Abstract
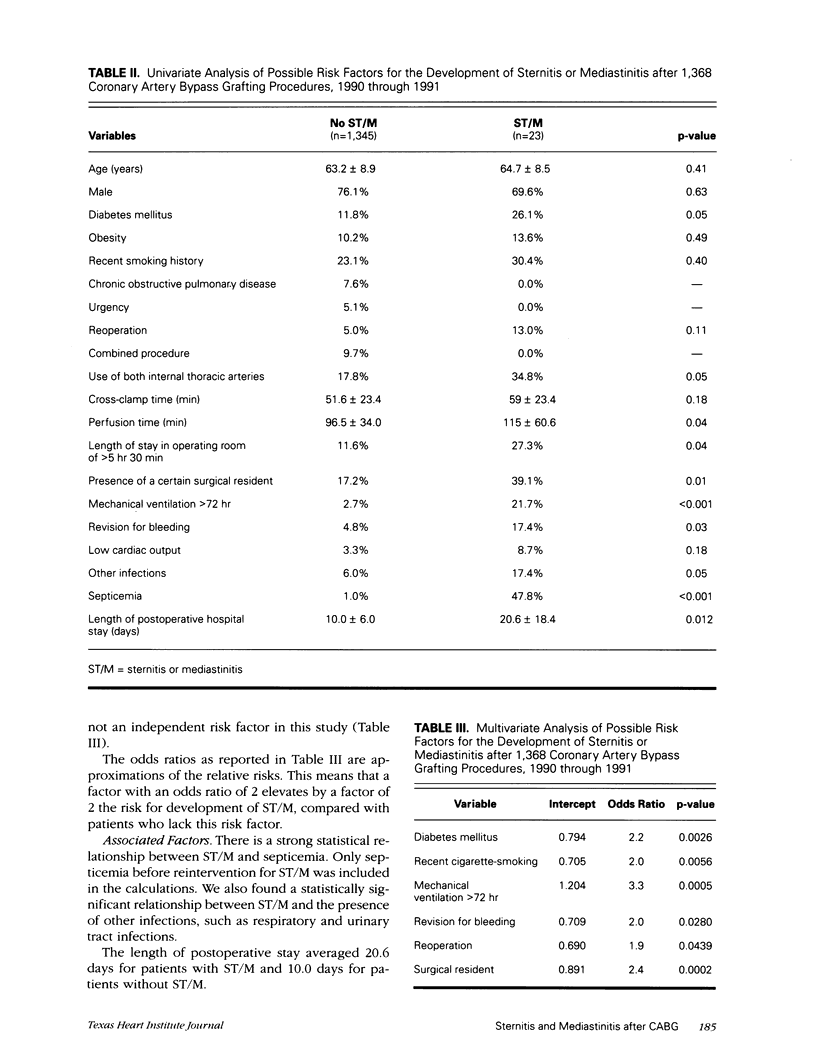
As part of a quality control program, we analyzed possible risk factors in the development of sternitis and mediastinitis after coronary artery bypass grafting. From 1 January 1990 through 31 December 1991, 1,368 consecutive coronary artery bypass grafting procedures were performed at our institution, either alone or in combination with other procedures. Twenty-three patients (1.7%) developed sternitis and/or mediastinitis; 7 (30.4%) of these patients died in an early postoperative phase. Univariate analysis revealed the following statistically significant (p < or = 0.05) risk factors: perfusion time, length of stay in operating room of longer than 5 hours 30 minutes, presence at the operation of a certain surgical resident, revision for bleeding, and postoperative mechanical ventilation lasting longer than 72 hours. After multivariate analysis, statistically significant independent risk factors were: diabetes mellitus, recent cigarette-smoking, reoperation, presence of a certain surgical resident at the operation, revision for bleeding, and length of mechanical ventilation of longer than 72 hours. The use of both internal thoracic arteries was not, in this study, shown to be an independent risk factor. We conclude that although the technique of using both internal thoracic arteries for myocardial revascularization carries no extra risk by itself in the development of sternitis or mediastinitis, associated factors such as prolonged stay in the operating room and reoperation could be responsible for a higher frequency of sternitis-mediastinitis in patients who have undergone this procedure. Therefore, it is advisable to use this technique selectively in high-risk patients. Close surveillance and reporting of wound infections is mandatory to detect risk factor related to the surgical staff (such as Staphylococcus aureus dissemination).
