Abstract
Purpose
Computer navigation has the potential to provide precise intraoperative knowledge to the surgeon. Previous studies with navigation have confirmed its function for improved component position but few studies have reported the accuracy and precision of navigation system in clinical use. With this study we propose to evaluate the efficacy of navigation in guiding cup placement.
Methods
Fifty-six patients undergoing primary total hip arthroplasty were prospectively included in this study. Stryker imageless navigation system which is accurate to 0.5° was used in all cases. Intraoperative data was collected for the acetabular component position using navigation for the freehand cup placement and the final cup placement done using navigation. Postoperative evaluation of component position was done with computed tomography (CT) and the deviation from intraoperative freehand and navigation values were calculated.
Results
The mean inclination of the freehand reading was 39.5° (range, 20°–58°), mean version of freehand reading was 10.7° (−6°– 27°), and the mean navigation reading was 43.2° (37°–49°) for inclination and 13.0° (−8° – 24°) for version. On postoperative CT scan analysis the mean inclination was 45.3° (34°–56°) and mean version was 15.1° (4°–25°). The deviation of the freehand inclination from the post operative CT scan reading was 11.4° (1°–30°) and the version deviated by a mean of 10.8° (2°–26°). The deviation of the navigation reading from the CT scan reading had a mean of 5.3° (1°–13°) for inclination and 5.6° (1°–17°) for version.
Conclusion
The accuracy of the navigation system over conventional freehand cup placement is validated by this study.
Introduction
The position of the acetabular component has historically been judged by the experience of the surgeon without precise intraoperative knowledge of the true relationship of the acetabulum to the pelvic position [1]. The consequence of clinical judgment alone could be the risk of component malposition associated with impingement of the femoral neck on the cup, which can cause dislocation, pain, accelerated wear, and loosening [2–6]. The surgeon’s performance of component implantation has traditionally always been measured by plain radiographs, which have been imprecise in comparison to the true position of the cup [7, 8]. The advent of computer navigation has revealed the imprecision of plain radiographic measurements and that of surgeons using mechanical guides for implant positioning [1, 9–12].
The primary function of computer navigation is to provide precise intraoperative knowledge to the surgeon, including acetabular component placement. Various studies in literature have assumed more accurate placement of components will provide fewer short-term complications and better long-term durability [3, 13–15]. Previous studies with computer navigation have confirmed its function as an instrument for improved component placement [1, 9–12]. These studies suggest computer navigation-assisted component placement by the surgeon is more predictable and reproducible because there is knowledge of the position of the acetabulum relative to the pelvis.
Due to relatively recent use of computer navigation, no studies document its contribution to improved long-term clinical outcomes. Few studies have measured and reported the accuracy and precision of the computer navigation system in clinical use. While previous clinical reports suggest reduced deviation from a target number for cup inclination and anteversion when using computer navigation, they have not reported the navigation system’s accuracy with precision [1, 9–12].
With this study we propose to evaluate the efficacy of navigation in guiding cup placement intraoperatively and, with the help of postoperative computerised tomography, determine the deviation of inclination and version values from their intraoperative findings. Our null hypothesis was that computer navigation was no more accurate than the conventional freehand/eyeballing techniques using the rim fit or transverse acetabular ligament.
Material and methods
Fifty-six patients were included in this prospective comparative study. All patients provided informed consent to participate in the study. All patients undergoing primary total hip arthroplasty (THA) were eligible for inclusion in the study. Patients’ age, sex, side involvement and indication for surgery were noted. Patients were examined preoperatively and leg lengths determined clinically and radiographically, and target leg length was recorded.
All procedures were carried out by a senior author (AK) who was experienced in navigated surgery and with the use of cemented and uncemented implants. The Stryker imageless navigation system (Stryker Orthopaedic, Freiberg, Germany) was used for all procedures and is accurate to 0.5°. Registration was performed supine, and the patient was then repositioned and secured in the lateral decubitus position in standard fashion. All procedures were performed through a standard posterior surgical approach and differed only in the type of component implanted and mode of fixation. The operating surgeon elected to use either cemented or press fit uncemented components, on the basis of patient age, activity, and surgeon preference.
