Abstract
Purpose
Here we report the short-term clinical and radiological results of the Profemur®-R cementless modular revision stem.
Methods
Between June 2002 and May 2006, 68 revision hip arthroplasties were consecutively performed using this stem. Survival at a mean follow-up of 5.2 years was 94%. According to the Paprosky classification, the femoral defect was classified as type 1 in 39 hips (57.3%), type 2 in 18 hips (26.5%), type 3A in ten hips (14.7%) and type 3B in one hip (1.5%).
Results
The Harris Hip Score was 49.57 before surgery and averaged 78.28 at the latest follow-up. The Merle d’Aubigne score improved from 9.15 preoperatively to 14.30 postoperatively. Stem stability rated according to the Agora Roentgenographic Assessment (ARA) scoring system averaged 5.22, suggesting a high likelihood of a durable implant.
Conclusion
The revision prosthesis examined in this study can be considered a viable and useful option in revision hip arthroplasty, even in patients with bony femoral defects.
Introduction
Because people are living longer and primary total hip replacements are becoming more common in relatively young, physically active patients, the incidence of total hip arthroplasty (THA) is increasing rapidly, and revision and re-revision rates are expected to follow an equal growth [1]. Revision hip arthroplasty following femoral-component failure can be particularly challenging in the presence of poor bone quality and bone stock, altered femoral geometry and substantial femoral defects resulting from removal of the stem and cement mantle, all of which can compromise a stable and durable implant fixation. In many cases in which reconstruction with conventional procedures, such as those used in primary arthroplasty, is often not feasible, cementless, porous-coated, tapered and fluted monoblock stems have been successfully applied and are considered the gold standard by many surgeons [2–5].
As an alternative, modular revision stems allow the surgeon to customise each component to the intraoperative needs, as they allow independent preparation of the proximal and distal femur to optimise femoral fill and fit, thus avoiding stress shielding [6–9]. Moreover, leg length, offset and anteversion can be individually adjusted. So far, however, only a few authors have analysed the results of this type of stem, even though its value is still controversial [10]. To compare the various revision concepts and their results, and to understand failure mechanisms and thereby hopefully improve future developments, accurate radiographic and clinical studies are essential. The aim of this study was to review and report on our experience with the Profemur®-R modular stem (Wright Medical Technology, Arlington, TN, USA).
Materials and methods
Patients and methods
Between June 2002 and May 2006, 76 consecutive revision arthroplasties of the hip using the Profemur®-R modular revision stem were performed and retrospectively analysed. The mean age at surgery was 67 (range 34-83) years. No patients were lost to follow-up. The study population consisted of 34 male and 39 female patients, with an average body mass index (BMI) of 26 (range 22-40). A bilateral Profemur® R implant was used in three patients. Eight patients died during follow-up from unrelated causes, reducing the final study population to 68 implants, with an average follow-up of 5.2 (range 4–7.6) years. The main indications for revision were infection (n = 19) and aseptic loosening (n = 30) (Table 1). All infections were revised using a two-stage procedure with an intermediate preformed spacer [11]. Persistent pain from cup impingement and scintigraphically documented mid-thigh pain necessitated revision in one and five cases, respectively. Revision was also performed for failed osteosynthesis, including failure of either the plate and screw fixation or the intramedullary nails in one and nine cases, respectively, resulting in pseudarthrosis or secondary degeneration of the joint. One patient was treated for a proximal femoral osteosarcoma. Twenty-five patients had previously undergone revision surgery, including two hips that had already been revised two and three times, respectively.
Table 1.
Indications for revision in the study population using the Profemur-R stem
| Indication for revision | Number of hips |
|---|---|
| Aseptic stem and cup loosening | 9 |
| Aseptic cup loosening | 5 |
| Aseptic stem loosening | 16 |
| Failure of primary osteosynthesis | 10 |
| Infection | 19 |
| Periprosthetic fracture with component loosening | 2 |
| Persistent pain | 6 |
| Tumour | 1 |
Clinical and radiological evaluation
All follow-up data were collected prospectively. Clinically, patients were evaluated according to the Harris Hip Score (HHS), the University of California—Los Angeles (UCLA) score and the Merle d’Aubigne (MDA) score [12]. Radiographic evaluation, comprising anteroposterior and lateral radiographs, was performed preoperatively, postoperatively and at follow-up. Bone defects were classified according to the Paprosky classification [13]. The femoral defect was classified as type 1 in 39 hips (57.3%), type 2 in 18 hips (26.5%), type 3A in ten hips (14.7%) and type 3B in one hip (1.5%). A significant femoral-bone defect (type 3A or higher) was present in eight cases of the subgroup revised for infection. Implant stability was measured using the Engh fixation scale and the Agora Roentgenographic Assessment (ARA) scoring system [14]. Failure was defined as revision arthroplasty or radiographic evidence of femoral component loosening, indicated by an Engh fixation score ≤10 or an ARA score <2. Vertical femoral migration of >5 mm was defined as subsidence [15].
