Abstract
The effectiveness of a cognitive-behavioral program, Transition Preparation Training (TPT), in combination with spina bifida (SB) management was compared to adolescents with SB who received only SB management. Design, setting and participants: Prospective controlled trial with an ethnically diverse sample (94%) of 65 adolescents with SB (31 in treatment group [mean age: 16.19]; 34 in control group [mean age: 15.71]) conducted at Childrens Hospital Los Angeles between September 2006 and September 2008. Interventions: TPT was a three-module, eight sessions program offered in a 2 day workshop format to facilitate development of health care transition plan. Main outcome measures: Subjective well being as measured by the Personal Adjustment and Role Skills Scale (PARS III), Role mastery measured using Community Life Skills Scale (CLSS), and Self Care Practice with the Denyes Self-Care Practice Instrument (DSCPI-90©). Results: No significant differences were found between groups of any treatment effect or treatment follow-up interaction. No substantial changes in the scores either between treatments of post treatments were found.
Keywords: Transition, adolescence, pediatrics, spina bifida, disability
Introduction
Spina bifida (SB), a neural tube defect occurring during the first month of gestation, affects approximately 1,500 infants born annually. SB manifestations vary depending on the extent of closure failure and the level of the spinal cord lesion ranging from benign small vertebral defect (SB occulta) to significant protrusion of the meninges and spinal cord within the sac with cerebral spinal fluid (myelomeningocele). The more severe forms of SB result in urinary and bowel incontinence, motor, sensory and reflex dysfunction, and musculoskeletal impairments (1).
The life expectancy of individuals born with SB has increased dramatically with the advances in medical management. Today, the life expectancy of individuals with SB extends well into adulthood, although accompanied by ongoing health problems, secondary conditions and less than satisfactory adulthood lifestyle outcomes and quality of life (2–6). The research data on young and older adults with SB indicate that rates of employment, educational level, socioeconomic status, indices of community involvement and social relationships are not comparable to adults without SB (6).
A preponderance of studies examining health outcomes of adolescents and young adults with SB in the transition from pediatric care indicate that their health status is adversely affected (2,3,8,9). These untoward outcomes include shunt malfunction, renal dysfunction, deterioration of locomotor skills and increased orthopedic problems (10). Other health problems were obesity, poor physical fitness, fatigue and increased cardiovascular disease risk (11).
A number of factors have been identified as contributing to their deteriorating health status post transition. These factors included limited access to health care services and instructional support to manage their SB regimen, service ineligibility, and lack of service coordination. Adolescent-related variables included lack of skills and knowledge in managing their SB and health care self advocacy (12–15) Adolescents and their families reported service-related gaps with transition planning which included inadequate assistance with information on community resources for health, transportation, education and employment (13–16).
Investigations exploring the lifestyle outcomes of individuals with SB demonstrate the numerous difficulties. Lower rates of high school completion, as high as 50%, college graduation and completion of vocational/technical certificate programs have been reported for students with SB as compared to peers (6). Rates of unemployment of adults with SB have been reported at 60% or greater (6,8,16). Reduced rates of community and social involvements were revealed as evidenced by the low percentages of individuals with SB who live independently, are married, and drive a car (6,8,16).
Experts have suggested that these negative outcomes are the result of a combination of psychosocial and environmental factors. Research findings reveal that the emotional and behavioral development of adolescents with SB lag behind their age-mates (17). Higher levels of dependency including prolonged reliance on parents for their self management regimen have been reported (3,17,18). A number of studies found adolescents with SB to be at higher psychosocial risk for behavioral adjustment, mental health problems and lower self esteem (18, 19). Experts have suggested that disparities in adulthood outcomes can be attributed partially to the inadequate preparation by their service providers for the developmental and lifestyle expectations of adulthood (2,4,20,21).
Currently, there is a lack of evidence on the effectiveness of service models to prepare adolescents with special health care needs, including those with SB for the transition to adulthood including the transfer from pediatric to adult health care (15,22). Most of the research conducted with transition aged adolescents with SB has explored psychosocial concerns, self management and provided descriptions of unmet needs (12,13,15,17). Testing intervention models is needed with the goal of developing evidence-based transition services and improving outcomes for adolescents with SB.
The goal of this prospective controlled trial, as part of a larger study, was to examine whether a cognitive-behavioral program of Transition Preparation Training (TPT), in combination with SB management, leads to improved transition subjective well being, role mastery, and self care practice. The specific aims of this project were to compare adolescents with SB who received TPT in combination with SB management to adolescents with SB who received only SB management by testing the following hypotheses: 1) greater improvement in subjective well-being as measured by the Personal Adjustment and Role Skills Scale (PARS III) will be observed in adolescents who receive TPT compared to adolescents who do not (23); 2) greater improvement in role mastery as measured by the Community Life Skills Scale (CLSS) will be observed in adolescents who receive TPT compared to adolescents who do not (24); and 3) greater improvement in self-care practice as measured by the Denyes Self-Care Practice Instrument (DSCPI-90©) will be observed in adolescents who receive TPT services compared to adolescents who do not (25).
Methods
A convenience sample of youth and their parents was recruited from the SBclinics at Childrens Hospital Los Angeles (CHLA) and Los Angeles County Medical Center (LAC) Women’s and Children’s Hospital according to the study’s inclusion criteria. Letters of invitation to participate were sent to a SB support group in Southern California. The data collection period was from September 2006 to September 2008.
