Abstract
Streptococcus pneumoniae is an important cause of bacterial keratitis, an infectious disease of the cornea. This study aimed to determine the importance of pneumolysin (PLY), a pneumococcal virulence factor, in keratitis using a clinical keratitis isolate (K1263) and its isogenic mutant deficient in PLY (K1263ΔPLY) and determine the effect of these strains on primary rabbit corneal epithelial (RCE) cells. Each strain was injected into the corneal stromas of rabbits, clinical examinations were performed, and the recovered bacterial loads were determined. Bacterial extracts were exposed to RCE cells, and morphology and viability were assessed. The mutant strain deficient in PLY, K1263ΔPLY, caused significantly lower ocular disease scores than the parent strain (K1263), although a higher bacterial load was recovered from corneas infected with the mutant strain. Histological examination showed increased inflammatory cells in the anterior chamber and increased edema in eyes infected with the parent strain. RCE cells exposed to the parent strain had significantly decreased cell viability and showed increased evidence of cellular damage. This study confirms that in a strain that can cause clinical keratitis, PLY is a significant cause of the damage associated with pneumococcal keratitis. It also shows for the first time that the results from an in vitro model using RCE cells correlates with in vivo results thereby establishing a less invasive way to study the mechanisms of pneumococcal keratitis.
Keywords: Pneumolysin, Keratitis, Streptococcus pneumoniae
Introduction
Bacterial keratitis is a devastating infection of the cornea that can lead to corneal scarring and vision loss [1–4]. Streptococcus pneumoniae keratitis frequently follows surgery or trauma to the eye and is more common in patients with coexisting ocular disease [4–7]. Approximately 30,000 cases of bacterial keratitis are reported each year in the United States alone [8]. The top causes of bacterial keratitis include [2,5,6,9–14]. Streptococcus pneumoniae, or pneumococcus, is an important worldwide pathogen capable of causing a variety of diseases including pneumonia, meningitis, otitis media and ocular infections [11,14–20]. Traditionally, pneumococcal infections affect primarily elderly individuals or young children due to their weakened immune systems [21]; however, pneumococcal eye disease can affect people of all ages. Pneumococci possess a variety of virulence factors including a polysaccharide capsule, pneumolysin (PLY), and neuraminidases (Nan) that enable this pathogen to cause disease.
Pneumolysin is a member of the family of bacterial cholesterol dependent cytolysins which also includes perfringolysin and listeriolysin [22]. It is highly conserved among clinical isolates and capable of causing many different toxic effects depending on its concentration and the cell type affected [23–27]. PLY, a 53 kDa thiol-activated cytolytic protein, has two functional domains, a pore forming (cytolytic) domain and a complement activating domain. At high concentrations, PLY binds cholesterol within the host cell and inserts into the lipid bilayer where it oligomerizes and forms a transmembrane pore that results in cell lysis [23]. At subcytolytic concentrations, PLY causes immunological damage by activating the classical complement pathway and the inflammatory response [24]. PLY activates this pathway extracellularly by binding antibody via the Fc region, though PLY can also activate complement in the absence of antibodies [24,28,29]. By activating complement, pneumococci are able to enhance the inflammatory response and thereby increase host tissue destruction via the host’s own immune response. Additionally, the domain of PLY that recognizes the Fc region is homologous to the region of C-reactive protein (CRP) that activates the classical complement cascade by directly binding C1q. It is possible that PLY may act as a CRP analogue and compete with CRP possibly reducing potential protective effects of CRP [30]. The importance of this homology in vivo remains unclear. PLY has also been shown to stimulate human monocytes to produce inflammatory cytokines, tumor necrosis factor alpha (TNF-α) and interleukin-1β (IL-1β) [25] as well as cause an increase in the surface expression of intercellular adhesion molecule 1 (ICAM-1) [26]. PLY can also induce apoptosis of dendritic cells [27].
The importance of PLY in ocular infections has been studied. Pneumococci lacking the ply gene showed attenuated virulence in a rabbit model of keratitis [31,32], however, this previous study used a non-ocular strain of S. pneumoniae that had been passaged annually in mice for 15 years to increase virulence [33]. Moreover, recent work has shown that pneumococcal pathogenicity in the cornea is different from other pneumococcal infections in the body in that the polysaccharide capsule of the bacterium is not necessary to cause disease [16,34]. Although PLY is known to be cytolytic to many types of cells [35–38], an effect of PLY on corneal cells has never before been reported. The study described herein aimed to determine the importance of PLY in vivo using a clinical keratitis isolate and a PLY-deficient isogenic mutant. Additionally, the in vivo importance of PLY was compared to an in vitro experimental system using primary rabbit corneal epithelial cells in an effort to correlate in vivo and in vitro findings. It is hypothesized that deletion of the gene encoding PLY in a clinical strain will cause Staphylococcus aureus, Pseudomonas aeruginosa and S. pneumoniae significant reduction in corneal virulence in vivo and cytotoxicity of corneal epithelial cells in vitro.
Methods
Bacterial strains
S. pneumoniae clinical keratitis strain K1263 was obtained from Regis Kowalski (Charles T. Campbell Eye Microbiology Laboratory, University of Pittsburgh Medical Center, Pittsburgh, PA), for use in this experiment. Bacteria were routinely grown on blood agar plates containing 5% sheep erythrocytes. Individual colonies were selected from the plate and grown in Todd Hewitt Broth (BD Biosciences, Sparks, MD) supplemented with 0.5% yeast extract (THY) at 37°C and 5% CO2 overnight. The overnight cultures were then diluted 1:100 in fresh THY and grown to an optical density corresponding to 108 colony forming units per mL (CFU/mL). Serial dilutions of each inoculum were cultured on 5% blood agar to verify the accuracy of the inoculum CFU.
