Abstract
Since 2001, the World Health Organization classification for hematopoietic and lymphoid neoplasms has provided a framework for defining acute leukemia (AL) subtypes, although few population-based studies have assessed incidence patterns and patient survival accordingly. We assessed AL incidence rates (IRs), IR ratios (IRRs), and relative survival in the United States (2001-2007) in one of the first population-based, comprehensive assessments. Most subtypes of acute myeloid leukemia (AML) and acute lymphoblastic leukemia/lymphoma (ALL/L) predominated among males, from twice higher incidence of T-cell ALL/L among males than among females (IRR = 2.20) to nearly equal IRs of acute promyelocytic leukemia (APL; IRR = 1.08). Compared with non-Hispanic whites, Hispanics had significantly higher incidence of B-cell ALL/L (IRR = 1.64) and APL (IRR = 1.28); blacks had lower IRs of nearly all AL subtypes. All ALL/L but only some AML subtypes were associated with a bimodal age pattern. Among AML subtypes, survival was highest for APL and AML with inv(16). B-cell ALL/L had more favorable survival than T-cell ALL/L among the young; the converse occurred at older ages. Limitations of cancer registry data must be acknowledged, but the distinct AL incidence and survival patterns based on the World Health Organization classification support biologic diversity that should facilitate etiologic discovery, prognostication, and treatment advances.
Introduction
Acute leukemias (ALs) account for ∼ 20 000 cancer diagnoses and 10 000 deaths annually in the United States,1 but the etiology of most ALs remains unknown.2 Descriptive epidemiologic studies can provide insight into etiology, identify susceptible populations, and provide information about patient survival in the general population, but to be informative are reliant on reproducible classification systems that allow for precise diagnoses. The World Health Organization (WHO) developed a consensus-based classification for hematopoietic and lymphoid neoplasms that defines distinct diseases by incorporating information on cell lineage, morphology, immunophenotype, and clinical and genetic features.3 Since its introduction in 2001 and update in 2008, the WHO classification has provided a framework for reproducibly defining hematopoietic and lymphoid entities worldwide.3,4
Although a few population-based studies recently have analyzed the incidence of AL using the WHO classification, none have included data beyond 20025,6 or characterized both incidence and survival by subtypes of AL. Despite limitations in cancer registry data, such as lack of centralized pathology review and potentially more limited diagnostic evaluation in the general population than in clinical trials, other studies using population-based cancer registries have successfully assessed patterns of hematologic malignancies and related disorders using various disease classification schemes for these neoplasms.5–8 Therefore, we sought to substantially extend initial population-based reports and provide the first comprehensive assessment of childhood and adult AL incidence and patient survival in the United States, guided by the WHO classification. We include AL cases diagnosed during 2001 to 2007, thereby maximizing the proportion likely to have been characterized with immunophenotyping and cytogenetic studies and treated with modern therapies and supportive care. An important clinical and public health objective of our population-based analysis was to identify whether subtype-specific incidence rates suggested biologic differences, etiologic differences, or both and to identify whether opportunities exist for improving diagnostic assessment and therapeutic interventions for particular subpopulations with AL.
Methods
We analyzed cases of AL diagnosed among residents of 17 population-based cancer registry areas of the Surveillance, Epidemiology and End Results (SEER) Program (SEER-17) during 2001 to 2007.9 SEER-17 registries cover ∼ 26% of the US population, including 8 states (Connecticut, Hawaii, Iowa, Kentucky, Louisiana, New Jersey, New Mexico, and Utah), 6 metropolitan areas (Atlanta, GA; Detroit, MI; Los Angeles, San Francisco–Oakland, and San Jose–Monterey, CA; and Seattle–Puget Sound, WA), the areas of greater California and rural Georgia, and the Alaska Native Tumor Registry.
Leukemia classification
Our analysis is limited to ALs defined in the third edition of the International Classification of Diseases for Oncology (ICD-O-3), which was implemented in the SEER Program for cancer cases diagnosed in 2001 and remains in use in 2011. We classified cases first according to cell lineage, considering separately the incidence of acute myeloid leukemia (AML), acute (precursor) lymphoblastic leukemia/lymphoma (ALL/L), and AL of ambiguous lineage.
The broad category of AML included ICD-O-3 morphology codes M-9840, 9861, 9866-9867, 9870-9874, 9891, 9895-9897, 9910, 9920, 9930-9931, and 9987 (Table 1; Figure 1). Guided by the WHO classification, we considered individual AML subtypes (specified in Table 2), including “group 1” (AML, not otherwise specified [NOS] and related entities, including myeloid sarcoma), “group 2” (entities with associated cytogenetic abnormalities), and “group 3” (AML with myelodysplasia-related changes and therapy-related myeloid neoplasms, including therapy-related myelodysplastic syndrome [MDS], NOS since the 2008 WHO classification considers therapy-related AML [t-AML] and therapy-related MDS [t-MDS] as a single biologic entity).4 All morphology codes for ALL/L (M-9727-9729, 9835-9837; Table 1; Figure 1) were newly introduced with ICD-O-3. We considered ALL/L subtypes with similar immunophenotypic characteristics (B cell, T cell) within the same category, based on the premise that the WHO considers leukemias and lymphomas different manifestations of the same disease.3,4 We were able to further classify ALL/L of unknown lineage (M-9727, 9835) into B-cell or T-cell subtype based on available immunophenotyping information (specified in Table 2). We considered acute undifferentiated leukemia (M-9801) and acute biphenotypic leukemia (M-9805) within the category of AL of ambiguous lineage (specified in Table 2).
Table 1.
Age-adjusted IRs and IRRs of AML and ALL/L according to race/ethnicity and age, SEER-17, 2001 to 2007
| AML |
ALL/L |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | IR | IRR | 95% CI | No. | % | IR | IRR | 95% CI | |
| Total | 19 497 | 100 | 38.0 | NA | 9 188 | 100 | 17.3 | NA | ||
| Race/ethnicity | ||||||||||
| Non-Hispanic whites | 14 177 | 72.7 | 39.9 | 1.00 | 4 761 | 51.8 | 16.6 | 1.00 | ||
| Hispanic whites | 2 216 | 11.4 | 32.3 | 0.81 | 0.77-0.85 | 2 907 | 31.6 | 24.9 | 1.50 | 1.43-1.58 |
| Blacks | 1 492 | 7.7 | 32.0 | 0.80 | 0.76-0.85 | 644 | 7.0 | 10.2 | 0.61 | 0.56-0.67 |
| APIs | 1 439 | 7.4 | 32.3 | 0.81 | 0.76-0.85 | 715 | 7.8 | 14.8 | 0.89 | 0.82-0.96 |
| Other/unspecified | 173 | 0.9 | ∼ | ∼ | 161 | 1.8 | ∼ | ∼ | ||
| Age, y | ||||||||||
| < 1 | 154 | 0.8 | 19.9 | 1.00 | 163 | 1.8 | 21.1 | 1.00 | ||
| 1-4 | 297 | 1.5 | 9.9 | 0.50 | 0.41-0.61 | 2 357 | 25.7 | 78.7 | 3.74 | 3.19-4.41 |
| 5-19 | 840 | 4.3 | 7.3 | 0.37 | 0.31-0.44 | 3 004 | 32.7 | 26.3 | 1.25 | 1.07-1.47 |
| 20-39 | 1 869 | 9.6 | 12.3 | 0.62 | 0.53-0.74 | 1 329 | 14.5 | 8.6 | 0.41 | 0.35-0.49 |
| 40-59 | 4 505 | 23.1 | 30.4 | 1.53 | 1.30-1.81 | 1 189 | 12.9 | 8.1 | 0.39 | 0.33-0.46 |
| 60-74 | 5 588 | 28.7 | 109.2 | 5.49 | 4.68-6.48 | 711 | 7.7 | 13.7 | 0.65 | 0.55-0.78 |
| ≥ 75 | 6 244 | 32.0 | 208.9 | 10.50 | 8.95-12.41 | 435 | 4.7 | 14.7 | 0.70 | 0.58-0.84 |
All IRs are age-adjusted to the 2000 US standard population and expressed per 1 000 000 person-years. IRRs are based on unrounded rates.
NA indicates not applicable; APIs, Asians/Pacific Islanders; and ∼, IRs and IRRs not calculated for other/unspecified race.