Intraoperative data were collected with respect to acetabular component position and orientation using the navigation system for freehand cup placement as well as for final cup placement done by navigation assistance. The version and inclination were recorded for the acetabulum at reaming, trial reduction and after insertion of the definitive acetabular component. The “target” position of version and inclination was determined by the surgeon and individualised for each patient. This was declared and recorded before definitive implantation. First the cup was placed freehand by the surgeon and the navigation reading for that position noted. Whatever the deviation from the target orientation was corrected with the navigation help and target cup alignment achieved (Figs. 1 and 2). During component insertion, live feedback from the navigation system allows component adjustment to target position. Once seated, no further readjustments were made and the final navigation reading was recorded. This was done in an effort to assess the surgeon's accuracy in achieving a desired goal position using freehand and navigated methods, not the accuracy of the surgeon's presurgical planning.
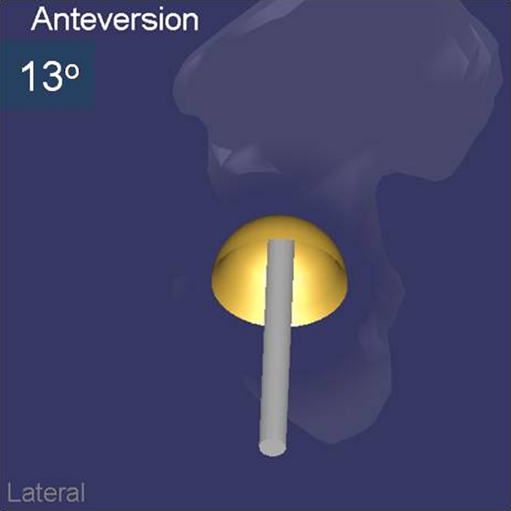
Fig. 1.
Final cup anteversion as measured by navigation
Fig. 2.
Final cup inclination as measured by navigation
The measurement of “final” component position was determined by postoperative computed tomography (CT) scans of the pelvis and the operated hip (Figs. 3 and 4). The most important adjustment done was to take the axial cuts perpendicular to the anterior pelvic plane, which was determined after the scout film on a spiral CT machine. All measurements were performed by a second surgeon (MSS), who was not involved with the surgery or the patient care. Acetabular component anteversion and inclination were measured and recorded. The cup inclination angle was measured directly on the anteroposterior scout film as the angle produced by the cup axis and the horizontal tangent drawn along both ischia. The cup version angle was measured on the broadest axial cut of the cup by the angle the cup margins subtended on the perpendicular drawn to the horizontal tangent along the ischia.
Fig. 3.
Post op CT evaluation of final cup inclination
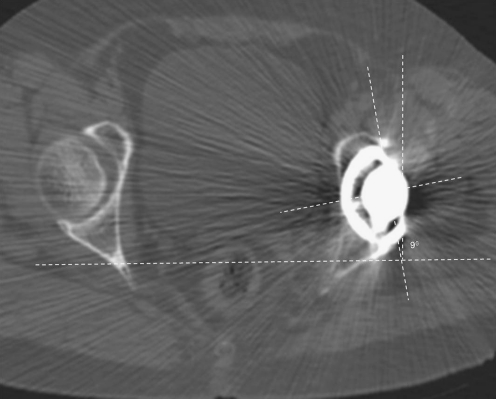
Fig. 4.
Post op CT evaluation of final cup version
To determine the accuracy of acetabular component positioning, the final orientation angles obtained for inclination and version (as determined by postoperative CT scans) were subtracted from the intraoperative values. The statistical significance of these differences, which we defined as dAf (deviation of intraoperative freehand inclination from CT inclination reading) and dVf (deviation of intraoperative freehand version from CT version reading) for the freehand reading and dAn (deviation of intraoperative navigation inclination from CT inclination reading) and dVn (deviation of intraoperative navigation version from CT version reading) for the navigation reading, was assessed.
