Abstract
Given the effectiveness of putative escape extinction as treatment for feeding problems, it is surprising that little is known about the effects of escape as reinforcement for appropriate eating during treatment. In the current investigation, we examined the effectiveness of escape as reinforcement for mouth clean (a product measure of swallowing), escape as reinforcement for mouth clean plus escape extinction (EE), and EE alone as treatment for the food refusal of 5 children. Results were similar to those of previous studies, in that reinforcement alone did not result in increases in mouth clean or decreases in inappropriate behavior (e.g., Piazza, Patel, Gulotta, Sevin, & Layer, 2003). Increases in mouth clean and decreases in inappropriate behavior occurred when the therapist implemented EE independent of the presence or absence of reinforcement. Results are discussed in terms of the role of negative reinforcement in the etiology and treatment of feeding problems.
Keywords: escape, escape extinction, feeding disorders, food refusal, food selectivity, gastroesophageal reflux disease, negative reinforcement, pediatric feeding disorders, transplant
Results of both basic and applied studies have shown that negative reinforcement plays a central role in the maintenance of human behavior (Iwata, 1987). In a typical negative reinforcement paradigm, a response produces the removal, reduction, postponement, or prevention of aversive stimulation, resulting in an increase in the probability of the response (Hineline, 1977). Many examples of human behavior that is maintained by negative reinforcement exist (Iwata, 1987). Feeding problems in children represent one example.
Many children with feeding disorders have medical problems (e.g., gastroesophageal reflux disease, GERD) that cause eating to be painful (Di Lorenzo et al., 2005; Garb & Stunkard, 1974). Thus, mealtime may be associated with pain, which may increase the probability that the child will exhibit refusal behavior (e.g., crying, batting at the spoon). Parents sometimes respond to refusal by removing, postponing, or terminating bite presentations (Borrero, Woods, Borrero, Masler, & Lesser, 2010; Piazza, Fisher, et al., 2003). The child then learns that refusal behavior produces escape from eating.
To illustrate, Borrero et al. (2010) conducted descriptive assessments with 25 children with feeding problems and their caregivers. Following the descriptive assessments, the authors calculated conditional probabilities for caregiver responses to inappropriate child behavior. The results of the conditional probability analysis showed that refusal frequently was followed by meal termination and escape from spoon or cup presentations. Piazza, Fisher, et al. (2003) conducted functional analyses to examine the role of negative reinforcement in the maintenance of feeding problems. Of the 10 children whose functional analyses were differentiated, 90% displayed inappropriate behavior that was maintained by escape from bite or drink presentations.
Given the importance of negative reinforcement in the maintenance of feeding problems, it is surprising that its effects following appropriate eating have not been evaluated. By contrast, investigators have used negative reinforcement for appropriate behavior in the treatment of other behavior problems (Lalli et al., 1999; Roberts, Mace, & Daggett, 1995; Steege et al., 1990; Vollmer, Marcus, & Ringdahl, 1995). For example, Lalli et al. (1999) compared the effects of positive (edible items) and negative (escape) reinforcement for compliance in the absence of escape extinction (EE) for individuals whose destructive behavior was maintained by escape from instructions. Positive reinforcement was more effective in increasing compliance and reducing destructive behavior than was negative reinforcement.
Nonetheless, it is not clear if the results of Lalli et al. (1999) are applicable to feeding problems for several reasons. First, Lalli et al. used edible items as reinforcement, and these items may not consistently function as reinforcement for children who refuse to eat. In addition, children with feeding problems may respond differently to positive and negative reinforcement-based treatment than children with destructive behavior. For example, Piazza, Patel, Gulotta, Sevin, and Layer (2003), in contrast with Lalli et al., showed that positive reinforcement in the absence of EE did not produce increases in acceptance for four children with feeding problems. Although positive reinforcement alone was not effective, positive reinforcement in combination with EE did produce beneficial effects (i.e., reduced inappropriate behavior or negative vocalizations) for some children. Therefore, it may be productive to conduct similar analyses of negative reinforcement for appropriate eating alone and in combination with EE.
The purpose of the current investigation was to extend the literature on the role of negative reinforcement in the treatment of food refusal. First, we conducted functional analyses to demonstrate that inappropriate behavior was maintained, at least in part, by negative reinforcement in the form of escape from bite or drink presentations (Bachmeyer et al., 2009). Next, we evaluated the effects of concurrent escape contingencies (30-s break) following both mouth clean (a product measure of swallowing) and inappropriate behavior relative to when escape was available for inappropriate behavior only. We then examined the effects of escape for mouth clean in conjunction with EE (nonremoval of the spoon) and compared it to EE alone.
METHOD
Participants, Setting, and Materials
The participants were five children who had been admitted to an intensive outpatient pediatric feeding disorders program. They were included in this study because their primary presenting problem was solid or liquid refusal or selectivity, and the children's parents indicated that using escape as reinforcement for appropriate eating or drinking and EE would be acceptable. In addition, the results of a functional analysis indicated that inappropriate behavior was maintained, at least in part, by escape from bite or drink presentations.