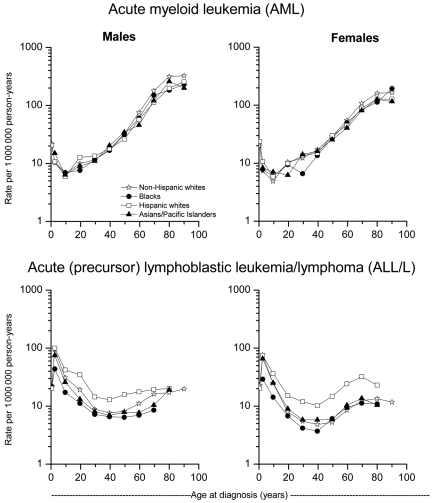
Figure 1.
Age-specific IRs of AML and ALL/L. Age-specific IRs of AML and ALL/L according to sex and race/ethnicity, SEER-17, 2001 to 2007.
Table 2.
Age-adjusted IRs and IRRs of AML, ALL/L, and AL of ambiguous lineage according to subtype and sex, SEER-17, 2001 to 2007
| Total |
Male |
Female |
Male-to-female |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | IR | Median age, y | No. | IR | No. | IR | IRR | 95% CI | |
| AML* | 19 497 | 100 | 38.0 | 66 | 10 590 | 46.8 | 8 907 | 31.6 | 1.48 | 1.44-1.52 |
| Subtype | ||||||||||
| Group 1 | 15 764 | 80.9 | 30.8 | 67 | 8 580 | 38.3 | 7 184 | 25.4 | 1.51 | 1.46-1.55 |
| AML, NOS; [M-9861] | 8 559 | 43.9 | 16.8 | 70 | 4 689 | 21.3 | 3 870 | 13.6 | 1.57 | 1.50-1.64 |
| AML with minimal differentiation; (FAB M0) [M-9872] | 770 | 3.9 | 1.5 | 67 | 432 | 1.9 | 338 | 1.2 | 1.60 | 1.38-1.85 |
| AML without maturation; (FAB M1) [M-9873] | 1 081 | 5.5 | 2.1 | 63 | 566 | 2.4 | 515 | 1.9 | 1.32 | 1.17-1.49 |
| AML with maturation; (FAB M2) [M-9874] | 1 254 | 6.4 | 2.4 | 66 | 647 | 2.9 | 607 | 2.2 | 1.33 | 1.19-1.49 |
| Acute myelomonocytic leukemia; (FAB M4) [M-9867] | 1 771 | 9.1 | 3.4 | 64 | 976 | 4.2 | 795 | 2.8 | 1.50 | 1.36-1.65 |
| Acute monoblastic and monocytic leukemia; (FAB M5) [M-9891] | 1 465 | 7.5 | 2.8 | 62 | 769 | 3.3 | 696 | 2.5 | 1.34 | 1.20-1.48 |
| Acute erythroid leukemia; (FAB M6) [M-9840] | 344 | 1.8 | 0.7 | 68 | 213 | 1.0 | 131 | 0.5 | 2.05 | 1.64-2.57 |
| Acute megakaryoblastic leukemia; (FAB M7) [M-9910] | 209 | 1.1 | 0.4 | 39 | 113 | 0.5 | 96 | 0.4 | 1.32 | 1.00-1.76 |
| Acute basophilic leukemia; [M-9870] | 5 | < 0.1 | ∼ | 71 | 2 | ∼ | 3 | ∼ | ∼ | |
| Acute panmyelosis with myelofibrosis; [M-9931] | 133 | 0.7 | 0.3 | 67 | 71 | 0.3 | 62 | 0.2 | 1.39 | 0.97-2.00 |
| Myeloid sarcoma; [M-9930] | 173 | 0.9 | 0.3 | 59 | 102 | 0.4 | 71 | 0.3 | 1.67 | 1.22-2.30 |
| Group 2 | 2 089 | 10.7 | 4.0 | 48 | 1 075 | 4.3 | 1 014 | 3.7 | 1.16 | 1.06-1.27 |
| AML with t(8;21); (FAB M2, t(8;21)) [M-9896] | 313 | 1.6 | 0.6 | 52 | 178 | 0.7 | 135 | 0.5 | 1.49 | 1.18-1.88 |
| AML with inv(16) or t(16;16); (FAB M4Eo) [M-9871] | 203 | 1.0 | 0.4 | 47 | 109 | 0.4 | 94 | 0.3 | 1.26 | 0.94-1.68 |
| APL with t(15;17); (FAB M3) [M-9866] | 1 440 | 7.4 | 2.7 | 47 | 721 | 2.9 | 719 | 2.6 | 1.08 | 0.97-1.20 |
| AML, 11q23 abnormalities; [M-9897] | 133 | 0.7 | 0.3 | 61 | 67 | 0.3 | 66 | 0.2 | 1.24 | 0.87-1.77 |
| Group 3 | 1 644 | 8.4 | 3.2 | 69 | 935 | 4.2 | 709 | 2.5 | 1.69 | 1.53-1.87 |
| AML with myelodysplasia-related changes; [M-9895] | 1 191 | 6.1 | 2.4 | 71 | 731 | 3.4 | 460 | 1.6 | 2.08 | 1.84-2.34 |
| Therapy-related myeloid neoplasms; [M-9920, 9987] | 453 | 2.3 | 0.9 | 63 | 204 | 0.9 | 249 | 0.9 | 0.99 | 0.82-1.20 |
| ALL/L* | 9 188 | 100 | 17.3 | 14 | 5 248 | 19.7 | 3 940 | 14.8 | 1.33 | 1.28-1.39 |
| Subtype | ||||||||||
| B-cell lymphoblastic leukemia/lymphoma; [M-9727(B), 9728, 9835(B), 9836] | 6 213 | 67.6 | 11.7 | 12 | 3 392 | 12.7 | 2 821 | 10.6 | 1.20 | 1.14-1.26 |
| T-cell lymphoblastic leukemia/lymphoma; [M-9727(T), 9729, 9835(T), 9837] | 1 396 | 15.2 | 2.6 | 18 | 965 | 3.6 | 431 | 1.6 | 2.20 | 1.96-2.47 |
| Lymphoblastic leukemia/lymphoma, unknown lineage; [M-9727(U), 9835(U)] | 1 579 | 17.2 | 3.0 | 12 | 891 | 3.4 | 688 | 2.6 | 1.34 | 1.21-1.48 |
| AL of ambiguous lineage* | 997 | 100 | 2.0 | 73 | 546 | 2.5 | 451 | 1.6 | 1.63 | 1.43-1.85 |
| Subtype | ||||||||||
| Acute undifferentiated leukemia; [M-9801] | 825 | 82.7 | 1.6 | 75 | 443 | 2.1 | 382 | 1.3 | 1.61 | 1.40-1.86 |
| Acute biphenotypic leukemia; [M-9805] | 172 | 17.3 | 0.3 | 53 | 103 | 0.4 | 69 | 0.3 | 1.71 | 1.24-2.36 |
All incidence rates are age-adjusted to the 2000 US standard population and expressed per 1 000 000 person-years. Incidence rate ratios are based on unrounded rates.
FAB indicates French-American-British classification; (B), B-cell immunophenotype; (T), T-cell immunophenotype; (U), immunophenotype not specified; and ∼, IRs not calculated for fewer than 10 cases.
Includes all ICD-O-3 morphology codes specified within the respective subtype categories. ICD-O-3 codes are specified within brackets.
Incidence
We calculated age-adjusted incidence rates (IRs) per 1 000 000 person-years, IR ratios (IRRs), and 95% confidence intervals (CIs) using the Incidence Rate Session in SEER*Stat Version 6.5.2 (www.seer.cancer.gov). All IRs were age-adjusted to the 2000 US standard population. We excluded from analysis 4.8% of cases (n = 1485) that were not specified to be microscopically confirmed, of which 66.3%, 9.8%, and 24.0% were classified as AML, ALL/L, and AL of ambiguous lineage, respectively. We included in our analysis all cases of AL, whether diagnosed as a first primary or subsequent malignancy. Of note, however, before 2010, the SEER Program did not collect information on AL that developed subsequent to a diagnosis of another leukemia (eg, AL after chronic myelogenous leukemia), MDS, or myeloproliferative neoplasm.