Statistical analysis was done using SPSS software 11.5 (SPSS, Chicago, Ill). This study was approved by the institutional ethical committee.
Results
Fifty-six patients were prospectively enrolled into this study. Twenty six were males and 30 were females. Mean age of the group was 55.8 years (range 29–72 years). Thirty-one patients had left hip replacement whilst in 25 the right hip was affected. The indication for surgery was primary osteoarthrosis in 32 cases, secondary osteoarthrosis due to trauma or dysplasia in 18 cases and inflammatory arthritis in six cases.
The mean inclination of the freehand reading was 39.5° (range, 20°–58°), the mean version of freehand reading was 10.7° (−6°– 27°), the mean navigation reading were 43.2° (37°–49°) for inclination and 13.0° (−8° – 24°) for version. On postoperative CT scan analysis the mean inclination was 45.3° (34°–56°) and mean version was 15.1° (4°–25°). On calculating the deviation of the freehand reading from the post operative CT scan reading the inclination deviated by a mean of 11.4° (1°–30°) and the version deviated by a mean of 10.8° (2°–26°). The deviation of the navigation reading from the CT scan reading was a mean of 5.3° (1°–13°) for inclination and 5.6° (1°–17°) for version (Table 1).
Table 1.
Results (all values in degrees)
| Sr. No. | Freehand | Navigation | CT value | D (freehand) | D (navigation) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Inclination | Version | Inclination | Version | Inclination | Version | dAf | dVf | dAn | dVn | |
| 1 | 32 | 2 | 40 | 10 | 46 | 8 | 14 | 6 | 6 | 2 |
| 2 | 40 | -6 | 42 | 4 | 55 | 20 | 15 | 26 | 13 | 16 |
| 3 | 26 | 7 | 40 | 11 | 48 | 22 | 22 | 15 | 8 | 11 |
| 4 | 52 | 12 | 44 | 14 | 39 | 17 | 13 | 5 | 5 | 3 |
| 5 | 34 | 24 | 48 | 13 | 42 | 10 | 8 | 14 | 6 | 3 |
| 6 | 41 | 8 | 40 | -4 | 49 | 12 | 8 | 4 | 9 | 16 |
| 7 | 21 | 9 | 39 | 16 | 51 | 15 | 30 | 6 | 12 | 1 |
| 8 | 34 | 18 | 41 | 13 | 47 | 9 | 13 | 9 | 6 | 4 |
| 9 | 47 | 0 | 44 | 13 | 41 | 7 | 6 | 7 | 3 | 6 |
| 10 | 37 | 14 | 48 | -8 | 54 | 9 | 17 | 5 | 6 | 17 |
| 11 | 58 | 27 | 42 | 15 | 44 | 18 | 14 | 9 | 2 | 3 |
| 12 | 32 | 6 | 48 | 14 | 44 | 20 | 12 | 14 | 4 | 6 |
| 13 | 39 | 10 | 44 | 18 | 48 | 24 | 9 | 14 | 4 | 6 |
| 14 | 20 | 18 | 38 | 13 | 47 | 12 | 27 | 6 | 9 | 1 |
| 15 | 46 | 14 | 42 | 9 | 34 | 7 | 12 | 7 | 8 | 2 |
| 16 | 32 | 24 | 47 | 12 | 53 | 16 | 21 | 8 | 6 | 4 |
| 17 | 53 | 20 | 43 | 16 | 38 | 11 | 15 | 9 | 5 | 5 |
| 18 | 42 | 17 | 48 | 8 | 43 | 5 | 1 | 12 | 5 | 3 |
| 19 | 51 | 8 | 43 | 16 | 39 | 13 | 12 | 5 | 4 | 3 |