This study was reviewed and approved by the CHLA Clinical Coordinating Committee (CCI) (CHLA’s Institutional Review Board [IRB]). The CHLA CCI served as the coordinating IRB for youth and parents recruited from the other two data collection sites. Informed consent was obtained from parents and adolescents (18 years), and assent from youth younger than 18 years of age. At each data collection, youth received $25 and their parents received $25 retail card. Additionally, youth enrolled in either the treatment or control groups were eligible for a raffle prize of a Playstation.
Eligibility criteria
Study eligibility criteria for inclusion for youth with SB were: a) 14 to 18 years; b) diagnosis of SB; d) English speaking; e) no history of intellectual disability or mental illness; and g) willingness to complete questionnaires independently or with surrogate assistance. Parental eligibility criteria were: a) has child with SB, 14 to 18 years; b) English or Spanish speaking; and c) mother/father/non-related guardian of youth in the study’s treatment or control groups.
Design
This was a prospective randomized controlled trial. After consent/assent were obtained, youth were randomly assigned to the usual SB management control group or to the TPT and usual SB management treatment group. The randomization scheme was a randomization to treatment versus control stratified by gender.
Outcome measures
Pre and post intervention data were collected from both groups of youth and their parents at T1 (baseline) and T2 (4 months later). Post treatment data (T2) were collected on average at 4.3 months; control data (T2) were collected at 4.1 months. Parents completed the PARS III (23) and the parent version of the TDQ. Adolescents completed five subscales of the CLSS (24), the DSCPI-90©) (25) and the youth version of the TDQ.
Subjective well-being
The PARS III (23) was used to measure subjective well-being. This instrument assesses the psychosocial adjustment of children and youth with SHCN without cognitive impairments. The PARS III contains 28 items measuring six areas of functioning associated with maladjustment: peer relations, dependency, hostility, productivity, anxiety-depression and withdrawal. It does not contain items about chronic condition symptomology that create potential measurement biases. Coefficient alpha estimates for all subscales range from 0.70 to 0.80. Estimates of internal consistency for total scores range from 0.88 to 0.90.
Role mastery
The Community Life Skills Scale (CLSS) (24) was used to collect data on the extent to which a respondent lives independently and uses community resources. This 33 item tool, using a binary scale (yes/no) contains 6 areas of foci measuring various types of community skills. Five CLSS subscales-(excluding the budgeting subscale) transportation, support services, support-involvement, interest-hobbies and regularity-organization-routines amounting to 28 items were used in this study. Cronbach alpha for the CLSS has been reported as .69 with initial administration and .63 at 1 and 2 years.
Self-care practice
Self-care practice was assessed using the Denyes Self-Care Practice Instrument (DSCPI-90©), (25) an 18 item self-report questionnaire measuring both general health behaviors (e.g., making decisions to maintain one’s health) and specific self-care behaviors (e.g. managing stress levels). Respondents record responses to items using a ratio scale from 0, referring to none at all, to 100, referring to all the time. Higher scores reflect a higher level of self-care abilities. Initial and subsequent evidence of internal consistency, alternate forms, and test-retest reliability, and content and construct validity were demonstrated by Denyes and others (25–33). Test-retest reliability of .84 to .92 has been reported in studies conducted primarily with adolescents (29–32). This tool has been used with healthy adolescents, and adolescents with type 1 diabetes (30, 31, 33).
Demographic questionnaires
The Transition Questionnaire Youth and Parent Versions (TDQ) were developed by the investigators. The TDQ is a 24 item self-report questionnaire that includes specifics about the youth’s SHCN, functional limitations, educational level and work experience, family composition, and race/ethnicity. It also contains items about the adolescent’s SB that include the level of the lesion, presence of shunt, number of shunt revisions, presence of hydrocephalus and number of complications experienced during the past year. The parent version contained eight items pertaining to age, gender, marital status, race/ethnicity, number of children, educational level, zip code (community SES), and parental relationship.
Transition preparation training program intervention
The Transition Preparation Training Program (TPT) was a three-module, eight session program offered in a 2 day workshop format (Day 1: 5 hours; Day 2: 4.5 hours) that involved the development of an adolescent-centered transition plan (Transition Roadmap to the Future) based on comprehensive assessment of the adolescent’s goals for the future. Module One (two sessions) involved a comprehensive assessment of the adolescent’s goals and dreams for the future related to health, school, work, community living, housing, recreation and leisure. This assessment was an interactive process led by the trainer involving the adolescent and other adolescent members of the group. Module Two (two sessions) involved creating a comprehensive transition plan to achieve the adolescent’s goals for the future, based upon the Module One assessment. The plan included identification of service needs, service referrals and contact information. Module Three (four sessions) provided adolescents with SB with learning opportunities to practice strategies for obtaining the services they identified in their transition plan. A number of instructional strategies were used that included the following: role playing, one-to-one consultation, coaching, reinforced learning, use of audio visual aids, accessing the Internet, and mentored learning
Participant flow
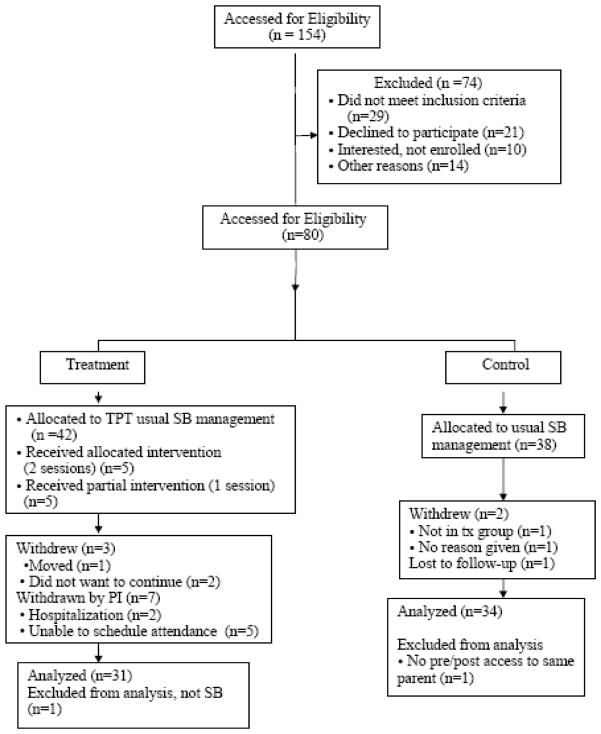
From a total of 154 youth who were assessed for eligibility, 80 youth with SB meeting inclusion criteria were randomized to treatment (42) and control (38) groups. Five withdrew, nine were excluded for various reasons and one was lost to follow-up, thus there were 31 youth in the treatment group and 34 in the control group. Of those in the treatment group, 5 attended the first workshop only. The flow chart as depicted in figure 1 summarizes participants recruited, group assignment, completion of the protocol, withdrawal from the study and those included in the data analysis.