Lauren was a 2-year-old girl whose medical history included a small bowel transplant. She had been admitted for solid and liquid refusal, gastrostomy (G-) tube dependence, and parenteral nutrition dependence. She consumed no solids or liquids by mouth. George was a 5-year-old boy whose medical history included a kidney transplant. He had been admitted for solid and liquid refusal and G-tube dependence. He consumed no solids or liquids by mouth. Carl was an 18-month-old boy whose medical history included insufficient oral intake and GERD. He had been admitted for food selectivity by type and texture, packing, and vomiting. He consumed approximately 90% of his nutritional needs by mouth, consisting of bottle-fed Elecare formula and Stage 2 jarred baby food (chicken and gravy only). Charles was a 5-year-old boy whose medical history included G-tube dependence. He had been admitted for insufficient oral intake and texture selectivity. Charles consumed approximately 65% of his nutritional needs by mouth, consisting of Stage 2 jarred baby foods and liquids from a bottle. Frank was a 21-month-old boy whose medical history included GERD and dysphagia. He had been admitted for insufficient oral intake and nasogastric-tube dependence. Frank consumed approximately 38% of his nutritional needs by mouth, consisting of Stages 1 and 2 jarred baby food and milk with Carnation Instant Breakfast (CIB). Prior to admission, each child participated in a medical evaluation to rule out or treat any possible medical causes of the feeding problem and to evaluate the child's safety and appropriateness for oral feeding. All children were cleared by their physician for the program.
Therapists conducted sessions in rooms (4 m by 4 m) with one-way observation and sound. The room was equipped with age-appropriate seating (i.e., high chair with a removable tray or a table), food or drink, eating or drinking utensils, and a bib that folded at the bottom to form a receptacle.
Data Collection and Interobserver Agreement
Observers recorded acceptance, mouth clean, and inappropriate behavior on laptop computers using an event-recording procedure. Observers scored the occurrence of acceptance and mouth clean. During solid sessions, observers scored acceptance if the child leaned toward the spoon, opened his or her mouth, and allowed the entire bolus of food (except for an amount smaller than the size of a pea) to enter the mouth within 5 s of the presentation in the absence of negative vocalizations and inappropriate behavior. During liquid sessions, observers scored acceptance if the child leaned toward the cup, opened his or her mouth, and allowed any portion of the liquid to enter the mouth within 5 s of the presentation in the absence of negative vocalizations and inappropriate behavior. A presentation occurred when the therapist placed the spoon or cup touching the child's lips, not including when the therapist placed the spoon or cup at the lips following re-presentation. We used different definitions for solids and liquids because it took longer for the therapist to deposit the bolus of liquids into the child's mouth than it did for the therapist to deposit the bolus of solids. The first time the bite or drink entered the child's mouth, the observer activated a timer for 30 s to signal the feeder to check the child's mouth (see Procedure for more detail). The observers scored mouth clean at the 30-s check if (a) the entire bolus had entered the child's mouth (except for an amount smaller than the size of a pea) and (b) no food or liquid larger than the size of a pea was in the child's mouth, which did not include the absence of food or liquid as a result of expulsion (spitting out the food). The observers scored a pack at the 30-s check if (a) the entire bolus had entered the child's mouth (except for an amount smaller than the size of a pea) and (b) food or liquid larger than the size of a pea remained in the child's mouth. If no bites or drinks entered the child's mouth during a session, the child did not have the opportunity to have a mouth clean. If the child expelled the bite or drink during the 30-s interval and did not have any solids or liquids larger than the size of a pea in his or her mouth at the 30-s check, the observer did not score either a mouth clean or a pack. Observers scored expel each time the child spit out food larger than the size of a pea. Observers scored the frequency of inappropriate behavior each time the child turned his or her head 45° degrees or more away from the spoon or cup; hit the spoon, cup, or feeder's arm or hand; or covered his or her mouth while the spoon or cup was at (i.e., within 4 cm of) the child's lips.
Data for acceptance and mouth clean were converted to a percentage after dividing the number of occurrences of acceptance or mouth clean by the number of bite or drink presentations (denominator for acceptance) or the number of bites or drinks that entered the child's mouth (denominator for mouth clean). Data on inappropriate behavior were converted to responses per minute by dividing the number of inappropriate behaviors by the duration of time the spoon or cup was at the child's lips.
Interobserver agreement for acceptance and mouth clean was calculated by partitioning the session into 10-s intervals; summing occurrence (a 10-s interval in which both observers scored the behavior) and nonoccurrence (a 10-s interval in which both observers did not score the behavior) agreements; dividing by the sum of occurrence agreements, nonoccurrence agreements, and disagreements (a 10-s interval in which one observer scored the occurrence of and the other observer did not score an occurrence of the behavior); and converting the ratio to a percentage. Exact agreements coefficients for inappropriate behavior were calculated by dividing the number of agreements (a 10-s interval in which both observers scored the same frequency of inappropriate behavior) by the number of agreements plus disagreements (a 10-s interval in which the observers scored a different frequency of inappropriate behavior) and converting the ratio to a percentage.
During the functional analysis, a second observer simultaneously but independently scored 30%, 31%, 32%, 59%, 39%, and 75% of sessions for Lauren, George, Carl, Charles (solids), Charles (liquids), and Frank, respectively. Mean agreement was 100% for acceptance, 100% for mouth clean, and 83% (range, 70% to 100%) for inappropriate behavior for Lauren; 100% for acceptance, 100% for mouth clean, and 85% (range, 68% to 100%) for inappropriate behavior for George; 100% for acceptance, 100% for mouth clean, and 85% (range, 69% to 100%) for inappropriate behavior for Carl; 100% for acceptance, 100% for mouth clean, and 94% (range, 83% to 100%) for inappropriate behavior for Charles (solids); 100% for acceptance, 100% for mouth clean, and 94% (range, 75% to 100%) for inappropriate behavior for Charles (liquids); and 100% for acceptance, 100% for mouth clean, and 86% (range, 73% to 100%) for inappropriate behavior for Frank.
