This report describes a case of diabetic myonecrosis in a patient with long standing diabetes mellitus (DM). This is a rare, possibly under-recognized complication of a common disease. This is a self-limiting complication and requires only conservative management. Failure to recognize this condition can result in significant morbidity. Physicians should always consider this entity in the differential diagnosis of acute muscle pain in a patient with DM.
Diabetes mellitus (DM) and its complications is a global challenge to health care systems. Ischemic heart disease, peripheral vascular disease, nephropathy and retinopathy are well recognized complications. Diabetic myonecrosis or diabetic muscle infarct (DMI) is a rare complication of diabetes or possibly under diagnosed. It is described in longstanding diabetes. Although it was first reported in 1965, only case reports and a systemic review of these cases have been published.1,2 It was also reported in some cases as the first manifestation of DM. Clinical presentation is with acute onset of muscle pain, commonly the thigh. Diabetes myonecrosis can be misdiagnosed as cellulitis, deep vein thrombosis or facsiatis. Magnetic resonance imaging (MRI) is sufficient, in the appropriate clinical context, to enable the diagosis, hence avoiding inappropriate treatment.3
A 57 year old female known to have past medical history of diabetes mellitus and hypertension for more then 20 years, on regular treatment with metformin, repaglinide, atenolol and amlodipine is described in this report. The patient developed severe excruciating left thigh pain and swelling for which she presented to a private clinic. The pain started 10 days before the presentation and worsened to the extent of limiting her activity to bed rest.
At the private clinic, she had Doppler ultrasound of the thigh which reported no evidence of deep vein thrombosis. She was started on anticoagulation with Low Molecular Weight Heparin(LMWH) followed by warfarin for presumed superficial thrombophlebitis. In addition she was treated with an antibiotic (augmentin) and NSAID to control her pain.
The pain persisted and she developed fever. The patient went back to the same clinic and was found to have a deterioration in renal function, with a creatinine of 590u/L, urea 30mmol/L, potassium 6.7mmol/L and bicarbonate of 13mmol/L. Her creatinine level was 135micromol/l at the first visit to the clinic. She was referred to the Sultan Qaboos University hospital for further evaluation and management of acute renal injury. The patient denied experiencing muscle trauma, skin breakdown or muscle weakness. Local examination revealed swelling and marked tenderness of left anteriomedial aspect of the thigh. The skin was warm but not erythematous. The patient had low grade fever of 37.8°C and her blood pressure was 156/72 mmHg. There were no muco-cutaneous, joint or systemic abnormal signs.
Laboratory studies for leukocyte, platelet, and eosinophil counts, C3, C4, ANA, hepatitis B surface antigen, and hepatitis C antibody yielded normal or negative findings. However, the patient had elevated ESR 116 and CK 168 U/L. Urine and blood cultures reported no growth. Chest x-ray was remarkable for mild cardiomegally. The patient remained oligouric despite initial fluid resuscitation and hemodialysis was started in addition to treatment with analgesics and antibiotic. The treatment with anticoagulants was stopped. MRI of the left thigh was performed and suggested myonecrosis of the vastus lateralis.
The patient was diagnosed with diabetic myonecrosis. The pain gradually subsided with conservative measures and bed rest. Treatment with analgesics was continued but the antibiotic was discontinued 3 days after her admission when her cultures reported no growth. At the time of hospital discharge, the patient was able to walk and her thigh pain had improved significantly. Dialysis was discontinued before the hospital discharge. Renal function improved but not to her baseline creatinine. Her creatinine at her last follow up visit, 2 months following her admission was 300micromol/L.
The patient reported here had long standing DM with nephropathy evident by then elevated baseline creatinine. She was presented with clinical manifestation typical of what is described, in case reports, as diabetic myonecrosis or muscle infarction. This condition is described more in women. Although the exact pathogenesis is unknown, it is assumed to be the microvasculer complication of longstanding DM. The typical clinical presentation include abrupt onset of pain in involved muscle. The most commonly involved muscles are of the thigh, but calf muscles can also be affected.4 Often, there is palpable mass and swelling with or without systemic signs. The pain usually persists for weeks then spontaneously resolves. Recurrent episodes have also been reported.
DMI needs to be differentiated from other common painful conditions that cause acute leg pain in a diabetic patient, including deep venous thrombosis, soft tissue abscess, haematoma, inflammatory myositis. Physician’s awareness should allow early diagnosis on the basis of clinical presentation, laboratory test and imaging, thereby avoiding biopsy and its potential complication.
MRI plays an important role in the diagnosis. The main findings associated with Diabetic muscle Infarction, DMI, are increased signal intensity of the muscles involved on T2 weighted images. The affected muscles are either isointense or hypointense on T1 weighted images. Foci of increased signal intensity on T1 weighted images may suggest focal hemorrhages. The affected muscles show modest amount of enhancement after administration of intravenous gadolinium. The enhancing muscles and fascia are almost always hyperintense on T2 weighted images. Areas within the muscles which show rim enhancement correspond to area of muscle infarction or necrosis within the ischemic muscle. Subcutaneous edema and subfascial fluid are commonly seen on the T2-weighted and inversion-recovery images.5-7
Sonographic findings of diabetic muscle infarction include internal linear echogenic structures coursing through the lesion; an absence of internal motion or swirling of fluid with transducer pressure; and a lack of a predominately anechoic area. These sonographic characteristics may help differentiate diabetic muscle infarction from abscess or necrotic tumor.8
Diabetic muscle infarction is frequently bilateral and the thigh is the most common site of involvement (81-87%) of the reposted cases. Although any of the muscles of the thigh may be involved, the musculi vastus were the most frequently affected.6The second most commonly affected site is the calf muscles.