| 20 | 30 | 13 | 37 | 20 | 46 | 25 | 16 | 12 | 9 | 5 |
| 21 | 49 | 5 | 40 | 17 | 35 | 20 | 14 | 15 | 5 | 3 |
| 22 | 33 | -3 | 43 | 9 | 49 | 15 | 16 | 18 | 6 | 6 |
| 23 | 41 | 4 | 45 | 16 | 56 | 19 | 15 | 15 | 11 | 3 |
| 24 | 49 | 8 | 40 | 19 | 44 | 12 | 5 | 4 | 4 | 7 |
| 25 | 28 | 14 | 43 | 16 | 40 | 21 | 12 | 7 | 3 | 5 |
| 26 | 37 | -1 | 45 | 12 | 48 | 18 | 11 | 19 | 3 | 6 |
| 27 | 38 | 12 | 41 | 16 | 43 | 18 | 5 | 6 | 2 | 2 |
| 28 | 47 | 16 | 46 | 8 | 38 | 10 | 9 | 6 | 8 | 2 |
| 29 | 40 | 20 | 38 | 11 | 43 | 4 | 3 | 16 | 5 | 7 |
| 30 | 27 | 6 | 41 | 14 | 46 | 20 | 19 | 14 | 5 | 6 |
| 31 | 52 | 10 | 45 | 17 | 47 | 21 | 5 | 11 | 2 | 4 |
| 32 | 45 | 2 | 41 | 14 | 36 | 24 | 9 | 22 | 5 | 10 |
| 33 | 39 | 4 | 46 | 10 | 48 | 19 | 9 | 15 | 2 | 9 |
| 34 | 49 | 13 | 43 | 19 | 50 | 15 | 1 | 2 | 7 | 4 |
| 35 | 36 | 20 | 45 | 12 | 48 | 9 | 12 | 11 | 3 | 3 |
| 36 | 29 | -5 | 39 | 11 | 44 | 15 | 15 | 20 | 5 | 4 |
| 37 | 32 | 3 | 43 | 10 | 46 | 18 | 14 | 15 | 3 | 8 |
| 38 | 38 | 9 | 49 | 15 | 46 | 23 | 8 | 14 | 3 | 8 |
| 39 | 43 | 15 | 46 | 9 | 53 | 5 | 10 | 10 | 7 | 4 |
| 40 | 53 | 20 | 44 | 10 | 40 | 13 | 13 | 7 | 4 | 3 |
| 41 | 48 | 14 | 41 | 19 | 35 | 16 | 13 | 2 | 6 | 3 |
| 42 | 44 | 24 | 47 | 15 | 43 | 4 | 1 | 20 | 4 | 11 |
| 43 | 40 | 6 | 46 | 13 | 47 | 21 | 7 | 15 | 1 | 8 |
| 44 | 32 | 9 | 43 | 16 | 48 | 19 | 16 | 10 | 5 | 3 |
| 45 | 36 | 18 | 47 | 8 | 53 | 12 | 17 | 6 | 6 | 4 |
| 46 | 39 | 19 | 42 | 13 | 48 | 5 | 9 | 14 | 6 | 8 |
| 47 | 43 | 6 | 46 | 15 | 56 | 14 | 13 | 8 | 10 | 1 |
| 48 | 35 | 3 | 40 | 12 | 46 | 18 | 11 | 15 | 6 | 6 |
| 49 | 47 | 9 | 42 | 18 | 44 | 21 | 3 | 12 | 2 | 3 |
| 50 | 51 | 15 | 45 | 24 | 39 | 20 | 12 | 5 | 6 | 4 |
| 51 | 46 | 21 | 41 | 17 | 44 | 13 | 2 | 8 | 3 | 4 |
| 52 | 41 | 8 | 44 | 5 | 51 | 14 | 10 | 6 | 7 | 9 |
| 53 | 38 | 2 | 47 | 18 | 43 | 14 | 5 | 12 | 4 | 4 |
| 54 | 32 | 11 | 43 | 11 | 41 | 21 | 9 | 10 | 2 | 10 |
| 55 | 29 | 16 | 39 | 20 | 47 | 10 | 18 | 6 | 8 | 10 |
| 56 | 43 | 4 | 48 | 17 | 46 | 25 | 3 | 21 | 2 | 8 |
dAf deviation of intraoperative freehand inclination from CT inclination reading, dVf deviation of intraoperative freehand version from CT version reading, dAn deviation of intraoperative navigation inclination from CT inclination reading, dVn deviation of intraoperative navigation version from CT version reading
There was statistical significant difference between the deviation of freehand reading and the deviation of navigation reading in the inclination values (p = 0.00) as well as the version values (p = 0.01) on the paired t-test and hence our null hypothesis was rejected.
