Abstract
18F-fluorodeoxyglucose (FDG) positron emission tomography and computed tomography (integrated FDG PET/CT) has been used to diagnose recurrence and differentiate postoperative changes from lymph node metastasis in colorectal cancer, although its accuracy is questionable. We report a prone thoracoscopic surgery for a rectal cancer patient in which false-positive mediastinal lymph nodes were found on FDG-PET/CT. A 60-year-old man underwent a laparoscopic high anterior resection and D3 lymph node dissection for rectal cancer. The histopathological diagnosis was moderately differentiated adenocarcinoma of the rectum, stage IIIB (pT3N1M0), necessitating oral fluoropyrimidine agent S-1. After the primary surgery, a solitary mediastinal lymph node measuring 30 mm in diameter was detected, and abnormal accumulation was confirmed by FDG-PET/CT (SUVmax, 11.7). Thoracoscopic resection was performed in the prone position, but histopathological results showed no metastasis. He was subsequently diagnosed with reactive lymphadenitis. The patient was discharged on postoperative day 4 in good condition and is alive without recurrence 12 months after surgery. PET/CT is useful for the detection of colorectal cancer recurrence; however, it does have a high false-positive rate for mediastinal lymph nodes. There is a limit to its diagnostic accuracy, and one must determine the indication for surgical treatment carefully. Surgery in the prone position is a useful and minimally invasive approach to the mediastinum and allows aggressive resection to be performed.
Key words: False-positive, FDG-PET/CT, Mediastinal lymph node, Thoracoscopic surgery, Prone position
Introduction
With the development of chemotherapy, control of metastatic colorectal cancer has increased in recent years. Aggressive resection of distant metastases, local recurrence, or peritoneal dissemination has been performed, and good results have been reported [1, 2]. Particularly, aggressive resection has been recommended for hematogenous metastasis; however, in pulmonary resection, the presence of mediastinal lymph node recurrence has been reported as a poor prognostic factor [3]. Recommendations for the resection of distant lymph node metastasis are lacking, but it is thought that solitary metastatic lesions should be resected.
The development of various diagnostic imaging such as PET/CT has contributed enormously to performing preoperative staging and detecting postoperative recurrence. Here, we present the case of a patient who had a solitary swollen mediastinal lymph node with high accumulation on PET/CT after primary resection of rectal cancer. The patient subsequently underwent thoracoscopic resection in the prone position. However, histopathological results showed no metastasis, and he was diagnosed with reactive lymphadenitis. We report 1 case study of false-positive diagnosis on PET/CT and compare our findings with previous literature.
Case Report
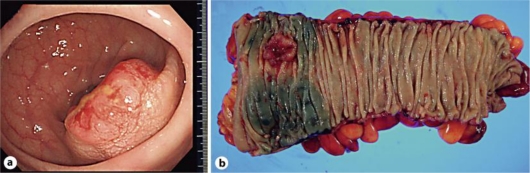
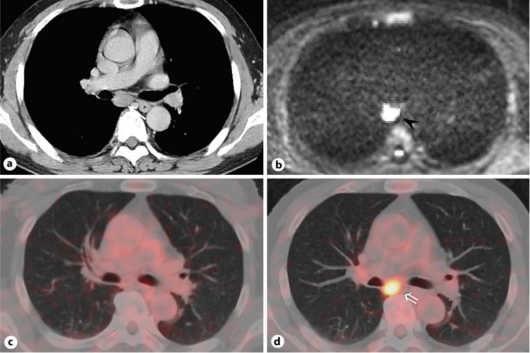
A 60-year-old patient presented with positive fecal occult blood and was subsequently diagnosed with rectal cancer (Rs). Laparoscopy-assisted high anterior resection with D3 lymph node dissection was performed. Histopathological examination revealed moderately differentiated adenocarcinoma, and the pathological stage was pT3N1M0, pStage IIIA (fig. 1a, b). The oral fluoropyrimidine agent S-1 (80 mg/m2 per day, administered for 4 weeks with a 2-week resting period) was administered for adjuvant chemotherapy. On postoperative day 239, a CT scan revealed a solitary swollen mediastinal lymph node (fig. 2a). The patient reported no symptoms of common cold, no palpable lymph nodes, and no murmur in the chest. Laboratory data, including blood count, biochemical findings, and C-reactive protein, were within normal range. The serum CEA level was also normal (1.8 ng/ml; normal value, <5.0 ng/ml); before primary surgical treatment, it was 5.8 ng/ml. T2-weighted MRI showed iso-high intensity, and diffusion-weighted MRI showed a high signal at the tracheal bifurcation (fig. 2b). PET/CT was performed, and abnormal 18F-FDG uptake appeared in the tracheal bifurcation. The standardized uptake value (SUVmax) was 11.7 (fig. 2c, d). Upper and lower gastrointestinal endoscopy revealed no abnormalities.