For preparation of cell-free intracellular and extracellular components of S. pneumoniae, bacteria were grown for 18 hours to an optical density of 0.8 at 600 nm and 1 mL aliquots were collected by centrifugation at 5000 × g for 10 minutes at 25°C. The extracellular components were removed and retained, and the bacterial pellet was suspended in 1 mL of PBS. While on ice, the suspension was sonicated using a microtip and a Sonicator 3000 (QSonica, LLC., Newtown, CT). The sample was sonicated 5 times for 15 seconds with a 30–60 second rest periods between cycles. Intracellular and extracellular portions were passed through 0.22 μm filters to remove any remaining bacteria. Samples were prepared and used immediately in experiments to avoid possible degradation of virulence factor activity.
Creation of PLY-negative mutant
A PLY-negative isogenic mutant was created using homologous D39, in which the pneumolysin gene was replaced with a cassette containing resistance to trimethoprim (Tmp) [26]. The parent strain, K1263, was grown in competence medium (CM) to A600 of 0.6. The cultures were diluted 1:50 in fresh CM. After 200 ng of competence-stimulating peptides 1 and 2 [39] were added, the cultures were incubated at 37°C and 5% CO2 for twelve minutes. One microgram of donor DNA was added to the mixture. A double-crossover event occurred in which the ply gene was replaced with the Tmp-resistance cassette of the donor DNA. Transformants were selected on 5% sheep blood agar plates containing 50 μg/mL trimethoprim and incubated overnight at 37°C and 5% CO2. Colonies that grew were further screened using PCR and hemolysis assays. The PCR reaction used primers PlymutF (5′-CCCGGTACCGGAGAAGGATTATATTGTCAAGGTTA-3′) and PlymutR (5′-CCCTCTAGACTCCAGACATATCATAGTTCAAGTAAAT-3′). These primers were designed to amplify approximately 500 bp on either side of ply in the pneumococcal chromosome. A successful deletion mutant was named K1263ΔPLY.
Hemolysis assay
The pneumolysin activity of the pneumococcal strains used in this experiment was assessed by hemolysis assay. The bacterial strains were grown overnight in THY to A600 of 0.8. The bacteria were collected by centrifugation and incubated with 100 μL lysis buffer (0.1% sodium deoxycholate, 0.1% sodium dodecyl sulfate, 0.15M sodium citrate) for 30 minutes at 37°C, after which 100 μL of PBS was added. Using a 96-well round bottom plate, 50 μL of sample cell lysate containing containing a protein concentration of 300 μg/mL was serially diluted into 100 μL of dithiothreitol (DTT) buffer (10 mL PBS, 0.01 g BSA, 0.015 g dithiothreitol). After the addition of 50 μL of 1% sheep red blood cells, the plate was incubated for 30 minutes at 37°C and 5% CO2, and centrifuged at 1000 × g for 10 minutes to collect non-lysed red blood cells. Lysis was measured by spectrophotometry of the resulting supernatants containing released hemoglobin at A450.
Rabbit corneal infections
New Zealand White rabbits (Harlan Rabbitry, Indianapolis, IN) were used in this study. They were maintained according to the guidelines of the University of Mississippi Medical Center Institutional Animal Care and Use Committee (IACUC) and the tenets of the Association for Research in Vision and Ophthalmology (ARVO) Resolution on the Use of Animals in Ophthalmic and Vision Research. Rabbits were anesthetized by subcutaneous injection of a mixture of xylazine (50 mg/kg; Lloyd Laboratories, Shenandoah, IA) and ketamine hydrochloride (10 mg/kg; Butler Animal Health Supply, Dublin, OH). Proparacaine hydrochloride (Akorn, Inc., Buffalo Grove, IL) was topically applied to each eye, and either S. pneumoniae K1263 or K1263ΔPLY (105 CFU in 10 μL) was injected intrastromally. Two observers, masked to the identity of the rabbit groups, used a biomicroscope to perform clinical examinations of infected rabbit corneas using seven ocular parameters: injection, chemosis, iritis, fibrin in the anterior chamber, hypopyon, corneal edema, and corneal infiltrate (infiltrate being defined as host cells, usually neutrophils, that infiltrate the eye in response to an infection) [40]. Each parameter was given a grade from 0 (normal) to 4 (most severe). The grades were totaled and averaged for the two observers resulting in an overall score ranging from 0 (normal) to a maximum of 28 (most severe). At 48 hours post-infection, rabbits were killed by an intravenous overdose of pentobarbital sodium (100 mg/mL; Sigma-Aldrich, St. Louis, MO). Corneas were removed, dissected, and homogenized in sterile PBS. Corneal homogenates were serially diluted and plated in triplicate on 5% sheep blood agar. Plates were incubated at 37°C for 24 hours. Colonies were counted and bacterial CFUs were determined and expressed in mean logarithmic units ± standard error of the means (SEM).
Histology of rabbit eyes
Whole rabbit eyes were dissected at 48 hours post-infection and placed in 4% paraformaldehyde. Histologic sectioning and hemotoxylin and eosin staining of the rabbit eyes were performed by Excalibur Pathology, Inc. (Moore, OK). Briefly, fixed eyes were processed to paraffin. Five micron sections were deparaffinized through xylene and rehydrated gradually in water containing decreasing concentrations of alcohol. The sections were stained with Gill III hematoxylin for 10 minutes, rinsed in water, dipped three times in acid alcohol, again rinsed in running water followed by ammonia water and 95% alcohol for one minute each. The sections were then treated with treosin for 15 seconds prior to three changes in 100% alcohold and three changes of xylene. The sections were finally coverslipped with resin.
Primary rabbit corneal epithelial cell line
Primary rabbit corneal epithelial cells were obtained as previously described [41]. Briefly, rabbits were anesthetized and euthanized as described above. The corneas were then excised from New Zealand white rabbit eyes, placed in 100-mm plates filled with 1% dispase in Keratinocyte Serum-Free Medium (KSFM; Invitrogen, Carlsbad, CA) and incubated at 4°C overnight. The following morning, a scalpel was used to gently remove the epithelial cells from the cornea. The rabbit transformation of donor DNA from a mutant of S. pneumoniae strain corneal epithelial (RCE) cells were suspended in 0.05% trypsin-EDTA (Invitrogen) and incubated for 30 minutes at 37°C. Cells were then suspended in KSFM supplemented with 1% penicillin-streptomycin, 0.1% amphotericin B and 10% fetal bovine serum. The RCE cells were maintained at 37°C and 5% CO2.
