Outcomes of interest |
State-level analyses1 | Multi-level analysis2 |
|
|---|---|---|---|
| State Legal Medical Marijuana Use up to 2004 | |||
| No | Yes | ||
| OR (95% CI) | |||
| % (95% CI) | % (95% CI) | ||
| Past Year Marijuana Abuse/Dependence |
1.27 (1.00, 1.54) | 2.61 (1.96, 3.25) | 1.81 (1.22, 2.67) |
| Past Year Marijuana Use |
3.57 (3.10, 4.03) | 7.13 (6.02, 8.24) | 1.92 (1.49, 2.47) |
| Past Year Marijuana Abuse/Dependence among current users |
35.34 (29.46, 41.21) | 37.68 (23.70, 51.66) | 1.03 (0.67, 1.60) |
NESARC: National Epidemiologic Survey on Alcohol and Related Conditions; 95% CI: 95% confidence interval
Adjusted for state-%-youth, state-%-males, state-high-school-graduation-rates, state-%-whites.
Adjusted for age, sex, race/ethnicity, education, income, marital status, urbanicity, state-%-youth, state-%-males, state-high-school-graduation-rates, state-%-whites.
3.2. Individual-level results
The third column of Table 1 presents the individual odds of past-year marijuana use and abuse/dependence, obtained as odds ratio estimates from our multi-level regression models. Using NESARC, the individual odds of past-year marijuana use differed between respondents who lived in states with and without medical marijuana laws. The odds of marijuana use in the past year were 1.92 times higher (95% confidence interval (95% CI): 1.49, 2.47; p<0.0001) among residents of states with rather than without medical marijuana laws. The individual odds of marijuana abuse/dependence also differed between respondents who lived in states with and without medical marijuana laws. The odds of marijuana abuse/dependence were 1.81 times higher (95% CI: 1.22, 2.67; p=0.0040) among residents of states that had legalized medical marijuana. However, when marijuana abuse/dependence was examined among marijuana users, the prevalence was very similar in states with and without medical marijuana laws, and the odds of abuse/dependence did not differ significantly.
4.0. DISCUSSION
This study indicates that states that legalized marijuana use for medical purposes have significantly higher rates of marijuana use and of marijuana abuse and dependence. The results for marijuana use were found at the state level in two national datasets, the NESARC and the NSDUH, and at the individual level in the NESARC. In addition, in the NESARC, respondents living in states with medical marijuana laws had significantly higher prevalence of marijuana use disorders (abuse/dependence) as defined by DSM-IV. However, in the NESARC, among those who were using marijuana, there was no increase in odds of abuse or dependence, suggesting that any relationship detected between state medical marijuana laws and marijuana abuse/dependence is explained by differences in marijuana use.
Our findings do not necessarily indicate a causal effect of legalization of medical marijuana on marijuana use or marijuana abuse/dependence; that would require a different study design. However, the findings do raise the need to consider possible explanations or mechanisms for the relationships we found, all of which could serve as the basis for further studies. We consider four potential mechanisms.
First, state-level community norms more supportive of marijuana use may contribute to the legalization of medical marijuana and to higher rates of marijuana use. Prior studies on drinking and smoking suggest a direct link between community approval of use and policy change (Lipperman-Kreda and Grube, 2009; Lipperman-Kreda et al., 2010). Regarding marijuana, passage of state medical marijuana laws may reflect underlying state-level community norms, especially when such legislation is passed by voter referenda. In addition, the medical marijuana laws that passed in state legislatures by wide margins of votes appear to reflect an underlying high level of support for such legislation prior to their enactment, as well as the absence of a strong and vocal minority opposition (Mikos, 2009; Scott, 2000).