A second observer simultaneously but independently scored 33%, 49%, 36%, 32%, 33%, and 47% of sessions for Lauren, George, Carl, Charles (solids), Charles (liquids), and Frank, respectively, during the treatment analysis. Mean agreement was 97% (range, 89% to 100%) for acceptance, 95% (range, 65% to 100%) for mouth clean, and 97% (range, 93% to 100%) for inappropriate behavior for Lauren; 98% (range, 85% to 100%) for acceptance, 99% (range, 89% to 100%) for mouth clean, and 99% (range, 79% to 100%) for inappropriate behavior for George; 97% (range, 88% to 100%) for acceptance, 98% (range, 86% to 100%) for mouth clean, and 96% (range, 86% to 100%) for inappropriate behavior for Carl; 99% (range, 95% to 100%) for acceptance, 99% (range, 92% to 100%) for mouth clean, and 99% (range, 93% to 100%) for inappropriate behavior for Charles (solids); 96% (range, 76% to 100%) for acceptance, 99% (range, 84% to 100%) for mouth clean, and 97% (range, 86% to 100%) for inappropriate behavior for Charles (liquids); 97% (range, 47% to 100%) for acceptance, 97% (range, 60% to 100%) for mouth clean, and 98% (range, 85% to 100%) for inappropriate behavior for Frank.
Design
We used a pairwise design (Iwata, Duncan, Zarcone, Lerman, & Shore, 1994) in the functional analysis to compare levels of inappropriate behavior in the test and control conditions for all participants except Charles (liquids and solids). We used a reversal design with Charles for liquids and solids. We used a combination of multielement and ABAB designs to compare levels of acceptance, mouth clean, and inappropriate behavior in the treatment analysis. During baseline (A), we alternated between escape for inappropriate behavior and escape for inappropriate behavior and mouth clean. During the B phase, we alternated between EE and EE plus escape for mouth clean.
General Procedure
For the current analysis, a trained therapist conducted approximately three meals per day with at least 1 hr between the start of each meal (e.g., 9:00 a.m., 12:00 p.m., 4:00 p.m.). Each meal consisted of multiple five-bite or five-drink sessions with brief breaks (e.g., 1 to 2 min) between sessions. The focus of treatment was solids for Lauren, George, and Carl; solids and liquids for Charles; and liquids for Frank. The caregivers of Lauren, George, Carl, and Charles selected approximately 8 to 16 foods for the therapist to present during meals. The therapist randomly selected three (Lauren) or four (George, Carl, and Charles) of the caregiver-identified foods to present in each meal, with the caveat that the therapist presented all of the foods in each phase of the assessment to control for any possible differences in behavior due to food type. The therapist presented only proteins and vegetables to Lauren and George based on the physician's recommendation. The therapist presented Carl and Charles with one food from each of the food groups of fruit, protein, starch, and vegetable. Foods were a pureed texture for all children. The therapist selected the order of food presentation randomly prior to the session. The therapist presented each bite on a small Maroon spoon containing 10.92 cc (Lauren) or 0.85 cc (all other children) of food. The therapist presented 2 cc (Charles) or 4 cc (Frank) of CIB mixed with whole milk (based on the recommendation of the program dietitian) in a pink cut-out cup. The program speech therapist prescribed the texture, utensils, and bolus sizes.
The therapist presented the spoon or cup touching the midline of the child's lips accompanied by a verbal prompt to “take a bite [drink]” approximately every 30 s. The therapist delivered brief verbal praise following acceptance. The therapist said “show me” 30 s after the bite or drink entered the child's mouth to determine if the child had swallowed. If the child did not open his or her mouth following the verbal prompt, the therapist used a small rubber-coated baby spoon to prompt the child to open his or her mouth. The prompt consisted of the therapist inserting the spoon into the child's mouth and turning it 90°, accompanied by a second verbal “show me” prompt. The therapist delivered brief praise for mouth clean following the first 30-s mouth check and presented the next bite or drink. The therapist did not provide any differential consequence if the child cried, gagged, coughed, or vomited.
The therapist delivered a verbal prompt to “swallow your bite [drink]” if any food or drink larger than the size of a pea remained in the child's mouth at the 30-s check (referred to as a pack). The therapist then presented the next bite or drink. If the therapist had presented all five bites or drinks, and the child was packing after the 30-s check, the therapist repeated the verbal prompt to “swallow your bite [drink]” every 30 s until no food or drink larger than the size of a pea was in the child's mouth. The therapist would have terminated the meal at 30 min if the child had not swallowed all five bites, but this was never necessary in any condition for any child.
Functional analysis
We conducted a functional analysis (Bachmeyer et al., 2009) with each participant to assess the extent to which escape functioned as reinforcement for inappropriate behavior. During the functional analysis, the therapist followed the general procedures described above in addition to the specific procedures for each condition described below. In all conditions, the therapist held the spoon or cup stationary (i.e., once the therapist positioned the spoon or cup, it did not move) for 30 s if the child did not accept the bite or drink and did not engage in inappropriate behavior. The therapist did not re-present expelled bites or drinks. During the control condition, the therapist provided no differential consequence for inappropriate behavior and interacted with the child (e.g., sang) in the presence of toys identified via a stimulus preference assessment throughout the session. During the escape condition, the therapist removed the spoon or cup for 30 s if the child engaged in inappropriate behavior and presented the next bite or drink after the 30-s escape interval. The therapist did not provide any other differential consequence following the child's inappropriate behavior (e.g., the therapist did not reprimand the child). Toys were not available. During the attention condition, the therapist provided 30 s of attention (e.g., “you like peas”) following inappropriate behavior while the spoon or cup remained stationary for 30 s. The therapist presented the next bite after the 30-s attention interval. Toys were not available. During the tangible condition (Frank only), the therapist provided 30 s of a tangible item (one of three highly preferred toys identified via stimulus preference assessment) after inappropriate behavior. The therapist presented the next bite after the 30-s interval. We conducted a tangible condition for Frank because we observed that his parents gave him toys when he engaged in inappropriate behavior during meals.