Cell culture exposure
Prior to exposure to bacterial extracts, RCE cells were suspended in 6-well or 96-well tissue culture plates in serum-free media in order to eliminate the inhibitory effect of serum cholesterol against pneumolysin. The tissue cultures were exposed to either medium alone or the intracellular or extracellular components of S. pneumoniae strains K1263 and K1263ΔPLY. Cells were co-incubated at 37°C in 5% CO2 for 1,3,6, or 24 hours. The bacteria-to-corneal epithelial cell ratio was approximately 100:1 for all of the experiments. After exposure to bacterial extracts, RCE cells were photographed and morphology was observed. Assays were performed in triplicate.
Cell viability
RCE cell viability was determined using a Live/Dead Viability/Cytotoxicity Kit (Invitrogen). Cell viability was determined on cells grown in a 96-well tissue culture plate, exposed to cell-free components and controls as described above, washed with Dulbecco’s PBS (D-PBS) and then treated with 100 μL D-PBS and 100 μL calcein AM for a final concentration of 2 μM calcein AM. A non-florescent calcein AM diffuses into intact live cells where it is hydrolyzed by intracellular esterases into calcein, a fluorescent compound that remains in the cell cytoplasm. Fluorescence was measured at 485/530 nm using a fluorescence microtiter plate spectrophotometer following a 30 minute incubation at room temperature. Values determined from RCE cells exposed to media alone were considered 100% live. Assays were performed in triplicate.
Statistics
Data were analyzed using the Statistical Analysis System (SAS) program for computers (Cary, NC). Clinical scores and cell viability data were analyzed using Non-parametric One-way ANOVA and CFU data were analyzed using General Linear Model of Least Square Means. A p value < 0.05 was considered significant.
Results
Creation of PLY-deficient mutant
A mutant deficient in PLY was successfully created in clinical keratitis strain K1263. Amplification of genomic DNA using primers PlymutF and PlymutR confirmed the presence of the Tmp resistance cassette with the flanking regions (1860 bp) in the mutant strain K1263ΔPLY and the presence of ply with flanking region (2605 bp) in parent strain K1263 (data not shown). The PLY-deficient mutant was confirmed with a hemolysis assay in which cell-free K1263 extract was able to lyse rabbit red blood cells while K1263ΔPLY was not (data not shown).
Rabbit challenge
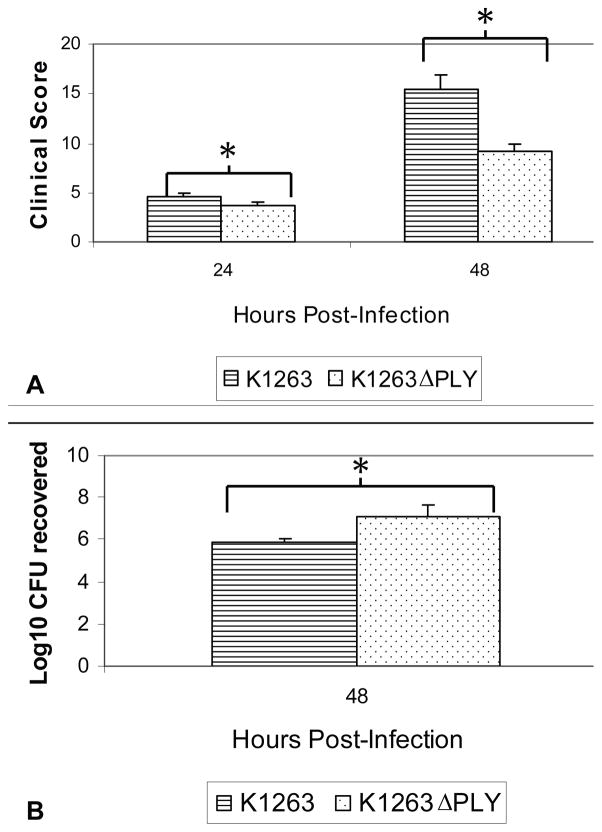
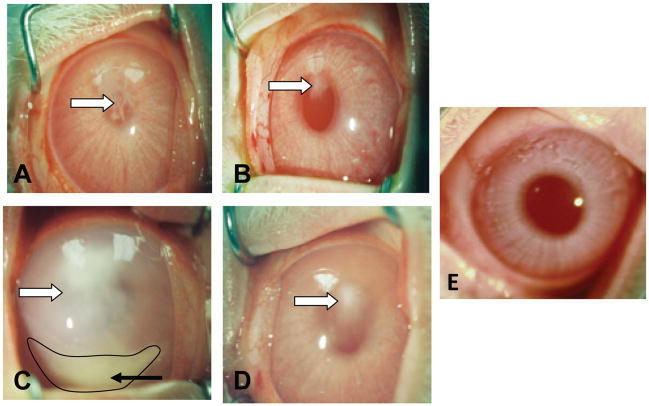
In a keratitis model of infection, the ocular pathology of the PLY-deficient mutant strain was significantly reduced when compared to the pathology caused by the parent strain. Clinical scores of rabbit corneas (n = 11) infected with K1263 (4.66 ± 0.37) were significantly higher than corneas (n = 17) infected with K1263ΔPLY (3.60 ± 0.26) at 24 hours post-infection (p = 0.023; Figure 1A). This difference increased at 48 hours post-infection such that the clinical scores of corneas infected with K1263 were 15.41 ± 1.42, significantly higher than those infected with K1263ΔPLY at 9.21 ± 0.78 (p = 0.0006; Figure 1). All seven parameters used for scoring keratitis were higher for the rabbits infected with parent strain K1263. Increased infiltration of immune cells (which are usually neutrophils in S. pneumoniae keratitis; unpublished findings) into the cornea was observed as early as 24 hours post-infection for corneas infected with K1263 when compared to those infected with K1263ΔPLY (Figure 2A–B). By 48 hours post-infection, there were considerably more infiltrating host cells in the eyes infected with K1263. Hypopyon, which is a collection of infiltrating host cells in the anterior chamber, was also present in the eyes of rabbits infected with K1263 but not with K1263ΔPLY (Figure 2C–D). Additionally, the log10 CFU recovered from corneas at 48 hours post-infection were significantly different between corneas such that those infected with the parent strain had less CFU recovered (5.86 ± 0.50, n = 10) than those infected with the mutant strain (7.13 ± 0.14, n = 16; p = 0.007, Figure 1B).