Fig. 1.
a Endoscopic findings for rectal cancer. b Resected specimen in primary surgery. A type-2 lesion measuring 23 mm in the rectosigmoid colon.
Fig. 2.
a CT showed a swollen mediastinal lymph node measuring 30 mm in diameter at the tracheal bifurcation (arrow). b Diffusion-weighted MRI showed a high signal in the tracheal bifurcation (arrowhead) due to restriction of diffusion. c Abnormal accumulation was not recognized on PET/CT before primary surgery. d PET/CT showed significant accumulation (SUVmax, 11.7) in the tracheal bifurcation (double arrow).
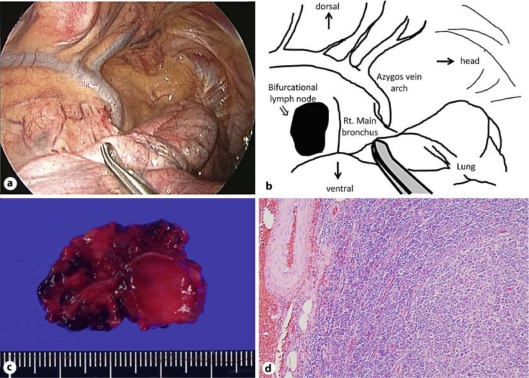
Thoracoscopic mediastinal lymph node resection was performed in the prone position on postoperative day 281. The surgical procedure was as follows: (1) a 12-mm port was inserted into the fifth intercostal space on the posterior axillary line with an 8-mm Hg pneumothorax; (2) a 12-mm camera port was inserted into the ninth intercostal space on the lower scapula line; (3) a 5-mm port was inserted into the seventh intercostal space on the posterior axillary line. The mediastinal lymph node was resected using thoracoscopy. Adhesions and invasion were not observed (fig. 3a, b). On histopathological examination, the resected specimen measuring 33 × 22 mm in diameter showed enlarged germinal centers without an epithelial component. Immunostaining was performed to detect follicular lymphoma; bcl-2 was negative, and the patient was diagnosed with reactive lymphadenitis (fig. 3c, d).
Fig. 3.
a Thoracoscopic view. b Illustration of intraoperative findings. A swollen bifurcational lymph node was observed (double arrow). c Macroscopic appearance of resected lymph node. d Histopathological findings of the specimen (HE staining, ×100) showed no metastatic lesion, but reactive lymphadenitis with expansion of germinal centers. Immunohistochemical staining for bcl-2 was negative.
The patient was discharged on postoperative day 4 without any postoperative complications. Oral capecitabine (Xeloda, 3,600 mg per day, administered for 2 weeks with a 1-week resting period) was administered for 6 months. Imaging follow-up was performed 2 months after thoracoscopic lymph node resection by CT scan. We confirmed that the suspicious lymph node was resected and other recurrent lesions did not appear. The patient is alive at more than 15 months after his second surgery and is being followed up closely.
Discussion
Since the publication of colorectal cancer treatment guidelines in Japan, providing appropriate treatment for these patients has become mandatory. Therefore, accurate preoperative diagnosis is important, and postoperative recurrence must be evaluated accurately by various methods of diagnostic imaging. Given the advent of FDG- PET and PET/CT in recent years, PET imaging has become essential for improving the detection rate. Studies have reported that PET imaging is more useful than MRI or multidetector-row CT (MDCT) [4, 5]. However, in colorectal cancer, the diagnostic capability for lymph node metastasis (reported as 29–51% sensitivity, 85–100% specificity, and 67–75% diagnostic accuracy) is insufficient compared to that for the primary tumor [6, 7, 9]. Especially for sensitivity, diffusion-weighted MRI is more useful than FDG-PET [6]. In our hospital, the diagnosis rate of lymph node metastases using preoperative PET/CT for 42 patients with colorectal cancer tended to be lower in specificity (77% sensitivity, 71% specificity, and 74% accuracy).
