Abstract
Purpose
The aim of this study was to review our experiences with tibial lengthening over an intramedullary nail in comparison to the conventional Ilizarov method.
Methods
We performed a retrospective comparison of tibial lengthening using the conventional Ilizarov method (group A: 23 limbs in 13 patients) versus over a nail (group B: 51 limbs in 26 patients). The percentage increase in tibial length, lengthening index, external fixation index, consolidation index and complications were assessed.
Results
The mean gain in tibial length was 7.4 cm, which represents a mean increase of 26.0%. There was no difference in lengthening index or consolidation index; however, the patients in group A wore the external fixator longer than those in group B (281.5 versus 129.0 days), which represents a larger external fixation index (40.0 versus 17.4 day/cm). Group A had a higher complication rate (1.0 versus 0.47 per tibia) than group B.
Conclusions
Tibial lengthening over an intramedullary nail confers advantages over the conventional Ilizarov method, including shorter time needed for external fixation and lower complication rates.
Introduction
Distraction osteogenesis using the conventional Ilizarov method is an excellent option and is widely used for limb lengthening and correction; however, such treatment requires a long period of external fixation in a frame during both distraction and consolidation phases [1–3]. Patients often tolerate the consolidation period poorly, and complications such as pin-tract infections and stiffness of the joints may develop. Moreover, if the external fixator is removed too early, it may result in axial deviation or refracture. Since Paley et al. first described it in 1997 [4], the surgical technique of lengthening over an intramedullary (IM) nail has gained wide acceptance because it reduces the duration required for external fixation and offers considerable improvements in patients’ comfort [5]. However, Watanabe et al. have reported that they encountered such a high rate of serious complications in patients treated with lengthening over an IM nail, including cases of deep infection and breakage of nails or locking screws, that they abandoned this technique and returned to the classic Ilizarov method [6].
The purpose of this study was to retrospectively compare tibial lengthening over an IM nail (group B) with the conventional Ilizarov method (group A) in individuals with leg-length discrepancy or short stature. We evaluated a variety of parameters including percentage increase, lengthening index, external fixation index, consolidation index and associated complications. To our knowledge, few studies on tibial lengthening over an IM nail involving large number of cases with same aetiology have been reported. We present here the results with regard to distracted bone formation and details of complications.
Materials and methods
This study was designed as a retrospective review and was approved by our hospital’s institutional review board. Between May 1996 and May 2006, 115 individuals (202 limbs) underwent tibial lengthening in our centre for different reasons. Patients with immature bone, soft tissue compromise, bone deformity of a severity that required gradual deformity correction, and currently active or history of infection or trauma at the site of lengthening were excluded. An Ilizarov external fixator (Yian lifang, Beijing, China) was used in both groups, and an additional intramedullary nail (Trauson, Changzhou, Jiangsu, China) was used in group B.
This study included 74 tibiae in 39 individuals (35 short stature, four congenital leg-length discrepancy), of whom 13 individuals (23 leg-lengthening procedures) were in group A and 26 (51 lengthening procedures) in group B. There were ten patients with short stature in group A and 25 in group B; there were three patients with congenital leg-length discrepancy in group A and one in group B. There were eight males and 31 females. The average age at the time of surgery was 22.7 years (range, 18–42 years) in group A and 25.4 years (range, 19–47 years) in group B. The mean preoperative length of the tibiae was 27.3 ± 2.5 cm in group A and 29.3 ± 2.3 cm in group B. The average duration of follow-up was 3.2 years (range, 2.2–4.3 years) in group A and 3.4 years (range, 1.8–5.0 years) in group B. All patient clinical and demographic data can be seen in Table 1.
Table 1.