Discussion
Acetabular component malposition has been implicated for various complications of total hip replacement including impingement, dislocation and early wear and loosening, among others [12, 16, 17]. Lewinnek et al. [13] have defined a safe zone for the acetabular component placement which they postulated would bring down the incidence of these complications. The safe zone widely accepted by various authors is inclination of 40°±10° and anteversion of 15°±10° [14, 18, 19].
In this comparative study to improve accuracy of acetabular component placement, we tried to assess the freehand angles (as assessed by the navigation system) and subsequently corrected to safe zone with navigation assistance. This was then evaluated with a postoperative CT scan to measure the actual cup orientation.
The term “freehand” in literature is not so clearly defined. Manual positioning of cup by eyeballing and referencing the same to anatomical structures such as the transverse acetabular ligament is what is inferred in this study. Transverse acetabular ligament has been suggested as one of the soft tissue landmarks by Archbold et al. [20] along with the acetabular rim and labrum. The main advantage of these structures being the 3-dimensional view and the patient specific morphology [19]. But the limitation we faced was the problem of defining the structures especially in very obese patients or in acetabuli affected by trauma or dysplasia. As almost 14.2% (n = 8) were found to have some form of primary or secondary dysplasia in the acetabulum, we found that the transverse acetabular ligament was difficult to delineate in these cases and we had to use bony landmarks such as the acetabular rim and the acetabular notch as defined by Maruyama et al. [21].
Both the techniques had a dislocation rate of 0.36% to 0.6% in the hands of surgeons who described them, so for a beginner who has little exposure to assessing these landmarks, freehand cup positioning is a challenging task. Hence, to overcome this challenge of minimising this wide variation, the navigation assisted cup placement has evolved in the last two decades.
Lawrence et al. [22] have tried to evaluate the same issue by considering that the navigation system was accurate to within 5° of the required values. They used a CT based navigation system and intraoperatively they manipulated the manual cup position to achieve 35–45° inclination. Bosker et al. [23] evaluated 200 acetabular components positioning with postoperative radiographs inserted by experienced surgeons as well as trainees. They found that experienced surgeons had a mean deviation of 4° inclination and 5° of anteversion. The resident trainee on the other hand misplaced the cup by a mean of 6.3° of inclination and 5.7° of version. They also concluded that the chance of accurate cup inclination is only 70% in the most experienced hands and it falls to 21.5% if the cup is to be placed within 5% of the safe zone values as described by Lewinnek et al.
In our study of 56 cups we analysed with postop CT for the deviation between freehand estimates and navigation suggested reading. The results showed that freehand values deviated by a mean of 11.4° for inclination (range 1°–30°) and 10.8° for version (range 2°–26°), whereas the navigation readings deviated for the same by 5.3° (1°–13°) and 5.6° (1°–17°), respectively. Our study also revealed a statistically significant difference between the deviation of freehand and navigation readings in both the inclination values and the version values; thus conclusively proving the superior accuracy of navigation assisted cup placement over the conventional technique.