Generally, local inflammation, abscess formation, inflammatory diseases, and lymphomas may be considered as the causes of false-positive lymph nodes on PET. Although false-positive para-aortic lymph nodes are occasionally identified on PET [10], to our knowledge, PET false-positive cases associated with colorectal cancer in mediastinal lymph nodes have not been found. The use of PET/CT for identification of mediastinal lymph nodes has been reported. The specificity is lower for tuberculosis, sarcoidosis, and lymphoma [11]. The sensitivity is lower for non-small cell lung cancer [12]. Physiological accumulation is often observed in hilar lymph nodes and has the following features: (1) nearly equal accumulation intensity on both sides, and (2) no swollen lymph nodes in the mediastinum on CT. On the other hand, solitary mediastinal lymph node metastases of cases of colorectal cancer have also been reported [13]. The present case did not meet the features of physiological accumulation in hilar lymph nodes and showed a solitary enlarged lymph node, high SUVs, and high intensity on diffusion-weighted MRI. Therefore, we diagnosed the patient with mediastinal lymph node metastasis of colorectal cancer and performed surgical treatment.
On the other hand, less invasive surgery is desirable for surgical treatment, and advances in video-assisted surgery have been remarkable in recent years. Thoracoscopic esophagectomy has become widespread because it provides a magnified view and an easier approach to the mediastinum. Furthermore, thoracoscopic esophagectomy in the prone position has been introduced in some institutions [14]. The biggest advantage of the prone position is a good view of the surgical field without displacing the heart and right lung because of gravity and artificial pneumothorax. Our case maximized the benefits of the prone position, and the patient had a good postoperative course.
Even though histopathological findings showed lymphadenitis, the patient had no distinct physical findings and inflammatory response. The possibility of viral infection cannot be ruled out, although it was difficult to diagnose correctly before surgical treatment. In cancer treatment, it is necessary to decide the appropriate strategy on a case-by-case basis with due consideration of the limits of various methods of diagnostic imaging. Moreover, evaluations of pre- and postoperative colorectal cancer recurrence and metastasis using integrated FDG PET/contrast-enhanced CT have been reported [15]. Kitajima et al. [15] reported 170 postoperative cases, with 93.2% sensitivity, 95.8% specificity, and 94.7% accuracy. Therefore, further improvement of accuracy in diagnostic imaging can be expected.
Conclusions
There is no consistent strategy for appropriate treatment of solitary lymph node metastasis in colorectal cancer patients. Especially for PET-positive lesions, both sensitivity and specificity may be insufficient. Mediastinoscopy and needle biopsy with bronchoscopy are useful methods; however, the possibility of disseminated cancer cells remains. In conclusion, our case report suggests that it is necessary to understand the limits of the diagnostic accuracy of PET/CT in determining the indication for surgical treatment. Additionally, the thoracoscopic approach in the prone position is one of the easy-to-use approaches to the mediastinum.
Disclosure Statement
The authors declare that they have no competing interests.