Second, the enactment of medical marijuana laws could lead to a change in community attitudes on both medical and non-medical marijuana use, including reduced disapproval and perceived riskiness of use, which could subsequently influence marijuana use and abuse/dependence. Prior work has shown a relationship between formal behavioral sanctions and the subsequent creation of informal social norms and regulation of behavior (Scott, 2000). However, the scarce existing evidence on the link between marijuana laws, attitudes and marijuana use raises questions about the validity of this type of causal link. Khatapoush et al., for example, found that while perceived harm of marijuana decreased after legalization of medical marijuana in California, approval of recreational use and actual recreational use did not change with the change in the laws (Khatapoush and Hallfors, 2004).
The position that community norms supportive of marijuana use may be an underlying mechanism explaining the higher rates of marijuana use and abuse/dependence in states that legalized medical marijuana (either as a “common cause” of changes in legislation and marijuana use or as a mediator linking legislation to marijuana use) is supported by the broader literature on group norms, which has demonstrated that group norms shape individual behavior and mental health (Asch, 1951, 1952; Cullen, 1983; Durkheim, 1938) and that social pressures to conform to the group norms influence the decision to engage in behaviors once norms are internalized. In the area of substance use, parallels can be established with alcohol use and cigarette smoking. For example, “cultures” of drinking (Skog, 1985) in the neighborhood (Ahern et al., 2008) and workplace (Barrientos-Gutierrez et al., 2007) have been linked with risk for binge drinking. Further, perceived disapproval of adolescent alcohol use is associated with less prevalent underage drinking (Kumar et al., 2002; Lipperman-Kreda et al., 2010). Permissive neighborhood smoking norms have also been associated with increased prevalence of smoking (Ahern et al., 2009).
A third potential mechanism underlying the association between medical marijuana laws and marijuana use and abuse/dependence is medical endorsement of its use for medical purposes. However, no consensus exists at this time on the effectiveness of marijuana as a treatment for symptoms of pain, nausea, vomiting and other problems caused by illnesses or treatment (Joy et al., 1999; MacCoun and Reuter, 2001a; Martín-Sánchez et al., 2009). The lack of medical consensus means that both pro and con proponents of medical marijuana laws can find research support for their positions, and the medical community has not delivered a clear message to the public.
A fourth potential mechanism relates to marijuana availability: legalization of medical marijuana may lead to greater commercial promotion and availability of the substance for recreational purposes, which may contribute to greater illicit use of marijuana. Pacula et al. examined state temporal variation in the adoption of active medical marijuana policies, and found that policies aimed at users (e.g., provisions for physicians to recommend marijuana or allowances for a medical necessity defense for those who use marijuana for medical purposes) led to changes in prices of marijuana in local markets, in a fashion that was consistent with anticipated increases in demand (Pacula et al., 2010). Yet related research indicates that decriminalizing marijuana in other countries (and thus increasing its commercial availability) did not lead to increased use (MacCoun and Reuter, 1997, 2001b; McGeorge and Aitken, 1997; Simons-Morton et al., 2010; Single, 1989), although one study in the Netherlands suggested that shifting from depenalization to active commercialization of marijuana was associated with increased marijuana use (MacCoun and Reuter, 2001b).
State legalization of medical marijuana may also be associated with potential health, economic, and social gains that we do not consider in this paper. Benefits of legalization may include relief of pain and nausea for cancer and HIV/AIDS patients, tax revenue from marijuana sales, control of crime, decreased costs of the criminal justice system, and reduction in the disproportionate incarceration of minorities for possession of small quantities of marijuana (Levine and Reinarman, 1991; van den Brink, 2008; Wodak, 2002). While we recognize such potential benefits, our study cannot make any statements on such aspects of legalization of medical marijuana.