In two of our early cases, navigation readings appeared to be way off the safe zone. The navigation estimated a retroversion of 8° in one case where the surgeon believed the cup was definitely in the range of 10–15° of anteversion by the anatomical landmarks. On reanalysing these two cases step-by-step, we found that we had most probably erred in the proper patient registration, which is very important in imageless system. Nogler et al. [12] investigated the use of navigation in cup positioning in cadavers and they proved the accuracy of the navigation system as compared to manual methods; but in their study they fixed screws on the bony landmarks to avoid any errors. Furthermore, obesity presents a major hindrance in identifying the points as we found in 18/56 cases of our study. Two of these cases only had navigation readings outside the safe zone. Following these initial experiences, we started to mark our bony landmark preoperatively with an ECG lead. This allowed us to avoid the errors with registration in subsequent cases especially in obese individuals.
The drawbacks of the navigation system are its cost and additional procedures intraoperatively, such as fixing tracker and registration which add on to the surgical time. These can be considered negligible in comparison to the advantages of navigation assisted cup positioning.
Conclusion
This study validates the accuracy of a navigation system over the conventional techniques. No matter which cup orientation is regarded as the best, this position can be reached with a narrower margin of error using navigation assistance than that attained by use of conventional freehand cup placement.
Acknowledgement
We would like to thank Ms. Neevan D’souza, Lecturer of Statistics, Department of PSM, Yenopoya Medical College, Mangalore for her assistance in this study.
References
- 1.Digioia AM, 3rd, Jaramaz B, Plakseychuk AY, Moody JE, Nikou C, Labarca RS, Levison TJ, Picard F. Comparison of a mechanical acetabular alignment guide with computer placement of the socket. J Arthroplasty. 2002;17:359–364. doi: 10.1054/arth.2002.30411. [DOI] [PubMed] [Google Scholar]
- 2.Barrack RL, Lavernia C, Ries M, Thornberry R, Tozakoglou E. Virtual reality computer animation of the effect of component position and design on stability after total hip arthroplasty. Orthop Clin North Am. 2001;32:569–577. doi: 10.1016/S0030-5898(05)70227-3. [DOI] [PubMed] [Google Scholar]
- 3.Charnley J, Cupic Z. The nine and ten year results of the low friction arthroplasty of the hip. Clin Orthop Relat Res. 1973;95:9–25. [PubMed] [Google Scholar]
- 4.D’Lima DD, Urquhart AG, Buehler KO, Walker RH, Colwell CW., Jr The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. J Bone Joint Surg Am. 2000;82:315–321. doi: 10.2106/00004623-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Scifert CF, Brown TD, Pedersen DR, Callaghan JJ. A finite element analysis of factors influencing total hip dislocation. Clin Orthop Relat Res. 1998;355:152–162. doi: 10.1097/00003086-199810000-00016. [DOI] [PubMed] [Google Scholar]
- 6.Yamaguchi M, Akisue T, Bauer TW, Hashimoto Y. The spatial location of impingement in total hip arthroplasty. J Arthroplasty. 2000;15:305–313. doi: 10.1016/S0883-5403(00)90601-6. [DOI] [PubMed] [Google Scholar]
- 7.Jaramaz B, DiGioia AM, 3rd, Blackwell M, Nikou C. Computer assisted measurement of cup placement in total hip replacement. Clin Orthop Relat Res. 1998;354:70–81. doi: 10.1097/00003086-199809000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Tannast M, Langlotz U, Siebenrock KA, Wiese M, Bernsmann K, Langlotz F. Anatomic referencing of cup orientation in total hip arthroplasty. Clin Orthop Relat Res. 2005;436:144–150. doi: 10.1097/01.blo.0000157657.22894.29. [DOI] [PubMed] [Google Scholar]