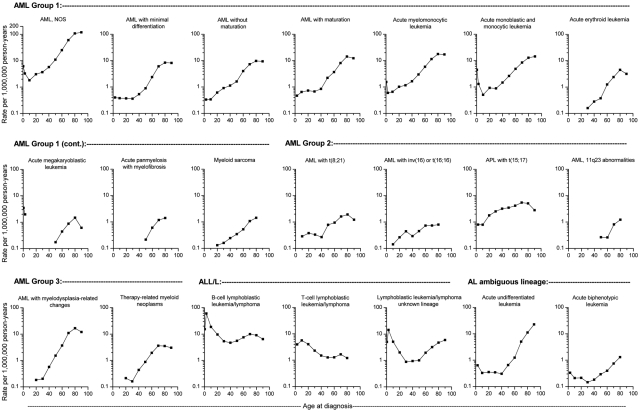
IRs were calculated overall and according to sex (male, female), age (< 1, 1-4, 5-19, 20-39, 40-59, 60-74, and ≥ 75 years), race/ethnicity (non-Hispanic whites, Hispanic whites, blacks, Asians/Pacific Islanders [APIs], and other/unspecified), calendar year, and leukemia subtype (specified in Table 2). Age-specific IRs were plotted on a log-linear scale using the midpoint of each specified age group (< 1, 1-4, 5-14, 15-24, 25-34, 35-44, 45-54, 55-64, 65-74, 75-84, and ≥ 85 years). IRs based on fewer than 10 cases are not shown in the tables and figures, similar to international convention.
Survival
To evaluate patient survival after a diagnosis of AL, we restricted the cohort to patients diagnosed during 2001 to 2006 (rather than 2007) and followed them for vital status through 2007 (n = 25 428). We excluded cases of AL diagnosed as a second or later primary cancer (n = 3921) or during July to December 2005 in Louisiana because of population displacement from Hurricane Katrina (n = 93), reported only by death certificate or autopsy (n = 10), with unknown age (n = 1), or with unknown survival time (n = 64). Through active tracing, the SEER Program has been successful in attaining more than 97% follow-up for vital status.
Cause-specific survival is a measure of net survival in the absence of other causes of death; observed survival is the probability of surviving all causes of death for a specified interval; and relative survival (RS) is the ratio of the proportion of observed to expected survivors in a comparable cohort of the general population. We focused our analysis on RS that is not reliant on a potentially inaccurate cause of death, accounts for the underlying disease process or ensuing associated complications, and provides a basis for comparison in the general population. The actuarial method in the SEER*Stat Survival Session was used to estimate 1- and 5-year RS and 95% CIs using monthly intervals. RS was calculated according to leukemia subtype and 4 age groups (< 20, 20-39, 40-59, and ≥ 60 years). We further divided the younger (< 1, 1-4, 5-19 years, or < 5, 5-19 years) and older (40-49, 50-59, 60-69, 70-79, and ≥ 80 years) age groups when the number of cases allowed. According to SEER Program convention, RS estimates based on fewer than 25 cases are not shown.
Results
Incidence
Overall AL patterns by sex, race, and age.
During 2001 to 2007, 29 682 individuals (IR = 57.2 per 1 000 000 person-years) were diagnosed with AL in SEER-17. Overall, AML accounted for 65.7% of cases (n = 19 497; IR = 38.0); ALL/L, 31.0% (n = 9,188; IR = 17.3); and AL of ambiguous lineage, 3.4% (n = 997; IR = 2.0). AML IRs were remarkably similar among Hispanic whites, blacks, and APIs (IR = 32.0-32.3), with rates for each racial/ethnic subgroup ∼ 20% lower than among non-Hispanic whites (IR = 39.9; Table 1). AML IRs demonstrated a bimodal age pattern, with an initial peak among infants (< 1 year, IR = 19.9), a decline in childhood, and then an exponential rise in IR with advancing age beginning in young adulthood (Table 1; Figure 1). Among blacks and APIs, the initial age peak occurred at 1 to 4 years; thereafter, IRs nadired at a slightly younger age among blacks and API males than API females. IRs for ALL/L followed different patterns by race/ethnicity and age. Hispanic whites had the highest incidence of ALL/L (IR = 24.9), which was 50% higher than the incidence among non-Hispanic whites; blacks had the lowest incidence of ALL/L (IR = 10.2), and non-Hispanic whites and APIs had intermediate IRs. ALL/L also was associated with a bimodal age pattern, but unlike AML, the initial age peak occurred among children 1 to 4 years of age with a decline at ages 20 to 59 years, followed by a modest rise in IRs at ages ≥ 60 years. The ALL/L predominance among Hispanic whites was absent in infants but was noted across virtually all older age groups.
AL subtypes and sex.
Incidence of AML was 48% higher among males than females, with a male predominance noted for all 3 AML groups (Table 2). With the exception of therapy-related myeloid neoplasms, which occurred approximately equally among males and females (male-to-female IRR = 0.99), all other AML subtypes had higher IRs among males, with male-to-female IRRs ranging from 1.08 for acute promyelocytic leukemia (APL) with t(15;17) to greater than 2.0 for AML with myelodysplasia-related changes and acute erythroid leukemia. APL with t(15;17) IRs were ∼ 20% lower among men than women up through ages 25 to 34 years, and at older ages IRs were generally higher among males (data not shown); however, only among the 75- to 84-year age group (male-to female IRR = 1.66; 95% CI, 1.12%-2.47%) did IRs for APL with t(15;17) differ significantly by sex. Similar to AML, ALL/L also was associated with higher IRs among males than females (IRR = 1.33). The male-to-female IRR for T-cell ALL/L was 2.20, significantly greater than that for B-cell ALL/L (IRR = 1.20) or ALL/L of unknown lineage (IRR = 1.34).
AL subtypes and race.
Compared with non-Hispanic whites, IRs of most AML and ALL/L subtypes were lower among Hispanic whites, blacks, and APIs (Table 3). Notable exceptions included significantly higher IRs for APL with t(15;17), B-cell/ALL/L, and ALL/L of unknown lineage among Hispanic whites compared with non-Hispanic whites (Hispanic white-to-non-Hispanic white IRR of 1.28, 1.64, and 1.49, respectively). Although differences were not significant, AML with inv(16) and acute biphenotypic leukemia IRs were more than 10% higher among Hispanic whites than non-Hispanic whites; acute megakaryoblastic leukemia and acute undifferentiated leukemia IRs were more than 10% higher among blacks than non-Hispanic whites; and acute megakaryoblastic leukemia, AML with t(8;21), and AML with 11q23 abnormalities IRs were more than 10% higher among APIs than non-Hispanic whites.
Table 3.