We note study limitations. First, we relied on cross-sectional data, and thus we cannot demonstrate a causal relationship between enactment of state medical marijuana laws and individual risk for illicit marijuana use. Future studies should use large-sample survey data collected in years prior to and after enactment of marijuana laws in states with and without such laws, to compare prevalences and trends. The fact that only two states changed their medical marijuana laws between the two NESARC study waves made this type of design difficult to implement with NESARC data. Second, the NESARC reported lower rates of marijuana use than the NSDUH, possibly due to NESARC use of interviewer- rather than self-administered questions on marijuana use. However, this concern is offset by two factors: a) the NESARC measure of marijuana abuse/dependence is highly sensitive among users compared to other measures, including the NSDUH (Grucza et al., 2007) and b) most importantly for the present purpose, we found the same relationship between medical marijuana laws and marijuana use in both the NESARC and the NSDUH. Third, the NESARC only released information regarding state of residence at Wave 1. While movement between waves could have led to misclassification of a subset of respondents, related research finding a significant relationship between minimum drinking age laws based on the state of birth and current substance use disorders indicates that misclassification may not be differential by state legalization status (Norberg et al., 2009). Fourth, we examined the relationship between state legalization by 2004 and marijuana abuse/dependence, and thus excluded four states that have legalized medical marijuana since 2004. To determine whether this affected our results, we re-did the NSDUH analysis using 2007-2008 data, adding the 2 states (Rhode Island and New Mexico) that legalized medical marijuana between 2004 and 2007. The results were not significantly different from those produced from the 2004-2005 data (P>0.05) and are available upon request. Finally, we compared states by legalization status. Future studies need to assess the variation in marijuana use related to heterogeneity of the laws across states, since allowances vary between states in factors such as home production permits, role of the doctor in determining access to marijuana, and the types of illnesses and conditions for which it is legal to access marijuana.
This study highlights the key role that macro-level factors, such as policy changes and community norms about substance use, play in shaping marijuana use and abuse/dependence. Future studies are also needed on the consequences of increased marijuana use, such as accidents, aggression, school drop out, psychosis, HIV and sexually transmitted disease rates (Fergusson et al., 2003a; Fergusson et al., 2003b; Hall and Degenhardt, 2009) as well as on the particular impact of medical marijuana legalization on youth, who bear a disproportionate burden of marijuana-related disorders (Budney and Moore, 2002), and are vulnerable to the advertising effects of other substances such as tobacco (Hanewinkel et al., 2011). In particular, future studies in the United States and elsewhere can build on our findings by comparing trends in community norms, marijuana use and abuse/dependence before and after the legalization of marijuana, to understand the relative contribution of medical marijuana legalization and community norms on changes in marijuana use and abuse/dependence.
Acknowledgements
We would like to thank Eliana Greenstein for her assistance in the data analysis.
We also thank NIAAA, NIDA and the New York State Psychiatric Institute for funding this study.
Role of Funding Source
This study was supported by K05 AA014223, R01DA018652, U01AA018111 and the New York State Psychiatric Institute (Hasin). The NIAAA, NIDA, and the New York State Psychiatric Institute had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
Drs. Cerdá and Hasin designed the study. Drs. Cerdá and Keyes managed the literature searches and summaries of previous related work. Dr. Wall undertook the statistical analysis, and Dr. Cerdá wrote the first draft of the manuscript, with sections also written by Drs. Wall and Keyes. Drs. Hasin and Galea provided critical input to multiple drafts of the paper. All authors contributed to and approved the final manuscript.
Conflict of Interest
All authors declare that they have no conflicts of interest.