- 9.Jolles BM, Genoud P, Hoffmeyer P. Computer-assisted cup placement techniques in total hip arthroplasty improve accuracy of placement. Clin Orthop Relat Res. 2004;426:174–179. doi: 10.1097/01.blo.0000141903.08075.83. [DOI] [PubMed] [Google Scholar]
- 10.Kalteis T, Handel M, Herold T, Perlick L, Baethis H, Grifka J. Greater accuracy in positioning of the acetabular cup by using an image-free navigation system. Int Orthop. 2005;29:272–276. doi: 10.1007/s00264-005-0671-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leenders T, Vandevelde D, Mahieu G, Nuyts R. Reduction in variability of acetabular cup abduction using computer assisted surgery: a prospective and randomized study. Comput Aided Surg. 2002;7:99–106. doi: 10.3109/10929080209146021. [DOI] [PubMed] [Google Scholar]
- 12.Nogler M, Kessler O, Prassl A, Donnelly B, Streicher R, Sledge JB, Krismer M. Reduced variability of acetabular cup positioning with use of an imageless navigation system. Clin Orthop Relat Res. 2004;426:159–163. doi: 10.1097/01.blo.0000141902.30946.6d. [DOI] [PubMed] [Google Scholar]
- 13.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220. [PubMed] [Google Scholar]
- 14.McCollum DE, Gray WJ. Dislocation after total hip arthroplasty. Causes and prevention. Clin Orthop Relat Res. 1990;261:159–170. [PubMed] [Google Scholar]
- 15.Ng Fu Yuen, Zhang JT, Chiu KY, Yan CH. A cadaveric study of posterior dislocation after total hip replacement—effects of head diameter and acetabular anteversion. Int Orthop. 2011;35(3):325–329. doi: 10.1007/s00264-010-0977-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paterno SA, Lachiewicz PF, Kelley SS. The influence of patient-related factors and the position of the acetabular component on the rate of dislocation after total hip replacement. J Bone Joint Surg Am. 1997;79:1202–1210. doi: 10.2106/00004623-199708000-00013. [DOI] [PubMed] [Google Scholar]
- 17.Kennedy JG, Rogers WB, Soffe KE, Sullivan RJ, Griffen DG, Sheehan LJ. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplast. 1998;13:530–534. doi: 10.1016/S0883-5403(98)90052-3. [DOI] [PubMed] [Google Scholar]
- 18.Saxler G, Marx A, Vandevelde D, Langlotz U, Tannast M, Wiese M, Michaelis U, Kemper G, Grutzner PA, Steffen R, Knoch M, Holland-Letz T, Bernsmann K. The accuracy of free-hand cup positioning—a CT based measurement of cup placement in 105 total hip arthroplasties. Int Orthop. 2004;28:198–201. doi: 10.1007/s00264-004-0542-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moskal JT, Capps SG. Improving the accuracy of acetabular component orientation: avoiding malposition. J Am Acad Orthop Surg. 2010;18:286–296. doi: 10.5435/00124635-201005000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Archbold HA, Mockford B, Molloy D, McConway J, Ogonda L, Beverland D. The transverse acetabular ligament: An aid to orientation of the acetabular component during primary total hip replacement. A preliminary study of cases investigating postoperative stability. J Bone Joint Surg Br. 2006;88:883–886. doi: 10.1302/0301-620X.88B7.17577. [DOI] [PubMed] [Google Scholar]
- 21.Maruyama M, Feinberg JR, Capello WN, D’Antonio JA. The Frank Stinchfield Award: Morphologic features of the acetabulum and femur. Anteversion angle and implant positioning. Clin Orthop Relat Res. 2001;393:52–65. doi: 10.1097/00003086-200112000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Dorr LD, Malik A, Wan Z, Long WT, Harris M. Precision and bias of imageless computer navigation and surgeon estimates for acetabular component position. Clin Orthop Relat Res. 2007;465:92–99. doi: 10.1097/BLO.0b013e3181560c51. [DOI] [PubMed] [Google Scholar]
- 23.Bosker BH, Verheyen PM, Horstmann WG, Tulp NJA. Poor accuracy of freehand cup positioning during total hip arthroplasty. Arch Orthop Trauma Surg. 2007;127:375–379. doi: 10.1007/s00402-007-0294-y. [DOI] [PMC free article] [PubMed] [Google Scholar]