Age-adjusted IRs and IRRs of AML, ALL/L, and AL of ambiguous lineage according to subtype and race/ethnicity, SEER-17, 2001 to 2007
| NHWs |
HWs |
Blacks |
APIs |
IRR |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HWs:NHWs |
Blacks:NHWs |
APIs:NHWs |
||||||||||||
| No. | IR | No. | IR | No. | IR | No. | IR | IRR | 95% CI | IRR | 95% CI | IRR | 95% CI | |
| AML* | 14 177 | 39.9 | 2 216 | 32.3 | 1 492 | 32.0 | 1 439 | 32.3 | 0.81 | 0.77-0.85 | 0.80 | 0.76-0.85 | 0.81 | 0.76-0.85 |
| Subtype | ||||||||||||||
| Group 1 | 11 580 | 32.4 | 1 683 | 25.6 | 1 210 | 26.4 | 1 150 | 26.0 | 0.79 | 0.75-0.84 | 0.82 | 0.77-0.87 | 0.80 | 0.75-0.85 |
| AML, NOS; [M-9861] | 6 355 | 17.6 | 821 | 13.6 | 719 | 16.1 | 583 | 13.5 | 0.77 | 0.71-0.84 | 0.91 | 0.84-0.99 | 0.77 | 0.70-0.84 |
| AML with minimal differentiation; (FAB M0) [M-9872] | 552 | 1.6 | 85 | 1.2 | 67 | 1.5 | 59 | 1.3 | 0.77 | 0.59-0.99 | 0.93 | 0.71-1.21 | 0.85 | 0.63-1.11 |
| AML without maturation; (FAB M1) [M-9873] | 764 | 2.2 | 145 | 2.1 | 62 | 1.3 | 102 | 2.2 | 0.97 | 0.79-1.18 | 0.59 | 0.44-0.77 | 1.03 | 0.83-1.27 |
| AML with maturation; (FAB M2) [M-9874] | 910 | 2.6 | 142 | 2.1 | 80 | 1.8 | 113 | 2.5 | 0.81 | 0.66-0.98 | 0.69 | 0.54-0.88 | 0.97 | 0.79-1.18 |
| Acute myelomonocytic leukemia; (FAB M4) [M-9867] | 1 282 | 3.6 | 223 | 3.2 | 128 | 2.8 | 122 | 2.7 | 0.87 | 0.74-1.02 | 0.77 | 0.63-0.93 | 0.75 | 0.62-0.91 |
| Acute monoblastic and monocytic leukemia; (FAB M5) [M-9891] | 1 106 | 3.2 | 167 | 2.3 | 84 | 1.6 | 99 | 2.2 | 0.72 | 0.60-0.87 | 0.52 | 0.41-0.65 | 0.69 | 0.55-0.85 |
| Acute erythroid leukemia; (FAB M6) [M-9840] | 266 | 0.7 | 28 | 0.4 | 17 | 0.4 | 29 | 0.7 | 0.53 | 0.33-0.80 | 0.48 | 0.27-0.79 | 0.92 | 0.60-1.36 |
| Acute megakaryoblastic leukemia; (FAB M7) [M-9910] | 117 | 0.4 | 40 | 0.4 | 25 | 0.4 | 22 | 0.5 | 1.00 | 0.64-1.54 | 1.18 | 0.72-1.86 | 1.28 | 0.77-2.04 |
| Acute basophilic leukemia; [M-9870] | 4 | ∼ | 0 | ∼ | 0 | ∼ | 1 | ∼ | ∼ | ∼ | ∼ | |||
| Acute panmyelosis with myelofibrosis; [M-9931] | 104 | 0.3 | 8 | ∼ | 11 | 0.3 | 10 | 0.2 | ∼ | 0.86 | 0.41-1.62 | 0.71 | 0.33-1.38 | |
| Myeloid sarcoma; [M-9930] | 120 | 0.3 | 24 | 0.3 | 17 | 0.4 | 10 | 0.2 | 0.83 | 0.49-1.35 | 1.07 | 0.59-1.80 | 0.61 | 0.28-1.16 |
| Group 2 | 1 319 | 4.0 | 410 | 4.5 | 178 | 3.2 | 165 | 3.4 | 1.13 | 1.00-1.27 | 0.81 | 0.69-0.95 | 0.85 | 0.72-1.00 |
| AML with t(8;21); (FAB M2, t(8;21)) [M-9896] | 215 | 0.6 | 38 | 0.4 | 24 | 0.4 | 34 | 0.7 | 0.67 | 0.44-0.98 | 0.70 | 0.44-1.08 | 1.12 | 0.76-1.62 |
| AML with inv(16) or t(16;16); (FAB M4Eo) [M-9871] | 136 | 0.4 | 41 | 0.5 | 8 | ∼ | 15 | 0.3 | 1.11 | 0.74-1.63 | ∼ | 0.71 | 0.38-1.22 | |
| APL with t(15;17); (FAB M3) [M-9866] | 871 | 2.6 | 316 | 3.3 | 140 | 2.5 | 101 | 2.0 | 1.28 | 1.11-1.46 | 0.95 | 0.79-1.14 | 0.77 | 0.61-0.94 |
| AML, 11q23 abnormalities; [M-9897] | 97 | 0.3 | 15 | 0.2 | 6 | ∼ | 15 | 0.4 | 0.84 | 0.42-1.51 | ∼ | 1.24 | 0.66-2.15 | |
| Group 3 | 1 278 | 3.5 | 123 | 2.1 | 104 | 2.4 | 124 | 2.9 | 0.60 | 0.49-0.73 | 0.67 | 0.54-0.82 | 0.81 | 0.67-0.98 |
| AML with myelodysplasia-related changes; [M-9895] | 941 | 2.6 | 84 | 1.5 | 62 | 1.5 | 96 | 2.3 | 0.58 | 0.45-0.73 | 0.59 | 0.44-0.76 | 0.87 | 0.70-1.08 |
| Therapy-related myeloid neoplasms; [M-9920, 9987] | 337 | 1.0 | 39 | 0.6 | 42 | 0.8 | 28 | 0.6 | 0.67 | 0.45-0.95 | 0.89 | 0.62-1.24 | 0.65 | 0.42-0.96 |
| ALL/L* | 4 761 | 16.6 | 2 907 | 24.9 | 644 | 10.2 | 715 | 14.8 | 1.50 | 1.43-1.58 | 0.61 | 0.56-0.67 | 0.89 | 0.82-0.96 |
| Subtype | ||||||||||||||
| B-cell lymphoblastic leukemia/lymphoma; [M-9727(B), 9728, 9835(B), 9836] | 3 133 | 11.0 | 2 094 | 18.1 | 368 | 5.8 | 510 | 10.6 | 1.64 | 1.55-1.74 | 0.52 | 0.47-0.59 | 0.96 | 0.87-1.06 |
| T-cell lymphoblastic leukemia/lymphoma; [M-9727(T), 9729, 9835(T), 9837] | 797 | 2.8 | 313 | 2.6 | 160 | 2.5 | 109 | 2.2 | 0.94 | 0.82-1.08 | 0.90 | 0.75-1.07 | 0.79 | 0.64-0.97 |
| Lymphoblastic leukemia/lymphoma, unknown lineage; [M-9727(U), 9835(U)] | 831 | 2.8 | 500 | 4.2 | 116 | 1.9 | 96 | 2.0 | 1.49 | 1.32-1.69 | 0.68 | 0.55-0.84 | 0.71 | 0.57-0.88 |
| AL ambiguous lineage* | 698 | 1.9 | 126 | 1.9 | 104 | 2.3 | 59 | 1.4 | 0.97 | 0.78-1.20 | 1.20 | 0.96-1.48 | 0.73 | 0.55-0.95 |
| Subtype | ||||||||||||||
| Acute undifferentiated leukemia; [M-9801] | 591 | 1.6 | 91 | 1.5 | 88 | 2.0 | 45 | 1.1 | 0.90 | 0.70-1.15 | 1.24 | 0.97-1.56 | 0.68 | 0.49-0.92 |
| Acute biphenotypic leukemia; [M-9805] | 107 | 0.3 | 35 | 0.4 | 16 | 0.3 | 14 | 0.3 | 1.30 | 0.82-2.00 | 0.99 | 0.53-1.71 | 0.97 | 0.51-1.70 |
All incidence rates are age-adjusted to the 2000 US standard population and expressed per 1 000 000 person-years. IRRs are based on unrounded rates.
NHWs indicates non-Hispanic whites; HWs, Hispanic whites; APIs, Asians/Pacific Islanders; FAB, French–American–British classification; (B), B-cell immunophenotype; (T), T-cell immunophenotype; (U), immunophenotype not specified; and ∼, IRs not calculated for fewer than 10 cases.
Includes all ICD-O-3 morphology codes specified within the respective subtype categories. ICD-O-3 codes are specified within brackets.
AL subtypes and age.
Age-specific incidence of subtypes of AML, ALL/L, and AL of ambiguous lineage are depicted in Figure 2 for all races and sexes combined. A bimodal IR pattern with an initial peak in infancy (< 1 year) was apparent for AML, NOS; acute myelomonocytic leukemia; acute monoblastic and monocytic leukemia; and acute megakaryoblastic leukemia. A slightly older initial age peak (1-4 years) occurred for B-cell ALL/L, ALL/L of unknown lineage, acute undifferentiated leukemia, and acute biphenotypic leukemia; an older (5-14 years), less prominent age peak was noted for T-cell ALL/L. In contrast, several AML subtypes occurred rarely in infancy and childhood, including AML with 11q23 abnormalities, AML with myelodysplasia-related changes, therapy-related myeloid neoplasms, acute erythroid leukemia, acute panmyelosis with myelofibrosis, and myeloid sarcoma. In adulthood, most AML subtypes increased sharply with advancing age, although a more attenuated rise in incidence with age was suggested for AML with inv(16) or t(16;16) and APL with t(15;17). Although only a subtle rise in incidence at older ages was suggested for B- and T-cell ALL/L, the incidence of ALL/L of unknown lineage rose prominently beginning in mid-life.
Figure 2.
Age-specific IRs of AML, ALL/L, and AL. Age-specific IRs of AML, ALL/L, and AL of ambiguous lineage according to subtype, SEER-17, 2001 to 2007.
Unspecified AL subtypes by calendar year.
Incidence of AML, NOS declined significantly from 2001 (IR = 19.3; 45.9% of AML cases) to 2002 (IR = 16.4, 42% of AML cases) but then remained relatively stable through 2007 (IR range, 15.8-16.7). In contrast, incidence of ALL/L of unknown lineage decreased progressively from 2001 (IR = 4.6) to 2007 (IR = 2.0), accounting for 27.6% and 10.8% of ALL/L cases, respectively. A continuous rise in incidence of B-cell ALL/L was observed from 2001 (IR = 9.6) to 2007 (IR = 13.4), with B-cell ALL/L accounting for 57.6% of ALL/L in 2001 and 74.8% in 2007. No temporal pattern was apparent for T-cell ALL/L.