References
- Ahern J, Galea S, Hubbard A, Midanik L, Syme SL. “Culture of drinking” and individual problems with alcohol use. Am. J. Epidemiol. 2008;167:1041–1049. doi: 10.1093/aje/kwn022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahern J, Galea S, Hubbard A, Syme SL. Neighborhood smoking norms modify the relation between collective efficacy and smoking behavior. Drug Alcohol Depend. 2009;100:138–145. doi: 10.1016/j.drugalcdep.2008.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akers RL, Krohn MD, Lanzakaduce L, Radosevich M. Social-Learning and deviant-behavior - specific test of a general-theory. Am. Sociol. Rev. 1979;44:636–655. [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th edition American Psychopathological Association; Washington, D.C: 1994. [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th edition. Washington, DC: 2000. text rev.) [Google Scholar]
- Armitage CJ, Conner M. Efficacy of the theory of planned behaviour: a meta-analytic review. Br. J. Soc. Psychol. 2001;40:471–499. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- Asch S. Effects of group pressure of the modification and distortion of judgements. In: Guetzkow H, editor. Groups, Leadership and Men: Research in Human Relations. Carnegie Press; Pittsburgh, PA: 1951. pp. 177–190. [Google Scholar]
- Asch S. Social Psychology. Prentice Hall; Upper Saddle River, NJ: 1952. [Google Scholar]
- Bandura A. Social Learning Theory. Prentice Hall; Upper Saddle River, NJ: 1977. [Google Scholar]
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Perspective. Princeton-Hall; Englewood Cliffs, NJ: 1986. [Google Scholar]
- Barrientos-Gutierrez T, Gimeno D, Mangione TW, Harrist RB, Amick BC. Drinking social norms and drinking behaviours: a multilevel analysis of 137 workgroups in 16 worksites. Occup. Environ. Med. 2007;64:602–608. doi: 10.1136/oem.2006.031765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beseler CL, Hasin DS. Cannabis dimensionality: dependence, abuse and consumption. Addict. Behav. 2010;35:961–969. doi: 10.1016/j.addbeh.2010.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beyers JM, Toumbourou JW, Catalano RF, Arthur MW, Hawkins JD. A cross-national comparison of risk and protective factors for adolescent substance use: The United States and Australia. J. Adolesc. Health. 2004;35:3–16. doi: 10.1016/j.jadohealth.2003.08.015. [DOI] [PubMed] [Google Scholar]
- Bland J, Altman D. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet i. 1986:307–310. [PubMed] [Google Scholar]
- Bland J, Altman D. Measuring agreement in method comparison studies. Stat. Methods Med. Res. 1999;8:135–160. doi: 10.1177/096228029900800204. [DOI] [PubMed] [Google Scholar]
- Botvin GJ, Griffin KW, Diaz T, Ifill-Williams M. Drug abuse prevention among minority adolescents: posttest and one-year follow-up of a school-based preventive intervention. Prev. Sci. 2001;2:1–13. doi: 10.1023/a:1010025311161. [DOI] [PubMed] [Google Scholar]
- Brooks C. Voters, satisficing, and policymaking: recent directions in the study of electoral politics. Ann. Rev. Sociol. 2006;32:191–211. [Google Scholar]
- Budney AJ, Hughes JR, Moore BA, Vandrey R. Review of the validity and significance of cannabis withdrawal syndrome. Am. J. Psychiatry. 2004;161:1967–1977. doi: 10.1176/appi.ajp.161.11.1967. [DOI] [PubMed] [Google Scholar]
- Budney AJ, Moore BA. Development and consequences of cannabis dependence. J. Clin. Pharmacol. 2002;42:28S–33S. doi: 10.1002/j.1552-4604.2002.tb06000.x. [DOI] [PubMed] [Google Scholar]
- Burstein P. The impact of public opinion on public policy: a review and an agenda. Polit. Res. Q. 2003;56:29–40. [Google Scholar]
- Burstein P. Why estimates of the impact of public opinion on public policy are too high: empirical and theoretical implications. Soc. Forces. 2006;84:2273–2289. [Google Scholar]