Patient clinical and demographic data
| Parameter | Group Aa | Group Bb |
|---|---|---|
| Number of patients | 13 | 26 |
| Number of tibiae | 23 | 51 |
| Age in years (range) | 22.7 (18 –42) | 25.4 (19 –47) |
| Gender (female/male) | 10/3 | 21/5 |
| Bilateral (short stature) | 10 | 25 |
| Congenital leg-length discrepancy | 3 | 1 |
a Conventional Ilizarov method
b Lengthening over a nail
Surgical technique and postoperative protocol
All operations were performed under regional anaesthesia and tourniquets were not used. With the multiple-drill-hole technique, careful corticotomy was performed at the proximal meta-diaphyseal junction of tibia, and at the distal one third junction of the fibula. An Ilizarov frame (composed of five full rings and four distraction rods, an additional 1/2 “U”-shaped ring for the calcaneus when the anticipated lengthening was more than 20%) was used. The wires with diameters of 2.0 mm were typically tensioned to 1000–1200 N, and the crossing angles were 60º or more to increase the stability [7]. At least one wire was used to fix the proximal or distal tibiofibular joint. In group A, each bone segment was mounted with four wires. In group B, the tibial intramedullary canal was at least 8 mm and unreamed nails were used. The nail was inserted carefully until it reached the distal metaphysis; then two proximal interlocking screws were inserted with the aid of a jig. A preconstructed Ilizarov frame was mounted with at least six wires.
Lengthening was started on day seven to ten postoperatively at a rate of 0.25 mm four times daily or with minor adjustments. The patients were encouraged to exercise and to perform gait training with a walker after surgery. Prophylactic intravenous antibiotics were administered for 48 hours. In the outpatient clinic, the individuals were examined every four weeks and screened for local signs of infection. In group A, the fixators were removed when the individual was fully weight-bearing, and after confirmation of complete radiographic consolidation. In group B, after the desired length was achieved, the Ilizarov fixators were removed and two distal interlocking screws were inserted (typical tibial lengthening over a nail seen in Fig. 1).
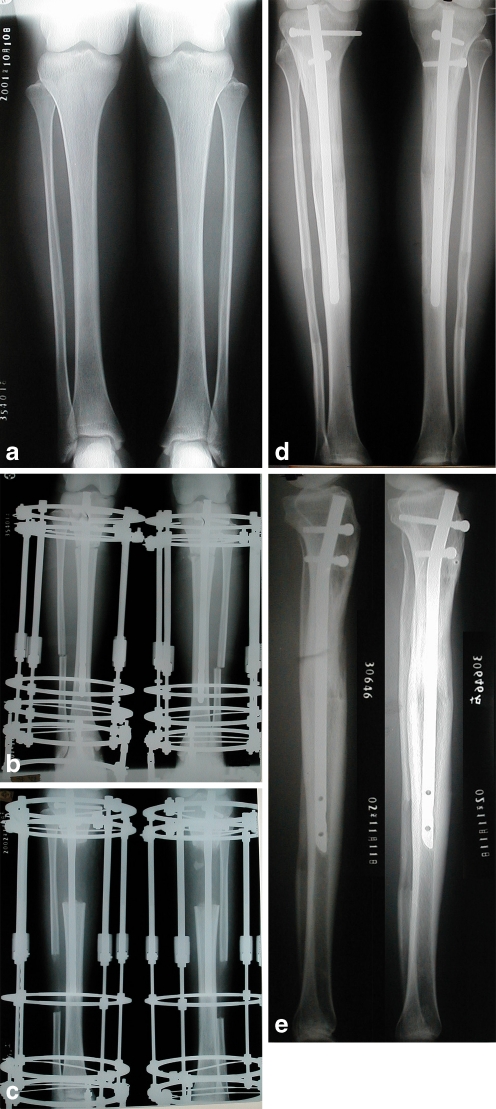
Fig. 1.