Treatment Evaluation of Negative Reinforcement
The therapist followed the general procedures described above in addition to the specific procedures for the conditions described below.
Escape for inappropriate behavior
The procedures were identical to the escape condition of the functional analysis.
Escape for inappropriate behavior and mouth clean
The procedures were identical to the escape for inappropriate behavior condition except that mouth clean resulted in a 30-s break from bite or drink presentations. That is, the therapist waited for 30 s after a mouth clean to present the next bite or drink. The therapist did not deliver additional reinforcers following mouth clean. We chose 30 s as the reinforcement interval for mouth clean because the results of the functional analysis showed that a 30-s escape interval functioned as reinforcement for inappropriate behavior. The goal of the study was to evaluate whether that same interval would function as reinforcement for mouth clean.
Escape extinction
The therapist held the spoon or cup at the child's lips and deposited the bite or drink any time the child's mouth was open if the child did not accept the bite or drink within 5 s of presentation. The therapist re-presented (i.e., scooped up the bite or drink with the spoon or cup and placed the bite or drink back into the child's mouth) expelled bites or drinks and provided no differential consequences for inappropriate behavior. Re-presentation did not reset the 30-s mouth check clock. That is, the therapist checked for a mouth clean 30 s after the bite or drink entered the child's mouth the first time and every 30 s thereafter if the child had not swallowed the bite or drink, independent of whether the child expelled the bite or drink within the 30-s interval. The session ended when the child had swallowed all five bites or drinks.
Escape extinction plus escape for mouth clean
The procedure was similar to EE with the addition that mouth clean resulted in a 30-s break (as described above).
RESULTS
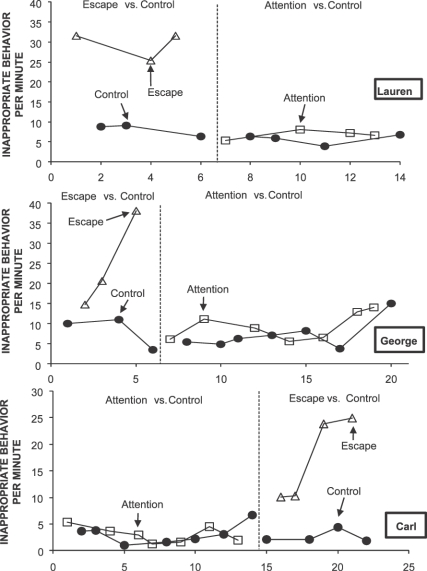
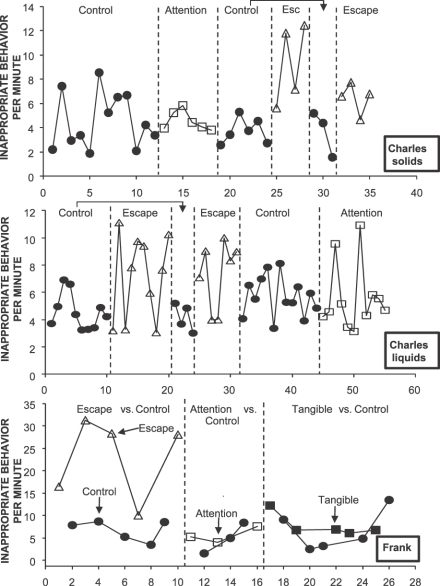
Results of the functional analyses are depicted in the top, middle, and bottom panels of Figure 1 for Lauren, George, and Carl and in Figure 2 (solids for Charles, top; liquid for Charles, middle; Frank, bottom). For all participants, rates of inappropriate behavior were higher in the escape condition than in the control condition. Rates of inappropriate behavior were lower in the attention, tangible (Frank), and control conditions. Acceptance and mouth clean (data not shown) remained at zero for all participants. These results suggested that inappropriate behavior was maintained, at least in part, by negative reinforcement in the form of escape.
Figure 1.
Inappropriate behavior per minute during escape and control conditions of the functional analysis for Lauren (top), George (middle), and Carl (bottom).
Figure 2.
Inappropriate behavior per minute during escape and control conditions of the functional analysis for Charles (liquids, top), Charles (solids, middle), and Frank (bottom).