Figure 1.
(A) Average clinical scores of keratitis at 24 and 48 hours post-infection caused by parent (n = 11) or PLY-deficient isogenic mutant strain (n = 17). Pathology of the corneas was evaluated with slit lamp examination and the average clinical scores are provided. P = 0.023 at 24 hours post-infection and p = 0.0006 at 48 hours post-infection. (B) Average log10 CFU recovered from the corneas infected with the parent strain (n = 10) or the mutant strain (n = 16) at 48 hours post-infection. P = 0.007. Parent = K1263, Mutant = K1263ΔPLY. (*) indicates a significant difference between the scores. Scores are reported as the mean scores ± standard errors of the means.
Figure 2.
Representative eyes showing keratitis caused by either the parent strain (A,C), the PLY-deficient isogenic mutant strain (B,D), or an uninfected control (E). At 24 hours post-infection, there was more infiltration of host PMNs in eyes infected with the parent strain (A) compared to eyes infected with the mutant strain (B). The clinical symptoms worsened by 48 hours post-infection and appeared more severe in eyes infected with the parent strain (C) than those infected with the mutant strain (D). Parent = K1263, Mutant = K1263ΔPLY. White arrows indicates corneal infiltrate. Hypopyon is indicated by the black arrow and outlined in black.
Histopathology
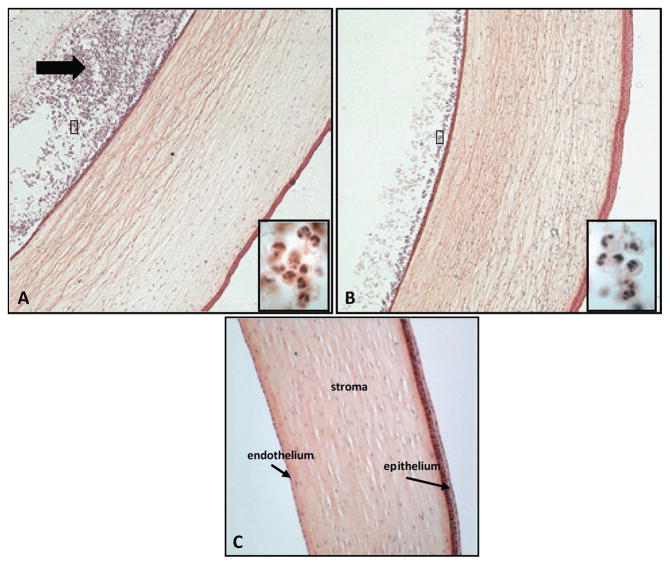
Histological examination of infected eyes show slight differences within the corneas such that the eye infected with the parent strain appeared slightly more edematous while the cornea infected with the PLY-deficient mutant strain had a slightly thicker epithelium layer (Figure 3). Athough, it is important to note, these observations may be due to small differences between the eyes of rabbits and may not be significant to the course of the infection. The striking difference between the two eyes is the considerably larger influx of immune cells into the aqueous humor of the eye infected with the parent strain compared to the eye infected with the mutant strain (Figure 3). Under higher magnification, the immune cells have the typical appearance of polymorphonuclear neutrophils (PMNs).
Figure 3.
Ocular histology from representative eyes infected with either the (A) parent, (B) the mutant strain, or (C) uninfected control. Boxed inserts (A & B) show higher magnification of PMNs in the anterior chambers of infected eyes. The corneas of the rabbits infected with the parent strain showed an influx of cells at the endothelium and in the anterior chamber (black arrow). Original magnification, 40X. Boxed insert magnification, 1000X.
Effects of PLY on corneal cells in vitro
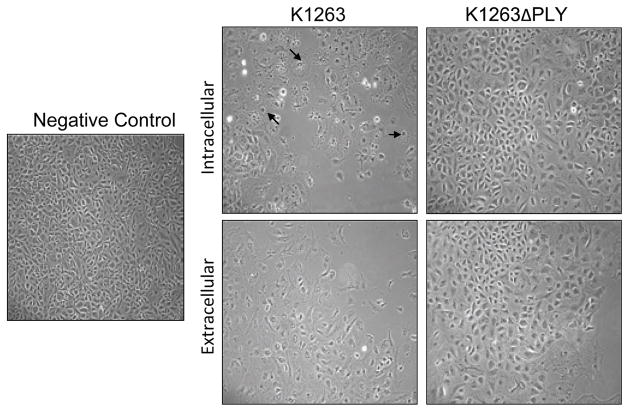
RCE cells exposed to K1263ΔPLY had reduced membrane damage and monolayer disruption, and higher percentages of live cells compared to cells exposed to the parent strain K1263 (Figures 4,5). These results were observed when cells were exposed to both the cell-free intracellular and extracellular components of bacteria. RCE cells exposed to either the intracellular or extracellular components of K1263 for three hours showed signs of cellular damage and death, whereas cells exposed to mutant bacteria showed reduced damage (Figure 4). Corneal cells exposed to the intracellular components of K1263 showed the most apparent disruption of the monolayer.
Figure 4.
Morphology of RCE cells treated with intracellular and extracellular components of K1263 and K1263ΔPLY for 3 hours at 37°C and 5% CO2. Black arrows indicate round, abnormal cells. Original magnification 100x.
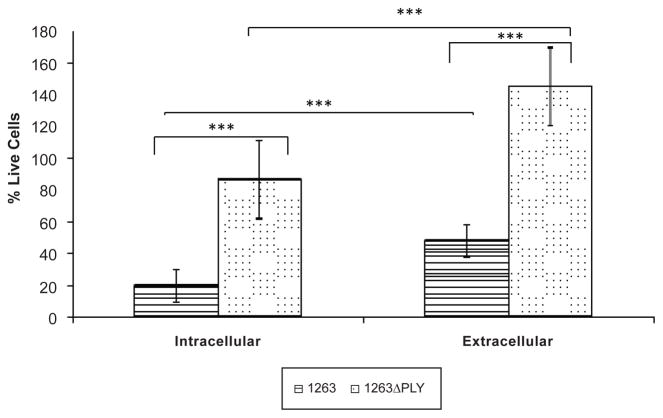
Figure 5.