Operative technique
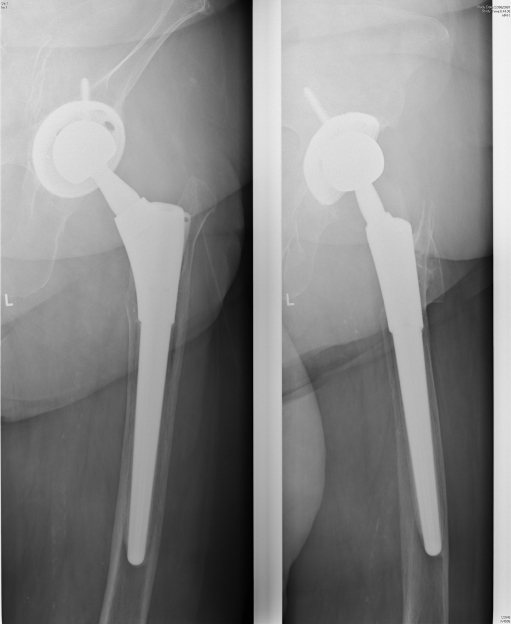
All revision operations were performed by the same senior surgeon through a posterolateral approach. If necessary, the approach was extended proximally or distally, depending on the intraoperative findings. Femoral-bone grafting was not performed in any of the procedures. Where possible, a posterior repair of the rotator soft tissue and capsule complex through drill holes in the posterior greater trochanter was performed at the end of each procedure to enhance stability. Mean blood loss was 884 (range 200–3,000) ml, and mean operating time was 144 (range 60–360) min. Postoperatively, indomethacin and low-molecular-weight heparin was administered for six weeks to prevent heterotopic ossification and thrombogenic complications, respectively. Patients were allowed partial or full weightbearing from day three postsurgery. In all cases, the Profemur®-R stem was used (Fig. 1). This cementless modular system is composed of four principal parts, which can be mounted by taper locks: a tapered distal stem with cutting flutes for the diaphyseal region, a proximal body, a modular neck and a head. The distal stem is available in diameter increments of 1 mm from 10 to 22 mm and in three lengths (135-mm straight, 157-mm curved and 215-mm curved). The two longer versions have an anatomical bowing. Radially arranged splines are extended along the distal stem. Fixation to the bone is obtained by press fit. The proximal parts are available in seven sizes to enable intraoperative adaptation to metaphyseal bone loss and are coated with hydroxyapatite. The ten neck sizes allow intraoperative adaptation to version, offset and leg length. A complete overview of all components used in this study population is provided in Table 2.
Fig. 1.
Profemur®-R modular hip system
Table 2.
Properties of the modular parts and bearing surfaces used in the study population
| Type of modular neck | No. | Size proximal part | No. | Size distal part | No. | Head diameter | No. | Bearing surfaces | No. |
|---|---|---|---|---|---|---|---|---|---|
| AR 15 long | 3 | Extra small | 1 | Short | 45 | 22 | 2 | Alumina – alumina | 6 |
| AR 15 short | 1 | Small | 25 | Medium | 18 | 28 | 11 | Alumina – PE | 5 |
| AR 8 long | 16 | Std 1 | 13 | Long | 5 | 32 | 31 | Alumina/PE – XLK (cross -inked) | 20 |
| AR 8 short | 4 | Std 2 | 13 | 36 | 11 | Metal – metal | 14 | ||
| AR/VV long | 8 | Std 3 | 9 | 50 | 6 | Metal – PE | 4 | ||
| AR/VV short | 3 | Std 4 | 6 | 54 | 3 | Metal – metal | 1 | ||
| S long | 21 | Large | 1 | 58 | 4 | Metal/PE – XLK (cross-linked) | 18 | ||
| S short | 7 | ||||||||
| VV long | 1 | ||||||||
| VV short | 4 |
AR15 15° anteversion/retroversion neck, AR 8 8° anteversion/retroversion neck, AR/VV 8° anteversion/retroversion with varus/valgus neck, S straight neck, VV varus/valgus neck, Std standard proximal part, PE polyethylene
In the 57 prosthetic revisions, both components were retrieved in 40 cases and both bearings in 48 cases. At the initial revision surgery, additional procedures were required in 29 cases: resection of a heterotopic ossification in one, and titanium cable cerclage in 28 [greater trochanter (n = 8), lesser trochanter (n = 1) and femoral diaphysis (n = 13))] Cable fixation had to be used for peroperative diaphyseal fracture (n = 8) or metaphyseal fissure (n = 14) on femoral implant removal or to close an additional transfemoral approach (n = 6).