The radiological differential diagnosis of diabetic muscle infarction includes soft-tissue abscess, pyomyositis, necrotizing fasciitis, and other causes of myositis. Necrotizing fasciitis is the major differential consideration that may not be distinguishable from diabetic muscle infarction on the basis of only MR imaging findings. Patients with necrotizing fasciitis are more likely to have fever, cellulitis, and an elevated peripheral white blood cell count. Severe pain is very characteristic of diabetic muscle infarction and may not be seen with necrotizing fasciitis or pyomyositis.9 Therefore, the diagnosis of diabetic muscle infarction remains a clinical and radiographic diagnosis.
Diabetes myonecrosis is a self-limiting disease, full recovery is expected overtime in most of the cases. Only general management is required including bed rest and analgesics. As a possible microvasculer complication antiplatelets could theoretically be effective. Tight glycemic control and cessation of smoking is prudent. Excisional biopsy, early debridement and mobility have lead to complications and delayed recovery.10
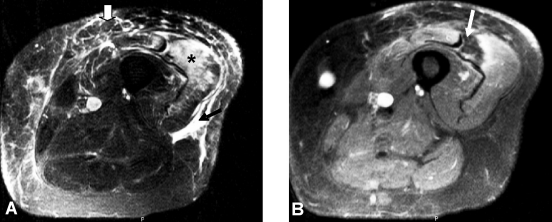
Figure 1.
A) Axial fat-suppressed T2-weighted image shows enlargement and increase signal intensity of the vastus lateralis muscles (*) and rectus femoris (open white arrow). There is fluid in subcutaneous tissue and intermuscular fascia (black arrow). B) Axial fat-suppressed gadolinium-enhance T1-weighted image shows areas of diffuse enhancement of the vastus lateralis and rectus femoris. There is focal rim enhancement with a low-signal-intensity center within the vastus lateralis (white arrow) suggestive of muscle necrosis.
Conclusion
Diabetic-associated muscle necrosis is an uncommon clinical entity. However, the incidence is likely to increase because of increasing global prevalence of diabetes. Physicians should always consider this entity in differential diagnosis of acute muscle pain in a diabetic patient. An early noninvasive diagnosis is possible by performing an MRI. Subsequent to reporting this case at the hospital, two more cases of diabetic myonecrosis were readily diagnosed in less then three months. Diabetic myonecrosis requires conservative management and minimal intervention to avoid complications and prolonged hospitalization. Biopsy is rarely indicated and if possible better avoided.
Acknowledgements
The authors reported no conflict of interest and no funding has been received on this work.
References
- 1.Angervall L, Stener B. Tumoriform focal muscular degeneration in two diabetic patients. Diabetologia 1965;1:39-42 . 10.1007/BF01338714 [DOI] [Google Scholar]
- 2.Trujillo-Santos AJ. Diabetic muscle infarction: an underdiagnosed complication of long-standing diabetes. Diabetes Care 2003. Jan;26(1):211-215 10.2337/diacare.26.1.211 [DOI] [PubMed] [Google Scholar]
- 3.Kattapuram TM, Suri R, Rosol MS, Rosenberg AE, Kattapuram SV. Idiopathic and diabetic skeletal muscle necrosis: evaluation by magnetic resonance imaging. Skeletal Radiol 2005. Apr;34(4):203-209 10.1007/s00256-004-0881-8 [DOI] [PubMed] [Google Scholar]
- 4.Umpierrez GE, Stiles RG, Kleinbart J, Krendel DA, Watts NB. Diabetic muscle infarction. Am J Med 1996. Sep;101(3):245-250 10.1016/S0002-9343(96)00156-8 [DOI] [PubMed] [Google Scholar]
- 5.Chason DP, Fleckenstein JL, Burns DK, Rojas G. Diabetic muscle infarction: radiologic evaluation. Skeletal Radiol 1996. Feb;25(2):127-132 10.1007/s002560050048 [DOI] [PubMed] [Google Scholar]
- 6.Jelinek JS, Murphey MD, Aboulafia AJ, Dussault RG, Kaplan PA, Snearly WN. Muscle infarction in patients with diabetes mellitus: MR imaging findings. Radiology 1999. Apr;211(1):241-247 [DOI] [PubMed] [Google Scholar]
- 7.Khoury NJ, el-Khoury GY, Kathol MH. MRI diagnosis of diabetic muscle infarction: report of two cases. Skeletal Radiol 1997. Feb;26(2):122-127 10.1007/s002560050205 [DOI] [PubMed] [Google Scholar]
- 8.Delaney-Sathy LO, Fessell DP, Jacobson JA, Hayes CW. Sonography of diabetic muscle infarction with MR imaging, CT, and pathologic correlation. AJR Am J Roentgenol 2000. Jan;174(1):165-169 [DOI] [PubMed] [Google Scholar]
- 9.Schmid MR, Kossmann T, Duewell S. Differentiation of necrotizing fasciitis and cellulitis using MR imaging. AJR Am J Roentgenol 1998. Mar;170(3):615-620 [DOI] [PubMed] [Google Scholar]
- 10.Kapur S, McKendry RJ. Treatment and outcomes of diabetic muscle infarction. J Clin Rheumatol 2005. Feb;11(1):8-12 10.1097/01.rhu.0000152142.33358.f1 [DOI] [PubMed] [Google Scholar]