Serial radiographs of tibial lengthening (length gained, 9 cm; percentage lengthening, 26.4%) in a 24-year-old woman. A Anteroposterior (AP) radiograph taken before operation. B Immediate postoperative AP radiograph showing nailing and external fixator application had been performed. C AP radiograph taken at completion of the lengthening phase. D, E AP and lateral radiographs taken after the completion of new bone maturation
Outcome measures
Four indices were used, namely, percentage increase, lengthening index, external fixation index and consolidation index. The percentage increase was defined as the length gained divided by the original length; the lengthening index as the duration of distraction phase divided by the length gained in centimetres; the external fixation index as the duration of external fixation divided by the length gained; and the consolidation index as the time of consolidation (from the operation day to the confirmation of consolidation) divided by the length gained. Consolidation was considered to be complete when anteroposterior and lateral radiographs confirmed at least three of four cortices were intact.
The independent Student’s t-test or the Mann-Whitney U-test was used to analyse the differences with regard to the radiographic parameters, gain in length, age and sex. Differences in the number of complications were assessed with the Pearson χ2 test. A P value of <0.05 was regarded as significant.
Results
The mean gain in tibial length was 7.4 cm (range, 3.6–11.0 cm), which represented a mean increase of 26.0% (range, 11.3–43.1%). An increase in length of 7.2 cm (range, 5.0–9.0 cm), or 26.9% (range, 14.3–33.3%), was achieved in group A, and an increase of 7.4 cm (range, 3.6–11.0 cm), or 25.6% (range, 11.3–43.1%) in group B (P > 0.05). The mean lengthening index was 14.4 d/cm (range, 9.7–20.7 d/cm) in group A and 13.3 d/cm (range, 8.2–18.5 d/cm) in group B (P = 0.371). The mean duration of external fixation was 281.5 days (range, 198–384) in group A and 129.0 days (range, 52–184) in group B, resulting in a mean external fixation index of 40.0 d/cm (range, 24.8–58.6 d/cm) in group A and 17.4 d/cm (range, 14.0–22.8 d/cm) in group B (P < 0.001). The mean consolidation index was 40.6 d/cm (range, 27.1–58.4 d/cm) in group A and 40.7 d/cm (range, 28.7–54.5 d/cm) in group B (P = 0.957) (shown in Table 2).
Table 2.
Comparisons of clinical result between two groups
| Parameter | Group A | Group B | P value |
|---|---|---|---|
| Length gaineda (cm) | 7.2 ± 1.2 | 7.4 ± 1.3 | 0.571 |
| Length gaineda (%) | 26.9 ± 5.4 | 25.6 ± 6.0 | 0.387 |
| Lengthening indexa (d/cm) | 14.4 ± 3.4 | 13.3 ± 2.6 | 0.371 |
| External fixation indexa (d/cm) | 40.0 ± 10.7 | 17.4 ± 2.4 | <0.001 |
| Consolidation indexa (d/cm) | 40.6 ± 8.3 | 40.7 ± 6.5 | 0.957 |
| Complications b | |||
| Problems | 20.0 (0.87) | 19.0 (0.37) | <0.001 |
| Obstacles | 3.0 (0.13) | 5.0 (0.10) | 0.678 |
| Sequelae | 0.0 | 0.0 | |
| Total | 23.0 (1.0) | 24.0 (0.47) | <0.001 |
There were 23 tibiae in group A and 51 in group B
a The values are given as the mean and standard deviation
b The values are given as the number of complications with the mean number per tibia in parentheses
According to Paley's classification system [1, 2], 23 complications occurred in group A, including 20 problems and three obstacles; whereas 24 complications occurred in group B, including 19 problems and five obstacles. No sequelae occurred in either group. The average number of complications was 1.0 per tibia in group A and 0.47 per tibia in group B (P < 0.001) (complication details shown in Table 3).
Table 3.