Relative survival
AML: subtypes and age.
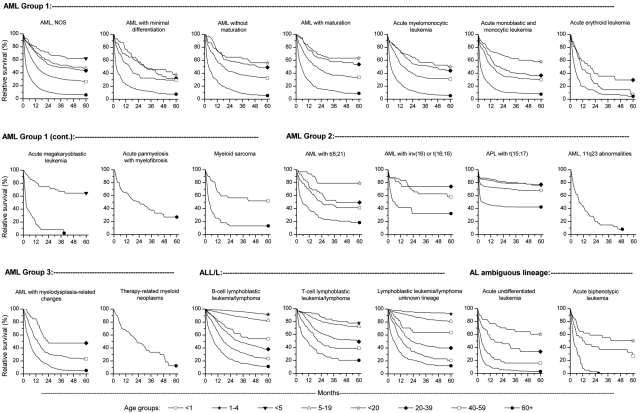
Infants (< 1 year) with AML had less favorable 1- and 5-year RS than older children and adolescents (1-4 and 5-19 years). This exception aside, beginning at 1 to 4 years, RS decreased progressively with increasing age at AML diagnosis (supplemental Table, available on the Blood Web site; see the Supplemental Materials link at the top of the online article). Based on broader age groups, a similar pattern of progressive decrease in patient survival with increasing age at diagnosis was observed for most AML subtypes (Figure 3; supplemental Table). Compared with all other subtypes of AML, for each age group studied, 5-year RS was most favorable for APL with t(15;17) and AML with inv(16). Survival also was favorable for AML with t(8;21) among individuals less than 20 years of age but intermediate among older age groups. Most AML group 1 subtypes had intermediate 5-year survival for age groups less than 60 years; prognosis was uniformly poor (RS < 10%) for patients diagnosed at ages 60 years or older, with the exception of acute panmyelosis with myelofibrosis and myeloid sarcoma. Among each affected age group, patients with acute erythroid leukemia tended to have the least favorable survival. In contrast to most other AML subtypes, survival for APL with t(15;17) decreased precipitously within the first 2 months of diagnosis, most prominently among the oldest age group, but thereafter remained generally stable over the ensuing 5-year period.
Figure 3.
RS of AML, ALL/L, and AL. RS of AML, ALL/L, and AL of ambiguous lineage according to subtype and age among individuals diagnosed in SEER-17 during 2001 to 2006 and followed through 2007.
ALL/L: subtypes and age
Similar to the pattern observed for AML, infants (< 1 year) with ALL/L had worse survival than older children and adolescents (1-4 and 5-19 years). Among ALL/L subtypes, children 1 to 4 years of age had the highest survival for all subtypes; thereafter, survival decreased with increasing age at diagnosis, with a relatively notable decline in survival beginning at ages 20 to 39 years for all ALL/L entities. Infants with B-cell ALL/L and ALL/L of unknown lineage had intermediate survival compared with the 5- to 19-year and 20- to 39-year age groups. Notably, children and young adults 1 to 4 and 5 to 19 years of age with B-cell ALL/L had more favorable survival than those with T-cell ALL/L. In contrast, survival for T-cell ALL/L was substantially higher than B-cell ALL among adults 20 to 39, 40 to 59, and 60 years or older of age. Survival for patients with ALL/L of unknown lineage was generally similar to that of B-cell ALL/L.
AL of ambiguous lineage: subtypes and age.
Similar to AML and ALL/L subtypes, survival of patients with AL of ambiguous lineage decreased markedly with advancing age. Most notably, individuals 60 years of age or older with acute undifferentiated leukemia, the most commonly affected age group, was particularly poor, with a 5-year survival rate of 3%.
Discussion
In the first comprehensive, population-based analysis of incidence patterns of AL subtypes and patient survival in the United States guided by the 2001 WHO classification scheme, we observed substantial differences in incidence among AL subtypes by age, sex, and race/ethnicity. Infants and children demonstrated increased susceptibility to ALL/L and some, but not all, AML subtypes, with variation in the age at occurrence of the initial incidence peak. Age patterns in adults also varied among AL subtypes with respect to the rate of rise in incidence with advancing age. Most, but not all, AL subtypes predominated among males and non-Hispanic whites. Despite the 43.9% of AML, NOS and 17.2% of ALL/L of unknown lineage, these frequencies have decreased compared with prior SEER-based studies.6 The decline in the IR for AML, NOS from 2001 to 2002 and then relative stability through 2007 suggests that a further decrease is unlikely with the current ICD-O-3 classification and will require additional disease entities, such as those proposed in the 2008 WHO classification for the next ICD-O revision (ICD-O-4). In contrast, the progressive decrease in incidence of ALL/L of unspecified lineage during 2001 to 2007 is consistent with increased use of immunophenotyping, reporting of immunophenotype to cancer registries, or both. We found that AL survival was highly dependent on age at diagnosis and notably less favorable across all subtypes among individuals diagnosed at 60 years of age or older. Among AML subtypes, survival was highest for group 2 entities, particularly for APL with t(15;17) and AML with inv(16) for most age groups. B-cell ALL/L had more favorable survival than T-cell ALL/L among the young, whereas the converse occurred at older ages. We conclude that AL subtypes defined by the WHO classification have distinct incidence and survival patterns pointing to biologic diversity and etiologic heterogeneity.
The striking differences in incidence patterns among AL subtypes by age are strongly supportive of etiologic heterogeneity. Certain subtypes demonstrated a bimodal incidence pattern by age, with variation of the initial peak from infancy (< 1 year) to early or later childhood (1-4 or 5-14 years, respectively). In contrast, some AML subtypes occurred rarely in infancy and childhood and increased exponentially with advancing age. Acute megakaryoblastic leukemia, acute panmyelosis with myelofibrosis, and AML with 11q23 abnormalities were largely limited to the adult population, although the early-onset age peak of acute megakaryoblastic leukemia we observed at ages less than 1 and 1 to 4 years is consistent with the median age of 23 months (range, 6.7-208.9 months) reported at a pediatric institution.10 Similar to our findings, other series have reported a median age of 42.5 years for adult acute megakaryoblastic leukemia11 and 67 years for acute panmyelosis with myelofibrosis.12
The age-dependent incidence patterns we observed are consistent with the age-specific patterns of recurrent chromosomal and genetic abnormalities that are a hallmark of AL.13–16 For example, the Philadelphia chromosome t(9;22) is the most common rearrangement in adult ALL/L, whereas high hyperdiploidy (51-65 chromosomes) and the t(12;21) translocation are the most common cytogenetic abnormalities in childhood ALL/L. In both infant ALL/L and AML, the t(4;11) translocation involving the MLL gene is the most common abnormality. However, 11q23 abnormalities involving MLL and various translocation partners are found across all ages. The multiple breakpoint positions within MLL have an age-dependent distribution, potentially accounting for the distinct biologic behavior of AL in infants compared with children and adults, despite phenotypically and cytogenetically similar disease.17 11q23 abnormalities have been described in AML evolving from MDS, therapy-related AML, and in several subtypes included in the French–American–British classification.3,18 The prominent adult-onset age pattern we observed in AML with 11q23 abnormalities, as was similarly seen with therapy-related myeloid neoplasms, may reflect the higher incidence of therapy-related neoplasms and MDS among adults than children. Together, these observations suggest that for selected AL subtypes, information on age may merit inclusion in future WHO classification revisions, as has been suggested for lymphoid neoplasms where age has been closely associated with disease biology or etiology (eg, pediatric marginal zone lymphoma, Epstein-Barr virus–positive diffuse large B-cell lymphoma of the elderly).4
The age-dependent incidence patterns further support the findings of Moorman and colleagues19 who assessed age-specific patterns of AL according to cytogenetic classification and suggested that these patterns might provide insight into the number of required molecular abnormalities for leukemogenesis. Based on the observation of constant incidence of APL (n = 149) across all ages, Vickers et al20 hypothesized that a single, rate-limiting genetic event might be sufficient to initiate the disease, assuming a constant mutation rate with advancing age. Other population-based studies,21,22 and the findings we report, also suggest a slowly progressive rise in incidence of APL with advancing age, which in our study was less prominent than for most group 1 and group 3 AML subtypes. Together, these reports underscore the need to consider the cytogenetic classification of AL subtypes in future etiologic research.