Percent live RCE cells following treatment with intracellular and extracellular components of K1263 and K1263ΔPLY for 3 hours at 37°C and 5% CO2. RCE cells exposed to media alone were considered 100% viable. Following incubation, cells were treated with 2 μM calcein AM and the absorbance measured at 485/530 nm. (*) indicates a significant difference between cell viability. Scores are reported as the mean scores ± standard errors of the means. N equals 3 for all groups.
Cell viability assays performed under identical conditions confirmed the morphology results. RCE cells had a significantly lower percentage of live cells following exposure to the intracellular components of the PLY-producing parent strain, K1263, than those exposed to the intracellular components of the non-PLY producing mutant strain, K1263ΔPLY (19.56% ± 5.99, n = 3 vs. 86.23% ± 14.16, n = 3; p = 0.013). Additionally, there was a significant difference between the viability of RCE cells exposed to the extracellular components of K1263 and K1263ΔPLY such that RCE cells exposed to the PLY-producing parent strain, K1263, had a reduced cellular viability compared to those exposed to the non-PLY producing mutant strain (47.83% ± 7.33, n = 3 vs. 145.26% ± 15.11, n = 3; p = 0.0044; Figure 5). Interestingly, there was also a significant difference between the cell viability of RCE cells exposed to the intracellular and extracellular components of the same bacteria. Exposure to the intracellular components of either K1263 or K1263ΔPLY resulted in increased cellular toxicity than exposure to the extracellular components of the same strain, with the p values being 0.040 and 0.046, respectively (Figure 5).
Discussion
This study demonstrated the importance of PLY in causing much of the damage associated with pneumococcal keratitis using a rabbit model of infection. Additionally, the in vivo results successfully correlated with an in vitro model using primary rabbit corneal epithelial cells. The ability to use cultured corneal epithelial cells will allow for increased experimentation and determination of more precise mechanistic details involved with pneumococcal infections of the eye.
Previous research with pneumococcal keratitis has shown that PLY may be the predominant virulence factor in the cornea [40] since other major factors, such as capsule, do not seem to play a role [16,34]. Because earlier research on the role of PLY in pneumococcal keratitis used a strain of S. pneumoniae that had been passaged systemically in mice for 15 years [33], we wished to examine the role of PLY using a clinical keratitis isolate. Examination of the role of PLY in keratitis with a clinical ocular strain was important to test because another virulence factor that has long been deemed to be essential for pathogenesis in non-ocular infections – the polysaccharide capsule – has been shown to be non-essential for keratitis [16,34]. The observation that pneumococcal virulence factors are not necessarily the same for corneas and other anatomical sites underscores the possibility that clinical ocular strains may be genetically different than other strains. Considering that pneumococci are readily transformable and have been shown to exchange genetic information with other bacteria [42–45], it is possible that certain strains are adapted for the eye and certain strains are adapted for other areas of the host. Our results corroborate with the earlier study such that eyes infected with the PLY-deficient strain developed significantly less pathology than the eyes infected with the parent strain (Figures 2,3). Although significantly reduced, the pathology was not completely eliminated upon deletion of PLY. It is possible that other, as yet unknown, virulence factors play a role within the cornea or that the deletion of PLY allows for an upregulation of a known virulence factor that normally would not be a major cause of corneal pathology. It is also possible that pneumococcal cell wall, which is known to induce similar levels of inflammation as whole pneumococci in various models of disease [46–48], is responsible for at least a portion of the pathology still observed in eyes infected with the mutant PLY-deficient strain. Though beyond the scope of this study, the testing of purified cell wall and other pneumococcal virulence factors such as autolysin and zinc metalloproteases, which also stimulate inflammation [49,50], with this rabbit model of keratitis would lead to a better understanding of pneumococcal corneal infections.
Bacterial recovery from infected corneas also corroborates with the earlier study such that the mean log10 CFU recovered from corneas infected with the parent strain was significantly less than that recovered from corneas infected with the mutant strain [40]. It is unknown as to why the bacterial load was higher in corneas infected with the mutant strain, but one explanation could be that the presence of PLY causes a more robust activation of the innate immune response causing more neutrophils to enter the eyes infected with the parent strain and therefore more bacteria phagocytosed in those eyes. By the same token, however, more influx of neutrophils into the anterior chamber resulted in more overall ocular damage due to the host inflammatory response. Our results show the anterior chamber of the eye infected with the parent strain obviously contained more neutrophils than the eye infected with the mutant strain. However, histopathology did not show more host cells present in the corneas infected with the parent strain; in fact, the representative cornea infected with the mutant strain appeared to possibly have more cells, although the inflammatory cells were not quantified (Figure 3). It is possible that determining the precise quantity and type of immune cells within the cornea and/or anterior chamber of infected eyes would better explain the strain-dependent variations in the recovered bacterial loads.
Our in vitro results provided complementary data to the results seen in the rabbit model of keratitis such that the RCE cells exposed to the PLY-deficient mutant strain had reduced cell damage and increased viability when compared to the RCE cells exposed to the parent strain (Figures 4, 5). Caution should be taken, however, in the correlation of these data because the cultured cells were epithelial cells whereas the in vivo model involves direct intrastromal injection, and the histology sections from the in vivo model did not show epithelial disruption. This difference is one of the drawbacks of using the rabbit as a model because topical infection of rabbit corneas cannot be achieved with S. pneumoniae. However, the mouse model of pneumococcal keratitis [51] uses a topical scratch method and demonstrates the disruption of the corneal epithelium. Interestingly, RCE cells exposed to the intracellular components of PLY-deficient mutant pneumococci still had increased pathology (approximately 14% cell death) compared to a negative control (Figure 5), showing that one or more additional virulence factors other than PLY may participate in causing corneal damage. One such factor could be hydrogen peroxide. Hirst, et al. (2000) showed that H2O2 released from a pneumococcal strain deficient in PLY was capable of causing ciliary stasis in ependymal cells in addition to H2O2-induced cellular toxicity [52]. The ability of H2O2 to cause toxicity in ocular epithelial cells, however, is still unknown.