Figure 1.
Diagram for this study.
Statistical analyses
Standard summary descriptive statistics were used for comparison of the two treatment groups including demographic and baseline variables.
Initially a linear regression random effects model was used to compare the summary scores which included a fixed term for treatment and follow up, as well as a treatment follow up interaction term. Since none of the data showed either a statistically significant or even a strong suggestion of an interaction, the final analysis was performed without any interaction terms. Thus the primary method of statistical analysis was a main effects model applied separately to all the outcome measurements of interest with the families included as a random effect.
Results
The period of recruitment was from September 2006 to September 2008. Nearly all (94%) of the participants in both the treatment and control groups were ethnically diverse with nearly 90% Latinos; 6% of the sample white. The mean age of youth in the experimental group was 16.19 years (SD = 1.33) and in the control group was 15.71 years (SD = 1.43). Most of the parents were monolingual Spanish speakers (48); the majority of parents were married and had attended secondary educational programs. The sociodemographic data of the youth enrolled in the study and their parents are presented in table 1.
Table 1.
Demographic data
| Youth | Experimental Group (n=31) | Control Group (n=34) | All (n=65) |
|---|---|---|---|
| Age in years [M (SD]) | 16.19 (1.33) | 15.71 (1.43) | 15.95 |
| N (%) | N (%) | N (%) | |
| Gender | |||
| Male | 13 (42) | 13 (40) | 27 (40) |
| Female | 18 (58) | 21 (60) | 39 (60) |
| Grade Level | |||
| High School | 26 (84) | 27 (80) | 53 (82) |
| College | 3 (10) | 1 (2) | 4 (6) |
| Not Identified | 2 (6) | 6 (18) | 8 (12) |
| Ethnicity | |||
| White | 3 (10) | 1 (3) | 4 (6) |
| Latino | 27 (87) | 31 (91) | 58 (90) |
| MultiEthnic | 1 (3) | 1 (3) | 2 (3) |
| Asian | 1 (3) | 1 (1) | |
| Parents | |||
| Age in years [M (SD]) | 43.25 (5.46) | 40.15 (6.54) | 41.84 |
| Biological Mother | 26 (84) | 33 (97) | 59 (92) |
| Biological Father | 3 (10) | 1 (3) | 4 (6) |
| Adoptive Mother | 1 (3) | 1 (1) | |
| Legal Guardian | 1 (3) | 1 (1) | |
| Marital Status | |||
| Married | 19 (62) | 18 (52) | 37 (57) |
| Living with Partner | 1 (3) | 2 (6) | 3 (5) |
| Separated | 5 (16) | 2 (6) | 7 (11) |
| Divorced | 1 (3) | 6 (18) | 7 (11) |
| Never Married | 4 (13) | 6 (18) | 10 (15) |
| Not Identified | 1 (3) | 1 (1) | |
| Highest Educational Level | |||
| Elementary | 9 (29) | 9 (27) | 18 (28) |
| Middle School (7, 8 grade) | 3 (10) | 3 (8) | 6 (9) |
| High School | 14 (45) | 16 (47) | 30 (46) |
| College | 1 (3) | 6 (18) | 7 (11) |
| Graduate School | 3 (10) | 3 (5) | |
| Other | 1 (3) | 1 (1) | |
| Ethnicity | |||
| White | 3 (10) | 1 (3) | 4 (6) |
| Latino | 27 (87) | 31 (91) | 58 (89) |
| Asian | 1 (3) | 1 (1) | |
| MultiEthnic | 1 (3) | 1 (1) | |
| Black | 1 (3) | 1 (1) |
Outcome measures
The only outcome measurement that showed any treatment effect was the support services sub-scale of the CLSS (p=0.010). However, this simply reflects a difference that was present at baseline. Because of the absence of any treatment effect or treatment follow-up interaction, the results for the two groups were combined to investigate possible changes over time. Only the dependency subscale from the PARS questionnaire (p=0.001) showed a significant increase post treatment and regularity-organization-routines subscale from the CLSS showed a significant decrease (p=0.011) in post treatment scores. Otherwise, there were no substantial changes in the scores of either group of post treatment measurements.