The male predominance of ALs5–7,23 showed substantial variation among AML subtypes, ranging from similar IRs for males and females for therapy-related myeloid neoplasms (IRR = 0.99) and APL (IRR = 1.08) to more than 2.0-fold higher incidence among males than females for AML with myelodysplasia-related changes, acute erythroid leukemia, and T-cell ALL/L. Similar to findings in a recent study from Sweden based on 105 cases,22 APL predominated among women at younger ages and among males at older ages, although sex differences in our study were nonsignificant across most age groups. It is notable that the male predominance in the incidence of AML with myelodysplasia-related changes parallels the estimated 70% higher incidence of MDS occurring among males than females.24 Acute erythroid leukemia may arise de novo but may similarly evolve from preceding MDS, thereby possibly accounting for the male predominance we observed, as also reported in clinical series.25 We noted the most prominent sex disparity for T-cell ALL/L, with incidence among males more than twice that among females. Notably, an inactivating mutation and deletions in that X-linked tumor suppressor gene PHF6 have been identified in T-cell ALL,26 possibly contributing to the male predominance for this subtype. Future studies of genetic and hormonal characteristics, environmental exposures (eg, pesticides, fertilizers, benzene, formaldehyde, and tobacco products) and exposure levels are likely to provide insight into the sex differences observed by AL subtype.
Distinct racial/ethnic patterns by disease subtype support differences in host susceptibility among the ALs. Although non-Hispanic whites had the highest rates of most subtypes, we also observed significantly elevated rates among Hispanic whites for APL with t(15;17), B-cell ALL/L, and ALL/L of unknown lineage, consistent with most previous reports.6,27–29 An earlier study in the SEER Program found the incidence rates of APL among Hispanics exceeded that among whites among those under age 45 years but not among older ages.30 Investigations of 3 breakpoint sites (bcr1, bcr2, and bcr3) of the PML gene involved in APL with t(15;17), have described significantly higher prevalence of bcr1 among individuals from Latin America compared with published reports of non-Latino populations in the United States and Europe.31,32 In addition, several recent genome-wide association studies of childhood ALL/L have identified risk loci with varying effects by racial/ethnic group for B- and T-cell ALL/L,33,34 further highlighting the importance of considering disease subtypes according to race/ethnicity and age in etiologic investigations.
Survival information and identification of prognostic features that influenced the WHO classification system of AML have been derived largely from clinical series. Our investigation, the first population-based study to comprehensively describe patient survival by AL subtype, revealed advancing age to be an important determinant for survival among nearly all AL subtypes. This overall age pattern is similar to the results for all AML subtypes combined, reported in other population-based studies.8,35–37 The 5-year RS of AML we report in SEER-17 (2001-2006) was generally comparable to the 5-year RS reported in Sweden (1997-2005),8 and notably improved among infants (< 1 year) compared with that previously reported in 9 SEER areas during 1995 to 1999 (RS = 39.0; 95% CI, 18.7%-59.3%).36 Individuals diagnosed with AML between 41 and 60 years of age in Sweden, had a 1-year RS of 61%8 that compares with 1-year RS of 63% and 53% of AML in the SEER Program among individuals 40 to 49 and 50 to 59 years of age, respectively.
We found substantial variation in survival among patients with different AML subtypes. Individuals with group 2 AML subtypes (5-year RS = 60.8%) had more favorable survival compared with group 1 or group 3 AML subtypes (5-year RS = 21.1% and 13.3%, respectively), consistent with the prognostic significance of cytogenetics reported in clinical trials, where (15;17), t(8;21), and inv(16) emerge as favorable features among individuals of all ages.38,39 Notable variation in survival was seen for APL with t(15;17) according to age at diagnosis in our study, with 76% to 77% RS for ages less than 40 years, 68% for ages 40 to 59 years, and 43% for ages more than 60 years. We confirmed recent population-based reports, including a SEER-based study, of a high early death rate after a diagnosis of APL, particularly among older patients.21,22 Possible reasons to account for the early death rate in APL, including disease sequelae (eg, hemorrhage and hyperleukocytosis), treatment complications, lack of timely initiation of treatment, and other factors, have been reviewed recently.21 Improving on the substantial heterogeneity that exists in the definition of treatment-related mortality across studies,40 should help elucidate reasons for early death rates in APL reported internationally. In addition, of particular interest was the apparent worse relative survival in all except the youngest (< 20 years) age groups for AML t(8;21) compared with APL with t(15;17) and AML with inv(16). Clinical series have reported similar overall (observed) 5-year survival among younger individuals (median age, 35 years; n = 377) with AML with t(15;17), t(8;21), and inv(16) (63%, 69%, and 61%, respectively), although survival differences by AML subtype have been reported among older patients (38%, 35%, and 17%, respectively; n = 78).38,39 Theoretically, a varying prevalence of KIT mutations in the general adult population with AML with t(8;21) compared with individuals participating in clinical trials could account, at least in part, for these findings. Notably, the adverse impact of KIT mutations on survival in AML with t(8;21) or inv(16) seems to be limited to adults.41,42
The overall survival patterns for group 1 AML subtypes were less diverse than the incidence patterns, perhaps related to the widespread use of cytarabine- and anthracycline-based therapy for all of these subtypes.43 The 2008 WHO classification includes provisional entities that incorporate information on new cytogenetic abnormalities that may facilitate development of targeted therapies and predict survival. Although information on presumed prognostic markers (eg, NPM1 and CEBPA) is not considered within distinct entities in the current WHO classification, as additional clinical data accumulate, newly defined AML subtypes that incorporate this information may be included in future revisions of the classification.
Our population-based data support previous clinical series showing that infants and older adults have a less favorable prognosis than children and young adults with ALL/L.44 Overall 5-year survival rates of ∼ 40% have been reported among adults with ALL/L, with individuals more than 60 years of age having 5-year overall survival rates of less than 10%.45 New in our study was the ability to compare RS patterns for B- versus T-cell ALL/L. Among patients in the general population diagnosed with ALL/L at ages 1 to 19 years, we demonstrated significantly higher survival for those with B-ALL/L compared with T-cell ALL/L. These findings contrast with previous results from clinical trials showing that cellular phenotype is of less prognostic importance in childhood ALL/L.44 However, for each age group 20 years or older, we found that T-cell ALL/L was associated with a more favorable survival than B-ALL/L, in agreement with clinical series that found significantly better 5-year overall survival for T-cell (48%) than B-cell survival phenotype (41%) among individuals 15 to 59 years of age.45 The age-specific survival differences in B-cell ALL/L we observed may, in part, be because of the increasing prevalence of t(9;22) with advancing age, a well-described, poor prognostic feature.46,47 Notably, tyrosine kinase inhibitors have favorably affected survival of Philadelphia chromosome-positive ALL across all ages.46,47 The 2008 WHO classification proposed a new category for B-cell ALL/L with t(9;22)(q34;q11.2) that will allow greater insight into future studies of etiology and survival of this disease entity.
Strengths of our study include the large numbers of cases available in a population-based setting, thus avoiding biases related to referral patterns or population differences in clinical series. Furthermore, the large number of cases categorized using ICD-O-3 codes allowed us to evaluate incidence and patient survival guided by the WHO classification. With improved classification over time, we report more than 80% of ALL/L cases with known B- versus T-cell lineage, far higher than previous large studies.5–7
Limitations of our analysis include the absence of a centralized expert hematopathology review. Although the proportion of AML, NOS was higher in an earlier report describing SEER data,6 a sizeable number of AML cases in our study were classified as AML, NOS (44% of our AML group), particularly at older ages. It is plausible that elderly individuals, untreated patients, and those diagnosed outside major academic centers may have undergone less intensive diagnostic testing, and thus the AML, NOS category probably includes cases that should be classified to more specific WHO AML subtypes in groups 1, 2, and 3. In addition, the AML, NOS group probably also contains cases with cytogenetic abnormalities that do not have a corresponding ICD-O-3 histology code. Although we are unable to differentiate AML cases that did not undergo complete diagnostic evaluation from those with abnormal karyotype but for which no ICD-O-3 code exists and those associated with normal karyotype, the frequency of AML with normal karyotype is reported to comprise 41% to 48% of cases of AML in other series.38,48,49
The occurrence of group 3 AML (AML with myelodysplasia-related changes and therapy-related myeloid neoplasms) is probably under-ascertained in these population-based data because the ICD-O codes for these entities were newly introduced in 2000, and history of previous cytotoxic therapy may not be reliably reported. As noted previously, our study does not include cases of AL occurring among individuals with MDS, myeloproliferative neoplasms, or other leukemias. A study of adults with non-APL AML in Sweden (1997-2005) reported 24% of cases were secondary to prior hematologic disease.35 Although we included in our incidence analysis patients with AL after nonhematologic malignancies (some of whom were treated with cytotoxic therapy for a first primary malignancy), these patients accounted for a small proportion (2%-5%) of the total number of cases and thus were unlikely to substantially bias the reported incidence data. Our survival analyses did not account for treatment which may, at least in part, account for the age-specific survival differences observed. Treatment with chemotherapy has been shown to be associated with improved survival and that use of chemotherapy is less frequent among older than younger patients.50
In summary, in the first comprehensive, population-based assessment of AL incidence and patient survival according to the 2001 WHO classification, the heterogeneous incidence patterns by sex, racial/ethnic group, and most strikingly by age suggest that the WHO classification can discriminate between etiologically distinct AL subtypes, biologically distinct AL subtypes, or both. Our survival data by AL subtypes serves as a contemporary clinical resource for patients with AL in the general population. The notable influence of older age on survival across all leukemia subtypes highlights the need to develop nontoxic therapies and to include these higher risk individuals in clinical trials. The distinct AL incidence and survival patterns by subtype suggest that the WHO classification will facilitate future etiologic discovery, prognostication, and treatment advances.