Results
Clinical results
Clinical scores preoperatively and at latest follow-up of the 68 cases are illustrated in Table 3. Regarding HHS, there was mainly an increase for the pain score.
Table 3.
Clinical scores preoperatively and at latest follow-up of the entire study group
| Preoperative | Latest follow-up | |
|---|---|---|
| HHS global | 49.6 | 75.1 |
| MDA | 9.2 | 13.8 |
| UCLA | 3.8 | 5.0 |
| HHS – pain | 2.1 | 5.1 |
| HHS – walk | 2.8 | 4.3 |
| HHS – mobility | 4.3 | 4.9 |
HHS Harris Hip Score, MDA Merle d’Aubigne score, UCLA University of California—Los Angeles score
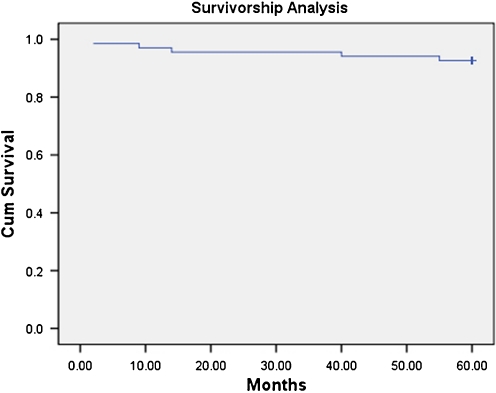
At a mean follow-up of 5.2 years, 63 (94%) stems were functioning well (Fig. 2). Five re-revisions had to be performed for various reasons. One case was revised for septic complications and was treated with a two-stage revision, again using the Profemur®-R. Two patients showed clear aseptic stem loosening (at a mean follow-up of four years), and one case was revised for measurable subsidence one year postoperatively (Fig. 3a–c). Those cases were revised on the femoral side, again using the Profemur®-R. In one case, re-revision was required due to femoral osteosarcoma recurrence, although the prosthesis was well fixed. In this case, a complete femoral resection was performed (Fig. 4).
Fig. 2.
Well-fixed Profemur®-R modular hip system in a 85-year-old female patient 5 years postsurgery
Fig. 3.
Seventy-seven-year-old female patient. a Profemur®-R system after two-stage revision 6 weeks postsurgery for infection. b Loosening and subsidence of Profemur®-R stem 3 years postsurgery due to undersizing. c Revision using a bigger Profemur®-R modular stem
Fig. 4.
Survivorship analysis of Profemur®-R system with cumulative survival at 5 years
Radiological results
Mean ARA and Engh scores were 5.22 and 25.16, respectively. Only seven patients had an ARA score ≤4. The two patients with a score <2 had obvious stem loosening. We observed lysis of the neck area in one case (1.5%), marked calcar atrophy in four (5.9%), subsidence/migration in one (1.5%), a reactive line <50% in three (4.4%) and reactive lines in Gruen zone 1a in five (7.4%). Pedestal was present in two cases (2.9%), but both were stable. Two cases (2.9%) presented cortical thickening in Gruen zone 5.
Complications
Table 4 provides an overview of all complications encountered during surgery and at follow-up. All intraoperative fissures or fractures occurred during removal of the primary prosthesis and not during insertion of the final implant. Titanium cable cerclage was used for stabilisation in all cases. As for late complications, the periprosthetic fracture was caused by trauma six weeks postoperatively. Dislocations occurred within six weeks postoperatively. The recurrent dislocation was triggered by trauma and required re-revision. The two single dislocations were treated by closed reduction and bracing for six weeks. We identified no failures of the modular taper connections at the different implant levels.
Table 4.