The baseline mean summary PARS scores of the treatment and control groups were 83.41 (SD = 8.68) and 81.45 (SD = 13.11) respectively (see table 2). The follow-up mean PARS summary scores of the treatment group was 85.7 (SD = 11.98) and control group was 84.4 (SD = 11.77). The highest and lowest subscale scores were similar for both treatment and control groups. The highest baseline and follow-up subscale scores were for the hostility subscale for the treatment and control groups. Both treatment and control groups lowest baseline and follow-up subscale scores were for the peer subscale.
Table 2.
PARS III
| SCORES | Time | Treatment | Control | p-value | p-value |
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Follow up | treatment | ||
| Summary | 1 | 83.41 (8.68) | 81.45 (13.11) | ||
| 0.126 | |||||
| 2 | 85.7 (11.98) | 84.41 (11.77) | |||
| Summary Total | 1 & 2 | 82.95 (12.44) | 84.56 (10.44) | 0.942 | |
| Subscales | 1 | ||||
| Peer | 1 | 10.3 (3.2) | 10.8 (2.7) | 0.308 | 0.987 |
| Peer | 2 | 10.3 (3.1) | 10.8 (2.7) | ||
| Dependency | 1 | 11.4 (1.8) | 11.1 (2.3) | 0.001 | 0.423 |
| Dependency | 2 | 12.6 (1.9) | 12.0 (1.6) | ||
| Hostility | 1 | 18.8 (3.0) | 18.7 (4.1) | 0.188 | 0.993 |
| Hostility | 2 | 19.5 (2.7) | 19.4 (3.3) | ||
| Productivity | 1 | 11.8 (2.7) | 11.4 (2.8) | 0.863 | 0.990 |
| Productivity | 2 | 11.4 (2.9) | 11.8 (3.1) | ||
| Anxiety-Depression | 1 | 18.5 (17.8) | 17.7 (3.5) | 0.604 | 0.064 |
| Anxiety-Depression | 2 | 19.0 (3.2) | 17.8 (3.5) | ||
| Withdrawn | 1 | 12.4 (2.3) | 11.7 (3.0) | 0.022 | 0.608 |
| Withdrawn | 2 | 12.9 (2.4) | 13.0 (2.4) |
1 refers to baseline data; 2 refers to follow-up data;
Peer has the lowest subscale score and Hostility has the highest subscale scores.
p-value based on a main effects regression model with family as a random effect.
The baseline DSCPI 90© mean score of the treatment group was 62.25 (SD = 17.29; range 0 to 93.61) and 58.99 (SD = 20.19; range, 16.66 to 99.44) of the control group (see table 3). Follow-up mean scores of the treatment and control groups were 63.29 (SD = 13.73; range, 31.11 to 86. 66) and 66.99 (SD = 17.61; range 27.5 to 99. 77), respectively. Highest and lowest DSCPI-90© item scores for both groups were the same. The lowest score for both groups for baseline and follow-up measurements was related to putting off doing things good for your health. The highest score on DSCPI-90© pre and post measurements was related to safety.
Table 3.
DSCPI-90©
| Scores | Time | Treatment | Control |
|---|---|---|---|
| Mean (S.D.) | Mean (S.D.) | ||
| Summary | 1 | 62.25 (17.29) | 58.99 (20.19) |
| 2 | 63.29 (13.73) | 66.99 (17.61) | |
| Results of hypothesis tests | Follow up | p = 0.031 | |
| treatment | p = 0.894 | ||
| Individual Item Means | |||
| 1. Do things good for health | 1 | 64.83 (23.99) | 58.17 (28.45) |
| 2 | 60.87 (20.38) | 63.55 (23.57) | |
| 2. Take good care of health | 1 | 70.32 (26.29) | 64.91 (28.26) |
| 2 | 72.61 (27.31) | 68.67 (23.94) | |
| 3. Follow through on decision you make about your health | 1 | 62.93 (31.81) | 65.32 (29.34) |
| 2 | 64.06 (25.85) | 61.58 (26.05) | |
| 4. Put off doing things that would be good for your health | 1 | 35.70^ (25.79) | 37^ (32.82) |
| 2 | 43.77^ (27.81) | 46^ (27.67) | |
| 5. Eat breakfast | 1 | 53.19 (38.17) | 59.20 (40.85) |
| 2 | 51.29 (35.47) | 67.17 (37.65) | |
| 6. Eat the kinds of foods you think are necessary for your health | 1 | 54.51 (29.89) | 49.17 (32) |
| 2 | 57.58 (23.58) | 53.67 (30.47) | |
| 7. Eat a balanced breakfast | 1 | 43.80 (32.27) | 41.67 (36.80) |
| 2 | 51.29 (26.67) | 50.64 (35.49) | |
| 8. Do things to maintain or achieve good nutrition | 1 | 55.96 (27.36) | 49.38 (35.84) |
| 2 | 54.83 (26.47) | 60.02 (32.62) | |
| 9. Get the amount of activity necessary for health | 1 | 60.77 (30.71) | 57.91 (31.06) |
| 2 | 62.25 (24.96) | 86.17 (91.80) | |
| 10. Get the amount of reset necessary for health | 1 | 70.80 (27.96) | 63.08 (28.21) |
| 2 | 68.19 (26.25) | 71 (23.85) | |
| 11. Maintain or achieve a balance between rest and activity | 1 | 66.06 (31.33) | 49.61 (33.5) |
| 2 | 60.96 (29.92) | 65.55 (24.82) | |
| 12. Get the amount of time alone necessary for health | 1 | 56.12 (32.34) | 61.5 (31.22) |
| 2 | 56.74 (33.28) | 64.58 (32.08) | |
| 13. Get the amount of time with others that is necessary for health | 1 | 70.22 (28.45) | 60.94 (36.24) |
| 2 | 70.93 (29.97) | 60.67 (36.42) | |
| 14. Maintain or achieve a balance between time alone and time with others | 1 | 58.41 (26.81) | 61.64 (31.91) |
| 2 | 62.74 (30.60) | 71.14 (28.71) | |
| 15. Do things to keep you bladder and bowel habits normal | 1 | 67.03 (36.66) | 73.88 (32.87) |
| 2 | 70.32 (30.92) | 79.52 (28.88) | |
| 16. Do things to keep safe | 1 | 90.74 #(18.77) | 82.32# (27.23) |
| 2 | 86.29# (21.25) | 86.26# (22.35) | |