Full text
PDF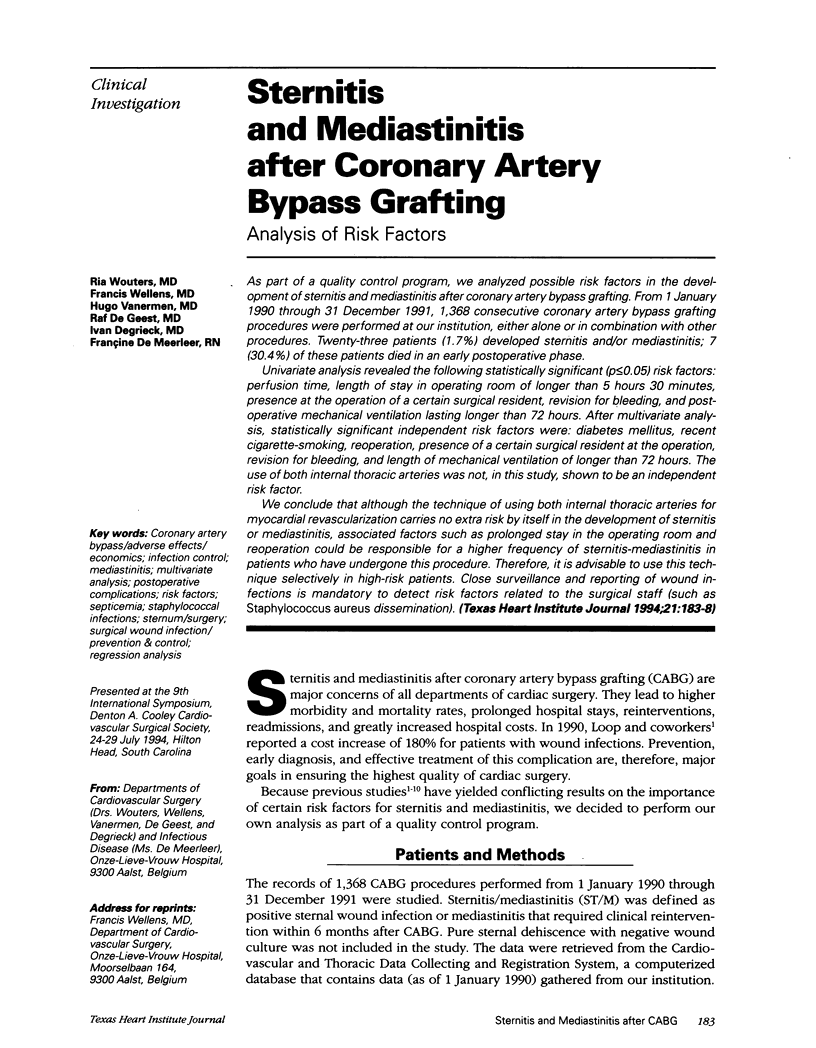




Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Fiore A. C., Naunheim K. S., Dean P., Kaiser G. C., Pennington G., Willman V. L., McBride L. R., Barner H. B. Results of internal thoracic artery grafting over 15 years: single versus double grafts. Ann Thorac Surg. 1990 Feb;49(2):202–209. doi: 10.1016/0003-4975(90)90139-w. [DOI] [PubMed] [Google Scholar]
- Galbut D. L., Traad E. A., Dorman M. J., DeWitt P. L., Larsen P. B., Kurlansky P. A., Button J. H., Ally J. M., Gentsch T. O. Seventeen-year experience with bilateral internal mammary artery grafts. Ann Thorac Surg. 1990 Feb;49(2):195–201. doi: 10.1016/0003-4975(90)90138-v. [DOI] [PubMed] [Google Scholar]
- Grossi E. A., Esposito R., Harris L. J., Crooke G. A., Galloway A. C., Colvin S. B., Culliford A. T., Baumann F. G., Yao K., Spencer F. C. Sternal wound infections and use of internal mammary artery grafts. J Thorac Cardiovasc Surg. 1991 Sep;102(3):342–347. [PubMed] [Google Scholar]
- Kohman L. J., Coleman M. J., Parker F. B., Jr Bacteremia and sternal infection after coronary artery bypass grafting. Ann Thorac Surg. 1990 Mar;49(3):454–457. doi: 10.1016/0003-4975(90)90254-4. [DOI] [PubMed] [Google Scholar]
- Kouchoukos N. T., Wareing T. H., Murphy S. F., Pelate C., Marshall W. G., Jr Risks of bilateral internal mammary artery bypass grafting. Ann Thorac Surg. 1990 Feb;49(2):210–219. doi: 10.1016/0003-4975(90)90140-2. [DOI] [PubMed] [Google Scholar]
- Loop F. D., Lytle B. W., Cosgrove D. M., Mahfood S., McHenry M. C., Goormastic M., Stewart R. W., Golding L. A., Taylor P. C. J. Maxwell Chamberlain memorial paper. Sternal wound complications after isolated coronary artery bypass grafting: early and late mortality, morbidity, and cost of care. Ann Thorac Surg. 1990 Feb;49(2):179–187. doi: 10.1016/0003-4975(90)90136-t. [DOI] [PubMed] [Google Scholar]
- Nagachinta T., Stephens M., Reitz B., Polk B. F. Risk factors for surgical-wound infection following cardiac surgery. J Infect Dis. 1987 Dec;156(6):967–973. doi: 10.1093/infdis/156.6.967. [DOI] [PubMed] [Google Scholar]
- Perrault L. P., Carrier M., Hébert Y., Hudon G., Cartier R., Leclerc Y., Pelletier L. C. Clinical experience with the right gastroepiploic artery in coronary artery bypass grafting. Ann Thorac Surg. 1993 Nov;56(5):1082–1084. doi: 10.1016/0003-4975(95)90019-5. [DOI] [PubMed] [Google Scholar]
- Seyfer A. E., Shriver C. D., Miller T. R., Graeber G. M. Sternal blood flow after median sternotomy and mobilization of the internal mammary arteries. Surgery. 1988 Nov;104(5):899–904. [PubMed] [Google Scholar]
- Ulicny K. S., Jr, Hiratzka L. F. The risk factors of median sternotomy infection: a current review. J Card Surg. 1991 Jun;6(2):338–351. doi: 10.1111/j.1540-8191.1991.tb00322.x. [DOI] [PubMed] [Google Scholar]