- Chatterji S, Saunders JB, Vrasti R, Grant BF, Hasin D, Mager D. Reliability of the alcohol and drug modules of the Alcohol Use Disorder and Associated Disabilities Interview Schedule--Alcohol/Drug-Revised (AUDADIS-ADR): an international comparison. Drug Alcohol Depend. 1997;47:171–185. doi: 10.1016/s0376-8716(97)00088-4. [DOI] [PubMed] [Google Scholar]
- Chilenski SM, Greenberg MT, Feinberg ME. The community substance use environment: the development and predictive ability of a multi-method and multiple-reporter measure. J. Community Appl. Soc. Psychol. 2010;20:57–71. doi: 10.1002/casp.1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton W, Thomas Y, Stinson FS, Grant B. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States - results from the National Epidemiologic Survey of Alcohol and Related Conditions. Arch. Gen. Psychiatry. 2007;64:566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- Compton WM, Conway KP, Stinson FS, Colliver JD, Grant BF. Prevalence, correlates, and comorbidity of DSM-IV antisocial personality syndromes and alcohol and specific drug use disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. J. Clin. Psychiatry. 2005;66:677–685. doi: 10.4088/jcp.v66n0602. [DOI] [PubMed] [Google Scholar]
- Compton WM, Grant BF, Colliver JD, Glantz MD, Stinson FS. Prevalence of marijuana use disorders in the United States: 1991-1992 and 2001-2002. JAMA. 2004;291:2114–2121. doi: 10.1001/jama.291.17.2114. [DOI] [PubMed] [Google Scholar]
- Cottler LB, Grant BF, Blaine J, Mavreas V, Pull C, Hasin D, Compton WM, Rubio-Stipec M, Mager D. Concordance of DSM-IV alcohol and drug use disorder criteria and diagnoses as measured by AUDADIS-ADR, CIDI and SCAN. Drug Alcohol Depend. 1997;47:195–205. doi: 10.1016/s0376-8716(97)00090-2. [DOI] [PubMed] [Google Scholar]
- Cullen F. Rethinking Crime and Deviance Theory: The Emergence of a Structuring Tradition. Roman and Allenheld; Totowa, NJ: 1983. [Google Scholar]
- Durkheim E. The Rules of Sociological Method. The Free Press; New York: 1938. [Google Scholar]
- Elek E, Miller-Day M, Hecht ML. Influences of personal, injunctive, and descriptive norms on early adolescent substance use. J. Drug Issues. 2006;36:147–171. [Google Scholar]
- Fergusson DM, Horwood LJ, Swain-Campbell NR. Cannabis dependence and psychotic symptoms in young people. Psychol. Med. 2003a;33:15–21. doi: 10.1017/s0033291702006402. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Swain-Campbell NR, Horwood LJ. Arrests and convictions for cannabis related offences in a New Zealand birth cohort. Drug Alcohol Depend. 2003b;70:53–63. doi: 10.1016/s0376-8716(02)00336-8. [DOI] [PubMed] [Google Scholar]
- Gelman A. Struggles with survey weighting and regression modeling. Stat. Sci. 2007;22:153–164. [Google Scholar]
- Grant BF, Dawson DA, Hasin DS. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV Version. National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 2001. [Google Scholar]
- Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, Saha TD, Smith SM, Pulay AJ, Pickering RP, Ruan WJ, Compton WM. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol. Psychiatry. 2009;14:1051–1066. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Harford TC, Dawson DA, Chou PS, Pickering RP. The Alcohol Use Disorder and Associated Disabilities Interview schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug Alcohol Depend. 1995;39:37–44. doi: 10.1016/0376-8716(95)01134-k. [DOI] [PubMed] [Google Scholar]
- Grant BF, Pickering R. The relationship between cannabis use and DSM-IV cannabis abuse and dependence: results from the national longitudinal alcohol epidemiologic survey. J. Subst. Abuse. 1998;10:255–264. doi: 10.1016/s0899-3289(99)00006-1. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch. Gen. Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Grucza RA, Abbacchi AM, Przybeck TR, Gfroerer JC. Discrepancies in estimates of prevalence and correlates of substance use and disorders between two national surveys. Addiction. 2007;102:623–629. doi: 10.1111/j.1360-0443.2007.01745.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall W, Degenhardt L. Adverse health effects of non-medical cannabis use. Lancet. 2009;374:1383–1391. doi: 10.1016/S0140-6736(09)61037-0. [DOI] [PubMed] [Google Scholar]