| 17. Do things to feel less stressed | 1 | 59.19 (33.74) | 56.14 (31.48) |
| 2 | 65.58 (28.62) | 72.26 (32.74) | |
| 18. Do things that help you “be all that you can be” | 1 | 79.83 (27.15) | 69.94 (32.70) |
| 2 | 78.87 (21.82) | 77.29 (24.75) |
1 refers to baseline data; 2 refers to follow-up data;
Highest DSCPI-90©
subscale; Lowest DSCPI-90© subscale;
Other than the decrease noted in the CLSS regularity subscale in post treatment scores, the lowest scored scale of both groups in pre and post measurements was the interests-hobbies scale. The highest subscale score for both groups for pre and post scores was the regularity-organization-routines scale (see table 4). As findings from the CLSS indicate, sample youth of both groups had scored low on the scale measuring social relationships and contact activities such as visiting and inviting friends.
Table 4.
CLSS
| Subscales | Time | Treatment | Control | Follow up | Treatment |
|---|---|---|---|---|---|
| Mean (S.D.) | Mean (S.D.) | p – value | p-value | ||
| Transportation | 1 | 3.09 (0.94) | 3.14 (0.82) | 0.339 | 0.906 |
| 2 | 3.29 (0.97) | 3.2 (0.97) | |||
| Support Services | 1 | 4.12 (0.99) | 3.76 (1.10) | 0.724 | 0.068 |
| 2 | 4.22 (1.05) | 3.79 (1.03) | |||
| Support Involvement | 1 | 3.80 (1.92) | 3.47(1.48) | 0.459 | 0.758 |
| 2 | 3.74 (1.75) | 3.79 (1.36) | |||
| Interests-Hobbies | 1 | 2.7^ (1.0) | 2.7^ (0.79) | 0.298 | 0.637 |
| 2 | 2.67^ (1.13) | 2.44^ (0.89) | |||
| Regularity-Organization-Routines | 1 | 6.29# (1.27) | 6.5# (1.13) | 0.002 | 0.689 |
| 2 | 5.87# (1.33) | 5.79#(1.47) | |||
| Summary Score | 1 | 19.51 (3.6) | 18.94 (3.47) | ||
| 2 | 19.12 (4.25) | 18.35 (3.42) |
1 refers to baseline data; 2 refers to follow-up data;
(p=0.011);
Lowest CLSS subscale scores;
Highest subscale CLSS scores.
Discussion
Despite the lack of significant findings, study findings are revealing when compared to other studies using these instruments. The PARS pre and post summary scores of TPT treatment and control groups were lower than reported in other studies of children and youth with and without chronic illnesses (23,34,35). As the T1 and T2 treatment and control groups DSCPI 90© mean scores indicate, this sample of youth with SB engaged in self care practices. The mean scores of adolescents in this study compared somewhat favorably to other groups of youth with and without chronic conditions studied (30–33). A number of studies have been conducted that have demonstrated that levels of community involvement and contact with peers are less compared to age mates (4,6,16). However, the findings of these analyses are limited as the hypotheses of the study were not supported. The factors which we posit as contributory to the negative findings of the study are discussed below.
There were several factors that may have been contributory to the lack of significant findings of this study. The strength of the intervention dose may have been insufficient to effect differences between groups. As this intervention was implemented, we recognized that the enrolled youth were less knowledgeable about their diagnostic condition and its self management than expected which we had not anticipated. As a result, we needed to reconfigure the goal-setting of the youths’ individualized transition plans to more basic precursor levels of knowledge and skill. Comparable findings of deficits in self management were reported in another study of youth with SB (36). Increasing the strength of the intervention dose with additional sessions to address learning needs and to reinforce learning may have been needed to demonstrate intervention effectiveness.
It was evident that these youths could not be classified as having achieved the stage of “transition readiness” needed for the transfer to adult health care services. The eligibility criteria used to screen potential study subjects were insufficient. It would have been helpful to enroll “transition ready” youth by excluding those who did not have the prerequisite knowledge and skills to engage fully in the TPT intervention. However, there is a dearth of empirically validated tools to assess transition readiness for any group of youth with SHCN. To address this concern, evidence-based criteria indicating transition readiness are needed to ensure subjects are appropriate for inclusion in future studies. Additionally, although youth were excluded who were diagnosed with a cognitive disability, this population often has subtle cognitive issues that may have affected their ability to participate.
An issue that we encountered in testing this intervention was the adolescents’ lack of adherence to the treatment protocol. Two major problems related to adherence were workshop attendance and transition plan follow-through as depicted in the flow chart (see figure 1).