Supplementary Material
Acknowledgments
The authors thank William F. Kern, MD (Department of Pathology, University of Oklahoma Health Sciences Center, Oklahoma City, OK), for valuable input on earlier versions of the manuscript; and David Check (Division of Cancer Epidemiology and Genetics, National Cancer Institute), for expert assistance with the figures.
This work was supported by the Department of Veterans Affairs Medical Center in Oklahoma City; and the Intramural Research Program, Department of Health and Human Services, National Cancer Institute, National Institutes of Health.
Footnotes
The online version of the article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: G.M.D., S.S.D., R.E.C., M.S.L., and L.M.M. conceived and designed research; G.M.D. performed statistical analysis; G.M.D., S.S.D., R.E.C., M.S.L., and L.M.M. analyzed and interpreted data; G.M.D. and L.M.M. wrote the manuscript; and G.M.D., S.S.D., R.E.C., M.S.L., and L.M.M. critically reviewed and edited the manuscript for important intellectual content.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Graça M. Dores, Department of Veterans Affairs Medical Center, 921 NE 13th St, Oklahoma City, OK 73104; e-mail: doresg@mail.nih.gov.
References
- 1.Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60(5):277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 2.Linet MS, Devesa SS, Morgan GJ. The leukemias. In: Schottenfeld D, Fraumeni JF Jr, editors. Cancer Epidemiology and Prevention. 3rd ed. New York, NY: Oxford University Press; 2006. pp. 841–871. [Google Scholar]
- 3.Jaffe ES, Harris NL, Stein H, Vardiman JW. World Health Organization Classification of Tumours. Pathology and Genetics of Haematopoietic and Lymphoid Tissues. Lyon, France: IARC Press; 2001. [Google Scholar]
- 4.Swerdlow SH, Campo E, Harris NL, et al. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues (4th ed) Lyon, France: International Agency for Research on Cancer; 2008. [Google Scholar]
- 5.Sant M, Allemani C, Tereanu C, et al. Incidence of hematologic malignancies in Europe by morphologic subtype: results of the HAEMACARE project. Blood. 2010;116(19):3724–3734. doi: 10.1182/blood-2010-05-282632. [DOI] [PubMed] [Google Scholar]
- 6.Yamamoto JF, Goodman MT. Patterns of leukemia incidence in the United States by subtype and demographic characteristics, 1997-2002. Cancer Causes Control. 2008;19(4):379–390. doi: 10.1007/s10552-007-9097-2. [DOI] [PubMed] [Google Scholar]
- 7.Morton LM, Wang SS, Devesa SS, Hartge P, Weisenburger DD, Linet MS. Lymphoma incidence patterns by WHO subtype in the United States, 1992-2001. Blood. 2006;107(1):265–276. doi: 10.1182/blood-2005-06-2508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Derolf AR, Kristinsson SY, Andersson TM, Landgren O, Dickman PW, Bjorkholm M. Improved patient survival for acute myeloid leukemia: a population-based study of 9729 patients diagnosed in Sweden between 1973 and 2005. Blood. 2009;113(16):3666–3672. doi: 10.1182/blood-2008-09-179341. [DOI] [PubMed] [Google Scholar]
- 9. Surveillance, Epidemiology and End Results (SEER) Program ( www.seer.cancer.gov) SEER*Stat Database: Incidence - SEER-9 Regs Research Data, Nov 2009 Sub (1973-2007) <Katrina/Rita Population Adjustment>, National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch, released April 2010, based on the November 2009 submission.
- 10.Athale UH, Razzouk BI, Raimondi SC, et al. Biology and outcome of childhood acute megakaryoblastic leukemia: a single institution's experience. Blood. 2001;97(12):3727–3732. doi: 10.1182/blood.v97.12.3727. [DOI] [PubMed] [Google Scholar]
- 11.Tallman MS, Neuberg D, Bennett JM, et al. Acute megakaryocytic leukemia: the Eastern Cooperative Oncology Group experience. Blood. 2000;96(7):2405–2411. [PubMed] [Google Scholar]
- 12.Thiele J, Kvasnicka HM, Zerhusen G, et al. Acute panmyelosis with myelofibrosis: a clinicopathological study on 46 patients including histochemistry of bone marrow biopsies and follow-up. Ann Hematol. 2004;83(8):513–521. doi: 10.1007/s00277-004-0881-8. [DOI] [PubMed] [Google Scholar]
- 13.Manola KN. Cytogenetics of pediatric acute myeloid leukemia. Eur J Haematol. 2009;83(5):391–405. doi: 10.1111/j.1600-0609.2009.01308.x. [DOI] [PubMed] [Google Scholar]
- 14.Moorman AV, Chilton L, Wilkinson J, Ensor HM, Bown N, Proctor SJ. A population-based cytogenetic study of adults with acute lymphoblastic leukemia. Blood. 2010;115(2):206–214. doi: 10.1182/blood-2009-07-232124. [DOI] [PubMed] [Google Scholar]
- 15.Mrózek K, Heinonen K, Bloomfield CD. Clinical importance of cytogenetics in acute myeloid leukaemia. Best Pract Res Clin Haematol. 2001;14(1):19–47. doi: 10.1053/beha.2000.0114. [DOI] [PubMed] [Google Scholar]
- 16.Vrooman LM, Silverman LB. Childhood acute lymphoblastic leukemia: update on prognostic factors. Curr Opin Pediatr. 2009;21(1):1–8. doi: 10.1097/MOP.0b013e32831f1f24. [DOI] [PubMed] [Google Scholar]
- 17.Jung R, Jacobs U, Krumbholz M, et al. Bimodal distribution of genomic MLL breakpoints in infant acute lymphoblastic leukemia treatment. Leukemia. 2010;24(4):903–907. doi: 10.1038/leu.2010.14. [DOI] [PubMed] [Google Scholar]
- 18.Coenen EA, Raimondi SC, Harbott J, et al. Prognostic significance of additional cytogenetic aberrations in 733 de novo pediatric 11q23/MLL-rearranged AML patients: results of an international study. Blood. 2011;117(26):7102–7111. doi: 10.1182/blood-2010-12-328302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moorman AV, Roman E, Willett EV, Dovey GJ, Cartwright RA, Morgan GJ. Karyotype and age in acute myeloid leukemia. Are they linked? Cancer Genet Cytogenet. 2001;126(2):155–161. doi: 10.1016/s0165-4608(00)00414-3. [DOI] [PubMed] [Google Scholar]
- 20.Vickers M, Jackson G, Taylor P. The incidence of acute promyelocytic leukemia appears constant over most of a human lifespan, implying only one rate limiting mutation. Leukemia. 2000;14(4):722–726. doi: 10.1038/sj.leu.2401722. [DOI] [PubMed] [Google Scholar]
- 21.Park JH, Qiao B, Panageas KS, et al. Early death rate in acute promyelocytic leukemia remains high despite all-trans retinoic acid. Blood. 2011;118(5):1248–1254. doi: 10.1182/blood-2011-04-346437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lehmann S, Ravn A, Carlsson L, et al. Continuing high early death rate in acute promyelocytic leukemia: a population-based report from the Swedish Adult Acute Leukemia Registry. Leukemia. 2011;25(7):1128–1134. doi: 10.1038/leu.2011.78. [DOI] [PubMed] [Google Scholar]
- 23.Thygesen LC, Nielsen OJ, Johansen C. Trends in adult leukemia incidence and survival in Denmark, 1943-2003. Cancer Causes Control. 2009;20(9):1671–1680. doi: 10.1007/s10552-009-9417-9. [DOI] [PubMed] [Google Scholar]
- 24.Rollison DE, Howlader N, Smith MT, et al. Epidemiology of myelodysplastic syndromes and chronic myeloproliferative disorders in the United States, 2001-2004, using data from the NAACCR and SEER programs. Blood. 2008;112(1):45–52. doi: 10.1182/blood-2008-01-134858. [DOI] [PubMed] [Google Scholar]