It is interesting to note that both the intracellular and extracellular components of the parent strain caused substantial damage, with the intracellular component causing the most significant cell pathology. While it is likely that factors in addition to PLY are causing host cellular damage, it is also possible that the intracellular component of K1263 caused such significant damage due to an incomplete extracellular release of PLY. This PLY would have then been released from the bacterial cells during the process of lysis by sonication. It was previously thought that PLY is released extracellularly by the action of autolysin, a pneumococcal protein that causes the bacterium to self-lyse [15]. Newer evidence shows that this process is more ambiguous than previously believed and PLY release can occur in an autolysin independent manner [53,54]. Additionally, the time in which PLY is released varies between strains in which some strains release PLY early in the bacterial life cycle while other strains release PLY late in the life cycle [53,55]. The difference in PLY release is one possible explanation for the reduced RCE cell viability observed following exposure to the intracellular components.
In summary, we have established an in vitro experimental system that correlates to what is observed in vivo. This will allow for additional data that would enhance and corroborate experiments performed in vivo. Additionally, PLY originating from a clinical keratitis isolate is a major virulence factor associated with pathology caused during pneumococcal keratitis. Since it is an important virulence factor in the cornea, PLY should be studied as a possible vaccine candidate for protection from pneumococcal keratitis. Better insight into the exact mechanisms used by PLY would be invaluable to our understanding and ultimately treatment of pneumococcal keratitis.
Acknowledgments
The authors would like to thank Mr. Regis Kowalski for providing the original bacterial strain K1263, and Dr. Larry McDaniel for providing ΔPLY2. We would also like to thank M. Elizabeth Fini and Gabriel M. Gordon (Keck School of Medicine, University of Southern California, Los Angeles, CA) for providing knowledgeable insight into the establishment of rabbit primary corneal epithelial cells.
This study was supported in part by Public Health Services Grant RO1 EY016195 (M.E.M.), National Eye Institute, National Institutes of Health, and by the University of Mississippi Medical Center.
Footnotes
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
- 1.Holden BA, Sweeney DF, Sankaridurg PR, Carnt N, Edwards K, et al. Microbial keratitis and vision loss with contact lenses. Eye Contact Lens. 2003:S131–S134. doi: 10.1097/00140068-200301001-00035. [DOI] [PubMed] [Google Scholar]
- 2.Jhanji V, Moorthy S, Vajpayee RB. Microbial keratitis in patients with down syndrome: a retrospective study. Cornea. 2009:163–165. doi: 10.1097/ICO.0b013e3181861d3a. [DOI] [PubMed] [Google Scholar]
- 3.Saeed A, D’Arcy F, Stack J, Collum LM, Power W, et al. Risk factors, microbiological findings, and clinical outcomes in cases of microbial keratitis admitted to a tertiary referral center in Ireland. Cornea. 2009;28:285–292. doi: 10.1097/ICO.0b013e3181877a52. [DOI] [PubMed] [Google Scholar]
- 4.Wagoner MD, Al-Ghamdi AH, Al-Rajhi AA. Bacterial keratitis after primary pediatric penetrating keratoplasty. Am J Ophthalmol. 2007;143:1045–1047. doi: 10.1016/j.ajo.2006.12.035. [DOI] [PubMed] [Google Scholar]
- 5.Norina TJ, Raihan S, Bakiah S, Ezanee M, Liza-Sharmini AT, et al. Microbial keratitis: aetiological diagnosis and clinical features in patients admitted to Hospital Universiti Sains Malaysia Singapore. Med J. 2008;49:67–71. [PubMed] [Google Scholar]
- 6.Bharathi MJ, Ramakrishnan R, Vasu S, Meenakshi R, Shivkumar C, et al. Epidemiology of bacterial keratitis in a referral centre in South India. Indian J Med Microbiol. 2003;21:239–245. [PubMed] [Google Scholar]
- 7.Bharathi MJ, Ramakrishnan R, Meenakshi R, Padmavathy S, Shivakumar C, et al. Microbial keratitis in South India: influence of risk factors, climate, and geographical variation. Ophthalmic Epidemiol. 2007;14:61–69. doi: 10.1080/09286580601001347. [DOI] [PubMed] [Google Scholar]
- 8.Pepose JS, Wilhelmus KR. Divergent approaches to the management of corneal ulcers. Am J Ophthalmol. 1992;114:630–632. doi: 10.1016/s0002-9394(14)74496-4. [DOI] [PubMed] [Google Scholar]
- 9.Bhave P, Chamie G. Streptococcus pneumoniae keratitis. J Hosp Med. 2008:353. doi: 10.1002/jhm.306. [DOI] [PubMed] [Google Scholar]
- 10.Dada T, Sharma N, Dada VK, Vajpayee RB. Pneumococcal keratitis after laser in situ keratomileusis. J Cataract Refract Surg. 2000:460–461. doi: 10.1016/s0886-3350(99)00349-1. [DOI] [PubMed] [Google Scholar]
- 11.Parmar P, Salman A, Kalavathy CM, Jesudasan CA, Thomas PA. Pneumococcal keratitis: a clinical profile. Clin Experiment Ophthalmol. 2003;26:44–47. doi: 10.1046/j.1442-9071.2003.00598.x. [DOI] [PubMed] [Google Scholar]
- 12.Bharathi MJ, Ramakrishnan R, Vasu S, Meenakshi, Palaniappan R. Aetiological diagnosis of microbial keratitis in South India - A study of 1618 cases. Indian J Med Microbiol. 2002;20:19–24. [PubMed] [Google Scholar]