Intense efforts were made to coordinate scheduling. Projected workshop attendance rarely matched the actual numbers attending, requiring the scheduling of additional workshops. Repeated reminder calls were made for data collection purposes and for scheduling workshop attendance. Follow-up dates for data collection were delayed due to problems with contacting subjects by phone or mail and unexpected family issues preventing scheduling of appointments. This level of effort called into question the intervention’s cost effectiveness and efficiency. Workshops to coincide with clinic visits or online training programs may be more viable training options to overcome the obstacles associated with real-time scheduled weekend training workshops.
Several reasons accounted for the youths’ lack of adherence with their transition plan follow-through. Forgetting to follow-through with their transition plan service referrals was a problem. Others were unclear as to what actions they needed to undertake based on their plan, following the first workshop. Many youth were uncomfortable to ask questions for clarification during the first workshop. For others, issues arose during the interim period that could not be resolved until the second workshop. Our intervention model did not include booster sessions to address these questions or issues.
Booster sessions involving one-on-one contact via email, text-messaging or telephonic contact involving the intervention team initiated either by the subject or team member may have been helpful in addressing these issues mentioned previously. Regularly scheduled booster sessions between the formal educational sessions would have the effect of reminding, encouraging and troubleshooting with the youth to increase adherence to their transition planning goals.
During the study it became evident that the time frame was insufficient to effect the change that youth identified in their transition plan. The goals identified by youth were based on long-range plans that would only be accomplished over a period of months, and even years. The one-month time frame of our intervention model was woefully insufficient to address these goals as the plan of action required would extend for months and years beyond the intervention such as obtaining a high school diploma or seeking employment.
The study sample was different from those reported in the literature as it consisted primarily of low SES bilingual Latino youth and their monolingual Spanish speaking parents (37,38). These demographic characteristics were associated with unique recruitment and retention issues. Lack of transportation, parental work schedules, the economic strain of inadequate housing and utilities (i.e. phones), and the demands of responding to family members’ needs with limited resources was evident in efforts to schedule data collection appointments and treatment group workshops. Families moved, phones were temporarily disconnected, scheduling conflicts due to family issues and parental employment created challenges.
We discovered the burden of responsibilities youth bore for learning the navigation skills needed to access services and supports. Parents, although willing, were unable to provide the instrumental support their children needed for the transition to the adult systems of care due to lack of knowledge of these systems, their inability to speak English, low literacy levels, and pressing family needs. Parents were unable to coach, reinforce, role model or provide information their children needed to access services. This inability to support their children was a source of frustration. This finding is similar as reported in other studies of youth without SHCN from low income neighborhoods (39,40). These studies demonstrated that adolescents and their parents had limited understanding of the youths’ health problems, the strategies for managing them and of navigating the health care system. Communication problems with providers existed in part as parents were reluctant to share information or they were unable to fully understand the providers’ health guidance. These problems were exacerbated with the non-English-speaking parents. A study of English-speaking parents of children with SB reported similar communication difficulties with providers resulting in inadequate understanding of their SB bowel management program (41).
Parental concerns about facilitating their children’s access to transition supports were apparent during the study. Several parents were disappointed when their children declined to assent or consent to participate in the study. A parent and adolescent withdrew from the study after learning they were randomly assigned to the control group, rather than the treatment group. Most parents commented favorably about their children’s participation in the treatment group feeling it was a valuable learning opportunity.
Future studies examining the association of demographic variables such as SES and cultural diversity with health care transition planning are warranted. Intervention studies that target both youth and their parents in contrast to youth only may suggest alternative empirically supported approaches.
A significant study design challenge was the development of an intervention model for testing. Testing of intervention models are in the seminal stages of development. Additional research is needed to develop and test intervention models in clinical trials that can be eventually applied to practice settings. Intervention outcomes may be better operationalized with the use of more focused and time-limited behaviors such as enrollment in a youth employment program rather than the long-term adulthood goal of employment.
The availability of empirically sound tools is limited. Some of the tools used in this study did not have the level of specificity and sensitivity needed. For example, the CLSS used binary responses that did not discriminate the type of usage, whether usage was self-initiated or the level of support needed. The PARS III may not have had the specificity needed to identify changes in youth of the study treatment or control arms. Translation of the PARS resulted in slightly different wording of the four-point interval and two different recall periods (one month and six months). Similar issues, not related to translation were reported in the validation study (23). Differences as measured by DSCP-I-90© found in the control rather than the treatment groups are difficult to explain. The lack of differences in the treatment group may be attributed to the awareness that youth developed about their SB knowledge and self management skill limitations discovered during their participation in the TPT workshops and not fully appreciated previously.
The research implications of this study reveal the limitations of this piloted model for application as a real-time intervention. Our experience leads us to conclude that the challenges identified with this intervention model reveal that it is not feasible clinically or economically. Nevertheless, given our experience with the TPT model, we believe a delivery model modification to an online electronic format, with booster sessions using a longitudinal design warrants testing. Studies are needed to explore the effectiveness of transition interventions examining medium to long term outcomes with varied samples of youth, particularly those from culturally and ethnically diverse populations. Future studies need to consider the selection of reliable and valid instruments to measure outcomes associated with a broad understanding of health encompassing the biopsychosocial context as well as quality of life.
Acknowledgments
Portions of the study were presented at the First World Conference on Spina Bifida Research and Care on March 16, 2009 in Orlando Florida. Support for this research investigation was funded by the National Institute on Nursing Research, National Institutes of Health (1R21 NR009415).