Details of complications
| Complications | Group A | Group B | ||||
|---|---|---|---|---|---|---|
| Total | Problems | Obstacles | Total | Problems | Obstacles | |
| Pin-tract infection | 11 | 11 | 0 | 8 | 8 | 0 |
| Wire breakage | 1 | 0 | 1 | 1 | 1 | 0 |
| Interlocking screw breakage | 0 | 0 | 0 | 3 | 3 | 0 |
| Intramedullary nail breakage | 0 | 0 | 0 | 1 | 0 | 1 |
| Premature consolidation | 1 | 0 | 1 | 1 | 0 | 1 |
| Delayed consolidation | 2 | 2 | 0 | 1 | 0 | 1 |
| Distal migration of fibula | 1 | 0 | 1 | 2 | 0 | 2 |
| Knee flexion contracture | 2 | 2 | 0 | 3 | 3 | 0 |
| Ankle flexion contracture | 4 | 4 | 0 | 4 | 4 | 0 |
| Axial deviation | 1 | 1 | 0 | 0 | 0 | 0 |
| Total | 23 | 20 | 3 | 24 | 19 | 5 |
| Rate of complication | 1.0 | 0.47 | ||||
Values are given as the number of tibiae. There were 23 tibiae in group A and 51 in group B
A transfixing wire broke in one case in each group; substitution of a new wire augmented to the ring meant that effective distraction was not jeopardised. Inferior subluxation and distal migration of the fibular head due to cutting out of wire was seen once in group A and twice in group B; once identified they were treated by reinsertion of a transfixing wire. Pin-track infections occurred in 11 tibiae (47.8%) in group A and eight (15.6%) in group B. No deep intramedullary infection occurred. A broken interlocking screw was found in three (5.9%) cases during the consolidation phase in group B, but none required further intervention. A broken intramedullary nail occurred in one case (1.9%) because of a motor vehicle accident; further surgery was required to exchange the nail.
One patient required repeat tibial osteotomy for premature consolidation in group A, and one required repeat fibular osteotomy in group B. In group A two cases had delayed consolidation with prolonged fixation; one case in group B required auto-iliac bone graft and exchange of intramedullary nail and both eventually achieved good consolidation.
In group A two knee (8.7%) and four ankle (17.4%) flexion contractures occurred, two of which were combined with ankle valgus, and full range of movement was regained with physiotherapy in knee and two ankles, the other two lacking 5° motion (no limitation of daily life) at the latest follow-up. In group B three knee (5.9%) and four ankle (7.8%) flexion contractures developed, one combined with ankle valgus, and all resolved fully with physiotherapy. No surgical lengthening of the Achilles tendon was required.
Discussion
Distraction osteogenesis by the Ilizarov method is a well-established technique for leg lengthening and deformity correction. However, the overall process of distraction and consolidation in a frame involves a high risk of complications. Moreover, early frame removal can induce secondary axial deformity and risk of fracture. In this retrospective study we found that, compared with the conventional Ilizarov method, tibial lengthening over an IM nail reduces the time required for external fixation, maintains the length gained and prevents refracture of newly formed bone.
We found that the mean external fixation index differed significantly between the two groups; however, the consolidation index was similar. Lengthening over a nail has gained wide acceptance, because it improves patients’ comfort and provides additional axial and rotational stability. Earlier removal of external fixation makes it easier for patients to exercise the surrounding joints fully before contractures become irreversible. Some authors have expressed concern that intramedullary nailing might compromise the endosteal blood supply and thus affect the quality of newly formed bone [8, 9]. We used unreamed nails and found no difference between the two groups in consolidation, which is similar to other results [10, 11].
We found that the overall rate of complications was relatively low, and differed significantly between the two groups. It has been noted that a greater lengthening percentage correlates well with a higher complication rate [12]. Mehmet et al. set a lengthening rate of 21.5% and a total lengthening of 6 cm as cut-off points, above which complications were more likely to occur [13]. In our group, the mean percentage of lengthening was 26.9% in group A, and 25.6% in group B, whereas the average number of complications was 1.0 per tibia and 0.47 per tibia, respectively. This is relatively low and satisfactory compared with the results of Hui et al., who reported an average number of complications of 2.56 per tibia for the conventional Ilizarov method, and 1.24 per tibia for lengthening over a nail [10]. They suggested that complications related to joint stiffness were the rule rather than the exception, even with lengthening over an IM nail. No obstacle or sequel affected surrounding joints in our group. We think that the strong structure composed of five full rings makes ambulation possible with the assistance of a walker, even during the distraction phase. Moreover, the special spring apparatus provided around the ankle joint allows rehabilitation during the whole procedure, thus preventing Achilles tendon contracture. Fat embolism is a major concern with combined intramedullary nail and external fixation, especially with simultaneous bilateral procedures. No fat embolism was observed in our group.