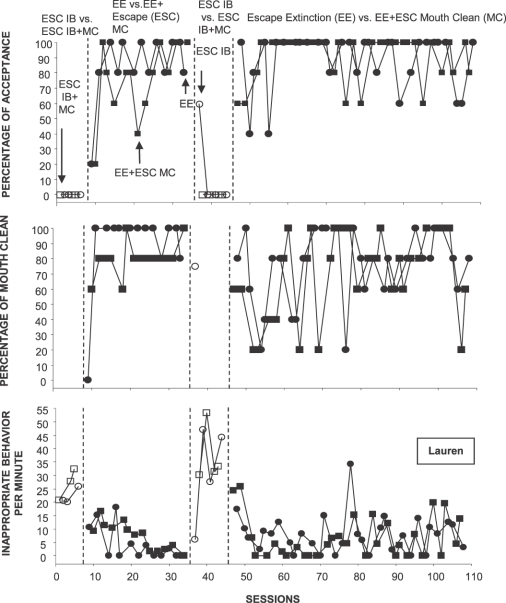
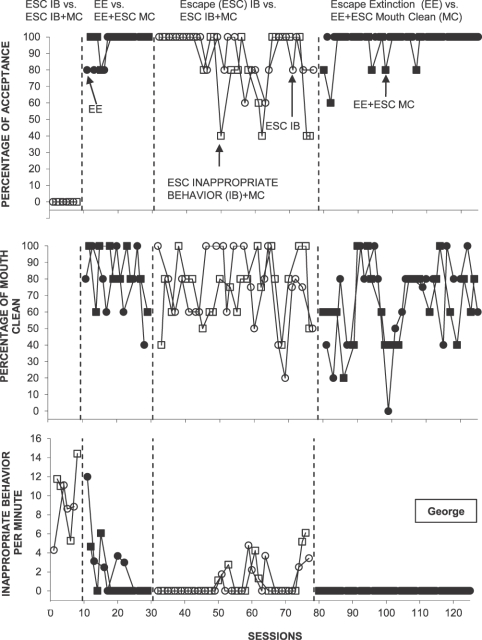
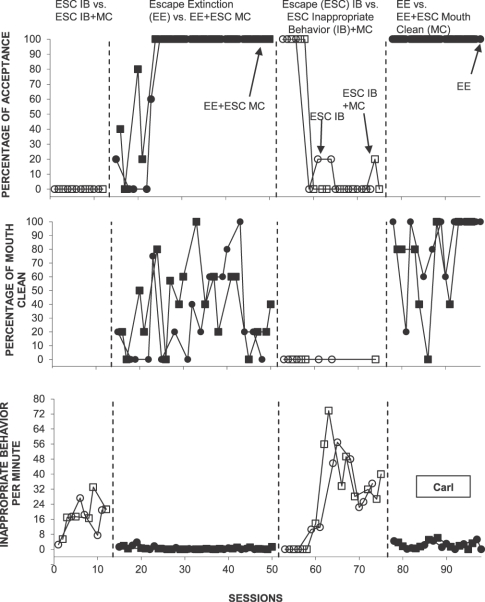
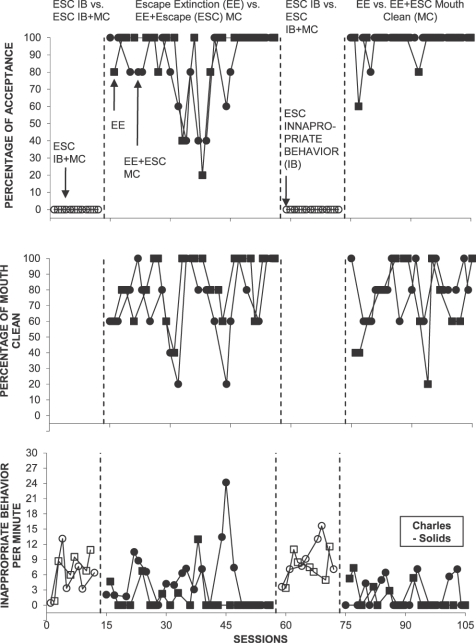
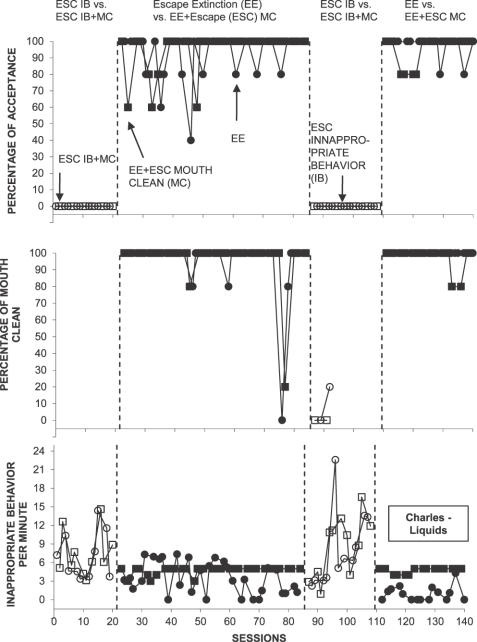
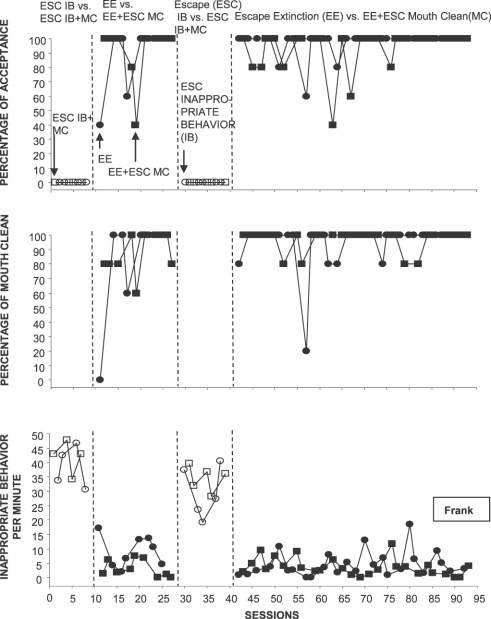
Percentage of acceptance, percentage of mouth clean, and rate of inappropriate behavior from the treatment evaluation are depicted in Figures 3 (Lauren), 4 (George), 5 (Carl), 6 (Charles, solids), 7 (Charles, liquids), and 8 (Frank). The general pattern of responding was similar for all participants. Acceptance remained low and inappropriate behavior remained high in both escape for inappropriate behavior and escape for inappropriate behavior and mouth clean conditions. There were no acceptance and no opportunities for mouth clean (therefore, no data appear on the panels for mouth clean) in the initial baseline. Acceptance and mouth clean increased and inappropriate behavior decreased during both EE and EE plus escape for mouth clean. Removal of EE resulted in decreases in acceptance and increases in inappropriate behavior for all participants; few or no opportunities for mouth clean for Lauren, Carl, Charles (liquids), Charles (solids), and Frank; and no change in mouth clean for George. Reimplementation of EE and EE plus escape for mouth clean produced increases in acceptance and mouth clean (except for George) and decreases in inappropriate behavior. For George, reimplementation of EE and EE plus escape for mouth clean produced increases in acceptance and decreases in inappropriate behavior and more variability in mouth clean initially.