- 25.Hasserjian RP, Zuo Z, Garcia C, et al. Acute erythroid leukemia: a reassessment using criteria refined in the 2008 WHO classification. Blood. 2010;115(10):1985–1992. doi: 10.1182/blood-2009-09-243964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Van Vlierberghe P, Palomero T, Khiabanian H, et al. PHF6 mutations in T-cell acute lymphoblastic leukemia. Nat Genet. 2010;42(4):338–342. doi: 10.1038/ng.542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marcos-Gragera R, Cervantes-Amat M, Vicente ML, et al. Population-based incidence of childhood leukaemias and lymphomas in Spain (1993-2002). Eur J Cancer Prev. 2010;19(4):247–255. doi: 10.1097/CEJ.0b013e328339e2f3. [DOI] [PubMed] [Google Scholar]
- 28.Pullarkat ST, Danley K, Bernstein L, Brynes RK, Cozen W. High lifetime incidence of adult acute lymphoblastic leukemia among Hispanics in California. Cancer Epidemiol Biomarkers Prev. 2009;18(2):611–615. doi: 10.1158/1055-9965.EPI-07-2949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Matasar MJ, Ritchie EK, Consedine N, Magai C, Neugut AI. Incidence rates of the major leukemia subtypes among US Hispanics, blacks, and non-Hispanic whites. Leuk Lymphoma. 2006;47(11):2365–2370. doi: 10.1080/10428190600799888. [DOI] [PubMed] [Google Scholar]
- 30.Matasar MJ, Ritchie EK, Consedine N, Magai C, Neugut AI. Incidence rates of acute promyelocytic leukemia among Hispanics, blacks, Asians, and non-Hispanic whites in the United States. Eur J Cancer Prev. 2006;15(4):367–370. doi: 10.1097/00008469-200608000-00011. [DOI] [PubMed] [Google Scholar]
- 31.Douer D, Santillana S, Ramezani L, et al. Acute promyelocytic leukaemia in patients originating in Latin America is associated with an increased frequency of the bcr1 subtype of the PML/RARalpha fusion gene. Br J Haematol. 2003;122(4):563–570. doi: 10.1046/j.1365-2141.2003.04480.x. [DOI] [PubMed] [Google Scholar]
- 32.Ruiz-Argüelles GJ, Garces-Eisele J, Reyes-Nunez V, Gomez-Rangel JD, Ruiz-Delgado GJ. More on geographic hematology: the breakpoint cluster regions of the PML/RARalpha fusion gene in Mexican Mestizo patients with promyelocytic leukemia are different from those in Caucasians. Leuk Lymphoma. 2004;45(7):1365–1368. doi: 10.1080/10428190310001657344. [DOI] [PubMed] [Google Scholar]
- 33.Han S, Lee KM, Park SK, et al. Genome-wide association study of childhood acute lymphoblastic leukemia in Korea. Leuk Res. 2010;34(10):1271–1274. doi: 10.1016/j.leukres.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 34.Yang W, Trevino LR, Yang JJ, et al. ARID5B SNP rs10821936 is associated with risk of childhood acute lymphoblastic leukemia in blacks and contributes to racial differences in leukemia incidence. Leukemia. 2010;24(4):894–896. doi: 10.1038/leu.2009.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Juliusson G, Antunovic P, Derolf A, et al. Age and acute myeloid leukemia: real world data on decision to treat and outcomes from the Swedish Acute Leukemia Registry. Blood. 2009;113(18):4179–4187. doi: 10.1182/blood-2008-07-172007. [DOI] [PubMed] [Google Scholar]
- 36.Linabery AM, Ross JA. Childhood and adolescent cancer survival in the US by race and ethnicity for the diagnostic period 1975-1999. Cancer. 2008;113(9):2575–2596. doi: 10.1002/cncr.23866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pulte D, Gondos A, Brenner H. Improvements in survival of adults diagnosed with acute myeloblastic leukemia in the early 21st century. Haematologica. 2008;93(4):594–600. doi: 10.3324/haematol.12304. [DOI] [PubMed] [Google Scholar]
- 38.Grimwade D, Walker H, Harrison G, et al. The predictive value of hierarchical cytogenetic classification in older adults with acute myeloid leukemia (AML): analysis of 1065 patients entered into the United Kingdom Medical Research Council AML11 trial. Blood. 2001;98(5):1312–1320. doi: 10.1182/blood.v98.5.1312. [DOI] [PubMed] [Google Scholar]
- 39.Grimwade D, Walker H, Oliver F, et al. The importance of diagnostic cytogenetics on outcome in AML: analysis of 1,612 patients entered into the MRC AML 10 trial. The Medical Research Council Adult and Children's Leukaemia Working Parties. Blood. 1998;92(7):2322–2333. [PubMed] [Google Scholar]
- 40.Ethier MC, Blanco E, Lehrnbecher T, Sung L. Lack of clarity in the definition of treatment-related mortality: pediatric acute leukemia and adult acute promyelocytic leukemia as examples. Blood. 2011;118(19):5080–5083. doi: 10.1182/blood-2011-07-363333. [DOI] [PubMed] [Google Scholar]
- 41.Paschka P, Marcucci G, Ruppert AS, et al. Adverse prognostic significance of KIT mutations in adult acute myeloid leukemia with inv(16) and t(8;21): a cancer and leukemia group B study. J Clin Oncol. 2006;24(24):3904–3911. doi: 10.1200/JCO.2006.06.9500. [DOI] [PubMed] [Google Scholar]
- 42.Pollard JA, Alonzo TA, Gerbing RB, et al. Prevalence and prognostic significance of KIT mutations in pediatric patients with core binding factor AML enrolled on serial pediatric cooperative trials for de novo AML. Blood. 2010;115(12):2372–2379. doi: 10.1182/blood-2009-09-241075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fernandez HF. New trends in the standard of care for initial therapy of acute myeloid leukemia. Hematology Am Soc Hematol Educ Program. 2010;2010:56–61. doi: 10.1182/asheducation-2010.1.56. [DOI] [PubMed] [Google Scholar]
- 44.Pui CH, Robison LL, Look AT. Acute lymphoblastic leukaemia. Lancet. 2008;371(9617):1030–1043. doi: 10.1016/S0140-6736(08)60457-2. [DOI] [PubMed] [Google Scholar]
- 45.Rowe JM, Buck G, Burnett AK, et al. Induction therapy for adults with acute lymphoblastic leukemia: results of more than 1500 patients from the international ALL trial: MRC UKALL XII/ECOG E2993. Blood. 2005;106(12):3760–3767. doi: 10.1182/blood-2005-04-1623. [DOI] [PubMed] [Google Scholar]
- 46.Foa R, Vitale A, Vignetti M, et al. Dasatinib as first-line treatment for adult patients with Philadelphia chromosome-positive acute lymphoblastic leukemia [published online ahead of print September 19, 2011]. Blood. doi: 10.1182/blood-2011-05-351403. doi: 10.1182/blood-2011-05-351403. [DOI] [PubMed] [Google Scholar]
- 47.Ottmann O, Dombret H, Martinelli G, et al. Dasatinib induces rapid hematologic and cytogenetic responses in adult patients with Philadelphia chromosome positive acute lymphoblastic leukemia with resistance or intolerance to imatinib: interim results of a phase 2 study. Blood. 2007;110(7):2309–2315. doi: 10.1182/blood-2007-02-073528. [DOI] [PubMed] [Google Scholar]
- 48.Grimwade D, Hills RK, Moorman AV, et al. Refinement of cytogenetic classification in acute myeloid leukemia: determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials. Blood. 2010;116(3):354–365. doi: 10.1182/blood-2009-11-254441. [DOI] [PubMed] [Google Scholar]
- 49.Bacher U, Kern W, Schnittger S, Hiddemann W, Haferlach T, Schoch C. Population-based age-specific incidences of cytogenetic subgroups of acute myeloid leukemia. Haematologica. 2005;90(11):1502–1510. [PubMed] [Google Scholar]
- 50.Alibhai SM, Leach M, Minden MD, Brandwein J. Outcomes and quality of care in acute myeloid leukemia over 40 years. Cancer. 2009;115(13):2903–2911. doi: 10.1002/cncr.24373. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.