Complications
| Complications | Number |
|---|---|
| Intraoperative complications | |
| Fissure lesser trochanter or femoral diaphysis | 14 |
| Fracture greater trochanter | 8 |
| Early complications | |
| Superficial wound infection | 1 |
| Late complications | |
| Deep infection | 1 |
| Aseptic loosening | 1 |
| Subsidence | 1 |
| Single dislocation | 2 |
| Recurrent dislocation | 1 |
| Periprosthetic fracture | 1 |
| Recurrence femoral osteosarcoma | 1 |
Discussion
To prevent proximal femoral atrophy induced by stress protection, a femoral stem should guarantee proximal force transmission, as rigid distal fixation might cause stress shielding of the proximal bone with further loss of proximal bone stock [6]. The contact between the implant and the bone should be maximal in order to ensure an optimal fixation. This can be achieved by surgical preparation of the femoral canal and perfect adaptation of the prosthesis to the shape of the femur, proximally and distally. Other factors determining the clinical results are stability, soft-tissue tension, limb length and presence of adequate femoral diaphysis, all of which can only be evaluated at surgery.
Due to poor long-term results of cemented revision stems, surgeons typically rely on porous-coated cementless stems in the revision setting to obtain adequate diaphyseal fixation [16–18]. In primary THA, proximally porous-coated stems that depend on metaphyseal fit and contact have shown good results. However, in revision THA, intimate contact between implant and bone is often difficult to achieve due to the deficient and/or sclerotic metaphyseal bone. Therefore, results of revision THA with a monoblock proximally porous-coated stem are unsatisfactory [19, 20]. With the longer extensively porous-coated stems, the regions of proximally deficient bone can be bypassed, and stability and fixation in more distal femoral bone can be achieved. The shape of the tapered Profemur®-R stem with eight radially arranged splines may provide more rotational stability, especially in smooth sclerotic cortices. Spline height is proportional to stem diameter and decreases from its maximum height distally to its minimum height proximally, resulting in good fixation and rotational stability, even in plain cortices.
Although no clinical studies document improved outcomes with modular stems over one-piece stems, the modularity of the prosthesis has numerous benefits, especially intraoperatively. In the revision setting, metaphyseal and diaphyseal bone loss is highly variable. With one-piece stems of any type, it is difficult to position the femoral-head centre at the correct length, offset and anteversion. Flexibility during the operation provided by choices of stem length, diameter, fixation type and proximal stem size and orientation allows a stable hip centre to be established. Modular femoral components with multiple-sized proximal and distal parts been designed to achieve maximal fit and fill of the femoral bone, ensuring a correct and stable head centre. Complications, including dislocation, heterotopic ossification, intraoperative femoral fracture and infection, are seen with approximately the same frequency as in modular and one-piece distal bypass fixation revision stems [21–23].
Many other modular cementless revision stems are available on the market today. The surgeon’s personal experience will determine which type of stem offers him or her the best possible solutions. In this respect, the main author also has experience with the Revitan® cementless modular revision stem (Zimmer, Warsau, IN, USA). This system consists of a distal part, straight or curved, available in different lengths. The curved distal part can also be locked distally with screws, which may be an additional possible advantage in some cases [24]. The proximal part exists also in different lengths and can be connected to the distal part in any position regarding version. However, no modular necks are available with this system.
Regardless of the rather short-term follow-up, we observed no loosening or breakage of connections, although proximal bone support was not always present (≥40% Paprosky 2). Cases of breakage have described, for example, with the Zimmer Modular Revision Hip Systems (ZMR®, Zimmer,) which had to be withdrawn from the market in March 2003. Analysis of the failures by the Zimmer indicated that the predominant failure mode was fatigue fracture, which is usually associated with inadequate proximal bone support of the prosthesis. Although concerns exist about possible fretting corrosion between modular parts, no problems in this respect have been observed by us so far for the Profemur®-R systems.
Intraoperative femoral fissures and/or fractures were present in 22 cases (32%) in our study, which is more than in other studies with modular and nonmodular systems. They were all caused by primary prosthesis removal and not by implantation of the modular stem. Importantly, the frequency of these complications decreased as surgical expertise increased. The risk of an intraoperative femoral fracture has been shown to be highest when a cementless component is used in revision THA, [25].