We found that pin-site infection differed significantly between the two groups (47.8% in group A, 15.7% in group B). The most serious potential disadvantage of lengthening over an IM nail is deep infection; however, no deep infection occurred in our groups. This is good compared with the deep infection rates of 5%, 14% and 15% previously reported by Silberg et al. [14], Song et al. [15] and Simpson et al. [16], respectively. We performed the surgery according to Paley’s recommendation to avoid contact between the pin and the nail [4]. We believe that earlier and more aggressive local medical intervention for pin site infection contributed to preventing deep infections.
Lengthening over an IM nail can easily be performed with the tibia, where the mechanical and anatomical axes coincide, as opposed to the femur, where the two axes are different and would cause additional translation [4, 17]. Axial deviation was not observed clinically or radiographically in group B. Angulation at the lengthening site occurred in only one tibia (4.3%) in group A, partly because of imbalanced distraction. It was treated by adjustment of the distraction rods and additional tightening of the wires and nuts. Our result is more acceptable than the 16% rate of secondary axial deviation that occurred in the series of Hui et al., in which an unstable two-ring Ilizarov frame was used [10]. We believe that the structure composed of five full rings is more effective to strengthen the stability.
Premature consolidation occurred in one case in each group during the distraction phase—one because of imbalance distraction and the other due to mechanical problems related to the external fixator (the lengthening index was 20.71). Delayed consolidation was observed twice in group A and once in group B, which might be due in part to a relatively large percentage of distraction (more than 33%). Further study is necessary to identify other factors that could be responsible for delayed consolidation. Distal migration of the fibula occurred in one case in each group, it seems that single-wire fixation of the proximal tibiofibular joint is inadequate and more secure fixation might be indicated [18].
The major limitation of our study is that it was retrospective and did not allow direct comparison of all aspects. Although there were no differences with respect to the sex, age and aetiology, decisions such as percentage lengthening and selection of lengthening method were based in part on the patients’ aims and economic background. Furthermore, it was difficult to assign a point of bony union. We assessed the time as corresponding to the patient’s ability to bear full weight and the presence of bridging of three of four cortices on radiographs. We do not think this compromised our conclusions, since we chose a consistent practical time point for healing. A prospective, randomised, controlled trial, which would eliminate the variable of patient selection, would be the best study to undertake next. Our results show that tibial lengthening over an IM nail provides advantages including a lower complication rate, shorter times needed in external fixation, more comfort and earlier rehabilitation.
Acknowledgments
This work was sponsored by National Natural Science Foundation of China (11072021).