- Hall W, Lynskey M. The challenges in developing a rational cannabis policy. Curr. Opin. Psychiatr. 2009;22:258–262. doi: 10.1097/YCO.0b013e3283298f36. [DOI] [PubMed] [Google Scholar]
- Hanewinkel R, Isensee B, Sargent JD, Morgenstern M. Cigarette advertising and teen smoking initiation. Pediatrics. 2011;127:e271–278. doi: 10.1542/peds.2010-2934. [DOI] [PubMed] [Google Scholar]
- Haney M. The marijuana withdrawal syndrome: diagnosis and treatment. Curr. Psychiatry Rep. 2005;7:360–366. doi: 10.1007/s11920-005-0036-1. [DOI] [PubMed] [Google Scholar]
- Hansen WB, Graham JW. Preventing alcohol, marijuana, and cigarette use among adolescents - peer pressure resistance training versus establishing conservative norms. Prev. Med. 1991;20:414–430. doi: 10.1016/0091-7435(91)90039-7. [DOI] [PubMed] [Google Scholar]
- Hasin D, Carpenter KM, McCloud S, Smith M, Grant BF. The alcohol use disorder and associated disabilities interview schedule (AUDADIS): reliability of alcohol and drug modules in a clinical sample. Drug Alcohol Depend. 1997;44:133–141. doi: 10.1016/s0376-8716(97)01332-x. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Keyes KM, Alderson D, Wang S, Aharonovich E, Grant BE. Cannabis withdrawal in the United States: results from NESARC. J. Clin. Psychiatry. 2008;69:1354–1363. doi: 10.4088/jcp.v69n0902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helzer JE, Bucholz KK, Gossop M. A dimensional option for the diagnosis of substance dependence in DSM-V. Int. J. Methods Psychiatr. Res. 2007;16(Suppl. 1):S24–33. doi: 10.1002/mpr.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use, 1975-2008. Volume II: College students. NIH Publication No 10-7586. National Institute on Drug Abuse; Bethesda, MD: 2009. [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future National Survey Results on Drug Use, 1975-2009. Volume I: Secondary school students. NIH Publication No 10-7584. National Institute on Drug Abuse; Bethesda, MD: 2010. [Google Scholar]
- Joy J, Watson S Jr, Benson J, editors. Marijuana and Medicine: Assessing the Science Base. National Academy Press; Washington, DC: 1999. [PubMed] [Google Scholar]
- Keyes K, Schulenberg J, O’Malley P, Johnston L, Bachman J, Li G, Hasin D. The social norms of birth cohorts and adolescent marijuana use in the United States. doi: 10.1111/j.1360-0443.2011.03485.x. In press. 1976-2007. Addiction. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khatapoush S, Hallfors D. “Sending the wrong message”: did medical marijuana legalization in California change attitudes about and use of marijuana? J. Drug Issues. 2004;34:751–770. [Google Scholar]
- Kumar R, O’Malley PM, Johnston LD, Schulenberg JE, Bachman JG. Effects of school-level norms on student substance use. Prev. Sci. 2002;3:105–124. doi: 10.1023/a:1015431300471. [DOI] [PubMed] [Google Scholar]
- Lax J, Phillips J. How should we estimate public opinion in the states? Am. J. Polit. Sci. 2009;53:107–121. [Google Scholar]
- Levine HG, Reinarman C. From prohibition to regulation - lessons from alcohol policy for drug policy. Milbank Q. 1991;69:461–494. [PubMed] [Google Scholar]
- Li TK, Hewitt BG, Grant BF. The Alcohol Dependence Syndrome, 30 years later: a commentary. The 2006 H. David Archibald Lecture. Addiction. 2007;102:1522–1530. doi: 10.1111/j.1360-0443.2007.01911.x. [DOI] [PubMed] [Google Scholar]