As mentioned, five re-revisions were performed on a total of 68 implanted revision stems, with a revision rate of 7.35%. This is consistent with the findings of Köster et al., who had a re-revision rate of 6.1% [26]. It should be noted that the results of our study are preliminary because the operating surgeon was still gaining experience with the system. The cases of loosening and subsidence were all operated on before May 2004 and were clearly undersized on postoperative radiographs. They can be considered as a technical error due to the surgeon’s learning curve.
Clinical results at the latest follow-up are comparable with those of other studies regarding the difference between pre- and postoperative HHS, MDA and UCLA scores. The HHS improved to 78.28 points, i.e. an increase of 18.71%, which is consistent with other studies [26–29]. The MDA score increased most for the subcategory pain and least for mobility. Radiological follow-up showed very good ARA (mean 5.22) and Engh (mean 25.6) scores. Only two cases had an ARA score <2 and had to be revised for loosening and subsidence.
The modular uncemented diaphyseal fixation stem offers good conditions for bone restoration and seems capable of solving most of the technical problems in cases of extensive bone loss. This is confirmed by the good clinical results found at the final follow-up. Therefore, we conclude that the Profemur®-R stem provides a good alternative for patients with large femoral defects in the revision setting. However, surgical expertise is essential with this demanding type of surgery, and a longer clinical follow-up is required to assess the long-term outcome of this implant.
References
- 1.Pedersen AB, Johnsen SP, Overgaard S, Søballe K, Sørensen HT, Lucht U. Total hip arthroplasty in Denmark: incidence of primary operations and revisions during 1996-2002 and estimated future demands. Acta Orthop. 2005;76(2):182–189. doi: 10.1080/00016470510030553. [DOI] [PubMed] [Google Scholar]
- 2.Weeden SH, Paprosky WG. Minimal 11-year follow-up of extensively porous-coated stems in femoral revision total hip arthroplasty. J Arthroplasty. 2002;17(4 Suppl 1):134–137. doi: 10.1054/arth.2002.32461. [DOI] [PubMed] [Google Scholar]
- 3.Engh CA, Jr, Ellis TJ, Koralewicz LM, McAuley JP, Engh CA., Sr Extensively porous-coated femoral revision for severe femoral bone loss: minimum 10-year follow-up. J Arthroplasty. 2002;17(8):955–960. doi: 10.1054/arth.2002.35794. [DOI] [PubMed] [Google Scholar]
- 4.Paprosky WG, Greidanus NV, Antoniou J. Minimum 10-year-results of extensively porous-coated stems in revision hip arthroplasty. Clin Orthop Relat Res. 1999;369:230–242. doi: 10.1097/00003086-199912000-00024. [DOI] [PubMed] [Google Scholar]
- 5.Böhm P, Bischel O. Femoral revision with the Wagner SL revision stem : evaluation of one hundred and twenty-nine revisions followed for a mean of 4.8 years. J Bone Joint Surg Am. 2001;83-A(7):1023–1031. [PubMed] [Google Scholar]
- 6.Mulroy WF, Harris WH. Revision total hip arthroplasty with use of so-called second generation cementing techniques for aseptic loosening of the femoral component. A fifteen-year-average follow-up study. J Bone Joint Surg Am. 1996;78-A:325–330. doi: 10.2106/00004623-199603000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Cameron HU. The 3-6-year results of a modular noncemented low-bending stiffness hip implant. A preliminary study. J Arthroplasty. 1993;8(3):239–243. doi: 10.1016/S0883-5403(06)80084-7. [DOI] [PubMed] [Google Scholar]
- 8.Kwong LM, Miller AJ, Lubinus P. A modular distal fixation option for proximal bone loss in revision total hip arthroplasty: a 2- to 6-year follow-up study. J Arthroplasty. 2003;18(3 Suppl 1):94–97. doi: 10.1054/arth.2003.50083. [DOI] [PubMed] [Google Scholar]
- 9.Wirtz DC, Heller KD, Holzwarth U, Siebert C, Pitto RP, Zeiler G, Blencke BA, Forst R. A modular femoral implant for uncemented stem revision in THR. Int Orthop. 2000;24(3):134–138. doi: 10.1007/s002640000135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Köster G, Walde TA, Willert HG. Five- to 10-year results using a noncemented modular revision stem without bone grafting. J Arthroplasty. 2008;23(7):964–970. doi: 10.1016/j.arth.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 11.Pattyn C, De Geest T, Ackerman P, Audenaert E. Preformed gentamicin spacers in two-stage revision hip arthroplasty: functional results and complications. Int Orthop. 2010 Nov 30. DOI 10.1007/s00264-010-1172-8 [DOI] [PMC free article] [PubMed]