Figure 3.
Percentage of acceptance (top), percentage of mouth clean (middle), and inappropriate behavior per minute (bottom) from the treatment analysis for Lauren.
Figure 4.
Percentage of acceptance (top), percentage of mouth clean (middle), and inappropriate behavior per minute (bottom) from the treatment analysis for George.
Figure 5.
Percentage of acceptance (top), percentage of mouth clean (middle), and inappropriate behavior per minute (bottom) from the treatment analysis for Carl.
Figure 6.
Percentage of acceptance (top), percentage of mouth clean (middle), and inappropriate behavior per minute (bottom) from the treatment analysis for Charles (solids).
Figure 7.
Percentage of acceptance (top), percentage of mouth clean (middle), and inappropriate behavior per minute (bottom) from the treatment analysis for Charles (liquids).
Figure 8.
Percentage of acceptance (top), percentage of mouth clean (middle), and inappropriate behavior per minute (bottom) from the treatment analysis for Frank.
DISCUSSION
The results of studies on functional analysis of feeding disorders suggest that negative reinforcement in the form of escape from eating plays a major role in the maintenance of inappropriate mealtime behavior (Girolami & Scotti, 2001; Najdowski et al., 2008; Piazza, Fisher, et al., 2003). Similarly, the results of the functional analyses of the five children in the current investigation showed that their inappropriate behavior was maintained, at least in part, by negative reinforcement in the form of escape from bite or drink presentations.
Although the results of the functional analyses showed that escape functioned as reinforcement for inappropriate behavior, escape did not appear to be a reinforcer for mouth clean when escape was available concurrently for inappropriate behavior (except, perhaps, for George). There may be a number of reasons why. First, none of the children accepted bites or drinks in the initial baseline; therefore, none of the children had an opportunity to experience the reinforcement contingency for mouth clean. However, after we implemented EE, all of the children contacted reinforcement for mouth clean, and Lauren, George, Carl, and Charles (liquids) contacted the contingency again in the reversal. Nevertheless, high levels of mouth clean were not sustained in the reversal to baseline for any of the children except George. It is possible that escape as reinforcement sustained mouth clean for George during the reversal. For the other children, it is possible that longer escape intervals for mouth clean relative to the length of escape for inappropriate behavior would have been effective in biasing responding toward mouth clean. Future studies should manipulate the length of the escape interval for both inappropriate and appropriate behavior to determine how reinforcement duration affects responding. Future research also could manipulate other parameters of reinforcement (e.g., quality, rate) to identify the manipulations that would bias responding in favor of appropriate behavior (Athens & Vollmer, 2010).
In the current investigation, we implemented the reinforcement contingency for mouth clean rather than for acceptance, because Patel, Piazza, Martinez, Volkert, and Santana (2002) showed that levels of acceptance and mouth clean were equivalent, independent of whether acceptance or mouth clean produced positive reinforcement. However, future studies should evaluate whether escape following acceptance is more effective than escape following mouth clean.
Piazza et al. (1997) suggested that responding might be biased toward inappropriate behavior when escape is available for both appropriate and inappropriate behavior. In the current investigation, the child could avoid eating altogether if he or she engaged in inappropriate behavior in baseline. By contrast, the child could access breaks from spoon or cup presentations only following mouth clean if the child consumed the bite or drink. Therefore, inappropriate behavior may have required less effort than mouth clean. Responding also may have favored inappropriate behavior due to the child's history of reinforcement. Borrero et al. (2010) showed that the conditional probability of a parent terminating the meal or removing the spoon or cup following inappropriate behavior was higher than the probability of those same events following acceptance. Results of Borrero et al. suggest that children with feeding disorders may have a long history of meal termination and spoon or cup removal following inappropriate behavior and that inappropriate behavior is more effective than consumption for producing meal termination or escape.
Although escape for mouth clean alone was not effective, acceptance and mouth clean increased and inappropriate behavior decreased when the therapist implemented EE. These results replicate those of a number of studies that have demonstrated the possible necessity of EE in the treatment of feeding problems (Ahearn, Kerwin, Eicher, Shantz, & Swearingin, 1996; Cooper et al., 1995; Hoch, Babbitt, Coe, Krell, & Hackbert, 1994; Patel et al., 2002; Piazza, Patel, et al., 2003; Reed et al., 2004). But why does EE appear to be so important for treating severe feeding problems?
Escape from eating is hypothesized to become a reinforcer for food refusal when medical conditions cause eating to be painful (Piazza, Fisher, et al., 2003). For example, children with GERD may associate eating with the pain that occurs when excess acid is released into the stomach or esophagus. Basic studies with both animals and humans have shown that pairing eating with an aversive event may result in learned or conditioned taste aversions (e.g., Garb & Stunkard, 1974). For example, Garcia, Kimeldorf, and Koelling (1955) exposed rats to a noxious stimulus (e.g., emetic agent) paired with a flavor and showed that the rats avoided the flavor even after removal of the noxious stimulus. These aversions may develop after only one or a few trials and after significant delays between eating and the aversive event (e.g., vomiting; Garcia, Hankins, & Rusiniak, 1974; Lindberg, Alvin, Chezik, & Ray, 1982; Riley & Clarke, 1977). These taste aversions in animals may be similar to the food refusal seen in children with severe feeding problems.