- Lipperman-Kreda S, Grube JW. Students’ perception of community disapproval, perceived enforcement of school antismoking policies, personal beliefs, and their cigarette smoking behaviors: results from a structural equation modeling analysis. Nicotine Tob. Res. 2009;11:531–539. doi: 10.1093/ntr/ntp033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipperman-Kreda S, Grube JW, Paschall MJ. Community norms, enforcement of minimum legal drinking age laws, personal beliefs and underage drinking: an explanatory model. J. Community Health. 2010;35:249–257. doi: 10.1007/s10900-010-9229-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacCoun R, Reuter P. Interpreting Dutch cannabis policy: reasoning by analogy in the legalization debate. Science. 1997;278:47–52. doi: 10.1126/science.278.5335.47. [DOI] [PubMed] [Google Scholar]
- MacCoun R, Reuter P, editors. Drug War Heresies: Learning from Other Vices, Times, and Places. Cambridge University Press; Cambridge, UK: 2001a. [Google Scholar]
- MacCoun R, Reuter P. Evaluating alternative cannabis regimes. Br. J. Psychiatry. 2001b;178:123–128. doi: 10.1192/bjp.178.2.123. [DOI] [PubMed] [Google Scholar]
- Martin CS, Chung T, Kirisci L, Langenbucher JW. Item response theory analysis of diagnostic criteria for alcohol and cannabis use disorders in adolescents: implications for DSM-V. J. Abnorm. Psychol. 2006;115:807–814. doi: 10.1037/0021-843X.115.4.807. [DOI] [PubMed] [Google Scholar]
- Martin CS, Chung T, Langenbucher JW. How should we revise diagnostic criteria for substance use disorders in the DSM-V? J. Abnorm. Psychol. 2008;117:561–575. doi: 10.1037/0021-843X.117.3.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martín-Sánchez E, Furukawa T, Taylor J, Martin J. Systematic review and meta-analysis of cannabis treatment for chronic pain. Pain Med. 2009;10:1353–1368. doi: 10.1111/j.1526-4637.2009.00703.x. [DOI] [PubMed] [Google Scholar]
- McGeorge J, Aitken CK. Effects of cannabis decriminalization in the Australian capital territory on university students’ patterns of use. J. Drug Issues. 1997;27:785–793. [Google Scholar]
- Mehmedic Z, Chandra S, Slade D, Denham H, Foster S, Patel AS, Ross SA, Khan IA, ElSohly MA. Potency trends of delta 9-THC and other cannabinoids in confiscated cannabis preparations from 1993 to 2008. J. Forensic Sci. 55:1209–1217. doi: 10.1111/j.1556-4029.2010.01441.x. [DOI] [PubMed] [Google Scholar]
- Mikos R. On the limits of supremacy: medical marijuana and the states’ overlooked power to legalize federal crime. Vanderbilt Law Rev. 2009;62:1421–1482. [Google Scholar]
- Nelson CB, Rehm J, Ustun TB, Grant B, Chatterji S. Factor structures for DSM-IV substance disorder criteria endorsed by alcohol, cannabis, cocaine and opiate users: results from the WHO reliability and validity study. Addiction. 1999;94:843–855. doi: 10.1046/j.1360-0443.1999.9468438.x. [DOI] [PubMed] [Google Scholar]
- Nielsen AL. Americans’ attitudes toward drug-related issues from 1975-2006: the roles of period and cohort effects. J. Drug Issues. 2010;40:461–493. [Google Scholar]
- Norberg K, Bierut L, Grucza R. Long-term effects of minimum drinking age laws on past-year alcohol and drug use disorders. Alcohol. Clin. Exp. Res. 2009;33:2180–2190. doi: 10.1111/j.1530-0277.2009.01056.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of Applied Studies . Results from the 2007 National Survey on Drug Use and Health: National findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2008. DHHS Publication No SMA 08-4343, NSDUH Series H-34. [Google Scholar]
- Pacula R, Kilmer B, Grossman M, Chaloupka F. Risks and prices: the role of user sanctions in marijuana markets. BE J. Econ. Anal. Policy. 2010;10:1–10. doi: 10.2202/1935-1682.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park D, Gelman A, Bafumi J. Bayesian multilevel estimation with poststratification: state-level estimates from national polls. Polit. Anal. 2004;12:375–385. [Google Scholar]
- Pedersen W, Skardhamar T. Cannabis and crime: findings from a longitudinal study. Addiction. 105:109–118. doi: 10.1111/j.1360-0443.2009.02719.x. [DOI] [PubMed] [Google Scholar]
- 2011 Procon.org. Medical Marijuana accessed in 2011.