References
- 1.Liptak GS. Spina bifida. In: Accardo PJ, editor. Capute and Accardo’s neurodevelopmental disabilities in infancy and childhood. 3. Baltimore, MD: Paul H Brookes; 2008. pp. 189–205. [Google Scholar]
- 2.Bowman RM, McLone DG, Grant JA, Tomita T, Ito JA. Spina bifida outcome: a 25-year prospective. Pediatr Neurosurg. 2001;34(3):114–20. doi: 10.1159/000056005. [DOI] [PubMed] [Google Scholar]
- 3.Nehring WM, Faux SA. Transitional and health issues of adults with neural tube defects. J Nurs Scholarship. 2006;38(1):63–70. doi: 10.1111/j.1547-5069.2006.00079.x. [DOI] [PubMed] [Google Scholar]
- 4.Roebroeck ME, Jahnsen R, Carona C, Kent RM, Chamberlain MA. Adult outcomes and lifespan issues for people with childhood-onset physical disability. Dev Med Child Neurol. 2009;51(8):670–8. doi: 10.1111/j.1469-8749.2009.03322.x. [DOI] [PubMed] [Google Scholar]
- 5.Verhoef M, Barf HA, Post MW, van Asbeck FW, Gooskens RH, Prevo AJ. Secondary impairments in young adults with spina bifida. Dev Med Child Neurol. 2004;46(6):420–7. doi: 10.1017/s0012162204000684. [DOI] [PubMed] [Google Scholar]
- 6.Boudos RM, Mukherjee S. Barriers to community participation: teens and young adults with spina bifida. J Pediatr Rehabil Med. 2008;1(4):303–310. [PubMed] [Google Scholar]
- 7.Barf HA, Verhoef M, Jennekens-Schinkel A, Post MW, Gooskens RH, Prevo AJ. Cognitive status of young adults with spina bifida. Dev Med Child Neurol. 2003;45(12):813–20. doi: 10.1017/s0012162203001518. [DOI] [PubMed] [Google Scholar]
- 8.McDonnell GV, McCann JP. Link between the CSF shunt and achievement in adults with spina bifida. J Neurol Neurosurg Psychiatry. 2000;68(6):222–7. doi: 10.1136/jnnp.68.6.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simeonsson RJ, McMillen JS, Huntington GS. Secondary conditions in children with disabilities: spina bifida as a case example. Ment Retard Dev Disabil Res Rev. 2002;8(3):198–205. doi: 10.1002/mrdd.10038. [DOI] [PubMed] [Google Scholar]
- 10.Rekate HL. The pediatric neurosurgical patient: the challenge of growing up. Semin Pediatr Neurol. 2009;16(1):2–8. doi: 10.1016/j.spen.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 11.Buffart LM, van den Berg-Emons RJ, Burdorf A, Janssen WG, Stam HJ, Roebroeck ME. Cardiovascular disease risk factors and the relationships with physical activity, aerobic fitness, and body fat in adolescents and young adults with myelomeningocele. Arch of Phys Med Rehabil. 2008;89(11):2167–73. doi: 10.1016/j.apmr.2008.04.015. [DOI] [PubMed] [Google Scholar]
- 12.Davis BE, Shurtleff DB, Walker WO, Seidel KD, Duguay S. Acquisition of autonomy skills in adolescents with myelomeningocele. Dev Med Child Neurol. 2006;48(4):253–8. doi: 10.1017/S0012162206000569. [DOI] [PubMed] [Google Scholar]
- 13.Buran CF, McDaniel AM, Brei TJ. Needs assessment in a spina bifida program: a comparison of the perceptions by adolescents with spina bifida and their parents. Clin Nurse Spec. 2002;16(5):256–62. doi: 10.1097/00002800-200209000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Walker WO. Primary care providers and medical homes for individuals with spina bifida. J Pediatr Rehabil Med. 2008;1(4):337–344. [PubMed] [Google Scholar]
- 15.Betz CL. Transition of adolescents with special health care needs: review and analysis of the literature. Issues Compr Pediatr Nurs. 2004;27:179–240. doi: 10.1080/01460860490497903. [DOI] [PubMed] [Google Scholar]
- 16.Hunt GM, Oakeshott P, Kerry S. Link between the CSF shunt and achievement in adults with spina bifida. [see comment] J Neurol Neurosurg Psychiatry. 1999;67(5):591–5. doi: 10.1136/jnnp.67.5.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Friedman D, Holmbeck GN, DeLucia C, Jandasek B, Zebracki K. Trajectories of autonomy development across the adolescent transition in children with spina bifida. Rehabil Psychol. 2009;54(1):16–27. doi: 10.1037/a0014279. [DOI] [PubMed] [Google Scholar]
- 18.Antle BJ, Montgomery G, Stapleford C. The many layers of social support: capturing the voices of young people with spina bifida and their parents. Health Soc Work. 2009;34(2):97–106. doi: 10.1093/hsw/34.2.97. [DOI] [PubMed] [Google Scholar]
- 19.Kirpalani HM, Parkin PC, Willan AR, Fehlings DL, Rosenbaum PL, King D, Van Nie AJ. Quality of life in spina bifida: importance of parental hope. Arch Dis Child. 2000;83(4):293–7. doi: 10.1136/adc.83.4.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Buffart LM, van den Berg-Emons RJ, van Meeteren J, Stam HJ, Roebroeck ME. Lifestyle, participation, and health-related quality of life in adolescents and young adults with myelomeningocele. Dev Med Child Neurol. 2009;51(11):886–94. doi: 10.1111/j.1469-8749.2009.03293.x. [DOI] [PubMed] [Google Scholar]