- 12.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51-A:737–755. [PubMed] [Google Scholar]
- 13.Della Valle CJ, Paprosky WG. The femur in revision total hip arthroplasty. evaluation and classification. Clin Orthop Relat Res. 2004;420:55–62. doi: 10.1097/00003086-200403000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Engh CA, Massin P, Suthers KE (1992 Nov) Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res 257:107–128, Erratum in: Clin Orthop 1992 Nov;(284):310-2 [PubMed]
- 15.McCutchen JW, Collier JP, Mayor MB. Osseointegration of titanium implants in total hip arthroplasty. Clin Orthop Relat Res. 1990;261:114–125. [PubMed] [Google Scholar]
- 16.Katz RP, Callaghan JJ, Sullivan PM, et al. Results of cemented femoral revision total hip arthroplasty using improved cementing techniques. Clin Orthop. 1995;319:178–183. [PubMed] [Google Scholar]
- 17.Pellicci PM, Wilson PD, Jr, Sledge CB, et al. Longterm results of revision total hip replacement: A follow-up report. J Bone Joint Surg Am. 1985;67-A:513–516. [PubMed] [Google Scholar]
- 18.Holt G, Hook S, Hubble M. Revision total hip arthroplasty: the femoral side using cemented implants. Int Orthop. 2011;35(2):267–273. doi: 10.1007/s00264-010-1167-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mulliken BD, Rorabeck CH, Bourne RB. Uncemented revision total hip arthroplasty: a 4-to-6-year review. Clin Orthop Relat Res. 1996;325:156–162. doi: 10.1097/00003086-199604000-00017. [DOI] [PubMed] [Google Scholar]
- 20.Berry DJ, Harmsen WS, Ilstrup D, Lewallen DG, Cabanela ME. Survivorship of uncemented proximally porous-coated femoral components. Clin Orthop Relat Res. 1995;319:168–177. [PubMed] [Google Scholar]
- 21.Engh CA, Culpepper WJ, 2nd, Kassapidis E. Revision of loose cementless femoral prostheses to larger porous coated components. Clin Orthop Relat Res. 1998;347:168–178. doi: 10.1097/00003086-199802000-00019. [DOI] [PubMed] [Google Scholar]
- 22.Krishnamurthy AB, MacDonald SJ, Paprosky WG. 5- to 13-year follow-up study on cementless femoral components in revision surgery. J Arthroplasty. 1997;12(8):839–847. doi: 10.1016/S0883-5403(97)90152-2. [DOI] [PubMed] [Google Scholar]
- 23.Moreland JR, Bernstein ML. Femoral revision hip arthroplasty with uncemented, porous-coated stems. Clin Orthop Relat Res. 1995;319:141–150. [PubMed] [Google Scholar]
- 24.Mertl P, Philippot R, Rosset P, Migaud H, Tabutin J, Velde D. Distal locking stem for revision femoral loosening and peri-prosthetic fractures. Int Orthop. 2011;35(2):275–282. doi: 10.1007/s00264-010-1182-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Davidson D, Pike J, Garbuz D, Duncan CP, Masri BA. Intraoperative periprosthetic fractures during total hip arthroplasty. Evaluation and management. J Bone Joint Surg Am. 2008;90-Am(9):2000–2012. doi: 10.2106/JBJS.H.00331. [DOI] [PubMed] [Google Scholar]
- 26.Köster G, Walde T, Willer HG. Five- to 10- year results using a noncemented modular revision stem without bone grafting. J Arthroplasty. 2008;23(7):964–970. doi: 10.1016/j.arth.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 27.Wirtz DC, Heller KD, Holzwarth U, et al. A modular femoral implant for uncemented stem revision in THR. Int Orthop. 2000;24:134–138. doi: 10.1007/s002640000135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Christie MJ, DeBoer DK, Tingstad EM, et al. Clinical experience with a modular noncemented femoral component in revision total hip arthroplasty: 4- to 7-year results. J Arthroplasty. 2000;15:840–848. doi: 10.1054/arth.2000.9059. [DOI] [PubMed] [Google Scholar]
- 29.Grünig R, Morscher E, Ochsner PE. Three-to 7-year results with the uncemented SL femoral revision prosthesis. Arch Orthop Trauma Surg. 1997;116(4):187–197. doi: 10.1007/BF00393708. [DOI] [PubMed] [Google Scholar]