References
- 1.Penna C, Nordlinger B. Colorectal metastasis (liver and lung) Surg Clin North Am. 2002;82:1075–1090. doi: 10.1016/s0039-6109(02)00051-8. [DOI] [PubMed] [Google Scholar]
- 2.Kobayashi K, Kawamura M, Ishihara T. Surgical treatment for both pulmonary and hepatic metastases from colorectal cancer. J Thorac Cardiovasc Surg. 1999;118:1090–1096. doi: 10.1016/S0022-5223(99)70106-6. [DOI] [PubMed] [Google Scholar]
- 3.Koga R, Yamamoto J, Saiura A, Yamaguchi T, Hata E, Sakamoto M. Surgical resection of pulmonary metastases from colorectal cancer: four favourable prognostic factors. Jpn J Clin Oncol. 2006;36:643–648. doi: 10.1093/jjco/hyl076. [DOI] [PubMed] [Google Scholar]
- 4.Schmidt GP, Baur-Melnyk A, Haug A, Utzschneider S, Becker CR, Tiling R, Reiser MF, Hermann KA. Whole-body MRI at 1.5 T and 3 T compared with FDG-PET-CT for the detection of tumour recurrence in patients with colorectal cancer. Eur Radiol. 2009;19:1366–1378. doi: 10.1007/s00330-008-1289-y. [DOI] [PubMed] [Google Scholar]
- 5.Metser U, You J, McSweeney S, Freeman M, Hendler A. Assessment of tumor recurrence in patients with colorectal cancer and elevated carcinoembryonic antigen level: FDG PET/CT versus contrast-enhanced 64-MDCT of the chest and abdomen. AJR Am J Roentgenol. 2010;194:766–771. doi: 10.2214/AJR.09.3205. [DOI] [PubMed] [Google Scholar]
- 6.Ono K, Ochiai R, Yoshida T, Kitagawa M, Omagari J, Kobayashi H, Yamashita Y. Comparison of diffusion-weighted MRI and 2-[fluorine-18]-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) for detecting primary colorectal cancer and regional lymph node metastases. J Magn Reson Imaging. 2009;29:336–340. doi: 10.1002/jmri.21638. [DOI] [PubMed] [Google Scholar]
- 7.Tsunoda Y, Ito M, Fujii H, Kuwano H, Saito N. Preoperative diagnosis of lymph node metastases of colorectal cancer by FDG-PET/CT. Jpn J Clin Oncol. 2008;38:347–353. doi: 10.1093/jjco/hyn032. [DOI] [PubMed] [Google Scholar]
- 8.Furukawa H, Ikuma H, Seki A, Yokoe K, Yuen S, Aramaki T, Yamagushi S. PET scanning is not superior to whole-body multi-detector helical computed tomography in the preoperative staging of colorectal cancer. Gut. 2006;55:1007–1011. doi: 10.1136/gut.2005.076273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kantorová I, Lipská L, Bêlohlávek O, Visokai V, Trubac M, Schneiderová M. Routine (18)F-FDG PET preoperative staging of colorectal cancer: comparison with conventional staging and its impact on treatment decision making. J Nucl Med. 2003;44:1784–1788. [PubMed] [Google Scholar]
- 10.Saisho S, Saito S, Yoshida T, Ishii M, Morita H, Yamaguchi S, Maeda A, Uesaka K, Furukawa H. Two cases of advanced/recurrent rectal cancer which showed false-positive for para-aortic lymph node in FDG-PET/CT. Jpn J Gastroenterol Surg. 2007;40:683–688. Japanese. [Google Scholar]
- 11.Kumar A, Dutta R, Kannan U, Kumar R, Khilnani GC, Gupta SD. Evaluation of mediastinal lymph nodes using F-FDG PET-CT scan and its histopathologic correlation. Ann Thorac Med. 2011;6:11–16. doi: 10.4103/1817-1737.74270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perigaud C, Bridji B, Roussel JC, Sagan C, Mugniot A, Duveau D, Baron O, Despins P. Prospective preoperative mediastinal lymph node staging by integrated positron emission tomography-computerised tomography in patients with non-small-cell lung cancer. Eur J Cardiothorac Surg. 2009;36:731–736. doi: 10.1016/j.ejcts.2009.05.044. [DOI] [PubMed] [Google Scholar]
- 13.Musallam KM, Taher AT, Tawil AN, Chakhachiro ZI, Habbal MZ, Shamseddine AI. Solitary mediastinal lymph node metastasis in rectosigmoid carcinoma: a case report. Cases J. 2008;1:69. doi: 10.1186/1757-1626-1-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Palanivelu C, Prakash A, Senthilkumar R, Senthilnathan P, Parthasarathi R, Rajan PS, Venkatachlam S. Minimally invasive esophagectomy: thoracoscopic mobilization of the esophagus and mediastinal lymphadenectomy in prone position - experience of 130 patients. J Am Coll Surg. 2006;203:7–16. doi: 10.1016/j.jamcollsurg.2006.03.016. [DOI] [PubMed] [Google Scholar]
- 15.Kitajima K, Murakami K, Yamasaki E, Domeki Y, Tsubaki M, Sunagawa M, Kaji Y, Suganuma N, Sugimura K. Performance of integrated FDG PET/contrast-enhanced CT in the diagnosis of recurrent colorectal cancer: comparison with integrated FDG PET/non-contrast-enhanced CT and enhanced CT. Eur J Nucl Med Mol Imaging. 2009;36:1388–1396. doi: 10.1007/s00259-009-1081-5. [DOI] [PubMed] [Google Scholar]