References
- 1.Fischgrund J, Paley D, Suter C. Variables affecting time to bone healing during limb lengthening. Clin Orthop Relat Res. 1994;301:31–37. [PubMed] [Google Scholar]
- 2.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed] [Google Scholar]
- 3.Tao Z, Sun ZH, Zheng YF, Ma XL, Wang P, Li H. Ilizarov method associated with bone lengthening for treating infected nonunion of tibia with large defects. Chin J Orthop. 2008;28(5):353–357. [Google Scholar]
- 4.Paley D, Herzenberg JE, Paremain G, Bhave A. Femoral lengthening over an intramedullary nail: a matched-case comparison with Ilizarov femoral lengthening. J Bone Joint Surg Am. 1997;79(10):1464–1480. doi: 10.2106/00004623-199710000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Kim H, Lee SK, Kim KJ, Ahn JH, Choy WS, Kim YI, Koo JY. Tibial lengthening using a reamed type intramedullary nail and an Ilizarov external fixator. Int Orthop. 2009;33:835–841. doi: 10.1007/s00264-008-0550-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kristiansen LP, Steen H. Lengthening of the tibia over an intramedullary nail using the Ilizarov external fixator. Major complications and slow consolidation in 9 lengthenings. Acta Orthop Scand. 1999;70:271–274. doi: 10.3109/17453679908997806. [DOI] [PubMed] [Google Scholar]
- 7.Spiegelberg B, Parratt T, Dheerendra SK, Khan WS, Jennings R, Marsh DR. Ilizarov principles of deformity correction. Ann R Coll Surg Engl. 2010;92(2):101–105. doi: 10.1308/003588410X12518836439326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reichert IL, McCarthy ID, Hughes SP. The acute vascular response to intramedullary reaming: microsphere estimation of blood flow in the intact ovine tibia. J Bone Joint Surg Br. 1995;77(3):490–493. [PubMed] [Google Scholar]
- 9.Sitter T, Wilson J, Browner B. The effect of reamed versus unreamed nailing on intramedullary blood supply and cortical viability. J Orthop Trauma. 1990;4:232. doi: 10.1097/00005131-199004020-00074. [DOI] [Google Scholar]
- 10.Park HW, Yang KH, Lee KS, Joo SY, Kwak YH, Kim HW. Tibial lengthening over an intramedullary nail with use of the Ilizarov external fixator for idiopathic short stature. J Bone Joint Surg Am. 2008;90(9):1970–1978. doi: 10.2106/JBJS.G.00897. [DOI] [PubMed] [Google Scholar]
- 11.Watanabe K, Tsuchiya H, Sakurakichi K, Yamamoto N, Kabata T, Tomita K. Tibial lengthening over an intramedullary nail. J Orthop Sci. 2005;10(5):480–485. doi: 10.1007/s00776-005-0939-z. [DOI] [PubMed] [Google Scholar]
- 12.Antoci V, Ono CM, Antoci V, Jr, Raney EM. Axial deformity correction in children via distraction osteogenesis. Int Orthop. 2006;30:278–283. doi: 10.1007/s00264-005-0071-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kocaoglu M, Eralp L, Kilicoglu O, Burc H, Cakmak M. Complications encountered during lengthening over an intramedullary nail. J Bone Joint Surg Am. 2004;86-A(11):2406–2411. doi: 10.2106/00004623-200411000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Silberg ET, Goulet JA, Greenfield ML. Femoral lengthening: conventional Ilizarov technique compared to lengthening over an intramedullary rod. Orthop Trans. 1997;21:71. [Google Scholar]
- 15.Song HR, Oh CW, Mattoo R, Park BC, Kim SJ, Park IH, Jeon IH, Ihn JC. Femoral lengthening over an intramedullary nail using the external fixator: risk of infection and knee problems in 22 patients with a follow-up of 2 years or more. Acta Orthop. 2005;76(2):245–252. doi: 10.1080/00016470510030652. [DOI] [PubMed] [Google Scholar]
- 16.Simpson AH, Cole AS, Kenwright J. Leg lengthening over an intramedullary nail. J Bone Joint Surg Br. 1999;81(6):1041–1045. doi: 10.1302/0301-620X.81B6.9359. [DOI] [PubMed] [Google Scholar]
- 17.Baumgart R, Betz A, Schweiberer L. A fully implantable motorized intramedullary nail for limb lengthening and bone transport. Clin Orthop Relat Res. 1997;343:135–143. doi: 10.1097/00003086-199710000-00023. [DOI] [PubMed] [Google Scholar]
- 18.Shyam AK, Song HR, An H, Isaac D, Shetty GM, Lee SH. The effect of distraction-resisting forces on the tibia during distraction osteogenesis. J Bone Join Surg [Am] 2009;91(7):1671–1682. doi: 10.2106/JBJS.G.01238. [DOI] [PubMed] [Google Scholar]