- 13.Green M, Apel A, Stapleton F. Risk factors and causative organisms in microbial keratitis. Cornea. 2008;27:22–27. doi: 10.1097/ICO.0b013e318156caf2. [DOI] [PubMed] [Google Scholar]
- 14.Kunimoto DY, Sharma S, Reddy MK, Gopinathan U, Jyothi J. Microbial keratitis in children. Ophthalmology. 1998:252–257. doi: 10.1016/s0161-6420(98)92899-8. [DOI] [PubMed] [Google Scholar]
- 15.Jedrzejas MJ. Pneumococcal virulence factors: structure and function. Microbiol Mol Biol Rev. 2001;65:187–207. doi: 10.1128/MMBR.65.2.187-207.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reed JM, O’Callaghan RJ, Girgis DO, McCormick CC, Caballero AR, et al. Ocular virulence of capsule-deficient Streptococcus pneumoniae in a rabbit keratitis model. Invest Ophthalmol Vis Sci. 2005;46:604–608. doi: 10.1167/iovs.04-0889. [DOI] [PubMed] [Google Scholar]
- 17.Callegan MC, Engel LS, Hill JM, O’Callaghan RJ. Corneal virulence of Staphylococcus aureus: roles of alpha-toxin and protein A in pathogenesis. Infect Immun. 1994;62:2478–2482. doi: 10.1128/iai.62.6.2478-2482.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Callegan MC, Engel LS, Clinch TE, Hill JM, Kaufman HE. Efficacy of tobramycin drops applied to collagen shields for experimental staphylococcal keratitis. Curr Eye Res. 1994;13:875–878. doi: 10.3109/02713689409015089. [DOI] [PubMed] [Google Scholar]
- 19.Hagan M, Wright E, Newman M, Dolin P, Johnson G. Causes of suppurative keratitis in Ghana. Br J Ophthalmol. 1995;79:1024–1028. doi: 10.1136/bjo.79.11.1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ormerod LD. Causation and management of microbial keratitis in subtropical Africa. Ophthalmology. 1987;94:1662–1668. doi: 10.1016/s0161-6420(87)33235-x. [DOI] [PubMed] [Google Scholar]
- 21.Robinson KA, Baughman W, Rothrock G, Barrett NL, Pass M, et al. Epidemiology of invasive Streptococcus pneumoniae infections in the United States, 1995–1998: Opportunities for prevention in the conjugate vaccine era. JAMA. 2001:1729–1735. doi: 10.1001/jama.285.13.1729. [DOI] [PubMed] [Google Scholar]
- 22.Tweten RK. Cholesterol-dependent cytolysins, a family of versatile poreforming toxins. Infect Immun. 2005;73:6199–6209. doi: 10.1128/IAI.73.10.6199-6209.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Palmer M. The family of thiol-activated, cholesterol-binding cytolysins. Toxicon. 2001;39:1681–1689. doi: 10.1016/s0041-0101(01)00155-6. [DOI] [PubMed] [Google Scholar]
- 24.Paton JC, Rowan-Kelly B, Ferrante A. Activation of human complement by the pneumococcal toxin pneumolysin. Infect Immun. 1984;43:1085–1087. doi: 10.1128/iai.43.3.1085-1087.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Houldsworth S, Andrew PW, Mitchell TJ. Pneumolysin stimulates production of tumor necrosis factor alpha and interleukin-1 beta by human mononuclear phagocytes. Infect Immun. 1994;62:1501–1503. doi: 10.1128/iai.62.4.1501-1503.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thornton J, McDaniel LS. THP-1 monocytes up-regulate intercellular adhesion molecule 1 in response to pneumolysin from Streptococcus pneumoniae. Infect Immun. 2005;73:6493–6498. doi: 10.1128/IAI.73.10.6493-6498.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Colino J, Snapper CM. Two distinct mechanisms for induction of dendritic cell apoptosis in response to intact Streptococcus pneumoniae. J Immunol. 2003;171:2354–2365. doi: 10.4049/jimmunol.171.5.2354. [DOI] [PubMed] [Google Scholar]
- 28.Boulnois GJ, Paton JC, Mitchell TJ, Andrew PW. Structure and function of pneumolysin, the multifunctional, thiol-activated toxin of Streptococcus pneumoniae. Mol Microbiol. 1991;5:2611–2616. doi: 10.1111/j.1365-2958.1991.tb01969.x. [DOI] [PubMed] [Google Scholar]
- 29.Mitchell TJ, Andrew PW, Saunders FK, Smith AN, Boulnois GJ. Complement activation and antibody binding by pneumolysin via a region of the toxin homologous to a human acute-phase protein. Mol Microbiol. 1991;5:1883–1888. doi: 10.1111/j.1365-2958.1991.tb00812.x. [DOI] [PubMed] [Google Scholar]
- 30.Boulnois GJ. Pneumococcal proteins and the pathogenesis of disease caused by Streptococcus pneumoniae. J Gen Microbiol. 1992;138:249–259. doi: 10.1099/00221287-138-2-249. [DOI] [PubMed] [Google Scholar]
- 31.Johnson MK, Hobden JA, O’Callaghan RJ, Hill JM. Confirmation of the role of pneumolysin in ocular infections with Streptococcus pneumoniae. Curr Eye Res. 1992;11:1221–1225. doi: 10.3109/02713689208999547. [DOI] [PubMed] [Google Scholar]
- 32.Ng EW, Samiy N, Rubins JB, Cousins FV, Ruoff KL, et al. Implication of pneumolysin as a virulence factor in Streptococcus pneumoniae endophthalmitis. Retina. 1997;17:521–529. [PubMed] [Google Scholar]