Like any avoidance behavior, once taste aversions develop, they have been notoriously difficult to extinguish in experiments with nonhuman species because the avoidance response prevents the organism from contacting the change from negative reinforcement to extinction (e.g., Bernstein, 1991; Garcia, Ervin, & Koelling, 1966; Garcia et al., 1955, 1974). The parallel in feeding disorders displayed by young children is that even if the child's medical problems are treated and eating no longer produces pain, the child never learns that eating is no longer painful if he or she continues to refuse to eat. That is, if the child never contacts food, he or she never has the opportunity to learn that eating is no longer painful. In fact, animal studies have shown that under some circumstances, extinction of the taste aversion occurs only when the animal has direct contact with the aversive taste (e.g., the taste is infused into the oral cavity; Spector, Smith, & Hollander, 1981, 1983). The results of the current investigation and others on EE (Ahearn et al., 1996; Cooper et al., 1995; Hoch et al., 1994; Piazza, Patel, et al., 2003) are similar in that, in some cases, consumption increases only when the child has direct contact with the food or drink through EE, which is why EE might be critical as treatment when the feeding problem is severe.
Although EE was effective, the presence of escape as reinforcement for mouth clean in conjunction with EE did not appear to contribute to the treatment effects. These results are different from those of Piazza, Patel, et al. (2003) and Reed et al. (2004), who showed that the presence of positive reinforcement in combination with EE was associated with some beneficial effects (i.e., reduced inappropriate behavior or negative vocalizations). It is not clear why escape as reinforcement for mouth clean in combination with EE did not contribute to treatment effects.
One question that remains unanswered is why some children develop feeding problems (Rommel, DeMeyer, Feenstra, & Veereman-Wauters, 2003) and others do not. For example, the majority of newborns exhibit spitting or vomiting (Belknap & McEvoy, 1994); nevertheless, most of these children do not develop feeding disorders. In addition, not all children diagnosed with a feeding disorder have diagnosed medical problems (Rommel et al.). It may be that children who develop feeding disorders have particular sensitivity to escape as reinforcement or have differential exposure to escape during eating (Borrero et al., 2010). In addition, other variables (e.g., attention, access to preferred foods or activities) also may function as reinforcement for food refusal (Bachmeyer et al., 2009; Piazza, Fisher, et al., 2003). Future research should examine the risk factors for the development of feeding problems. Children identified to be at risk could be followed over time to examine their reinforcement histories to determine if differential sensitivity or exposure to escape influences the development of feeding problems. Future research also should examine how biological (e.g., GERD) and behavioral variables interact in both the etiology and treatment of feeding problems.
Acknowledgments
This investigation was supported in part by Grant 1 K24 HD01380-01 from the Department of Health and Human Services, the National Institute of Child Health and Human Development.
REFERENCES
- Ahearn W.H, Kerwin M.L, Eicher P.S, Shantz J, Swearingin W. An alternating treatments comparison of two intensive interventions for food refusal. Journal of Applied Behavior Analysis. 1996;29:321–332. doi: 10.1901/jaba.1996.29-321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Athens E.A, Vollmer T.R. An investigation of differential reinforcement of alternative behavior without extinction. Journal of Applied Behavior Analysis. 2010;43:569–589. doi: 10.1901/jaba.2010.43-569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachmeyer M.H, Piazza C.C, Fredrick L.D, Reed G.K, Rivas K.D, Kadey H.J. Functional analysis and treatment of multiply controlled inappropriate mealtime behavior. Journal of Applied Behavior Analysis. 2009;42:641–658. doi: 10.1901/jaba.2009.42-641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belknap W.M, McEvoy C.F. Sucking and swallowing and gastroesophageal reflux. In: Oski F.A, editor. Pediatrics. Philadelphia: Lippincott; 1994. pp. 428–430. (Ed.) [Google Scholar]
- Bernstein I.L. Flavor aversion. In: Getchell T.V, Doty R.L, Bartoshuk L.M, Snow J.B, editors. Smell and taste in health and disease. New York: Raven Press; 1991. pp. 417–428. (Eds.) [Google Scholar]
- Borrero C.S.W, Woods J.N, Borrero J.C, Masler E.A, Lesser A.D. Descriptive analyses of pediatric food refusal and acceptance. Journal of Applied Behavior Analysis. 2010;43:71–88. doi: 10.1901/jaba.2010.43-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper L.J, Wacker D.P, McComas J.J, Brown K, Peck S.M, Richman D, et al. Use of component analyses to identify active variables in treatment packages for children with feeding disorders. Journal of Applied Behavior Analysis. 1995;28:139–153. doi: 10.1901/jaba.1995.28-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Lorenzo C, Colletti R.B, Lehmann H.P, Boyle J.T, Gerson W.T, Hyams J.S, et al. Chronic abdominal pain in children: A technical report of the American Academy of Pediatrics and the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition: AAP Subcommittee and NASPGHAN Committee on Chronic Abdominal Pain. Journal of Pediatric Gastroenterology & Nutrition. 2005;43:249–261. doi: 10.1097/01.mpg.0000154661.39488.ac. [DOI] [PubMed] [Google Scholar]
- Garb J.L, Stunkard A.J. Taste aversions in man. American Journal of Psychiatry. 1974;131:1204–1207. doi: 10.1176/ajp.131.11.1204. [DOI] [PubMed] [Google Scholar]