- Pull CB, Saunders JB, Mavreas V, Cottler LB, Grant BF, Hasin DS, Blaine J, Mager D, Ustun BT. Concordance between ICD-10 alcohol and drug use disorder criteria and diagnoses as measured by the AUDADIS-ADR, CIDI and SCAN: results of a cross-national study. Drug Alcohol Depend. 1997;47:207–216. doi: 10.1016/s0376-8716(97)00091-4. [DOI] [PubMed] [Google Scholar]
- Saha T, Chou S, Grant BF. Toward an alcohol use disorder continuum using item response theory: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol. Med. 2006;36:931–941. doi: 10.1017/S003329170600746X. [DOI] [PubMed] [Google Scholar]
- Scott R. The limits of behavioral theories of law and social norms. VA Law Rev. 2000;86:1603–1647. [Google Scholar]
- Simons-Morton B, Pickett W, Boyce W, ter Bogt TFM, Vollebergh W. Cross-national comparison of adolescent drinking and cannabis use in the United States, Canada, and the Netherlands. Int. J. Drug Policy. 2010;21:64–69. doi: 10.1016/j.drugpo.2009.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Single EW. The impact of marijuana decriminalization: an update. J. Public Health Policy. 1989;10:456–466. [PubMed] [Google Scholar]
- Skog OJ. The collectivity of drinking cultures - a theory of the distribution of alcohol consumption. Br. J. Addiction. 1985;80:83–99. doi: 10.1111/j.1360-0443.1985.tb05294.x. [DOI] [PubMed] [Google Scholar]
- Subramanian S, Kawachi I. Income inequality and health: what have we learned so far? Epidemiol. Rev. 2004;26:78–91. doi: 10.1093/epirev/mxh003. [DOI] [PubMed] [Google Scholar]
- Taylor DR, Poulton R, Moffitt TE, Ramankutty P, Sears MR. The respiratory effects of cannabis dependence in young adults. Addiction. 2000;95:1669–1677. doi: 10.1046/j.1360-0443.2000.951116697.x. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services [Accessed in 2011];Office of Applied Studies, National Survey on Drug Use and Health, State level data on alcohol, tobacco, and illegal drug use. http://www.oas.samhsa.gov/states.cfm. [Google Scholar]
- Ustun B, Compton W, Mager D, Babor T, Baiyewu O, Chatterji S, Cottler L, Gogus A, Mavreas V, Peters L, Pull C, Saunders J, Smeets R, Stipec MR, Vrasti R, Hasin D, Room R, Van den Brink W, Regier D, Blaine J, Grant BF, Sartorius N. WHO Study on the reliability and validity of the alcohol and drug use disorder instruments: overview of methods and results. Drug Alcohol Depend. 1997;47:161–169. doi: 10.1016/s0376-8716(97)00087-2. [DOI] [PubMed] [Google Scholar]
- van den Brink W. Forum: decriminalization of cannabis. Curr. Opin. Psychiatr. 2008;21:122–126. doi: 10.1097/YCO.0b013e3282f57e04. [DOI] [PubMed] [Google Scholar]
- Vrasti R, Grant BF, Chatterji S, Ustun BT, Mager D, Olteanu I, Badoi M. Reliability of the Romanian version of the alcohol module of the WHO Alcohol Use Disorder and Associated Disabilities: interview schedule --Alcohol/Drug-Revised. Eur. Addict. Res. 1998;4:144–149. doi: 10.1159/000018947. [DOI] [PubMed] [Google Scholar]
- Wodak A. For and against - cannabis control: costs outweigh the benefits - For. Br. Med. J. 2002;324:105–106. doi: 10.1136/bmj.324.7329.105. [DOI] [PMC free article] [PubMed] [Google Scholar]