- 33.Briles DE, Nahm M, Schroer K, Davie J, Baker P, et al. Antiphosphocholine antibodies found in normal mouse serum are protective against intravenous infection with type 3 Streptococcus pneumoniae. J Exp Med. 1981;153:694–705. doi: 10.1084/jem.153.3.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Norcross EW, Tullos NA, Taylor SD, Sanders ME, Marquart ME. Assessment of Streptococcus pneumoniae capsule in conjunctivitis and keratitis in vivo neuraminidase activity increases in nonencapsulated pneumococci following conjunctival infection. Curr Eye Res. 2010;35:787–798. doi: 10.3109/02713683.2010.492462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Braun JS, Hoffmann O, Schickhaus M, Freyer D, Dagand E, et al. Pneumolysin causes neuronal cell death through mitochondrial damage. Infect Immun. 2007;75:4245–4254. doi: 10.1128/IAI.00031-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zysk G, Schneider-Wald BK, Hwang JH, Bejo L, Kim KS, et al. Pneumolysin is the main inducer of cytotoxicity to brain microvascular endothelial cells caused by Streptococcus pneumoniae. Infect Immun. 2001;69:845–852. doi: 10.1128/IAI.69.2.845-852.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rubins JB, Duane PG, Charboneau D, Janoff EN. Toxicity of pneumolysin to pulmonary endothelial cells in vitro. Infect Immun. 1992;60:1740–1746. doi: 10.1128/iai.60.5.1740-1746.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tuomanen EI. Pathogenesis of pneumococcal inflammation: otitis media. Vaccine. 2000;19:S38–S40. doi: 10.1016/s0264-410x(00)00276-0. [DOI] [PubMed] [Google Scholar]
- 39.Pozzi G, Masala L, Iannelli F, Manganelli R, Havarstein LS, et al. Competence for genetic transformation in encapsulated strains of Streptococcus pneumoniae: two allelic variants of the peptide pheromone. J Bacteriol. 1996;178:6087–6090. doi: 10.1128/jb.178.20.6087-6090.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Johnson MK, Hobden JA, O’Callaghan RJ, Hill JM. The role of pneumolysin in ocular infections with Streptococcus pneumoniae. Curr Eye Res. 1990;11:1107–1114. doi: 10.3109/02713689008997584. [DOI] [PubMed] [Google Scholar]
- 41.Ouyang J, Shen YC, Yeh LK, Li W, Coyle BM, et al. Pax6 overexpression suppresses cell proliferation and retards the cell cycle in corneal epithelial cells. Invest Ophthalmol Vis Sci. 2006;47:2397–2407. doi: 10.1167/iovs.05-1083. [DOI] [PubMed] [Google Scholar]
- 42.Cvitkovitch DG. Genetic competence and transformation in oral streptococci. Crit Rev Oral Biol Med. 2001;12:217–243. doi: 10.1177/10454411010120030201. [DOI] [PubMed] [Google Scholar]
- 43.Wu K, Zhang X, Shi J, Li N, Li D, et al. Immunization with a combination of three pneumococcal proteins confers additive and broad protection against Streptococcus pneumoniae infections in mice. Infect Immun. 2010;78:1276–1283. doi: 10.1128/IAI.00473-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Santagati M, Lupo A, Scillato M, Di Martino A, Stefani S. Conjugal mobilization of the mega element carrying mef(E) from Streptococcus salivarius to Streptococcus pneumoniae. FEMS Microbiol Lett. 2009;290:79–84. doi: 10.1111/j.1574-6968.2008.01408.x. [DOI] [PubMed] [Google Scholar]
- 45.Ding F, Tang P, Hsu MH, Cui P, Hu S, et al. Genome evolution driven by host adaptations results in a more virulent and antimicrobial-resistant Streptococcus pneumoniae serotype 14. BMC Genomics. 2009;10:158. doi: 10.1186/1471-2164-10-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Carlsen BD, Kawana M, Kawana C, Tomasz A, Giebink GS. Role of the bacterial cell wall in middle ear inflammation caused by Streptococcus pneumoniae. Infect Immun. 1992;60:2850–2854. doi: 10.1128/iai.60.7.2850-2854.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tuomanen E, Liu H, Hengstler B, Zak O, Tomasz A. The induction of meningeal inflammation by components of the pneumococcal cell wall. J Infect Dis. 1985;151:859–868. doi: 10.1093/infdis/151.5.859. [DOI] [PubMed] [Google Scholar]
- 48.Tuomanen E, Rich R, Zak O. Induction of pulmonary inflammation by components of the pneumococcal cell surface. Am Rev Respir Dis. 1987;135:869–874. doi: 10.1164/arrd.1987.135.4.869. [DOI] [PubMed] [Google Scholar]
- 49.Bruyn GA, Zegers BJ, van Furth R. Mechanisms of host defense against infection with Streptococcus pneumoniae. Clin Infect Dis. 1992;14:251–262. doi: 10.1093/clinids/14.1.251. [DOI] [PubMed] [Google Scholar]
- 50.Blue CE, Paterson GK, Kerr AR, Bergé M, Claverys JP, et al. ZmpB, a novel virulence factor of Streptococcus pneumoniae that induces tumor necrosis factor alpha production in the respiratory tract. Infect Immun. 2003;71:4925–4935. doi: 10.1128/IAI.71.9.4925-4935.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Moore QC, 3rd, McCormick CC, Norcross EW, Onwubiko C, Sanders ME, et al. Development of a Streptococcus pneumoniae Keratitis Model in Mice. Ophthalmic Res. 2009;42:141–146. doi: 10.1159/000229028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hirst RA, Sikand KS, Rutman A, Mitchell TJ, Andrew PW, et al. Relative roles of pneumolysin and hydrogen peroxide from Streptococcus pneumoniae in inhibition of ependymal ciliary beat frequency. Infect Immun. 2000;68:1557–1562. doi: 10.1128/iai.68.3.1557-1562.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Balachandran P, Hollingshead SK, Paton JC, Briles DE. The autolytic enzyme LytA of Streptococcus pneumoniae is not responsible for releasing pneumolysin. J Bacteriol. 2001;183:3108–3116. doi: 10.1128/JB.183.10.3108-3116.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Price KE, Camilli A. Pneumolysin localizes to the cell wall of Streptococcus pneumoniae. J Bacteriol. 2009;191:2163–2168. doi: 10.1128/JB.01489-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Briles DE, Hollingshead SK, Swiatlo E, Brooks-Walter A, Szalai A, et al. PspA and PspC: their potential for use as pneumococcal vaccines. Microb Drug Resist. 1997;3:401–408. doi: 10.1089/mdr.1997.3.401. [DOI] [PubMed] [Google Scholar]