- Garcia J, Ervin R.R, Koelling R.A. Learning with prolonged delay of reinforcement. Psychonomic Science. 1966;5:121–122. [Google Scholar]
- Garcia J, Hankins W.G, Rusiniak K.W. Behavioral regulation of the milieu interne in man and rat. Science. 1974;185:824–831. doi: 10.1126/science.185.4154.824. [DOI] [PubMed] [Google Scholar]
- Garcia J, Kimeldorf D.J, Koelling R.A. Conditioned aversion to saccharin resulting from exposure to gamma radiation. Science. 1955;122:157–158. [PubMed] [Google Scholar]
- Girolami P.A, Scotti J.R. Use of analog functional analysis in assessing the function of mealtime behavior problems. Education and Treatment in Mental Retardation and Developmental Disabilities. 2001;36:207–223. [Google Scholar]
- Hineline P.N. Negative reinforcement and avoidance. In: Honig W.K, Staddon J.E.R, editors. Handbook of operant behavior. Englewood Cliffs, NJ: Prentice Hall; 1977. pp. 364–414. (Eds.) [Google Scholar]
- Hoch T, Babbitt R.L, Coe D.A, Krell D.M, Hackbert L. Contingency contacting: Combining positive reinforcement and escape extinction procedures to treat persistent food refusal. Behavior Modification. 1994;18:106–128. doi: 10.1177/01454455940181007. [DOI] [PubMed] [Google Scholar]
- Iwata B.A. Negative reinforcement in applied behavior analysis: An emerging technology. Journal of Applied Behavior Analysis. 1987;20:361–378. doi: 10.1901/jaba.1987.20-361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwata B.A, Duncan B.A, Zarcone J.R, Lerman D.C, Shore B.A. A sequential, test-control methodology for conducting functional analyses of self-injurious behavior. Behavior Modification. 1994;18:289–306. doi: 10.1177/01454455940183003. [DOI] [PubMed] [Google Scholar]
- Lalli J.S, Vollmer T.R, Progar P.R, Wright C, Borrero J, Daniel D, et al. Competition between positive and negative reinforcement in the treatment of escape behavior. Journal of Applied Behavior Analysis. 1999;32:285–296. doi: 10.1901/jaba.1999.32-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindberg M.A, Alvin L.B, Chezik D.D, Ray D. Flavor-toxicosis associations: Tests of three hypotheses of long delay learning. Physiology & Behavior. 1982;29:439–442. doi: 10.1016/0031-9384(82)90263-3. [DOI] [PubMed] [Google Scholar]
- Najdowski A.C, Wallace M.D, Penrod B, Tarbox J, Reagon K, Higbee T.S. Caregiver-conducted experimental functional analyses of inappropriate mealtime behavior. Journal of Applied Behavior Analysis. 2008;41:459–465. doi: 10.1901/jaba.2008.41-459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel M.R, Piazza C.C, Martinez C.J, Volkert V.M, Santana C.M. An evaluation of two differential reinforcement procedures with escape extinction to treat food refusal. Journal of Applied Behavior Analysis. 2002;35:363–374. doi: 10.1901/jaba.2002.35-363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piazza C.C, Fisher W.W, Brown K.A, Shore B.A, Katz R.M, Sevin B.M, et al. Functional analysis of inappropriate mealtime behaviors. Journal of Applied Behavior Analysis. 2003;36:187–204. doi: 10.1901/jaba.2003.36-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piazza C.C, Fisher W.W, Hanley G.P, Remick M.L, Contrucci S.A, Aitken T.L. The use of positive and negative reinforcement in the treatment of escape-maintained destructive behavior. Journal of Applied Behavior Analysis. 1997;30:279–297. doi: 10.1901/jaba.1997.30-279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piazza C.C, Patel M.R, Gulotta C.S, Sevin B.S, Layer S.A. On the relative contribution of positive reinforcement and escape extinction in the treatment of food refusal. Journal of Applied Behavior Analysis. 2003;36:309–324. doi: 10.1901/jaba.2003.36-309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed G.K, Piazza C.C, Patel M.R, Layer S.A, Bachmeyer M.H, Bethke S.D, et al. On the relative contribution of noncontingent reinforcement and escape extinction in the treatment of food refusal. Journal of Applied Behavior Analysis. 2004;37:27–41. doi: 10.1901/jaba.2004.37-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley A.L, Clarke C.M. Conditioned taste aversions: A bibliography. In: Barker L.M, Best M.R, Domjan M, editors. Learning mechanisms in food selection. Waco, TX: Baylor University Press; 1977. pp. 593–616. (Eds.) [Google Scholar]
- Roberts M.L, Mace F.C, Daggett J.A. Preliminary comparison of two negative reinforcement schedules to reduce self-injury. Journal of Applied Behavior Analysis. 1995;28:579–580. doi: 10.1901/jaba.1995.28-579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rommel N, DeMeyer A.M, Feenstra L, Veereman-Wauters G. The complexity of feeding problems in 700 infants and young children presenting to a tertiary care institution. Journal of Pediatric Gastroenterology. 2003;37:75–84. doi: 10.1097/00005176-200307000-00014. [DOI] [PubMed] [Google Scholar]
- Spector A.C, Smith J.C, Hollander G.R. A comparison of dependent measures used to quantify radiation-induced taste aversion. Physiology and Behavior. 1981;27:887–901. doi: 10.1016/0031-9384(81)90059-7. [DOI] [PubMed] [Google Scholar]
- Spector A.C, Smith J.C, Hollander G.R. The effect of post-conditioning CS experience on recovery from radiation-induced taste aversion. Physiology and Behavior. 1983;30:647–649. doi: 10.1016/0031-9384(83)90236-6. [DOI] [PubMed] [Google Scholar]
- Steege M.W, Wacker D.P, Cigrand K.C, Berg W.K, Novak C.G, Reimers T.M, et al. Use of negative reinforcement in the treatment of self-injurious behavior. Journal of Applied Behavior Analysis. 1990;23:459–467. doi: 10.1901/jaba.1990.23-459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vollmer T.R, Marcus B.A, Ringdahl J.E. Noncontingent escape as treatment for self-injurious behavior maintained by negative reinforcement. Journal of Applied Behavior Analysis. 1995;28:15–26. doi: 10.1901/jaba.1995.28-15. [DOI] [PMC free article] [PubMed] [Google Scholar]