- 21.Hurley AD, Bell S. Educational and vocational outcome of adults with spina bifida in relationship to neuropsychological testing. Eur J Pediatr Surg. 1994;1:17–8. doi: 10.1055/s-2008-1066146. [DOI] [PubMed] [Google Scholar]
- 22.Binks JA, Barden WS, Burke TA, Young NL. What do we really know about the transition to adult-centered health care? A focus on cerebral palsy and spina bifida. Arch Physical Med Rehabil. 2007;88(8):1064–73. doi: 10.1016/j.apmr.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 23.Walker DK, Stein RE, Perrin EC, Jessop DJ. Assessing psychosocial adjustment of children with chronic illnesses: a review of the technical properties of PARS III. J Dev Behav Pediatr. 1990;11(3):116–21. [PubMed] [Google Scholar]
- 24.Barnard K. Community life skills scale: resource manual for professionals using the community life skills scale. Seattle, WA: NCAST-AVENUW, Univ Washington, Center Human Dev Disabil; 1991. [Google Scholar]
- 25.Denyes MJ. Self-are practice intstrument. Detroit, MI: Coll Nurs Waye State Univ; 1990. [Google Scholar]
- 26.Denyes MJ. Orem’s model used for health promotion: directions from research. Adv Nurs Sci. 1988;11(1):13–21. doi: 10.1097/00012272-198810000-00003. [DOI] [PubMed] [Google Scholar]
- 27.Denyes MJ, Orem DE, Bekel G. Self-care: a foundational science. Nurs Sci Q. 2001;14(1):48–54. doi: 10.1177/089431840101400113. [DOI] [PubMed] [Google Scholar]
- 28.Baker LK. Predictors of self-care in adolescents with cystic fibrosis: a test and explication of Orem’s theories of self-care and self-care deficit. Detroit, MI: Wayne State Univ; 1991. [DOI] [PubMed] [Google Scholar]
- 29.Frey MA, Denyes MJ. Health and illness self-care in adolescents with IDDM: a test of Orem’s theory. Adv Nurs Sci. 1989;12(1):67–75. doi: 10.1097/00012272-198910000-00009. [DOI] [PubMed] [Google Scholar]
- 30.McCaleb A, Cull VV. Sociocultural influences and self-care practices of middle adolescents. J Pediatr Nurs. 2000;15(1):30–5. [PubMed] [Google Scholar]
- 31.McCaleb A, Edgil A. Self-concept and self-care practices of healthy adolescents. J Pediatr Nurs. 1994;9(4):233–8. [PubMed] [Google Scholar]
- 32.Slusher IL. Self-care agency and self-care practice of adolescents. Issues Compr Pediatr Nurs. 1999;22(1):49–58. doi: 10.1080/014608699265383. [DOI] [PubMed] [Google Scholar]
- 33.Dashiff CJ, McCaleb A, Cull V. Self-care of young adolescents with type 1 diabetes. J Pediatr Nurs. 2006;21(3):222–32. doi: 10.1016/j.pedn.2005.07.013. [DOI] [PubMed] [Google Scholar]
- 34.Hendriksen JG, Poysky JT, Schrans DG, Schouten EG, Aldenkamp AP, Vles JS. Psychosocial adjustment in males with Duchenne muscular dystrophy: psychometric properties and clinical utility of a parent-report questionnaire. J Pediatr Psychol. 2009;34(1):69–78. doi: 10.1093/jpepsy/jsn067. [DOI] [PubMed] [Google Scholar]
- 35.Chernoff RG, Ireys HT, DeVet KA, Kim YJ. A randomized, controlled trial of a community-based support program for families of children with chronic illness: pediatric outcomes. Arch Pediatr Adolesc Med. 2002;156(6):533–9. doi: 10.1001/archpedi.156.6.533. [DOI] [PubMed] [Google Scholar]
- 36.Buran CF, Sawin KJ, Brei TJ, Fastenau PS. Adolescents with myelomeningocele: activities, beliefs, expectations, and perceptions. Dev Med Child Neurol. 2004;46(4):244–52. doi: 10.1017/s0012162204000404. [DOI] [PubMed] [Google Scholar]
- 37.Buffart LM, Westendorp T, van den Berg-Emons RJ, Stam HJ, Roebroeck ME. Perceived barriers to and facilitators of physical activity in young adults with childhood-onset physical disabilities. J Rehabil Med. 2009;41(11):881–5. doi: 10.2340/16501977-0420. [DOI] [PubMed] [Google Scholar]
- 38.van Mechelen MC, Verhoef M, van Asbeck FW, Post MW. Work participation among young adults with spina bifida in the Netherlands. Dev Med Child Neurol. 2008;50(10):772–7. doi: 10.1111/j.1469-8749.2008.03020.x. [DOI] [PubMed] [Google Scholar]
- 39.Atkins R, Bluebond-Langner M, Read N, Pittsley J, Hart D. Adolescents as health agents and consumers: results of a pilot study of the health and health-related behaviors of adolescents living in a high-poverty urban neighborhood. J Pediatr Nurs. 2009 doi: 10.1016/j.pedn.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 40.Lareau A. Unequal childhoods: class, race, and family life. Berkeley, CA: Univ Calif Press; 2003. [Google Scholar]
- 41.Sawin KJ, Thompson NM. The experience of finding an effective bowel management program for children with spina bifida: the parent’s perspective. J Pediatr Nurs. 2009;24(4):280–91. doi: 10.1016/j.pedn.2008.03.008. [DOI] [PubMed] [Google Scholar]